Supplemental Digital Content is available in the text.
Abstract
Introduction:
Clinical pathways (CPs) translate best available evidence to the local care context and intend to inform clinical decision-making, optimize care, and decrease variation. This article describes a CPs program improvement process at a free-standing academic children’s hospital. Aims: (1) improve the pathway development process; (2) identify and address gaps; (3) strengthen measurement; (4) increase efficiency in cycle time to build a pathway; (5) increase multidisciplinary participation; (6) integrate into the electronic health record ; and (7) and increase pathway utilization.
Methods:
We renovated the CP program using a structured, improvement process. A series of internal stakeholder and external colleague interviews informed the process. To improve the program, we developed and implemented different interventions.
Results:
The streamlined process reduced the overall time for completion from a median of 15 to 5 months (measured from the date of first meeting with the clinical improvement team to approval), a 70% increase in efficiency. Between 1994 and 2015, the hospital had 33 CPs. There was a 78% increase in the total number of pathways after the renovation with 26 additional pathways.
Conclusions:
Renovation of the CP program led to early success through an improved development process, alleviation of programmatic gaps, inclusion of measures within each pathway, increased timely completion, multidisciplinary involvement, integration into the electronic health record, and improved utilization. Initial results are encouraging, and the lessons learned should be helpful to other programs. Further program development is ongoing, focusing on continued improvements in implementation and overall program measures.
INTRODUCTION
Clinical pathways (CPs) are a method used to implement available evidence into clinical practice to improve the standard of care for patients.1 CPs translate national guidelines and best available evidence into a usable format to help physicians and patients make decisions in specific clinical circumstances.2–4 More than 80% of US hospitals have implemented CPs.5 This method has been promoted to reduce unintended variation in care, unnecessary resource use, and improve the quality of healthcare.6–13
In 1994, the Children’s Hospital of Colorado (CHCO) implemented a process for the development of clinical care guidelines, now termed CPs. In 1995, the first guideline focused on bronchiolitis/viral pneumonia.7 The successful intrainstitutional adoption and clinical outcomes laid the foundation for the development of the CP program. In subsequent years, one full-time CP project manager created and distributed new pathways via paper or email to providers. While this allowed for the creation of pathways, there was little capacity to accelerate the process. Development, review, implementation, and tracking of any associated measures were at the discretion of the teams that developed/utilized each pathway.
The CP program renovation occurred via a structured, iterative quality improvement initiative with project management oversight. The specific aims were to: (1) improve the pathway development process; (2) identify and address gaps; (3) strengthen measurement; (4) increase efficiency; (5) increase multidisciplinary participation; (6) integrate into the electronic health record (EHR); and (7) increase pathway utilization.
METHODS
Context
CHCO is an academic center serving Colorado and the surrounding states. A central academic campus and 16 satellite Network of Care (NOC) locations provide care to children. There are approximately 700,000 outpatient visits annually including 150,000 emergency department/urgent care visits and approximately 19,000 inpatient admissions annually. We have had a single EHR since 2003 (Epic, Epic Systems, Madison, Wis.). The Organizational Research Risk and Quality Improvement Review Panel reviewed and approved this project as a quality improvement initiative.
Clinical Effectiveness Team
In 2014, CHCO formed a Clinical Effectiveness (CE) team consisting of one part-time medical and one full-time administrative director, 2 full-time project managers (including the CP project manager), 2 full-time process improvement specialists, and one full-time data analyst. This CE team fostered collaboration among clinical leaders to achieve best outcomes and improve clinical performance. CE achieved these goals through a systematic organization-wide approach to prioritization, design, measurement, and monitoring of clinical improvement (CI) activities. Oversight, development and implementation of clinical pathways (CPs) and related EHR solutions, measures, and data analytics were among the included activities although the team also participated in other process improvement projects across the hospital.
Gap Analysis and Interviews
The CP project manager conducted a needs assessment to identify gaps, challenges, and opportunities for improvement in CP development. The needs assessment included internal stakeholder interviews and external colleague interviews.
Eighteen internal stakeholders, representing a range of clinical disciplines (eg, medicine, nursing, pharmacy, and clinical informatics) participated (Table 1). We emailed the questions to each stakeholder one week in advance followed by an in-person interview. The interviews identified process gaps along with recommendations. Suggested alterations included the clear delineation and communication of tasks, roles, and timelines for CI team members (ie, pathway author teams), the careful selection of relevant metrics coupled with analytics support to inform and drive practice, and the creation of a multidisciplinary review body to evaluate and approve pathways.
Table 1.
Summary of Internal Stakeholder Interviews
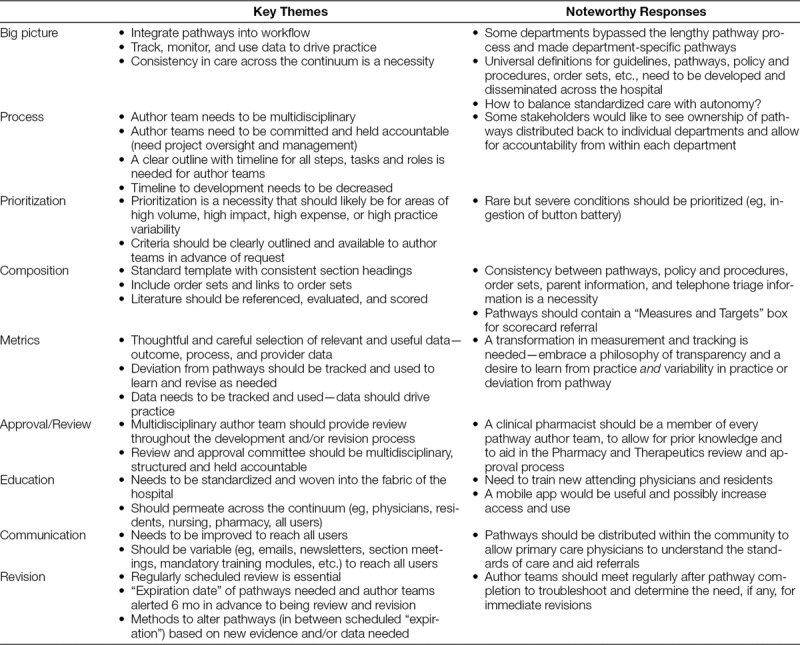
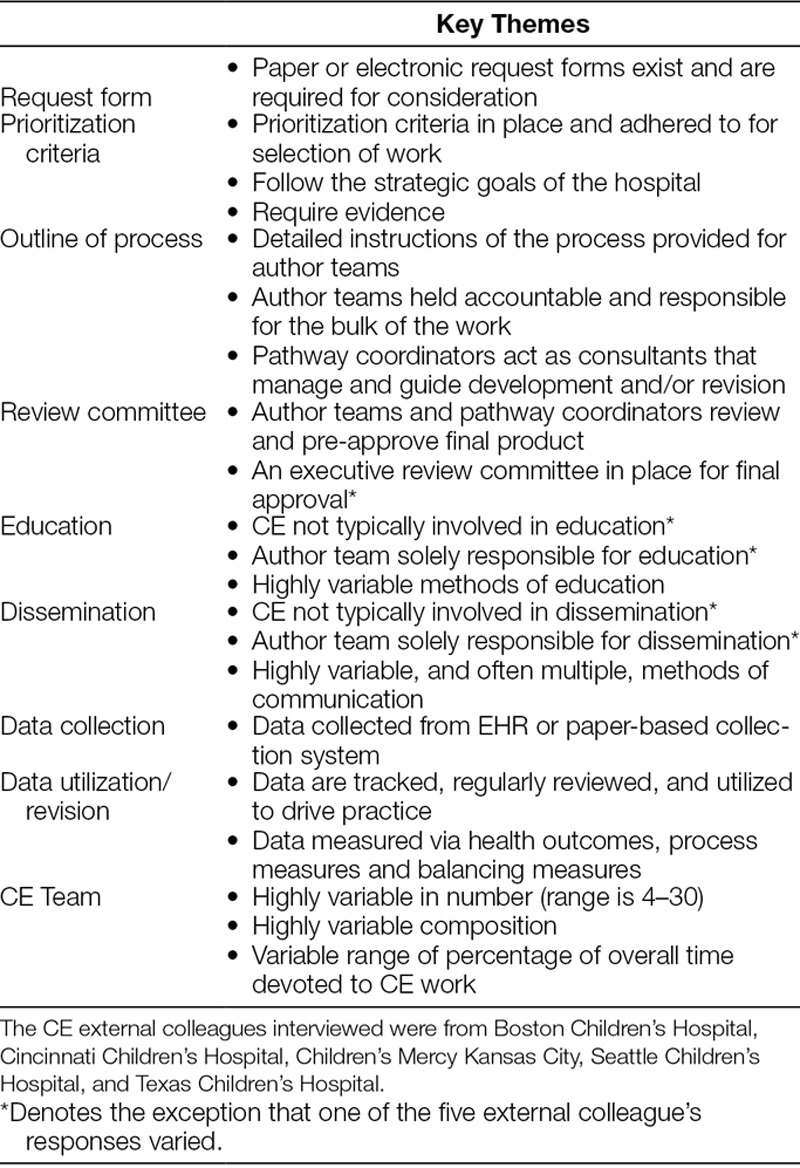
The CP project manager also interviewed external colleagues within established pathway programs from 5 peer hospitals. Each of the external colleagues identified common elements characteristic of a successful CP program (Table 2).
Table 2.
Summary of External Colleague Interviews
INTERVENTIONS
Request and Prioritization
We developed a project request form to capture details essential to prioritization of pathway development. Included details were the scope, clinical champion, team members, proposed measures, and the potential pathway impact. We designed a prioritization matrix, composed of 3 main scoring elements; impact, readiness, and resource requirements, to assess and score pathway requests. Quality (volume of patients, risk of patient population, reach of the work), cost (save money, resources, or both for the hospital or the patient), and experience (enhancement of the experience of the patient/family, care team, or provider) evaluated the impact. Cultural and/or organizational buy-in, the commitment of the clinical champion, and the clinical infrastructure available to support the CP work evaluated readiness. CE team staffing needs to successfully complete a pathway accounted for resource requirements. We created a Likert Scale with scores ranging from 1 to 4, where a “1” denotes no criteria fulfillment and a “4” fulfills all criteria in the category. High prioritization scores demonstrated high impact and commitment from the requesting CI team (Figure 1, CE Prioritization Rubric, available as Supplemental Digital Content 2 at http://links.lww.com/PQ9/A96).
Timelines and Process Maps
CP development timelines and process maps provided a comprehensive roadmap to CI teams undertaking the pathway development/revision process (Figs. 1 and 2). The pathway development timeline depicts a general overview of the process by stage (ie, prepare, develop, implement, and improve) along with team member roles and responsibilities. Process maps, for both new and revised pathways, represent the ideal state of progress and expand upon the timeline via the addition of granular detail for each stage, such as specific tasks and associated team member responsibilities.
Fig. 1.
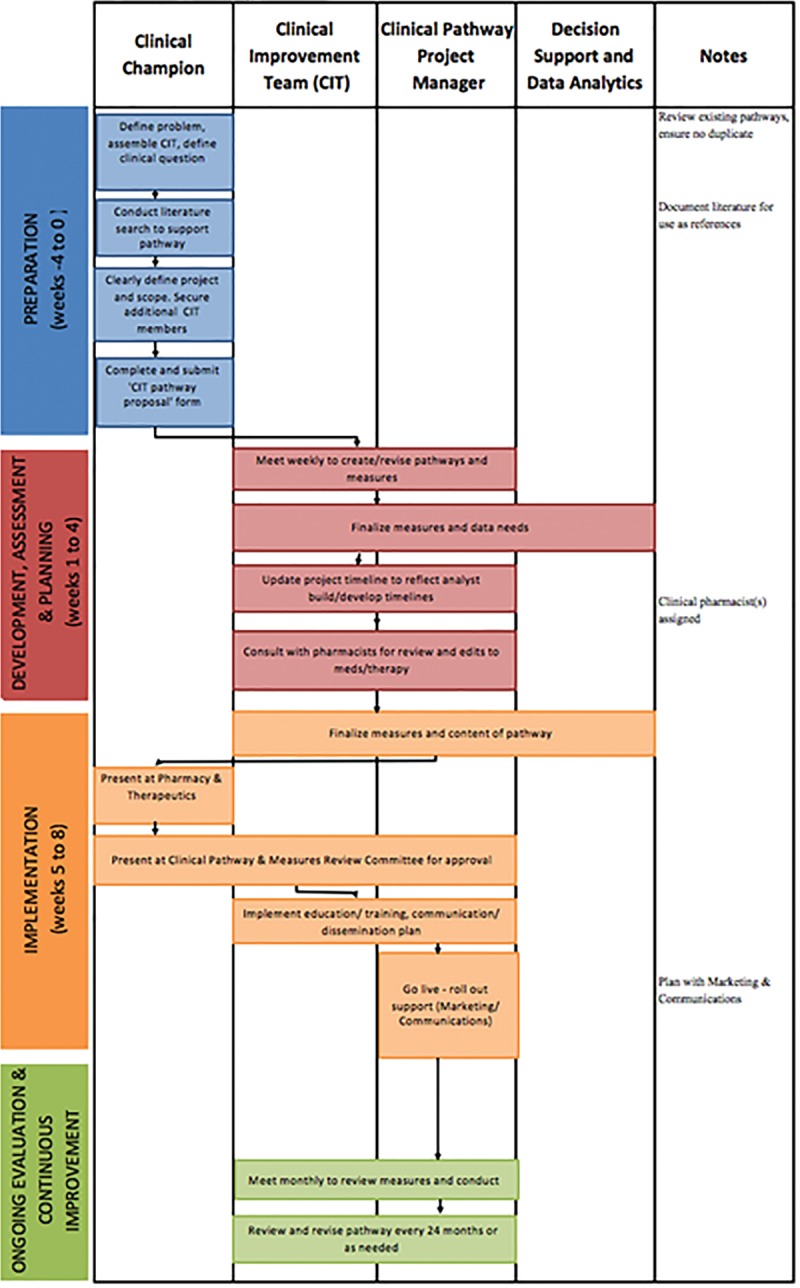
Clinical pathway development timeline for new pathways.
Fig. 2.
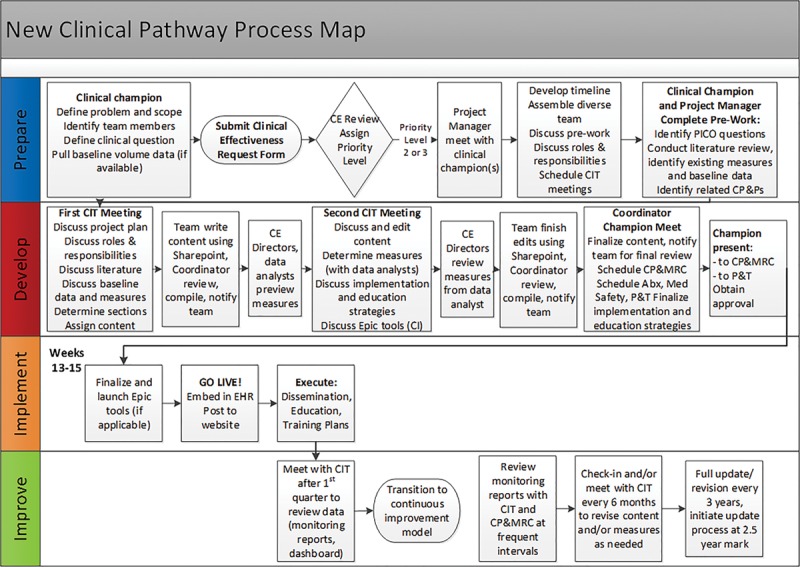
Clinical pathway development process map for new pathways.
Standardization of Content and Templates
In partnership with Marketing and Communication, we developed a template with standardized subheadings and algorithm specifications to provide consistency in layout and content across the pathways and the inclusion of similar and essential clinical information. A front-page algorithm served as an easy-to-access, one-page overview. We added a table of contents with embedded hyperlinks to allow for rapid access to commonly accessed portions of each pathway and a list of team members’ names, credentials, department, or unit of primary appointment and email addresses.
Collaboration and Editing
An internal, web-based platform (ie, SharePoint) improved efficiency of pathway development and allowed team members to more effectively collaborate via simultaneous access and editing of a shared electronic document.
Expanded Multidisciplinary and Cross-organizational Team Involvement
The CE team expanded the CI teams by inviting representation from all key departments, units, and roles impacted by the care described in the pathway. When possible, we invited stakeholders from NOC satellite sites, community-based primary care providers, and parents of patients to participate.
The CP project manager also formed a collaborative partnership with clinical pharmacy to streamline the review and approval of medications within new and/or revised pathways. The CP project manager attended monthly Pharmacy and Therapeutics committee meetings and notified them of upcoming new and/or revised pathways in need of pharmacy assistance. The Pharmacy and Therapeutics committee co-chair assigned pharmacists to CPs based on the pharmacist’s area of expertise to facilitate their involvement throughout the CP development/revision process.
Creation of a CPs and Measures Committee provided a monthly forum for the review and approval of new and/or revised pathway content, algorithms and measures. We invited multidisciplinary committee members with wide-ranging expertise. This committee included CE team members, hospital leadership, emergency medicine, hospital medicine, surgery, intensive care, and nursing. This committee also provided high-level strategic direction and served as a link to stakeholder groups from across the organization.
Electronic Health Record/Health Information Technology Integration
Incorporation of CPs into the provider workflow is necessary to enhance decision support and decrease unintended variation in care at the bedside and across patient encounters. Formation of a partnership with Clinical Application Services developed new tools in the EHR that would support pathway integration into the clinical workflow. Interactive, problem-solving “Technical Discovery Session” forums provided a venue for Clinical Application Services, Clinical Informatics (physicians and nurses trained in EHR building and analytics), CE, and CI teams to proactively brainstorm possible EHR tools and implementation strategies. Teams highlighted the “problem to be solved” and left the meeting with an action plan for developing an order set, clinical decision support tools, and/or new approaches to collect discrete data in the EHR for analytic purposes. This new approach facilitated increased access to pathways within the established clinical workflow.
New Dissemination and Education Tools
Three key strategies facilitated awareness and utilization of CPs. First, we created an internal-facing pathways page on the hospital intranet site to facilitate access for CHCO members. Second, we designed an external-facing website to disseminate pathways to community healthcare professionals. CE collaborated with the hospital’s provider relations team to educate community-based providers on new and updated pathways. Third, the CE team created a standardized dissemination template to assist CI teams in customizing a dissemination plan specific to pathway content and scope, paired with a contact list outlining key stakeholders in each department, unit, and location (Figure 2, Pathway Dissemination Plan, available as Supplemental Digital Content 2 at http://links.lww.com/PQ9/A97). As part of each pathway’s review/approval process the CI team presents the dissemination plan to the CPs and Measures Committee.
Measurement/Analytic Planning and Infrastructure Development
To ensure continual improvement of the pathway program, the CE team assigned measurement roles and responsibilities to report process, outcome, and balancing measures for each specific pathway and for the overarching program (Table 3).
Table 3.
Outcome, Process, and Balancing Measures
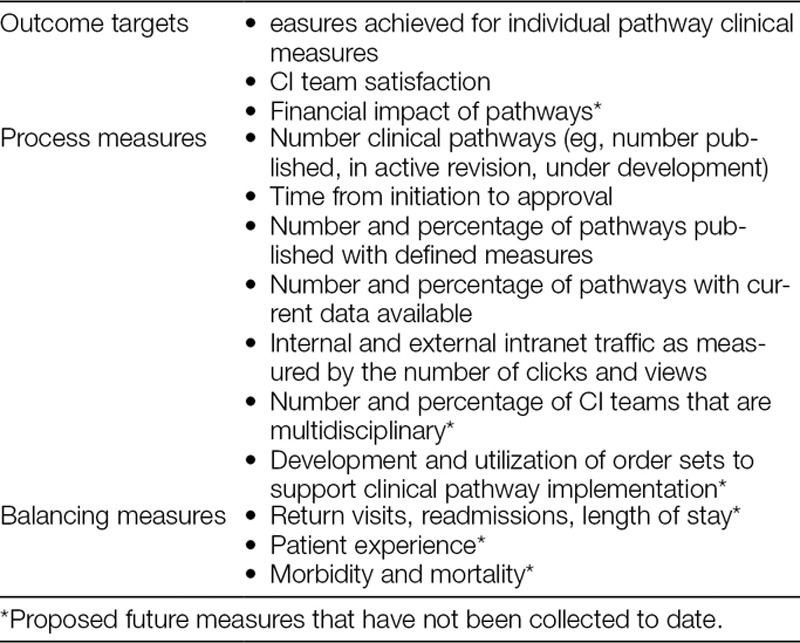
Pathway-specific process, outcome, and balancing measures are determined during CP development that align with nationally recognized measures, and serve as the basis for data analytics, reporting and continuous improvement. CE team clinical data analysts query baseline data from the EHR for pathway-specific measures, assist with data validation, and develop scheduled reports to allow for data monitoring over time.
We track specific program-level pathway measures for each pathway. Program-level process measures, such as the number of pathways integrated into the EHR, analyze the performance of several working “parts” within the pathway system. Proposed balancing measures, such as readmissions, alert users of unintended clinical outcomes related to the implementation of pathways. Program-level outcome measures, including the impact on CI teams, patients, their families, and the cost of care, track the impact of pathways across the organization.
RESULTS
Clinical Improvement Team Satisfaction
The CE program solicited feedback from a survey of 124 clinical team members conducted in February 2018. The survey yielded a 39.5% response rate. Of the 49 respondents, 57% were providers, 10% were nurses, and 33% were in other roles. In a question about partnership between CI teams and the CE team, 32% rated the partnership as “extremely effective” and 53% rated it as “pretty effective.” In general, all comments were positive regarding the program renovation, with a majority noting the increased coordination, guidance, and structure.
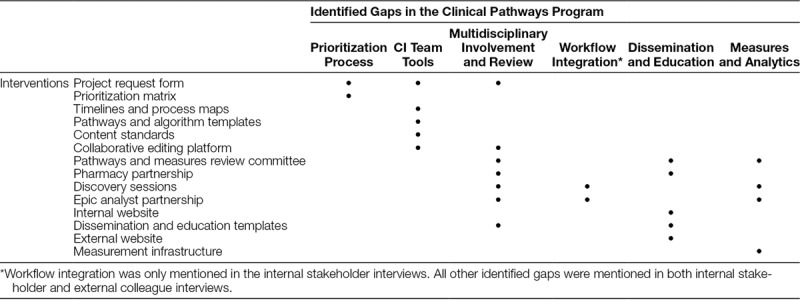
Summary of Gap Analysis
The identification of key gaps served as the foundation for the development of interventions designed to improve the efficiency and final product of the CP program (Table 4). All internal stakeholders universally identified the need to decrease the time to completion. Other gaps included the need for supplementary tools (process maps and timelines with defined roles and tasks) to guide the pathway development process, the need for pathway integration into the clinical workflow (EHR), the inclusion of valuable measures within each pathway and data/analytics to track measures and determine the impact of the pathways. Poor process efficiency before renovation was likely due to the lack of a clearly defined and structured pathway development process, and having only one full-time pathway project manager for the entire hospital.
Table 4.
Identified Gaps and Resulting Interventions
Volume and Improved Efficiencies in Pathway Development
The streamlined development process has reduced overall cycle time to build a pathway. Before program renovation, the initial median cycle time to pathway completion was 15 months, ranging from 6 to 24 months. The current median cycle time to pathway completion is now 5 months, ranging from 2 to 8 months, a 70% increase in efficiency. Between the year of the inception of the program and 2015, 33 CPs were available. As of May 2018, there were 56 completed pathways with 3 new pathways under development and 2 existing pathways under revision, which represents a 78% increase in the total number of CPs.
Number of Pathways with Measures and Current Data
The CP program renovation resulted in an increase in the number of pathways with clinically relevant associated measures with at least one outcome, process, and balancing measure for each pathway. Before program renovation 38% of the CPs had associated measures compared to 58% with measures as of May 2018. This increase was due to the incorporation of measures into new pathways and the addition of measures to revised pathways.
Multidisciplinary Clinical Improvement Teams
All CI teams are composed of providers from each involved specialty and ancillary staff with specialization in the pathway topic. To further improve the management of patients across care settings, we actively recruit a parent partner and a community-based primary care provider to participate in CP development. To date, 7 pathways involved a parent partner and 9 pathways involved a community-based primary care provider.
Electronic Health Record Integration
Before the CP program renovation, 17 of 33 (52%) CPs had related order sets and/or clinical decision support in the EHR. CPs were available as a word document and not embedded in the EHR. As of May 2018, 38 of 57 (67%) of the CPs have related order sets, and this number will continue to rise as we review and update the older pathways up for revision in 2019 and 2020. Only one pathway has a clinical decision support tool. The CPs are currently static reference documents housed within the EHR but are not within the provider workflow for active clinical decision support. Ongoing partnership with the EHR vendor will result in the continued development of new technological solutions for the interactive use of EHR pathways.
Dissemination and Education Tools
The internal-facing pathways page created on the hospital intranet site to facilitate access by CHCO team members had 13,120 views from May 2017 to May 2018. Asthma, diabetic ketoacidosis, urinary tract infection, bronchiolitis, and appendicitis were the 5 most frequently viewed pathways. The external-facing website designed to disseminate pathways to our community health care professional partners had 4,299 views from May 2017 to May 2018. Bronchiolitis, asthma, appendicitis, croup, and uncomplicated community acquired pneumonia CPs were the most often viewed externally.
DISCUSSION
There is evidence of early success in standardizing the CP development process as demonstrated by improvement in the overall development process, alleviation of gaps, improvement in the number of pathways with associated measures and efficiency increases, multidisciplinary involvement, integration into the EHR, and overall utilization. We believe these changes will help to reduce unnecessary variation in care provided for specific conditions within our hospital system and ultimately improve outcomes for children.14
The strengths of this program renovation included wide stakeholder engagement and involvement through a gap analysis and involvement of multidisciplinary improvement teams. With these iterative changes, we have increased the visibility of the CP program within our institution and observed a rise in pathway requests. We have increased our efficiency in cycle time to build a pathway, added associated tools within the EHR and implemented measures to determine if the CPs are effective.
Remaining Constraints
Although the implementation of a systematic approach to CP development has resulted in improvement across several areas, there are still several constraints.
Prioritization
In the context of prioritization, the CE team needs to continue to balance the need and demand for pathway development with the capacity of the CE team members.
Multidisciplinary Teams
Another constraint is the desire that each team be multidisciplinary and includes physicians from multiple disciplines and backgrounds, medical residents, community physicians, providers from the NOC, pharmacy, nursing, and parents. Although the compilation of a multidisciplinary CI team is critical to success, the actual coordination of such teams can be challenging.
Physician Autonomy
A limitation to utilization of CPs is constraint on physician autonomy. In the context of the creation of CPs intended for universal adoption throughout all affected medical specialties, the specialization of knowledge can become both a source of and a barrier to innovation. This division of expertise often creates boundaries that can become problematic when merging—or adhering to—knowledge between different medical specialties.
Location and Resources
The initial phase of the renovation of the CP program centered on the primary academic campus of the hospital. Although this could potentially limit internal spread and sustainability, the basic elements of each pathway should be universal and easily implemented at all satellite locations. As a large, metropolitan academic medical center, the findings from our program renovation may not easily extend to other smaller, more rural, or community-based programs. There may be resource constraints in other hospital settings that do not allow the generalizability of the described changes.
Measuring Effectiveness
Finally, measuring the effectiveness of the overarching CP program is challenging. Although we have process measures for the program overall, we continue to examine how to best demonstrate success of the program through effective outcome and balancing measures.
Next Steps
Broad goals for the future of the CP program involve the inclusion of at least one actively tracked clinically relevant outcome, process, and balancing measure within each pathway to allow for continual monitoring and assessment. Incorporation of pathways into the EHR, particularly at critical decision points, will allow for their use as interactive decision aids seamlessly integrated into provider workflow to foster utilization and adherence. Accessible and dynamic pathway measurement tools that integrate clinical, financial, and patient experience data will allow CI teams to better understand the impact of CPs in reducing unintended care variation and improve patient outcomes.
CONCLUSIONS
Using a systematic approach to identify and improve gaps in the CP program, we achieved important improvements in our cycle time to produce a pathway and in the number of pathways built. This will significantly enhance our ability to standardize best practices and serve as a necessary step to measure improvement in the value equation (outcomes/cost) into the future.
ACKNOWLEDGMENTS
We would like to acknowledge Denise Pickard, Mike Rannie, and Dr. James Todd for their innovative work that laid the foundation for the CP program at Children’s Hospital Colorado.
DISCLOSURE
This study was supported by departmental funds. The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online June 13, 2019.
Presented at the 2016 American Academy of Pediatrics (AAP) National Conference and Exhibition.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Pugh-Bernard A, Nickels S, Melendez J, Shawkat J, Rolison E, Swanson A, Bajaj L, Hyman D, Bakel LA. A Strategy for the Renovation of a Clinical Pathways Program. Pediatr Qual Saf 2019;3:e178.
REFERENCES
- 1.Campbell H, Hotchkiss R, Bradshaw N, et al. Integrated care pathways. BMJ. 1998;316:133–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kinsman L, Rotter T, James E, et al. What is a clinical pathway? Development of a definition to inform the debate. BMC Med. 2010;8:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawal AK, Rotter T, Kinsman L, et al. What is a clinical pathway? Refinement of an operational definition to identify clinical pathway studies for a Cochrane systematic review. BMC Med. 2016;14:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotter T, Kinsman L, James EL, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database of Syst Rev. 2010. [DOI] [PubMed] [Google Scholar]
- 5.Saint S, Hofer TP, Rose JS, et al. Use of critical pathways to improve efficiency: a cautionary tale. Am J Manag Care. 2003;9:758–765. [PubMed] [Google Scholar]
- 6.Johnson KB, Blaisdell CJ, Walker A, et al. Effectiveness of a clinical pathway for inpatient asthma management. Pediatrics. 2000;106:1006–1012. [PubMed] [Google Scholar]
- 7.Bekmezian A, Fee C, Weber E. Clinical pathway improves pediatrics asthma management in the emergency department and reduces admissions. J Asthma. 2015;52:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray AL, Alpern E, Lavelle J, et al. Clinical pathway effectiveness: febrile young infant clinical pathway in a pediatric emergency department. Pediatr Emerg Care. 2017;33:e33–e37. [DOI] [PubMed] [Google Scholar]
- 9.Donà D, Zingarella S, Gastaldi A, et al. Effects of clinical pathway implementation on antibiotic prescriptions for pediatric community-acquired pneumonia. PLoS One. 2018;13:e0193581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel NA, Bly RA, Adams S, et al. A clinical pathway for the postoperative management of hypocalcemia after pediatric thyroidectomy reduces blood draws. Int J Pediatr Otorhinolaryngol. 2018;105:132–137. [DOI] [PubMed] [Google Scholar]
- 11.DeLaroche AM, Sivaswamy L, Farooqi A, et al. Pediatric stroke clinical pathway improves the time to diagnosis in an emergency department. Pediatr Neurol. 2016;65:39–44. [DOI] [PubMed] [Google Scholar]
- 12.Chen SH, Yeh KW, Chen SH, et al. The development and establishment of a care map in children with asthma in Taiwan. J Asthma. 2004;41:855–861. [DOI] [PubMed] [Google Scholar]
- 13.Kaiser SV, Rodean J, Bekmezian A, et al. ; Pediatric Research in Inpatient Settings (PRIS) Network. Effectiveness of pediatric asthma pathways for hospitalized children: a multicenter, national analysis. J Pediatr. 2018;197:165–171.e2. [DOI] [PubMed] [Google Scholar]
- 14.Tyler A, Krack P, Bakel LA, et al. Interventions to reduce over-utilized tests and treatments in bronchiolitis. Pediatrics. 2018;141. [DOI] [PubMed] [Google Scholar]


