Abstract
We retrospectively identified autism spectrum disorder (ASD) incident cases among 31,220 individuals in a population-based birth cohort based on signs and symptoms uniformly abstracted from medical and educational records. Inclusive and narrow research definitions of ASD (ASD-RI and ASD-RN, respectively) were explored, along with clinical diagnoses of ASD (ASD-C) obtained from the records. The incidence of ASD-RI, ASD-RN, and ASD-C increased significantly from 1985–1998, then ASD-RI and ASD-RN plateaued while the rate of ASD-C continued to increase during 1998–2004. The rising incidence of research-defined ASD may reflect improved recognition and documentation of ASD signs and symptoms. Although the frequency of threshold ASD symptoms stabilized, the rate of ASD-C continued to increase, narrowing the gap between clinical ascertainment and symptom documentation.
Keywords: Autism spectrum disorder, incidence, epidemiology, time trends
Autism spectrum disorder (ASD) is a clinically and etiologically heterogeneous neurodevelopmental disorder characterized by early-onset deficits in social communication and interaction and an unusually restricted and repetitive repertoire of behaviors and interests (American Psychiatric Association 2013). ASD is associated with substantial health loss burden across the lifespan, and an accurate epidemiological description is needed to guide public health policy and to stimulate and inform etiologic research (Baxter et al. 2015; Christensen et al. 2016). Despite widespread attention to the marked increase in reported prevalence of ASD over the last 3 decades, identification and quantification of cases is complex and comparisons among existing studies are hampered by differences in study design and source populations, so uncertainties about time trends and other important aspects of the descriptive epidemiology of ASD persist (Baxter et al. 2015; Jensen et al. 2014).
In the early 2000s, it became common to use the term “autism spectrum disorders” to include the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) (American Psychiatric Association 2000) diagnostic categories autistic disorder (AD), Asperger’s disorder (AS), and pervasive developmental disorder not otherwise specified (PDDNOS) (Johnson and Myers 2007; Myers and Johnson 2007). This was prompted by research demonstrating that the separate diagnostic categories (AD, AS, and PDDNOS) had little scientific justification and were not used reliably, even by experts (Lord et al. 2012). Consequently, when the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) was published in 2013, the DSM-IV-TR diagnostic categories AD, AS, childhood disintegrative disorder (CDD), and PDDNOS were replaced by a single diagnostic term, ASD (American Psychiatric Association 2000; American Psychiatric Association 2013). Throughout this paper, we use ASD to represent, collectively, DSM-IV-TR-defined AD, AS, and PDDNOS.
When evaluating the epidemiologic literature, it is important to differentiate between incidence, the number of new ASD cases in a population occurring over a defined period of time divided by the amount of person-time observed, and prevalence, the proportion of individuals with ASD in the population at a given point in time. Incidence studies are usually the preferred approach to studying causation (i.e., whether an exposure increases disease occurrence) (Pearce 2012). Large, population-based longitudinal birth cohort studies are powerful resources for determining incidence rates and evaluating trends over time, which is crucial for informing etiologic research (Frost 1939; Liddell 1988; Hennekens and Buring 1987a; Katusic et al. 2017). As noted by Jensen and colleagues (Jensen et al. 2014), “studies on incidence rates from the same geographical area capture time trends more readily than studies reporting prevalence rates.” However, ASD incidence data adequate for examining time trends and assessing causation are scarce (Jensen et al. 2014; Raz et al. 2015; Baxter et al. 2015). Prevalence data, which are useful for identifying and planning for educational, social, and medical service needs as well as limited examination of time trends, are more readily available but quite variable in terms of source populations and study methods (Baxter et al. 2015; Hennekens and Buring 1987b; Jensen et al. 2014). Recent ASD prevalence rates in the United States (US) range from 1.25% in an analysis of a general population cohort using a commercial managed health care administrative database (Palmer et al. 2017) to 2.0%–2.41% in survey studies that determine prevalence based on parent report of ASD diagnosis (Blumberg et al. 2013; Zablotsky et al. 2015; Xu et al. 2018). Similarly, recent estimates based on national registry data in Sweden, Denmark, and Iceland were also over 1% (Idring et al. 2015; Saemundsen et al. 2013; Atladottir et al. 2015); parent-reported prevalence was 2.4% in 2010 and 3.9% in 2014 according to Australian surveys (May et al. 2017); and a prospective study from South Korea using active screening and follow-up diagnostic assessments yielded an estimated ASD prevalence of 2.64% (Kim et al. 2011).
Substantial increases in the estimated prevalence of ASD over the last 3 decades have been identified by studies using special education and developmental services administrative data (Newschaffer et al. 2005; California Department of Developmental Services 2007; Polyak et al. 2015), national family surveys (Schieve et al. 2012; Blumberg et al. 2013; Zablotsky et al. 2015; May et al. 2017), active public health surveillance conducted by the Centers for Disease Control (CDC) Autism and Developmental Disabilities Monitoring (ADDM) Network (Christensen et al. 2016; Baio et al. 2018), and national registries (Hansen et al. 2015; Isaksen et al. 2012; Saemundsen et al. 2013; Idring et al. 2015; Lundstrom et al. 2015; Raz et al. 2015). However, there is controversy about whether the available prevalence data actually establish that there has been a true increase in ASD (Brugha et al. 2011; Rice et al. 2012; Isaksen et al. 2013; Baxter et al. 2015). If there has been an increase in prevalence of ASD, it is not clear whether there has been a true secular increase in incidence due to etiologic factors in addition to the contribution of non-etiologic factors such as changes in identification and diagnostic practices, variation in study methods, and increased public awareness and availability of services (Christensen et al. 2016; Rice et al. 2012; Hansen et al. 2015; Lundstrom et al. 2015; Baxter et al. 2015).
As a step toward improving the understanding of the epidemiology of ASD, we retrospectively identified all incident cases of ASD in a large population-based birth cohort of individuals born in Olmsted County, Minnesota, between 1976 and 2000, using systematic medical and educational record-based identification of potential ASD (PASD) cases followed by detailed record abstraction and application of DSM-IV-TR-based operational ASD research criteria. ASD incidence was explored using two research definitions: A broader, more inclusive definition encompassing DSM-IV-TR AD, AS, and PDDNOS criteria (ASD-RI), and a more narrow, conservative definition based on DSM-IV-TR AD criteria (ASD-RN). We studied two ASD research definitions with different quantitative criterion thresholds for case definition because of the wide spectrum of severity among individuals with ASD, known distribution of ASD symptoms throughout the general population, and scientifically arbitrary nature of categorical diagnostic thresholds (Clark et al. 2017; Constantino 2011; Constantino and Todd 2003; Kamio et al. 2013; Hyman 2010; Posserud et al. 2006). The present paper has 2 primary purposes: (1) to provide a detailed description of the methods, procedures, and resources used to identify all incident cases of broadly and narrowly defined ASD in this well-characterized, longitudinally-followed population-based birth cohort, and (2) to present incidence rates and time trends of research-defined ASD (ASD-RI and ASD-RN) and clinically diagnosed ASD (ASD-C) by birth year and calendar year.
Methods
Study Setting
Olmsted County, Minnesota is 90 miles from any urban center and is home to Mayo Clinic. According to U.S. census data in 2000, the Olmsted County population is comparable to the U.S. with respect to median age (35.0 years vs. 35.3 years), and male gender (49.1% vs. 49.1%) (St Sauver et al. 2012a) The Olmsted County population is more racially homogeneous than the U.S. (white, 90.3% vs. 75.1%) enabling us to concentrate future investigations on other possible risk factors (e.g., biological characteristics, comorbidities, socioeconomic status), minimizing potential confounding due to race and ethnicity.
Study Resources
The Rochester Epidemiology Project (REP) medical record linkage system.
The REP captures longitudinal medical data for virtually all individuals who resided in Olmsted County Minnesota from 1966 to the present, regardless of age, sex, disease status, socioeconomic status, or insurance status (Rocca et al. 2012; St Sauver et al. 2012b; Melton 1996).
The REP is widely recognized as a unique resource for conducting population-based epidemiologic studies. Every Mayo Clinic patient, since 1907, has been assigned a unique identifier. As part of routine medical practice, detailed information from every encounter at Mayo Clinic, its two affiliated hospitals in Rochester, Minnesota, and its community practice clinics is contained in the patient-based medical record, including clinical documentation from primary care, psychiatry, other medical specialty and psychology clinics, emergency department visits, hospitalizations, and home visits as well as laboratory, radiology, and pathology results, social services reports, correspondence with private tutorial/therapeutic facilities, and birth/death certificate data. For persons who were born in Olmsted County, these data are available from birth until a patient no longer receives medical care in the community. Diagnoses assigned at each encounter are coded and maintained in continuously updated electronic files. Under the auspices of the REP, the diagnostic index and record linkage was expanded to include information from Olmsted Medical Center and its affiliated hospital and branch offices, and private practitioners in the region, beginning in 1966 (Rocca et al. 2012; Melton 1996; Kurland et al. 1970). The validity of the REP linkage methods and census enumeration are well-established, and many published studies have documented reliability and validity of specific variables considered in studies using the REP (Rocca et al. 2012; St Sauver et al. 2011; St Sauver et al. 2012a).
School Resources.
The Mayo Clinic Institutional Review Board, Independent School District (ISD) No. 535 school board, and equivalent authorities governing private schools, approved contractual research agreements to allow research team members to access the cumulative, richly documented school records of all birth cohort members ever registered at any of the 43 public, parochial, and private schools (including those who subsequently moved, graduated, or died) and those who were home schooled. Conditions and procedures developed to conduct studies using school records follow Minnesota Law concerning data privacy [M.S.13.32,subd.3(f)] and Federal Law concerning disclosure of personally identifiable information from educational records without prior consent [(34CFR99.31(a)(6)(i)(c)]. The cumulative school records include all school assessments, individual/group cognitive and achievement test results, Individualized Education Program (IEP) reports and long-term outcomes (e.g. dropout, expulsion, absenteeism, graduation status). They also include notes related to any type of learning difficulty or performance or behavior concern documented by teachers, therapists, school psychologists, physicians, social workers, school nurses, counselors, or parents, and correspondence with private tutorial/therapeutic facilities.
Study Population – Olmsted County Birth Cohort
The study population consists of all children born from January 1, 1976 through December 31, 2000 to mothers who were residents of Olmsted County at the time of the child’s birth (N=43,215) (Katusic et al. 2017). Among these 43,215 children, medical record access for research purposes was available for 39,890 children, in accordance with Minnesota state privacy law, statute 144.335. The target population for this study consists of 31,220 children who still lived in Olmsted County at or after 3 years of age, who we longitudinally followed from birth until adulthood, emigration, or death using the resources of the REP and ISD #535. The cut-off age of 3 years was chosen because the social, communication, and other behavioral characteristics of ASD are more consistently recognized at or beyond this age.
Identification of all Autism Spectrum Disorder (ASD) Incident Cases
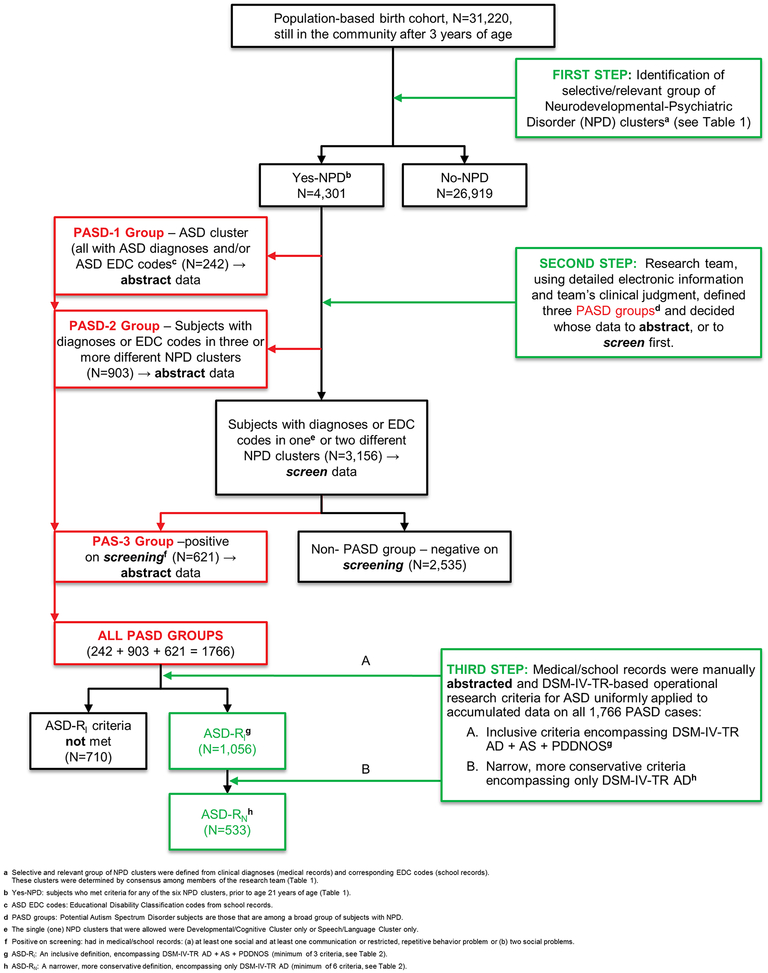
ASD case status was determined using two operational research definitions, inclusive (ASD-RI) and narrow (ASD-RN), so that incidence and time trends could be evaluated for each. The rigorous epidemiologic approach to identification of all ASD incident cases among the 31,220 birth cohort children who stayed in Olmsted County after 3 years of age consisted of three main steps (Figure 1), involving multiple sources of information from the REP and the public and private schools in ISD #535. The first step in identifying ASD incident cases, ascertaining individuals with selected relevant neurodevelopmental/psychiatric disorders (NPD), was an essential precursor to identifying cases with potential autism spectrum disorder (PASD) (second step), from which we then identified ASD incident cases (third step). This effort was led by a study team that consisted of a senior child psychologist, two developmental pediatricians, a speech/language pathologist, and an MD epidemiologist with 20 years of expertise in the research of childhood developmental and behavioral disorders.
Fig. 1.
Steps in identifying ASD incident cases.
First Step: Neurodevelopmental/Psychiatric Disorder (NPD) Case Definition and Identification
The initial step was to identify conditions with signs and symptoms overlapping the core social, communicative, and behavioral features of ASD and those that are commonly comorbid, or coexisting, with ASD, which we categorized within six broad NPD clusters based on clinical expertise and team consensus (Table 1). Individuals with these conditions were ascertained based on diagnostic codes from medical records and educational disability classification (EDC) codes from school records (Table 1). The clinical diagnoses within the REP from 1976 through 2015 were originally coded using two different coding systems, Hospital Adaption of the International Classification of Diseases, Eighth Revision (HICDA) and International Classification of Diseases, Ninth Revision (ICD-9), depending on the year of diagnosis and the source. For each of the 31,220 individuals in the birth cohort, the study statistician electronically obtained all ICD-9 and HICDA diagnosis codes prior to age 21 years from medical records and all EDC codes from educational records. This information was consolidated into an individual summary for each individual that included a separate line for each unique diagnosis code (and corresponding ICD-9 or HICDA text description), in chronological order from birth, along with the first and last date and number of times each diagnosis was recorded and the age at which it was first recorded. The summary also included the date of birth, date of last visit (whether associated with a diagnosis of interest or not), and EDC codes and dates from the school records. Based on this detailed information, 4,301 individuals were identified as NPD cases due to having at least one diagnosis or EDC code within one or more of the clusters (Table 1, Figure 1). Examples of diagnoses and EDC codes that comprise each of the six NPD clusters are described in the legend of Table 1. Individuals who only had codes in the neurologic/motor cluster were not classified as NPD cases if they did not have diagnoses or EDC codes in any of the other NPD clusters. Individuals were then prioritized into one of six NPD profiles based on their combination of NPD clusters (see rows of Table 1).
Table 1.
Neurodevelopmental/psychiatric disorder (NPD)a cases (N=4,301) within the population-based birth cohort (N=31,220)
Selective and relevant group of NPDs among whom all potential autism spectrum disorder (PASD) cases are identified. (See Figure 1).
The NPD clusters were defined from clinical diagnoses from the medical record and the corresponding educational disability classification (EDC) codes from the school records. These clusters were determined by consensus among members of research team (psychologist, two developmental pediatricians, speech/language pathologist, MD epidemiologist).
Individuals in each row have a diagnosis and/or EDC code in the NPD cluster with the solid black box with or without one or more of comorbid NPD clusters presented by gray boxes in corresponding row. Individuals with only Neuro/Motor clusters were not included as NPD cases. Rows were organized according to highest priority (i.e., significance) in identification of PASD.
ASD Cluster consisted of the EDC code for ASD along with ASD related diagnoses, for example: Autistic Disorder, Early Infantile Autism, Infantile Autism, PDDNOS, Autism Spectrum Disorders, Asperger’s Syndrome.
Childhood Psychosis Cluster included diagnoses such as childhood schizophrenia, childhood psychosis, and disintegrative psychosis.
Developmental/Cognitive Cluster included the EDC codes for developmental cognitive disabilities and developmental delay and diagnoses such as mental retardation/intellectual disability, borderline mental retardation/borderline intelligence, and delayed development.
Speech/Language Cluster consisted of the EDC code for speech/language impaired and diagnoses such as autistic speech, telegraphic speech, echolalia, and mixed receptive-expressive language disorder.
Non-Psychosis Childhood Psychiatric Cluster consisted of the EDC code for emotional/behavioral disorder and diagnoses such as attention-deficit hyperactivity disorder, hyperkinetic conduct disorder of childhood, obsessive-compulsive disorder, unspecified disturbance of conduct, oppositional disorder of childhood, self-injurious behavior, and anxiety disorders.
Neurologic/Motor Cluster included the EDC code for physically impaired and traumatic brain injury disabled and diagnoses such as epilepsy, seizure disorder.
Second Step: Potential ASD (PASD) Case Definition and Identification
From the group of individuals with NPD, we identified individuals with “potential ASD” (PASD). The PASD group is the population that went on to detailed record abstraction to identify research-defined ASD cases. This group represents the pool of patients with developmental and behavioral symptoms who present to clinicians for diagnosis and treatment. Using the NPD cluster profile data (see First Step) and a priori relative likelihood of harboring true ASD cases (determined by clinical expertise), three PASD groups were defined. These included two groups that would go directly to full record abstraction based on various combinations of diagnoses and EDC codes alone, and one group that required screening of a prioritized, relevant subset of records; in the latter case, only those who screened positive went on to full record abstraction (Figure 1):
PASD-1 group (Figure 1, Online Resource 1; N=242). This group consisted of all individuals with diagnoses or EDC codes in the ASD cluster, with or without comorbidity in the other NPD clusters, and their medical/school records were directly abstracted.
PASD-2 group (Figure 1, Online Resource 1; N=903). This group included individuals who had diagnoses or EDC codes in three or more different NPD clusters and whose medical/school records were directly abstracted.
- PASD-3 group (Figure 1, Online Resource 1; N=621). In order to identify the PASD-3 group, the medical records of the remaining 3,156 individuals who had diagnoses or EDC codes in either just one NPD cluster (if that cluster was developmental/cognitive or speech/language) or in two NPD clusters were screened to identify descriptions of problems that were congruent with ASD signs and symptoms specified in DSM-IV-TR. By using a strictly developed protocol for screening of prioritized relevant parts of medical records, two subgroups were identified:
- Those who were positive on screening (Figure 1, Online Resource 1), based on having either: (i) at least one social criterion and at least one communication or RRB criterion or (ii) two social criteria documented in their medical record, were classified into the PASD-3 group (N=621) and their medical/school records were abstracted.
- Those who were negative on screening were classified into the NON-PASD group (Figure 1, N=2535), and they were excluded from further work.
The NPD cluster profiles of the individuals in PASD-1 (N=242), PASD-2 (N=903), and PASD-3 (N=621) are summarized in Online Resource 1.
Third Step: Autism Spectrum Disorder (ASD) Incident Case Definition and Identification
Medical/school records of all individuals from PASD-1, PASD-2, and PASD-3 (N=1,766) were manually reviewed to abstract data through a systematic, multi-staged process allowing accumulation of all needed information in an established research folder for each PASD case. This was achieved by creating a data collection form, training data abstractors to follow a detailed protocol for abstraction of data using an extensive Data Dictionary (Online Resource 2), and implementing quality control procedures. The Data Dictionary was developed by research team members and consisted of relevant descriptive phrases found in medical or school records that correspond to 58 social, communication, and RRB signs/symptoms contributing to the 12 DSM-IV-TR “A” criteria (Online Resource 3) (American Psychiatric Association 2000). The abstractors met weekly with the senior child psychologist and with other team members as needed to discuss questions, and the Data Dictionary was continuously updated to include additional relevant descriptive phrases. The abstractors carefully read all documentation in the pertinent sections of each medical record, recorded prior to 21 years of age, to identify descriptive phrases that mapped to any of the 58 ASD sign/symptom categories in the Data Dictionary. For each subject, the abstractors recorded the first and last dates that the signs/symptoms were documented on each subject’s data collection form, along with the source (i.e., school or medical records) and who observed each problem (e.g., primary care or specialist physician, psychologist, speech-language pathologist, social worker, teacher, etc.). In addition, the abstractors also recorded the dates and scores from individually-administered IQ tests.
The study statistician used the abstracted information and the DSM-IV-TR-based operational research criteria (Table 2) to initially identify 1,296 individuals as research-identified ASD incident cases. The age at which research diagnostic criteria were met was based on the index date, defined as the earliest date when an individual met the minimum research criteria for ASD-RI; that is, the earliest date/age at which at least two social criteria and at least one communication or RRB criterion had been documented.
Table 2.
Operational research definitions of ASD based on DSM-IV-TRa criteria
| ASD-RIc | ASD-RNd | |
|---|---|---|
| Total # of criteria metb | ≥3 | ≥6 |
| Restricted, repetitive behavior | at least 1 | at least 1 |
| Exclusionary diagnosese: | CDD Rett’s disorder |
CDD Rett’s disorder |
Abbreviations: ASD: Autism spectrum disorder; ASD-RI: Research-defined ASD, inclusive criteria; ASD-RN: Research-defined ASD, narrow criteria; CDD: Childhood disintegrative disorder.
Due to retrospective nature of the data, which does not allow questioning the caregiver about the timing of symptom onset, the DSM-IV-TR age of onset (<3 years) criterion was not included.
Criteria determination is based on problems abstracted from medical and educational records, representing 58 groups of signs and symptoms of ASD that map to 12 distinct DSM-IV-TR criteria (4 social interaction, 4 communication, and 4 restricted, repetitive behavior) (Online Resource 3).
ASD-RI: The inclusive research definition of ASD (ASD-RI), which encompasses the DSM-IV-TR autistic disorder (AD), Asperger’s disorder (AS), and pervasive developmental disorder not otherwise specified (PDDNOS) diagnostic categories, is based on the criteria for PDDNOS, which required “severe and pervasive impairment in the development of reciprocal social interaction associated with impairment in either verbal or nonverbal communication skills or with the presence of stereotyped behavior, interests, and activities…” (American Psychiatric Association, 2000). We operationalized “severe and pervasive impairment in the development of reciprocal social interaction” as meeting 2 of the 4 social interaction criteria (also required for AD and AS). Additionally, the definition requires meeting at least 1 of the communication criteria or 1 of the restricted, repetitive behavior criteria.
ASD-RN: A subset of individuals with ASD-RI also meet stricter, more narrow research criteria (ASD-RN) based on the DSM-IV-TR criteria for AD (a total of at least 6 criteria met, including at least 2/4 social interaction criteria, 1/4 communication criteria, and 1/4 restricted, repetitive behavior criteria).
Exclusionary diagnoses were identified by diagnostic codes and confirmed by expert review of the records.
The final step in the identification of all ASD incident cases consisted of identifying and excluding potential false positives. This work involved manually reviewing the organized detailed information for each of 1,296 initial ASD incident cases using the clinical expertise of the research team. For each individual, members of the research team reviewed the consolidated summary described in the first step, supplemented with information on psychiatric diagnoses (e.g., psychosis, depression, bipolar disorder, etc.) along with the first and last date and number of times each diagnosis was recorded and the age at which it was first recorded; details of abstracted ASD problems congruent with DSM-IV-TR criteria (problem category, age, and who observed the problem); and IQ scores, type of test, and age at administration. Based on this information, clinical judgments were made by the research team, and individuals whose abstracted signs/symptoms were more clearly the result of conditions other than ASD (such as adolescent-onset psychosis, bipolar disorder, or major depression) were excluded from ASD incident case group. This final step identified 1,056 ASD-RI and 533 ASD-RN incident cases in the population-based birth cohort of 31,220 individuals. These ASD incident cases and the PASD groups from which they were identified are specified in Table 3.
Table 3.
To help to control for changes in special education laws and DSM criteria over the nearly 4 decades of data collected (1976–2015), two procedures were in place: 1) regardless of originally assigned medical diagnoses (all diagnoses related to the 6 NPD diagnostic clusters) or school handicap codes (from MN Department of Education), ASD signs/symptoms were uniformly abstracted from medical/school records of all 1,766 PASD cases; 2) our research criteria for ASD status were uniformly applied to the accumulated abstracted data for all 1,766 PASD cases.
Statistical Analysis
Statistical analyses were conducted using R version 3.4.2 (R Core Team 2017). We used a log-Gaussian Cox process (Møller et al. 1998) with a Bayesian Smoothing Spline ANOVA covariance function (Reich et al. 2009; Storlie et al. 2013) to model the incidence of clinically diagnosed ASD (ASD-C) and research-identified ASD (ASD-RI and ASD-RN), respectively, prior to 21 years of age across age, birth year and gender. This model adjusts for issues such as censoring and imbalance of gender, age, and birth year. The model is fit in a Bayesian framework with weak priors using a Markov chain Monte Carlo algorithm to approximate the posterior distribution of the incidence curve across birth year, age, and gender. Unless stated otherwise, the estimates provided below use the posterior mean as a point estimate and 95% credible intervals (CIs) to summarize the uncertainty. A subject’s duration of follow-up was calculated from their date of birth until the event date prior to 21 years of age; otherwise their follow-up was censored at the earliest of either their last clinical visit to a REP-affiliated provider prior to December 31, 2015 or their 21st birthday. Incidence rates by calendar year are expressed as cases per 1000 person-years and cumulative incidence rates by birth year are expressed as cases per 100 individuals. Because of birth cohort includes individuals born during 1976 to 2000, the various estimates by calendar year are only presented for the period 1985–2004, due to the fact that individuals are aging-in and aging-out of the cohort. For example, an estimate of an incidence rate in 2010 would require a substantial extrapolation since there are no individuals aged 0–9 years in this study in the year 2010. The model-based approach does allow for some extrapolation, within reason. We settled on 1985–2004 as a good compromise, since in 1985 there are individuals aged 0–10 years in the data, and in 2004, there are individuals aged 4–21 years in the data. The peak age of diagnosis in this study occurred at age 6 to 7 years.
Results
Of the 31,220 individuals still in the community after 3 years of age who comprise the study cohort, 51.3% were male and 82.6% were Caucasian. Just 14.4% had their last clinical visit to a REP-affiliated provider at less than 15 years of age, and 57.9% had clinical follow-up beyond 21 years of age. As noted in Figure 1, 1,766 individuals were identified as potential ASD (PASD) cases; among them, 1,056 (3.38% of the cohort) met the inclusive research criteria for ASD (ASD-RI) and 533 (1.71%) met the narrow research criteria for ASD (ASD-RN) by age 21 years. In addition, 242 individuals (0.78% of the cohort) had been identified clinically as having ASD (ASD-C) based on medical diagnoses and/or educational classification; 234 (97%) of the 242 clinically-diagnosed individuals met the inclusive research criteria (ASD-RI) and 210 (87%) met the narrow research criteria (ASD-RN). One individual had a confirmed diagnosis of Rett syndrome (0.003% of the cohort). Demographic and follow-up characteristics of the study cohort are presented in Table 4, including the breakdown of race, gender, ASD diagnostic criteria, and age at last follow-up for each birth period.
Table 4.
Demographic and follow-up characteristics of the 31,220 individuals still in the community after 3 years of age who comprise the study cohort
| Measure | Birth Period | Overall | ||||
|---|---|---|---|---|---|---|
| 1976–1980 | 1981–1985 | 1986–1990 | 1991–1995 | 1996–2000 | ||
| No. in community after 3 years of age | 5298 | 6393 | 6831 | 6466 | 6232 | 31,220 |
| Baseline | ||||||
| Male gender, N (%) | 2778 (52.4%) | 3300 (51.6%) | 3450 (50.5%) | 3288 (50.8%) | 3193 (51.2%) | 16009 (51.3%) |
| Race, N (%) | ||||||
| White | 3956 (74.7%) | 5162 (80.7%) | 5928 (86.8%) | 5692 (88.0%) | 5056 (81.1%) | 25794 (82.6%) |
| Asian | 24 (0.5%) | 76 (1.2%) | 197 (2.9%) | 224 (3.5%) | 314 (5.0%) | 835 (2.7%) |
| Black or African American | 14 (0.3%) | 20 (0.3%) | 36 (0.5%) | 102 (1.6%) | 339 (5.4%) | 511 (1.6%) |
| Hawaiian or Pacific Islander | 3 (0.1%) | 8 (0.1%) | 5 (0.1%) | 15 (0.2%) | 15 (0.2%) | 46 (0.1%) |
| American Indian or Alaskan Native | 9 (0.2%) | 12 (0.2%) | 25 (0.4%) | 15 (0.2%) | 17 (0.3%) | 78 (0.2%) |
| Other | 45 (0.8%) | 98 (1.5%) | 98 (1.4%) | 163 (2.5%) | 307 (4.9%) | 711 (2.3%) |
| Unknown or chose not to disclose | 1247 (23.5%) | 1017 (15.9%) | 542 (7.9%) | 255 (3.9%) | 184 (3.0%) | 3245 (10.4%) |
| ASDa criteria | ||||||
| No. met ASD-RI criteriab | 69 | 163 | 294 | 278 | 252 | 1056 |
| Age met ASD-RI criteria, Median (IQR) | 9.7 (7.4, 14.3) | 10.3 (7.2, 13.1) | 8.8 (6.7, 12.0) | 7.5 (5.2, 10.4) | 6.7 (4.2, 9.4) | 8.1 (5.7, 11.3) |
| No. met ASD-RN criteriac | 23 | 55 | 135 | 146 | 175 | 533 |
| Age met ASD-RN criteria, Median (IQR) | 7.8 (5.8, 12.9) | 7.7 (5.9, 10.0) | 7.6 (5.2, 10.6) | 6.6 (4.6, 8.8) | 5.6 (3.7, 8.6) | 6.9 (4.4, 9.5) |
| No. met ASD-C criteriad | 6 | 14 | 53 | 65 | 104 | 242 |
| Age met ASD-C criteria, Median (IQR) | 15.3 (13.5, 16.7) | 12.8 (10.1, 16.0) | 10.4 (7.9, 14.1) | 7.0 (4.2, 12.0) | 5.4 (3.3, 8.4) | 7.5 (4.3, 12.4) |
| Follow-up | ||||||
| Age at last follow-up for individuals not meeting the ASD-RI criteria | ||||||
| Median (IQR) | 32.9 (22.2, 36.4) | 29.1 (22.4, 31.8) | 25.0 (21.9, 26.7) | 21.0 (19.4, 22.5) | 16.3 (14.9, 17.8) | 22.3 (17.6, 27.7) |
| Categorized, N (%) | ||||||
| 3 - <6 years | 306 (5.9%) | 286 (4.6%) | 376 (5.8%) | 366 (5.9%) | 399 (6.7%) | 1733 (5.7%) |
| 6 - <10 years | 202 (3.9%) | 189 (3.0%) | 246 (3.8%) | 217 (3.5%) | 257 (4.3%) | 1111 (3.7%) |
| 10 - <15 years | 154 (2.9%) | 188 (3.0%) | 160 (2.4%) | 154 (2.5%) | 911 (15.2%) | 1567 (5.2%) |
| 15 - <21 years | 435 (8.3%) | 529 (8.5%) | 626 (9.6%) | 2345 (37.9%) | 4413 (73.8%) | 8348 (27.7%) |
| 21+ years | 4132 (79.0%) | 5038 (80.9%) | 5129 (78.5%) | 3106 (50.2%) | 0 (0.0%) | 17405 (57.7%) |
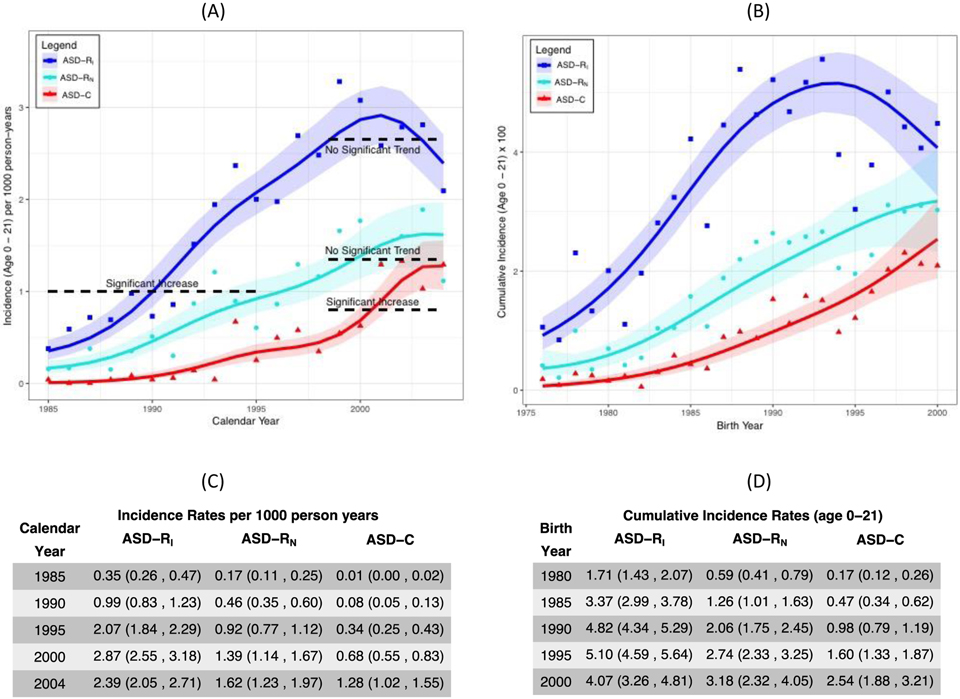
Figure 2(A) presents the incidence of ASD-RI, ASD-RN, and ASD-C (per 1000 person-years) by calendar year of first meeting criteria, averaged across gender and age (0–21 years). The solid curves are the respective posterior mean estimates for ASD-RI, ASD-RN and ASD-C incidence, while the bands are 95% simultaneous credible bands (CBs). That is, 95% of curves from the posterior distribution will fall entirely within these bands. These CBs can be used to draw statistical inference with respect to trends. If a horizontal line from one year to another cannot fit inside the bands, then there is a statistically significant trend during that time period. For example, in Figure 2(A), the horizontal line drawn between calendar year 1985 and 1995 cannot fit inside of the CBs for ASD-RI. Therefore, we can conclude that the incidence of ASD-RI was increasing as a function of calendar year. Similar logic allows us to conclude that there is no significant trend in ASD-RI between 1998 and 2004. However, there was a significant increase in the incidence of clinical diagnosis of ASD-C during 1998 to 2004. As presented numerically in Figure 2(C), in 1985, the incidence of ASD-C was 0.01 cases/1000 person-years (95% CI: 0.00, 0.02), and the incidence of ASD-RI was 0.35 cases/1000 person-years (95% CI: 0.26, 0.47). By 2004, the incidence of ASD-C increased to 1.28 cases/1000 person-years (95% CI: 1.02, 1.55), which was significantly different from 2000 (0.68 cases/1000 person-years [95% CI: 0.55, 0.83]). In contrast, by 2004, the incidence of ASD-RI also increased to 2.39 cases/1000 person-years [95% CI: 2.05, 2.71], but it was not significantly different from 2000 (2.87 cases/1000 person-years [95% CI: 2.55, 3.18]).
Fig. 2.
(A) Incidence by age 21 (per 1000 person-years) of research-identified inclusive (ASD-RI) and narrow (ASD-RN) autism spectrum disorder and clinically diagnosed autism spectrum disorder (ASD-C), according to calendar year of first meeting criteria and averaged across gender. See body of text in the Results section for explanation of the horizontal dotted lines used to draw statistical inference with respect to trends. (B) Cumulative incidence by age 21 (×100) of research-identified autism spectrum disorder (ASD-RI and ASD-RN) and clinically diagnosed autism spectrum disorder (ASD-C), according to birth year and averaged across gender. The solid curves for both (A) and (B) are the respective posterior mean estimates for ASD-RI, ASD-RN and ASD-C incidence, while the bands are 95% simultaneous credible bands; 95% of curves from the posterior distribution will fall entirely within these bands. (C) Numerical data corresponding to (A). (D) Numerical data corresponding to (B).
In Figure 2(B) a similar pattern is evident in the cumulative incidence of ASD-RI, ASD-RN and ASD-C by age 21 years, according to birth year, averaged across gender. Specifically, there is a significant rise in ASD-RI, ASD-RN, and ASD-C among individuals born between 1976 and 1993. However, cumulative incidence of ASD-RI and possibly ASD-RN seemingly stopped increasing for birth years 1993 onward (i.e., leveling off), whereas the cumulative incidence of ASD-C continued to increase in a statistically significant manner. As summarized numerically in Figure 2(D), for individuals born in 1980, the cumulative incidence of ASD-C was 0.17% (95% CI: 0.12, 0.26), and the cumulative incidence of ASD-RI was 1.71% (95% CI: 1.43, 2.07). However, while the cumulative incidence of ASD-C increased to 1.60% (95% CI: 1.33, 1.87) and 2.54% (95% CI: 1.88, 3.21) for individuals born in 1995 and 2000, respectively, the cumulative incidence of ASD-RI was not significantly different for individuals born in 1995 compared to 2000 (5.10% [95% CI: 4.59, 5.64] and 4.07% [95% CI: 3.26, 4.81]).
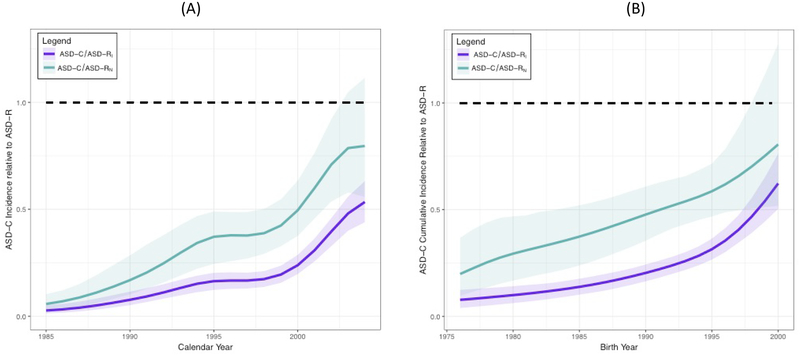
The rate ratio (RR) for the incidence of ASD-C relative to ASD-RI and ASD-RN according to calendar year is presented in Figure 3(A). Although in calendar year 1998 individuals were 87% (RR=0.13) less likely to receive a clinical diagnosis of ASD than meet criteria for ASD-RI, individuals were just 44% (RR=0.56) less likely in 2004. In other words, the gap between ASD-C and ASD-RI has been narrowing, especially since 1998. Figure 3(B) presents the rate ratio (RR) for the cumulative incidence of ASD-C relative to ASD-RI and ASD-RN, respectively according to birth year.
Fig. 3.
(A) Rate ratio of ASD-C incidence to ASD-RI and ASD-RN incidence, respectively, according to calendar year. (B) Rate ratio of ASD-C cumulative incidence to ASD-RI and ASD-RN cumulative incidence, respectively, according to birth year. The solid curves are the respective posterior mean estimates for ASD-RI and ASD-RN incidence, while the bands are 95% simultaneous credible bands; 95% of curves from the posterior distribution will fall entirely within these bands.
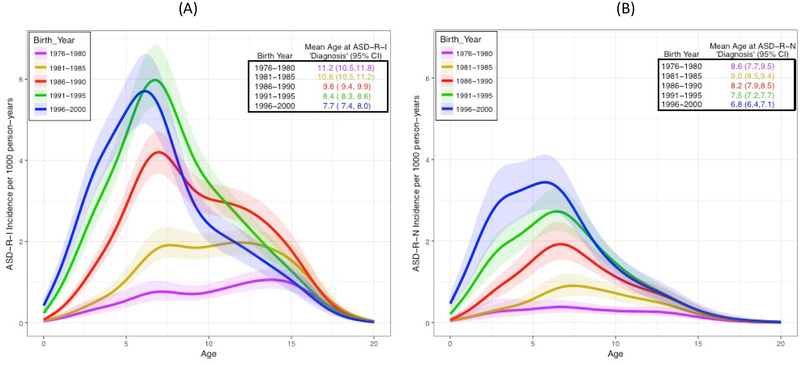
Figure 4 depicts the age-specific ASD-RI and ASD-RN incidence (per 1000 person-years) for five separate birth periods (averaged across gender); the mean age of meeting criteria for each birth period is also summarized within each figure. As shown in Figure 4(A), not only has the incidence of ASD-RI increased in the later birth periods, but individuals are continually meeting the ASD-RI criteria at a younger age, and thus the mean age of meeting the ASD-RI criteria has significantly decreased across the 4 most recent birth periods. Similar trends across the birth periods were observed for the age-specific ASD-RN incidence (Figure 4(B).
Fig. 4.
The age-specific incidence per 1,000 person-years for five separate birth periods (averaged across calendar year) for (A) ASD-RI and (B) ASD-RN. The solid curves are the respective posterior mean estimates for ASD-RI and ASD-RN incidence, while the bands are 95% simultaneous credible bands; 95% of curves from the posterior distribution will fall entirely within these bands.
Discussion
Uncertainties about incidence rates, time trends, and other important aspects of the epidemiology of ASD persist, due in part to a dearth of large, population-based incidence studies in which the same diagnostic criteria are applied uniformly over an extended time period. Within a population-based birth cohort of 31,220 individuals who were born in Olmsted County, Minnesota between 1976 and 2000 and remained in the community beyond 3 years of age, we retrospectively identified 1,056 (3.38%) who met inclusive research criteria for ASD (ASD-RI; encompassing DSM-IV-TR AD, AS, and PDDNOS criteria) by the time they reached 21 years of age, moved out of the community, or died. Included among the 1,056 individuals were 533 individuals (1.7%) who met a more narrow, conservative research definition of ASD (ASD-RN; based on DSM-IV-TR AD criteria). Record review revealed that 242 individuals (0.78% of the study cohort) had been identified clinically as having ASD (ASD-C) based on medical diagnosis, educational classification, or both. However, these crude frequency rates do not account for duration of follow-up, and incidence rates are a more relevant means of examining frequency of occurrence of a disease or disorder.
ASD incidence and time trends
When incidence rates (age 0–21 years, expressed per 1000 person-years) are evaluated by calendar year in which diagnostic criteria were met, it is evident that ASD-RI, ASD-RN, and clinically-diagnosed ASD (ASD-C) increased significantly between 1985 and 1998, then the incidence of ASD-RI and ASD-RN began to plateau while ASD-C continued to increase between 1998 and 2004 (Figure 2A). This resulted in a reduction of the discrepancy between research-defined ASD and clinically diagnosed ASD incidence rates over time (Figure 3). A similar pattern is observed when cumulative incidence to age 21 years is examined according to birth year. For conditions in which the diagnosis tends to be stable and the mortality rate is low, such as ASD, prevalence and cumulative incidence measures are virtually identical over a defined time or age period, so the two measures are comparable across studies if matched appropriately(Rice et al. 2012). The cumulative incidence of ASD-RI, ASD-RN, and ASD-C increased significantly among individuals born between 1976 and 1993 (Figure 2(B)), followed by stabilization of the rates of ASD-RI and ASD-RN among individuals born from 1993 through 2000, while the cumulative incidence of ASD-C continued to increase significantly. We performed a sensitivity analysis restricting follow-up to prior to age 15. Thus, all subjects, including the individuals born in 2000, had the opportunity for a full 15 years of follow-up, and the pattern of increasing incidence followed by stabilization was the same (Online Resource 4).
The pattern of rising ASD occurrence followed by leveling-off has also been observed in several studies of ASD frequency among 8-year-old children (Christensen et al. 2016; Raz et al. 2015; Taylor et al. 2013). For example, an Israeli study utilizing a comprehensive national database demonstrated a rise in ASD prevalence from 2000 to 2012 (birth years 1992–2004), followed by apparent stabilization (Raz et al. 2015). Similarly, the CDC ADDM Network reported a rise in ASD prevalence in each 2-year period from 2000 to 2010, but no change between 2010 and 2012 for the 8 sites (representing 78% of the total study population) that submitted methodologically comparable data for both surveillance years (Christensen et al. 2016). However, this apparent plateau may not have continued through 2014, since there was a statistically significant increase in estimated ASD prevalence from 2012 (1.75%) to 2014 (2.0%) in the 4 ADDM Network sites with methodologically comparable data from those surveillance years (Baio et al. 2018). Whether these 4 sites, which represented 35% of the total study population for 2012 and 2014 and reported higher ASD prevalence (1.75 % in 2012 and 2.0% in 2014) than the other 7 sites (1.36% in 2012 and 1.6% in 2014), are representative enough of the total study population to conclude that there was an overall increase among the 11 sites is unclear. Another study, conducted in the UK, found an earlier plateau in annual incidence of ASD; after rising sharply during the 1990s, steady state was reached in the early 2000s and maintained through 2010 (Taylor et al. 2013). In the present study (Online Resource 5), cumulative incidence to age 8 years of research-defined ASD (ASD-RI and ASD-RN) followed a pattern similar to cumulative incidence to age 21 years, increasing throughout the 1980s and early 1990s and then leveling off for the 1993–2000 birth year groups (i.e., prevalence among 8-year-olds began to level off around calendar year 2001, about a decade earlier than the plateau in the US and Israeli studies but very similar to the UK study).
The rising incidence of research-defined ASD may reflect improved recognition and documentation of ASD signs and symptoms due to increased public and professional awareness (Keyes et al. 2012; Idring et al. 2015; Liu et al. 2010), until a plateau was reached beginning in 1998. Although the occurrence of ASD symptoms, as determined by meeting ASD-RI or ASD-RN criteria, was stable from 1998–2004, the rate of clinical diagnosis continued to increase, narrowing the gap between clinical ascertainment and symptom documentation (Figures 2 and 3). Stability of ASD symptoms during a period of increasing clinical diagnosis of ASD was also observed in a large Swedish population over a 10-year period from 1993–2002 (Lundstrom et al. 2015). In addition, several studies have provided evidence that a shift over time toward diagnosing ASD in individuals with less severe symptoms has contributed to the increasing prevalence of ASD (Keyes et al. 2012; Whitehouse et al. 2017; May et al. 2017). This type of temporal change in the threshold at which clinicians make a diagnosis provides one explanation of how the rate of ASD-C could increase in the absence of evidence of a change in the frequency of symptoms during the same period of time. The absence of a significant increase in ASD symptoms sufficient to meet ASD-RI or ASD-RN during the late 1990s and early 2000s (Figure 2(A) and 2(B)) does not support the hypothesis that there was a secular increase in the rate of ASD phenotype during that time period, despite the increasing rate of clinical diagnosis. Instead, our findings are more consistent with the other studies described, which suggest a shift in diagnostic threshold resulting in a continued rise in clinical diagnosis despite unchanging frequency of documented signs and symptoms.
Professional and public awareness of ASD increased dramatically during the study period. For example, from 1980–2010 there was a 12-fold increase in the number of annual ASD research publications, with a rapid increase beginning in 2000 and a growth rate far greater than that for comparable research areas (Office of Autism Research Coordination (OARC)). The impact of social influences such as increased awareness of ASD and availability of diagnostic resources is apparent not only in general incidence and prevalence studies, but also in studies of spatial variation; much of the geographic variation in ASD occurrence is explained by these factors, and not by risk factors such as maternal age, birth year, sex, community income, or prenatal exposure to air pollutants (Hoffman et al. 2017; Keyes et al. 2012; Liu et al. 2010; Mazumdar et al. 2013; Wing and Potter 2002).
It is possible that the introduction of autism to the DSM in 1980 (DSM-III), substantial changes in the DSM diagnostic criteria in 1987 (DSM-III-R), 1994 (DSM-IV), and 2013 (DSM-5), and perhaps even minor changes in 2000 (DSM-IV-TR), contributed significantly to changes in prevalence by influencing clinical documentation of symptoms. There is evidence, for example, that changes in diagnostic criteria and practices contributed substantially to increases in ASD prevalence in Denmark and Australia based on registry and administrative data (Bent et al. 2017; Hansen et al. 2015; Nassar et al. 2009). The DSM-III-R (1987) and DSM-IV (1994) definitions were more inclusive than that of DSM-III (1980) and allowed increased diagnostic flexibility, whereas the DSM-5 (2013) definition is less inclusive and represents a move toward a more rigorous definition with higher specificity (Baker 2013; Smith et al. 2015). However, any potential impact of DSM criteria changes on clinical documentation of symptoms in the present study is speculative. It is difficult to quantify the precise magnitude and timing of the impact of changes in diagnostic criteria on diagnosis or clinical documentation of symptoms due to variation in timing of professional awareness and clinical uptake as well as potential confounding factors such as concurrent legislation, professional training initiatives, and public awareness campaigns that may also have contributed to increased awareness and changes in documentation (DeVilbiss and Lee 2014; Hansen et al. 2015; Park et al. 2016). For example, in addition to acute effects, changes in DSM diagnostic criteria might have led to gradual changes due to growing awareness of signs and symptoms of ASD among clinicians or orientation of standardized rating scales and diagnostic instruments to the new criteria, in which case the temporal lag between the criteria changes and associated changes in ASD diagnosis might make associations difficult or impossible to identify (Smith et al. 2015; Hansen et al. 2015).
Age at which diagnostic criteria were first met
As ASD symptom documentation and clinical diagnosis of ASD increased, the mean age at which ASD-RI and ASD-RN were met declined significantly, which is consistent with other studies demonstrating a decrease in the mean age at which ASD is diagnosed (Baio et al. 2018; Jensen et al. 2014; Christensen et al. 2016; Raz et al. 2015). It is likely that increased parent and professional awareness was responsible for more frequent and earlier recognition and documentation of ASD symptoms.
Comparison of ASD-C to other studies using passive case ascertainment
Methodological differences allow only limited comparison of our data to previously published studies, since incidence data from large, population-based birth cohorts with active case ascertainment across a broad age range over several decades are not available. Studies that are available for comparison vary widely in case-finding methods, ages included, and source populations. Registry-based studies and other study designs that rely on passive ascertainment of clinically-diagnosed individuals are generally assumed to provide conservative, or lower-limit, estimates of occurrence (Rice et al. 2012; Jensen et al. 2014; Baxter et al. 2015), and are most comparable to our ASD-C group, which represents a retrospectively ascertained registry of individuals in the birth cohort who had received a medical diagnosis and/or educational classification of ASD. The frequency of clinical ASD classification (ASD-C) in our cohort increased throughout the study period, confirming the reports of increased prevalence from other registry and service database studies (Atladottir et al. 2015; Davidovitch et al. 2013; Hansen et al. 2015; Jensen et al. 2014; Keyes et al. 2012; Lundstrom et al. 2015). Because the result of the analysis is an estimate of the incidence curve as a function of birth year, age, and gender, we can convert this result as needed for direct comparison to various estimates of other quantities reported from other studies using different cohorts. For example, the cumulative incidence rates of ASD-C through 2011 for four 3-year birth cohorts (1.09% for birth years 1990–1992, 1.37% for 1993–1995, 1.61% for 1996–1998, and 1.75% for 1999–2000) in Olmsted county were similar to prevalence rates in Denmark for the same birth year groups (1.09%, 1.51%, 1.47%, and 1.36%), whereas corresponding prevalence rates in Finland, Sweden, and Western Australia were somewhat lower, particularly in the later birth-year cohorts (Online Resource 6) (Atladottir et al. 2015). The annual incidence rates (age 0–8 years) of ASD-C in our cohort were 2- to 3-times those in the UK General Practice Research Database for each year between 2004 and 2010, and the cumulative incidence rates through age 8 years (i.e., the prevalence among 8-year-olds) were 4- to 6.5-times the comparable UK registry prevalence rates (Online Resource 7) (Taylor et al. 2013).
Active case ascertainment: ASD-RI and ASD-RN
Clearly, more individuals met criteria for ASD based on symptoms uniformly abstracted from records (ASD-RI, ASD-RN) than were clinically diagnosed (ASD-C) (Figure 2(A) and 2(B)). For example, the average cumulative incidence of ASD by age 21 years among individuals born in the youngest 5-year birth cohort group (born 1996–2000) was 4.6% using the inclusive research definition, 3.0% using the narrow research definition, and 2.1% based on clinical diagnosis. This is consistent with the fact that studies that utilize active case ascertainment typically find higher rates of ASD than those involving passive case ascertainment (Kim et al. 2011; Rice et al. 2012; Blumberg et al. 2013; Zablotsky et al. 2015; Baxter et al. 2015; Christensen et al. 2016; Baio et al. 2018). Our protocol for active retrospective ascertainment of ASD cases included a broader, more inclusive case definition (ASD-RI) and a more narrow, conservative case definition (ASD-RN), reflecting other research showing that ASD traits vary widely in severity and are distributed throughout the general population (Constantino 2011; Constantino and Todd 2003; Posserud et al. 2006; Kamio et al. 2013), and acknowledging the scientifically arbitrary nature of categorical diagnostic thresholds (Clark et al. 2017; Hyman 2010). These research definitions of ASD represent compilations of core signs and symptoms derived from 12 DSM-IV-TR core criteria (American Psychiatric Association 2000). ASD-RN is based on the AD definition and therefore requires a minimum of 6 criteria from 3 categories (including at least 2 social, 1 communication, and 1 RRB), whereas ASD-RI is designed to encompass AS and PDDNOS as well as AD, so a minimum of 3 criteria are required (2 social and 1 either communication or RRB). The research-defined ASD incidence estimates, therefore, reflect two different semi-quantitative thresholds for case definition based on ASD signs and symptoms and, necessarily, the rates are higher when the lower threshold is used to define a case (ASD-RI). ASD-RI and ASD-RN could be viewed as upper and lower limit estimates, respectively, of the true ASD incidence range.
Comparison of ASD-RI and ASD-RN to other studies using active case ascertainment
Our research-defined ASD (ASD-RI and ASD-RN) cumulative incidence data can be compared to some degree with data from prevalence studies utilizing various types of active case ascertainment. For example, the CDC ADDM Network active surveillance system also utilizes review of medical records at all sites (though the sources are limited to health care providers who evaluate and treat children with developmental disabilities) and educational records at some, but not all, sites (Christensen et al. 2016; Baio et al. 2018). As demonstrated in Table 5, our cumulative ASD incidence estimates through age 8 years (i.e., prevalence among 8-year-olds) and the CDC ADDM Network estimates of ASD prevalence in 8-year-old children (Christensen et al. 2016; Baio et al. 2018) can be directly compared for surveillance years 2000–2008 (birth years 1992–2000). The CDC ADDM Network ASD prevalence rates are similar to the ASD-C rates from our study (e.g., 95% CIs from our study overlap with the ranges across sites provided by CDC) and both CDC ASD and Olmsted county ASD-C prevalence rates increased throughout the overlapping surveillance years. Although the prevalence rates of ASD-RI and ASD-RN in our cohort are much higher than the overall CDC ASD prevalence rates through the same birth years, our ASD-RI prevalence rate for 2008 is comparable to the CDC site with the highest prevalence rate (2.46% versus 2.12%), and our ASD-RI and ASD-RN prevalence rates have leveled off in the more recent periods (Christensen et al. 2016). The differences may be attributable to methodological issues involving case ascertainment, comprehensiveness of available records, data abstraction strategies, and perhaps differences in community access to diagnosticians. In contrast, our estimates of cumulative incidence through age 5 years among children born in 1994–1996 were generally lower than those obtained in a Japanese study using a prospective two-stage screening-confirmation approach (Kawamura et al. 2008) (Online Resource 8). However, our ASD-RI and ASD-RN estimates are close to those obtained in a South Korean study involving prospective ascertainment of cases via population-based screening over a 1-year period in 2005/2006 followed by diagnostic evaluation of screen-positive cases (also a two-stage screening-confirmation approach), which estimated the prevalence of ASD among 7- to 12-year-old children to be 2.64% (95% CI 1.91, 3.37) (Kim et al. 2011). Our corresponding estimates of prevalence among 7- to 12-year-old children in 2005 are taken to be the average of the corresponding cumulative incidence rates for children in the same age range (i.e., birth years 1993–1998, through ages 7 to 12 years): 3.10% for ASD-RI (95% CI 2.85, 3.35), 1.81% for ASD-RN (95% CI 1.60, 2.00), and 0.84% for ASD-C (95% CI 0.72, 0.96). Notably, the 95% confidence intervals for ASD-RI and ASD-RN overlap with those found by Kim et al (Kim et al. 2011).
Table 5.
ASD prevalence rate among 8-year-olds reported by the CDC ADDM Network along with the estimated prevalence rate of ASD-RI, ASD-RN, and ASD-C among 8-year-olds from the same birth years in our cohort
| Birth year | Surveillance year | CDC prevalence (range)a | ASD-C prevalence (95% CI)b | ASD-RN prevalence (95% CI)c | ASD-RI prevalence (95% CI)c |
|---|---|---|---|---|---|
| 1992 | 2000 | 0.67 (0.45, 0.99) | 0.43 (0.32, 0.54) | 1.39 (1.16, 1.66) | 2.57 (2.26, 2.91) |
| 1994 | 2002 | 0.66 (0.33, 1.06) | 0.61 (0.47, 0.76) | 1.65 (1.35, 1.91) | 2.90 (2.57, 3.29) |
| 1996 | 2004 | 0.80 (0.46, 0.98) | 0.90 (0.72, 1.09) | 1.92 (1.52, 2.30) | 3.01 (2.66, 3.48) |
| 1998 | 2006 | 0.90 (0.42, 1.21) | 1.21 (0.93, 1.49) | 2.14 (1.57, 2.59) | 2.82 (2.39, 3.23) |
| 2000 | 2008 | 1.13 (0.48, 2.12) | 1.44 (1.09, 1.82) | 2.29 (1.56, 2.96) | 2.46 (1.98, 2.89) |
| 2002 | 2010 | 1.47 (0.57, 2.19) | |||
| 2004 | 2012 | 1.46 (0.82, 2.46) | |||
| 2006 | 2014 | 1.68 (1.31–2.93) |
Abbreviations: ASD: Autism Spectrum Disorder; CDC: Centers for Disease Control; ADDM: Autism and Developmental Disabilities Monitoring; ASD-C: clinically-diagnosed ASD; ASD-R: research-defined ASD (narrow and inclusive)
Average of the CDC ADDM Network ASD prevalence estimates (per 100 children) at different ADDM network sites. Range for CDC estimates represents the range the CDC prevalence at different ADDM network sites (Christensen et al. 2016).
ASD-C: prevalence estimates per 100 children for clinically diagnosed ASD; 95% CI for the ASD-C is 95% a credible interval for the ASD-C prevalence.
ASD-RN and ASD-RI: research-defined ASD (narrow and inclusive, respectively); 95% CIs for the ASD-RI and ASD-RN are 95% credible intervals for the ASD-RI and ASD-RN prevalences, respectively.
Study Strengths
Methodology is fundamentally important in determining ASD incidence and prevalence estimates (Baxter et al. 2015; Kim et al. 2011; Fombonne 2009). Despite the retrospective nature of our study, there are substantial methodological strengths, including the unique large, population-based birth cohort, active case ascertainment across a broad age range, uniform application of the same DSM-IV-TR-based operational research diagnostic criteria throughout the entire study period, availability of comprehensive medical and educational records, and longitudinal follow-up over many years, all of which have been emphasized as desirable features for studies of the epidemiology of ASD (Yeargin-Allsopp et al. 2008; Fombonne 2009; Kim et al. 2011; Baxter et al. 2015). Although the detailed abstraction of signs and symptoms from medical and educational records is laborious, our retrospective, record-based study design avoids the incomplete population screening coverage and low rates of participation in diagnostic evaluation of screen-positive cases that are potential limitations of active two-stage screening-confirmation approaches (Kim et al. 2011; Elsabbagh et al. 2012; Idring et al. 2015). Because this is an incidence study, the data are appropriate for evaluating time trends and informing etiologic research, including identification of potentially modifiable risk factors (Hennekens and Buring 1987b; Elsabbagh et al. 2012). It is difficult to interpret changes over time in ASD incidence and prevalence estimates from studies that rely on case registries or other administrative data, since increased rates would be expected in association with broadening of case definition in clinical care and/or improvements in case ascertainment. In this study, we were able to minimize the impact of changes in case-finding and clinical broadening of case definition over time by using the same multi-source case ascertainment methodology and uniformly applying the same ASD research definitions (ASD-RI and ASD-RN) to abstracted signs and symptoms throughout the study period. Clinical diagnosis rates (ASD-C), but not ASD-RI or ASD-RN, could be impacted by diagnostic substitution, which is diagnostic recategorization toward ASD and away from other diagnoses (e.g., intellectual disability or language disorder) when ASD became increasingly familiar to health care and education professionals and/or when access to better services was facilitated by having the ASD diagnosis (Elsabbagh et al. 2012; Bishop et al. 2008; Coo et al. 2008; Miller et al. 2013; Polyak et al. 2015).
Study Limitations
Several limitations of the present study also merit discussion. Because the study was designed and initiated prior to publication of DSM-5, the research definitions represent operationalized DSM-IV-TR criteria. However, this is advantageous for comparison to the vast majority of published epidemiological studies of ASD, which also used DSM-IV-TR criteria. Although fewer people meet DSM-5 ASD diagnostic criteria than DSM-IV-TR criteria, the symptom profiles of individuals who meet DSM-5 criteria and those who meet DSM-IV-TR criteria (but not DSM-5 criteria) are very similar (Beighley and Matson 2014; Beighley et al. 2013), and many studies suggest a high rate of agreement between the 2 sets of criteria (Bennett and Goodall 2016; Kim et al. 2014). For example, 81% of 6,577 8-year-old children meeting ADDM Network ASD criteria based on DSM-IV-TR also met DSM-5 criteria (Maenner et al. 2014). ASD case definition was based on retrospective record review, without direct assessment of participants by the study team to establish diagnostic validity. Loss of study individuals because of emigration before 3 years of age is a potential source of bias. Although we cannot exclude this possibility, potential migration bias was evaluated in a previous Olmsted County birth cohort study of the epidemiology of learning disabilities, and it was determined that in the context of the large number of children who remained in the community, the slight differences between migrants and non-migrants were unlikely to compromise the study findings (Katusic et al. 1998).
Due to the retrospective nature of the study, first-level screening for ASD risk was based on diagnoses and educational classifications, and it is possible that some ASD cases could have been missed because they never received any of the various medical diagnoses or educational exceptionality descriptions that were used to identify potential ASD cases. However, the likelihood of this occurring was minimized by using complementary medical and educational records and including not only autism-related diagnoses (e.g., AD, AS, and PDDNOS), but also those with substantial overlapping symptoms, such as intellectual disability, language disorders, obsessive-compulsive disorder, childhood psychoses, and ADHD, to establish the broad neurodevelopmental/psychiatric disorder (NPD) clusters in the first step of case ascertainment (Table 1). Failure to abstract meaningful ASD signs and symptoms from records could also result in missed cases. This possibility was minimized by extensive training of the research assistants who performed record abstraction and use of precisely defined, DSM-IV-TR-based operational research criteria and an extensive Data Dictionary of pertinent descriptive phrases. The record abstraction process, creation of the Data Dictionary, and training of research assistants were informed by our experience conducting previous retrospective, population-based studies on Olmsted County cohorts using educational and medical records (Katusic et al. 2001; Barbaresi et al. 2002; Barbaresi et al. 2005).
A retrospective, record-based approach also has the potential to over identify ASD cases. Abstraction from records emphasizes the accumulation of signs and symptoms of ASD, whereas the process of clinical diagnosis involves taking into consideration other factors, such as contradictory information or the situational nature of a particular symptom, when determining whether a clinical feature should count toward meeting diagnostic criteria. The potential impact of this phenomenon was minimized by certain features of the abstraction process. For example, when a symptom or sign was identified, the record was searched for additional occurrences and contradictory information and situational qualifiers were noted; when there was any question about the validity of the sign/symptom as a contributor to the ASD criterion, it was brought to the full research team for review. This is an advantage of our manual abstraction protocol relative to the use of automated algorithms to identify ASD cohorts based on text extracted from electronic health records using natural language processing systems (Lingren et al. 2016). In addition, final manual review of the consolidated summary for each subject prior to diagnostic categorization identified individuals whose abstracted ASD signs and/symptoms were clearly the result of conditions other than ASD (such as psychosis, bipolar disorder, or major depression), and these individuals were excluded as false positives (as described in Methods). Finally, the incidence of ASD-RN, which can be viewed as a lower-limit estimate of ASD incidence, is unlikely to be impacted substantially by “over calling,” since the vast majority of individuals meeting 6 or more criteria would still meet 3 or more criteria even if 1 or 2 were incorrect.
Uncertainty associated with assigning the age of onset is another limitation inherent to the retrospective nature of the study. However, establishing the age of onset is challenging with other study designs as well, since there is substantial overlap of symptoms with other developmental disabilities, especially in very young children. Although uncertainty associated with age of onset impacts estimates of annual incidence, the cumulative incidence calculations, particularly those through age 21 years, are not substantially affected. Finally, according to 2000 census data, the population of Olmsted County is more racially homogeneous (white, 90.3% vs. 75.1%), wealthier (median household income, $51,316 vs. $41,994), and more highly educated (high school graduates, 91.1% vs. 80.4%) than the general US population, which may limit generalizability of the findings (St Sauver et al. 2012a). Epidemiological findings from any single geographic population must be interpreted in the context of available data from other populations, and extrapolations and generalizations must be judged on a study-by-study basis, considering demographic variables relevant to the study question. However, results from epidemiological studies in Olmsted County have generally been consistent with national data when national data are available (St Sauver et al. 2012a).
Conclusions
Currently, the most comprehensive view of the frequency of occurrence of ASD and how it has changed over time comes from consideration of a variety of study types and the relative strengths and weaknesses of each. This retrospective, record-based study adds incidence data from a large, population-based birth cohort with active case ascertainment across a broad age range over almost 4 decades. Two different thresholds for symptom-based ASD case definition were employed to reflect the continuous distribution of autistic traits within the population and allow examination of time trends in incidence for both broadly- and narrowly-defined ASD. Although it is likely that the observed increase in the incidence of research-defined ASD is due to increased public and professional awareness and identification of ASD symptoms, we cannot exclude the possibility of a secular increase in incidence prior to 1998. However, despite widespread concern about an “epidemic” of ASD, the lack of change in the frequency of threshold ASD signs and symptoms in the late 1990s and early 2000s is not consistent with a true secular increase in ASD during that period of time.
Supplementary Material
Acknowledgements
The authors wish to acknowledge Dr. Leonard T. Kurland for his vision in initiating the Rochester Epidemiology Project and Dr. Robert C. Colligan for his insight, enthusiasm, and collegiality across his 47 years of research in developmental disabilities at the Mayo Clinic. We also thank study coordinators Ms. Candice Klein and Mr. Tom Bitz and other members of the team for data collection, Ms. Sondra Buehler for assistance in manuscript preparation, and Independent School District No. 535 for their cooperation and collaboration.
Funding: This study was funded by research grants from the National Institutes of Health, Public Health Service (MH093522 and AG034676).
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
Ethical Approval Medical research involving human subjects includes research on identifiable human material or identifiable data. All procedures performed in studies involving human subjects were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Informed consent This retrospective study of medical records data did not involve any participant contact.
References
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. VA: American Psychiatric Association. [Google Scholar]
- Atladottir HO, Gyllenberg D, Langridge A, Sandin S, Hansen SN, Leonard H, et al. (2015). The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. European Child and Adolescent Psychiatry, 24(2), 173–183. https://doi:10.1007/s00787-014-0553-8. [DOI] [PubMed] [Google Scholar]
- Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, et al. (2018). Prevalence of Autism Spectrum Disorder among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveillence Summaries, 67(6), 1–23. https://doi:10.15585/mmwr.ss6706a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JP (2013). Autism at 70--redrawing the boundaries. New England Journal of Medicine, 369(12), 1089–1091. https://doi:10.1056/NEJMp1306380. [DOI] [PubMed] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Pankratz VS, Weaver AL, Weber KJ, et al. (2002). How common is attention-deficit/hyperactivity disorder? Incidence in a population-based birth cohort in Rochester, Minn. Archives of Pediatrics and Adolescent Medicine, 156(3), 217–224. [DOI] [PubMed] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, & Jacobsen SJ (2005). The incidence of autism in Olmsted County, Minnesota, 1976–1997: results from a population-based study. Archives of Pediatrics and Adolescent Medicine, 159(1), 37–44. https://doi:10.1001/archpedi.159.1.37. [DOI] [PubMed] [Google Scholar]
- Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, & Scott JG (2015). The epidemiology and global burden of autism spectrum disorders. Psychological Medicine, 45(3), 601–613. https://doi:10.1017/S003329171400172X. [DOI] [PubMed] [Google Scholar]
- Beighley JS, & Matson JL (2014). Comparing social skills in children diagnosed with authism spectrum disorder according to the DSM-IV-TR and the DSM-5. Journal of Developmental and Physical Disabilities, 26(6), 689–701. [Google Scholar]
- Beighley JS, Matson JL, Rieske RD, Jang J, Cervantes PE, & Goldin RL (2013). Comparing challenging behavior in children diagnosed with autism spectrum disorders according to the DSM-IV-TR and the proposed DSM-5. Developmental Neurorehabilitation, 16(6), 375–381. https://doi:10.3109/17518423.2012.760119. [DOI] [PubMed] [Google Scholar]
- Bennett M, & Goodall E (2016). A meta-analysis of DSM-5 autism diagnoses in relation to DSM-IV and DSM-IV-TR. Review Journal of Autism and Developmental Disorders, 3, 119–124. [Google Scholar]
- Bent CA, Barbaro J, & Dissanayake C (2017). Change in autism diagnoses prior to and following the introduction of DSM-5. Journal of Autism and Developmental Disorders, 47(1), 163–171. https://doi:10.1007/s10803-016-2942-y. [DOI] [PubMed] [Google Scholar]
- Bishop DV, Whitehouse AJ, Watt HJ, & Line EA (2008). Autism and diagnostic substitution: evidence from a study of adults with a history of developmental language disorder. Devopmental Medicine and Child Neurology, 50(5), 341–345. https://doi:10.1111/j.1469-8749.2008.02057.x. [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Bramlett MD, Kogan MD, Schieve LA, Jones JR, & Lu MC (2013). Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011–2012. National Health Statistics Reports (65), 1–11, 11 p following 11. [PubMed] [Google Scholar]
- Brugha TS, McManus S, Bankart J, Scott F, Purdon S, Smith J, et al. (2011). Epidemiology of autism spectrum disorders in adults in the community in England. Archives of General Psychiatry, 68(5), 459–465. https://doi:10.1001/archgenpsychiatry.2011.38. [DOI] [PubMed] [Google Scholar]
- California Department of Developmental Services (2007). Autistic spectrum disorders: Changes in the California caseload, an update: June 1987 - June 2007. Sacramento, CA: California Health and Human Services Agency, Department of Developmental Services. [Google Scholar]
- Christensen DL, Baio J, Braun KV, Bilder D, Charles J, Constantino JN, et al. (2016). Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveillance Summaries, 65(No. SS-3), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Cuthbert B, Lewis-Fernandez R, Narrow WE, & Reed GM (2017). Three Approaches to Understanding and Classifying Mental Disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychological Science in the Public Interest, 18(2), 72–145. https://doi:10.1177/1529100617727266. [DOI] [PubMed] [Google Scholar]
- Constantino JN (2011). The quantitative nature of autistic social impairment. Pediatric Research, 69(5 Pt 2), 55R–62R. https://doi:10.1203/PDR.0b013e318212ec6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, & Todd RD (2003). Autistic traits in the general population: a twin study. Archives of General Psychiatry, 60(5), 524–530. https://doi:10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]
- Coo H, Ouellette-Kuntz H, Lloyd JE, Kasmara L, Holden JJ, & Lewis ME (2008). Trends in autism prevalence: diagnostic substitution revisited. Journal of Autism and Developmental Disorders, 38(6), 1036–1046. https://doi:10.1007/s10803-007-0478-x. [DOI] [PubMed] [Google Scholar]
- Davidovitch M, Hemo B, Manning-Courtney P, & Fombonne E (2013). Prevalence and incidence of autism spectrum disorder in an Israeli population. Journal of Autism and Developmental Disorders, 43(4), 785–793. https://doi:10.1007/s10803-012-1611-z. [DOI] [PubMed] [Google Scholar]
- DeVilbiss EA, & Lee BK (2014). Brief report: trends in US National autism awareness from 2004 to 2014: the impact of national autism awareness month. Journal of Autism and Developmental Disorders, 44(12), 3271–3273. https://doi:10.1007/s10803-014-2160-4. [DOI] [PubMed] [Google Scholar]
- Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcin C, et al. (2012). Global prevalence of autism and other pervasive developmental disorders. Autism Research, 5(3), 160–179. https://doi:10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fombonne E (2009). Epidemiology of pervasive developmental disorders. Pediatric Research, 65(6), 591–598. https://doi:10.1203/PDR.0b013e31819e7203. [DOI] [PubMed] [Google Scholar]
- Frost WH (1939). The age selection of mortality from tuberculosis in successive decades. American Journal of Hygiene, 30, 91–96. [DOI] [PubMed] [Google Scholar]
- Hansen SN, Schendel DE, & Parner ET (2015). Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices. JAMA Pediatrics, 169(1), 56–62. https://doi:10.1001/jamapediatrics.2014.1893. [DOI] [PubMed] [Google Scholar]
- Hennekens CH, & Buring JE (1987a). Cohort studies In Mayrent SL, (Ed.), Epidemiology of Medicine. Boston/Toronto: Little, Brown and Company. [Google Scholar]
- Hennekens CH, & Buring JE (1987b). Measures of disease frequency and association In Mayrent SL (Ed.), Epidemiology in Medicine. Boston/Toronto: Little, Brown and Company. [Google Scholar]
- Hoffman K, Weisskopf MG, Roberts AL, Raz R, Hart JE, Lyall K, et al. (2017). Geographic patterns of autism spectrum disorder among children of participants in Nurses’ Health Study II. American Journal of Epidemiology, 186(7), 834–842. https://doi:10.1093/aje/kwx158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SE (2010). The diagnosis of mental disorders: the problem of reification. Annual Review of Clinical Psychology, 6, 155–179. https://doi:10.1146/annurev.clinpsy.3.022806.091532. [DOI] [PubMed] [Google Scholar]
- Idring S, Lundberg M, Sturm H, Dalman C, Gumpert C, Rai D, et al. (2015). Changes in prevalence of autism spectrum disorders in 2001–2011: findings from the Stockholm youth cohort. Journal of Autism and Developmental Disorders, 45(6), 1766–1773. https://doi:10.1007/s10803-014-2336-y. [DOI] [PubMed] [Google Scholar]
- Isaksen J, Diseth TH, Schjolberg S, & Skjeldal OH (2012). Observed prevalence of autism spectrum disorders in two Norwegian counties. European Journal of Paediatric Neurology, 16(6), 592–598. https://doi:10.1016/j.ejpn.2012.01.014. [DOI] [PubMed] [Google Scholar]
- Isaksen J, Diseth TH, Schjolberg S, & Skjeldal OH (2013). Autism spectrum disorders--are they really epidemic? European Journal of Paediatric Neurology, 17(4), 327–333. https://doi:10.1016/j.ejpn.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Jensen CM, Steinhausen HC, & Lauritsen MB (2014). Time trends over 16 years in incidence-rates of autism spectrum disorders across the lifespan based on nationwide Danish register data. Journal of Autism and Developmental Disorders, 44(8), 1808–1818. https://doi:10.1007/s10803-014-2053-6. [DOI] [PubMed] [Google Scholar]
- Johnson CP, & Myers SM (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215. https://doi:10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- Kamio Y, Inada N, Moriwaki A, Kuroda M, Koyama T, Tsujii H, et al. (2013). Quantitative autistic traits ascertained in a national survey of 22 529 Japanese schoolchildren. Acta Psychiatrica Scandinavica, 128(1), 45–53. https://doi:10.1111/acps.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katusic SK, Colligan RC, Barbaresi WJ, Schaid DJ, & Jacobsen SJ (1998). Potential influence of migration bias in birth cohort studies. Mayo Clinic Proceedings, 73(11), 1053–1061. https://doi:10.4065/73.11.1053. [DOI] [PubMed] [Google Scholar]
- Katusic SK, Colligan RC, Barbaresi WJ, Schaid DJ, & Jacobsen SJ (2001). Incidence of reading disability in a population-based birth cohort, 1976–1982, Rochester, Minn. Mayo Clinic Proceedings, 76(11), 1081–1092. https://doi:10.4065/76.11.1081. [DOI] [PubMed] [Google Scholar]
- Katusic SK, Colligan RC, Myers SM, Voigt RG, Yoshimasu K, Stoeckel RE, et al. (2017). What can large population-based birth cohort study ask about past, present and future of children with disorders of development, learning, and behavior? Journal of Epidemiology and Community Health, 71(4), 410–416. https://doi:10.1136/jech-2016-208482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamura Y, Takahashi O, & Ishii T (2008). Reevaluating the incidence of pervasive developmental disorders: impact of elevated rates of detection through implementation of an integrated system of screening in Toyota, Japan. Psychiatry and Clinical Neurosciences, 62(2), 152–159. https://doi:10.1111/j.1440-1819.2008.01748.x. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Susser E, Cheslack-Postava K, Fountain C, Liu K, & Bearman PS (2012). Cohort effects explain the increase in autism diagnosis among children born from 1992 to 2003 in California. International Journal of Epidemiology, 41(2), 495–503. https://doi:10.1093/ije/dyr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Fombonne E, Koh YJ, Kim SJ, Cheon KA, & Leventhal BL (2014). A comparison of DSM-IV pervasive developmental disorder and DSM-5 autism spectrum disorder prevalence in an epidemiologic sample. Journal of the American Academy of Child and Adolescent Psychiatry, 53(5), 500–508. https://doi:10.1016/j.jaac.2013.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E, Lim EC, et al. (2011). Prevalence of autism spectrum disorders in a total population sample. American Journal of Psychiatry, 168(9), 904–912. https://doi:10.1176/appi.ajp.2011.10101532. [DOI] [PubMed] [Google Scholar]
- Kurland LT, Elveback LR, & Nobrega FT (1970). Population studies in Rochester and Olmsted County, Minnesota, 1900–1968 In: Kessler II,Levin MI MI. (Eds), The Community as an Epidemiologic Laboratory (pp. 47–70). Baltimore, MD: John’s Hopkins University Press. [Google Scholar]
- Liddell FD (1988). The development of cohort studies in epidemiology: a review. Journal of Clinical Epidemiology, 41(12), 1217–1237. [DOI] [PubMed] [Google Scholar]
- Lingren T, Chen P, Bochenek J, Doshi-Velez F, Manning-Courtney P, Bickel J, et al. (2016). Electronic health record based algorithm to identify patients with autism spectrum disorder. PloS One, 11(7), e0159621 https://doi:10.1371/journal.pone.0159621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu KY, King M, & Bearman PS (2010). Social influence and the autism epidemic. American Journal of Sociology, 115(5), 1387–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Petkova E, Hus V, Gan W, Lu F, Martin DM, et al. (2012). A multisite study of the clinical diagnosis of different autism spectrum disorders. Archives of General Psychiatry, 69(3), 306–313. https://doi:10.1001/archgenpsychiatry.2011.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundstrom S, Reichenberg A, Anckarsater H, Lichtenstein P, & Gillberg C (2015). Autism phenotype versus registered diagnosis in Swedish children: prevalence trends over 10 years in general population samples. BMJ, 350, h1961 https://doi:10.1136/bmj.h1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenner MJ, Rice CE, Arneson CL, Cunniff C, Schieve LA, Carpenter LA, et al. (2014). Potential impact of DSM-5 criteria on autism spectrum disorder prevalence estimates. JAMA Psychiatry, 71(3), 292–300. https://doi:10.1001/jamapsychiatry.2013.3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May T, Sciberras E, Brignell A, & Williams K (2017). Autism spectrum disorder: updated prevalence and comparison of two birth cohorts in a nationally representative Australian sample. BMJ Open, 7(5), e015549 https://doi:10.1136/bmjopen-2016-015549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazumdar S, Winter A, Liu KY, & Bearman P (2013). Spatial clusters of autism births and diagnoses point to contextual drivers of increased prevalence. Social Science and Medicine, 95, 87–96. https://doi:10.1016/j.socscimed.2012.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton LJ 3rd (1996). History of the Rochester Epidemiology Project. Mayo Clinic Proceedings, 71(3), 266–274. https://doi:10.1016/S0025-6196(11)63966-9. [DOI] [PubMed] [Google Scholar]
- Miller JS, Bilder D, Farley M, Coon H, Pinborough-Zimmerman J, Jenson W, et al. (2013). Autism spectrum disorder reclassified: a second look at the 1980s Utah/UCLA Autism Epidemiologic Study. Journal of Autism and Developmental Disorders, 43(1), 200–210. https://doi:10.1007/s10803-012-1566-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Møller J, Syversveen AR, & Waagepetersen RP (1998). Log Gaussian Cox processes. Scandinavian Journal of Statistics, Theory and Applications, 25(3), 451–482. [Google Scholar]
- Myers SM, & Johnson CP (2007). Management of children with autism spectrum disorders. Pediatrics, 120(5), 1162–1182. https://doi:10.1542/peds.2007-2362. [DOI] [PubMed] [Google Scholar]
- Nassar N, Dixon G, Bourke J, Bower C, Glasson E, de Klerk N, et al. (2009). Autism spectrum disorders in young children: effect of changes in diagnostic practices. International Journal of Epidemiology, 38(5), 1245–1254. https://doi:10.1093/ije/dyp260. [DOI] [PubMed] [Google Scholar]
- Newschaffer CJ, Falb MD, & Gurney JG (2005). National autism prevalence trends from United States special education data. Pediatrics, 115(3), e277–282. https://doi:10.1542/peds.2004-1958. [DOI] [PubMed] [Google Scholar]
- Office of Autism Research Coordination (OARC) National Institute of Mental Health and Thomson Reuters, Inc., on behalf of the Interagency Autism Coordinating Committee (IACC). IACC/OARC Autism Spectrum Disorder Research Publications Analysis Report: The Global Landscape of Autism Research, July 2012. Retrieved from the Department of Health and Human Services Interagency Autism Coordinating Committee website: http://iacc.hhs.gov/publiations-analysis/july2012/index.shtml on September 19, 2018.
- Palmer N, Beam A, Agniel D, Eran A, Manrai A, Spettell C, et al. (2017). Association of sex with recurrence of autism spectrum disorder among siblings. JAMA Pediatrics, 171(11), 1107–1112. https://doi:10.1001/jamapediatrics.2017.2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park HY, Harwood RL, Yu SM, Kavanagh L, & Lu MC (2016). Autism and other developmental disabilities research programs of the Maternal and Child Health Bureau. Pediatrics, 137 Suppl 2, S61–66. https://doi:10.1542/peds.2015-2851C. [DOI] [PubMed] [Google Scholar]
- Pearce N (2012). Classification of epidemiological study designs. International Journal of Epidemiology, 41(2), 393–397. https://doi:10.1093/ije/dys049. [DOI] [PubMed] [Google Scholar]
- Polyak A, Kubina RM, & Girirajan S (2015). Comorbidity of intellectual disability confounds ascertainment of autism: implications for genetic diagnosis. American Journal of Medical Genetics. Part B: Neuropsychiatric Genetics, 168(7), 600–608. https://doi:10.1002/ajmg.b.32338. [DOI] [PubMed] [Google Scholar]
- Posserud MB, Lundervold AJ, & Gillberg C (2006). Autistic features in a total population of 7–9-year-old children assessed by the ASSQ (Autism Spectrum Screening Questionnaire). Journal of Child Psychology and Psychiatry and Allied Disciplines, 47(2), 167–175. https://doi:10.1111/j.1469-7610.2005.01462.x. [DOI] [PubMed] [Google Scholar]
- R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- Raz R, Weisskopf MG, Davidovitch M, Pinto O, & Levine H (2015). Differences in autism spectrum disorders incidence by sub-populations in Israel 1992–2009: a total population study. Journal of Autism and Developmental Disorders, 45(4), 1062–1069. https://doi:10.1007/s10803-014-2262-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich BJ, Storlie CB, & Bondell HD (2009). Variable selection in Bayesian smoothing spline ANOVA models: Application to deterministic computer codes. Technometrics, 51(2), 110–120. https://doi:10.1198/TECH.2009.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Rosanoff M, Dawson G, Durkin MS, Croen LA, Singer A, et al. (2012). Evaluating changes in the prevalence of the Autism Spectrum Disorders (ASDs). Public Health Reviews, 34(2), 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, & Melton LJ 3rd (2012). History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clinic Proceedings, 87(12), 1202–1213. https://doi:10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saemundsen E, Magnusson P, Georgsdottir I, Egilsson E, & Rafnsson V (2013). Prevalence of autism spectrum disorders in an Icelandic birth cohort. BMJ Open, 3(6), 1–6. https://doi:10.1136/bmjopen-2013-002748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieve LA, Rice C, Yeargin-Allsopp M, Boyle CA, Kogan MD, Drews C, et al. (2012). Parent-reported prevalence of autism spectrum disorders in US-born children: an assessment of changes within birth cohorts from the 2003 to the 2007 National Survey of Children’s Health. Maternal and Child Health Journal, 16 Suppl 1, S151–157. https://doi:10.1007/s10995-012-1004-0. [DOI] [PubMed] [Google Scholar]
- Smith IC, Reichow B, & Volkmar FR (2015). The effects of DSM-5 criteria on number of individuals diagnosed with autism spectrum disorder: a systematic review. Journal of Autism and Developmental Disorders, 45(8), 2541–2552. https://doi:10.1007/s10803-015-2423-8. [DOI] [PubMed] [Google Scholar]
- St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, & Rocca WA (2012a). Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clinic Proceedings, 87(2), 151–160. https://doi:10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Pankratz JJ, Brue SM, et al. (2012b). Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. International Journal of Epidemiology, 41(6), 1614–1624. https://doi:10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, & Rocca WA (2011). Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. American Journal of Epidemiology, 173(9), 1059–1068. https://doi:10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storlie CB, Reich BJ, Helton JC, Swiler LP, & Sallaberry CJ (2013). Analysis of computationally demanding models with continuous and categorical inputs. Reliability Engineering System Safety, 113(30–41). [Google Scholar]
- Taylor B, Jick H, & Maclaughlin D (2013). Prevalence and incidence rates of autism in the UK: time trend from 2004–2010 in children aged 8 years. BMJ Open, 3(10), e003219 https://doi:10.1136/bmjopen-2013-003219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehouse AJ, Cooper MN, Bebbington K, Alvares G, Lin A, Wray J, et al. (2017). Evidence of a reduction over time in the behavioral severity of autistic disorder diagnoses. Autism Research, 10(1), 179–187. https://doi:10.1002/aur.1740. [DOI] [PubMed] [Google Scholar]
- Wing L, & Potter D (2002). The epidemiology of autistic spectrum disorders: is the prevalence rising? Mental Retardation and Developmental Disabilities Research Reviews, 8(3), 151–161. https://doi:10.1002/mrdd.10029. [DOI] [PubMed] [Google Scholar]
- Xu G, Strathearn L, Liu B, & Bao W (2018). Prevalence of Autism Spectrum Disorder among US children and adolescents, 2014–2016. JAMA, 319(1), 81–82. https://doi:10.1001/jama.2017.17812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeargin-Allsopp M, Boyle C, van Naarden-Braun K, & Trevathan E (2008). The epidemiology of developmental disabilities In Accardo PJ (Ed.), Capute & Accardo’s Neurodevelopmental Disabilities in Infancy and Childhood, Third Edition: Volume I: Neurodevelopmental Diagnosis and Treatment (pp. 61–104). Baltimore, MD: Paul H. Brookes Publishing Co. [Google Scholar]
- Zablotsky B, Black LI, Maenner MJ, Schieve LA, & Blumberg SJ (2015). Estimated prevalence of autism and other developmental disabilities following questionnaire changes in the 2014 National Health Interview Survey. National Health Statistics Report (87), 1–20. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.