Abstract
Overweight and obese mothers in the United States have disproportionately lower rates of exclusive breastfeeding than mothers of normal weight. The Ten Steps to Successful Breastfeeding (Ten Steps), a series of evidence‐based practices designed to support breastfeeding initiation, duration, and exclusivity, demonstrate effectiveness at the population level. It is unknown, however, whether they are consistently provided to women across all maternal body mass index (BMI) categories. We sought to determine whether pre‐pregnancy BMI is associated with the implementation and effectiveness of the Ten Steps. We used data from Listening to Mothers III, a cross‐sectional survey administered to a sample of mothers who delivered in U.S. hospitals between July 2011 and June 2012. Measures of the Ten Steps were based on maternal self‐report on Listening to Mothers III. Our analytic sample was limited to mothers of term infants intending to breastfeed (N = 1,506, weighted). We conducted chi‐square testing and constructed weighted multivariable logistic regression models to account for potential confounders. Results suggest that two practices (i.e., holding their babies skin‐to‐skin for the first time and being encouraged to breastfeed on demand) were more strongly associated with exclusive breastfeeding among mothers with obesity than other mothers. Additionally, mothers with obesity reported holding babies skin‐to‐skin significantly less often than other mothers. Thus, interventions aimed at helping mothers with obesity to hold their babies skin‐to‐skin in the first hour and teaching them to breastfeed on demand have the potential to decrease the breastfeeding disparities in this population.
Keywords: baby friendly hospital initiative, breastfeeding, breastfeeding duration, breastfeeding promotion, breastfeeding support, maternal obesity
Key messages.
High hospital breastfeeding support is associated with improved exclusive breastfeeding duration among mothers of all body mass index categories.
Early skin‐to‐skin is less prevalent among obese mothers than overweight and normal‐weight mothers, yet this practice had the highest association with exclusive breastfeeding at 1 week among obese mothers.
Efforts to improve exclusive breastfeeding among obese mothers may benefit from focusing on early skin‐to‐skin feeding and education about feeding on demand.
1. INTRODUCTION
Exclusive breastfeeding for the first 6 months is important for optimal health of both infants and mothers (American Academy of Pediatrics, 2012). Mothers who are overweight or obese have lower rates of breastfeeding initiation and have shorter average duration of both any and exclusive breastfeeding than mothers who are of normal weight (Amir & Donath, 2007; Oddy et al., 2006; O'Sullivan, Perrine, & Rasmussen, 2015; Turcksin, Bel, Galjaard, & Devlieger, 2014; Wojcicki, 2011). Reasons for this disparity are multifactorial and include anatomic, physiologic, and psychosocial factors (Nommsen‐Rivers, Chantry, Peerson, Cohen, & Dewey, 2010; Rasmussen, Hilson, & Kjolhede, 2001, 2002; Rasmussen & Kjolhede, 2004). Larger breast size, more prevalent among women with elevated body mass index (BMI), can lead to logistic challenges getting a baby to latch (Amir & Donath, 2007). Additionally, previous studies have demonstrated both an increased risk of delayed lactogenesis and a diminished prolactin response to infant suckling among overweight and obese mothers (Nommsen‐Rivers et al., 2010; Rasmussen et al., 2001). Furthermore, the stigmatization of obesity in maternity and post‐partum care settings has been shown to be associated with decreased utilization of health care and increased stress among obese women and may adversely affect early lactation support for this population (Garner, Ratcliff, Devine, Thornburg, & Rasmussen, 2014; Lindhart, Rubak, Mogensen, Lamont, & Joergensen, 2013; Puhl & Heuer, 2010).
The Ten Steps to Successful Breastfeeding (Ten Steps) are a bundle of maternity practices shown to support breastfeeding initiation and exclusivity and prolong duration that have been endorsed by numerous health and professional organizations such as the World Health Organization (WHO), American Academy of Pediatrics, and the Academy of Breastfeeding Medicine (Chantry, Eglash, & Labbok, 2015; Kramer et al., 2001; Nickel, Labbok, Hudgens, & Daniels, 2013; American Academy of Pediatrics; WHO, 1998). Despite this evidence, it is unclear whether the Ten Steps effectively reduce breastfeeding inequities. Differential or inconsistent implementation of these practices across maternal BMI categories could exacerbate breastfeeding disparities (Yang, Platt, Dahhou, & Kramer, 2014). Given that overweight and obese mothers experience additional breastfeeding challenges, if they also do not receive the care outlined in the Ten Steps, then disparities could widen. One study using Centers for Disease Control and Prevention (CDC) Pregnancy Risk Assessment Monitoring System data from three states in the United States found the Ten Steps to be differentially implemented across mothers of varying prepregnancy BMI (Kair & Colaizy, 2016); however, this has not been confirmed in other settings.
Additionally, it is unknown whether these practices are equally effective in promoting exclusive breastfeeding across maternal BMI categories. Differential effects of the Ten Steps have been previously reported by maternal age and maternal depression status (Sipsma, Jones, & Nickel, 2017; Sipsma, Kornfeind, & Kair, 2017) but to our knowledge have not been explored by maternal BMI category. Given that more than half of pregnant women in the United States are overweight or obese, it is of significant public health importance to know the effectiveness of the Ten Steps in promoting exclusive breastfeeding in this population (Deputy, Dub, & Sharma, 2018).
We sought to determine the extent to which prepregnancy BMI is associated with the implementation and effectiveness of hospital practices to promote breastfeeding using precollected survey data, a national sample of mothers across the United States. We hypothesized that overweight and obese mothers would have decreased exposure to many of the Ten Steps and that exposure to these practices would be associated with improved odds of exclusive breastfeeding at 1 week and 3 months.
2. METHODS
The Institutional Review Boards at University California Davis and Benedictine University determined this study was exempted from review, as data were de‐identified and publicly available.
2.1. Study population
We used self‐reported data from Listening to Mothers III (LTMIII), a cross‐sectional survey administered online to a sample of mothers of singleton births occurring in U.S. hospitals between July 2011 and June 2012. Mothers were between 3 and 18 months post‐partum at the time of the survey. LTMIII data are publicly available online and include survey responses from 2,400 women who are 18–45 years of age, delivered a singleton infant who was still alive at the time of the survey, and were able to complete the survey in English. We limited our analytic sample to mothers who delivered healthy babies at 37 weeks of gestation or later and who reported planning to breastfeed either exclusively or in combination with formula. We excluded babies who received care in the neonatal intensive care unit, as we expected these maternal–infant dyads to have greater challenges breastfeeding. The total sample size was 1,598 (Figure 1; 1,506 mothers, weighted).
Figure 1.
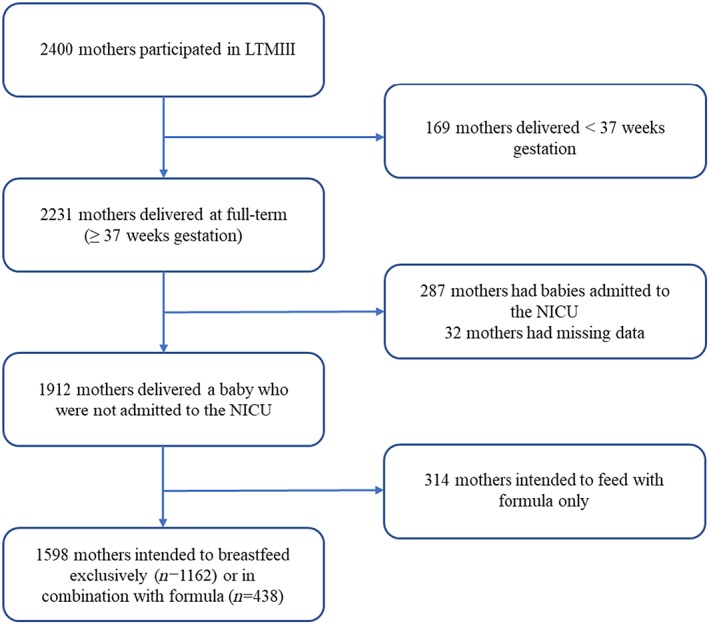
Flow diagram of participant inclusion. LTMIII: Listening to Mothers III
2.2. Measures
Measures for hospital practices were based upon Steps 4 through 10 of the Ten Steps to Successful Breastfeeding from the WHO (1998, 2018). Steps 1–3 are not applicable to individual‐level post‐partum care and were not measured in the LTM III. Maternal BMI categories were classified by their self‐reported prepregnancy BMI according to the CDC definitions: normal 18.5–24.9, overweight 25–29.9, and obese ≥30 (CDC, 2017). Mothers were considered to be exclusively breastfeeding at 1 week if mothers indicated that they were feeding their baby breast milk only at 1 week. If women indicated that they were feeding their baby breast milk only at the time of the survey, they were considered to have been exclusively breastfeeding at 3 months. If they were not exclusively breastfeeding at the time of the survey, they were asked how long they fed their child breast milk only. They selected possible options (e.g., 1 and 2 months) and were considered to have been exclusively breastfeeding at 3 months if the reported duration was 3 months or longer.
We considered several variables to control for potential confounding (Goyal, Attandasio, & Kozhimannil, 2014; Sipsma, Jones, & Nickel, 2017) including maternal age at the time of the interview (≤19, 20–24, 25–29, 30–34, or ≥35 years), race/ethnicity (non‐Hispanic White, non‐Hispanic Black, Hispanic, or Other), education (high school or less, some college, or college graduate or higher), use of Medicaid (yes or no), marital status (married or not), exclusive breastfeeding intention at the end of pregnancy (breastfeeding only or in combination with formula), parity (first baby or not), and mode of delivery (vaginal or Caesarean section).
2.3. Analysis
We used frequencies to describe the analytic sample, reported exposure to hospital practices, and breastfeeding behaviours. We then conducted chi‐square testing to examine whether or not exclusive breastfeeding and reported exposure to practices differed by maternal BMI categories. Last, we used a series of multivariable logistic regression models to determine whether or not the effect of reported exposure to practices on exclusive breastfeeding varied by BMI categories. Models used exclusive breastfeeding (at 1 week and 3 months) as the outcome and the hospital practices as the exposure variables of interest and included the potential confounders to isolate the independent effect between the practices and our breastfeeding outcomes. We also included interaction terms between dummy variables used to represent maternal BMI categories and the hospital practices. We tested the inclusion of each set of interaction terms in individual models. In our results, we describe the simple effects for each maternal BMI category. The prevalence of missing data was low (<5%), and thus, we used a complete case analysis. We used IBM SPSS Statistics version 24 and incorporated the weighting variables as recommended by the LTM III.
3. RESULTS
Characteristics of respondent mothers are shown in Table 1. Exclusive breastfeeding at 1 week and at 3 months varied significantly across maternal prepregnancy BMI categories, as shown in Table 2.
Table 1.
Sociodemographic characteristics of mothers included in our analytic sample from Listening to Mothers III (n = 1,506, weighted)a
| Characteristic | n (%) |
|---|---|
| Maternal age, years | |
| ≤19 | 84 (5.6) |
| 20–24 | 343 (22.8) |
| 25–29 | 432 (28.7) |
| 30–34 | 411 (27.3) |
| ≥35 | 236 (15.7) |
| Maternal education, years | |
| High school or less | 555 (36.9) |
| Some college | 465 (30.9) |
| College graduate or higher | 486 (32.3) |
| Maternal race/ethnicityb | |
| Non‐Hispanic White | 858 (57.4) |
| Non‐Hispanic Black | 206 (13.8) |
| Hispanic | 339 (22.7) |
| Other | 92 (6.2) |
| Married | 967 (64.2) |
| Primary insurancec | |
| Medicaid or CHIP | 519 (35.1) |
| Private | 765 (51.8) |
| Other government | 135 (9.1) |
| Self‐pay | 58 (3.9) |
| Primiparous | 588 (39.0) |
| Vaginal delivery | 1,084 (71.9) |
| Maternal prepregnancy BMI | |
| Underweight/normal | 854 (56.7) |
| Overweight | 378 (25.1) |
| Obese | 274 (18.2) |
| Breastfeeding intention | |
| Exclusively | 1,026 (68.1) |
| In combination with formula | 481 (31.9) |
| Exclusive breastfeeding | |
| 1 week | 955 (63.4) |
| 3 months | 798 (53.0) |
Note. BMI: body mass index.
Our analytic sample included mothers who delivered a healthy baby at term or later and who reported planning to breastfeed exclusively or in combination with formula.
Missing 11 (0.7%) responses.
Missing 30 (2.0%) responses.
Table 2.
Breastfeeding outcomes by prepregnancy BMI status
| Overall | Prepregnancy BMI category N (%) | |||||
|---|---|---|---|---|---|---|
| Description | n (%) |
Normal/underweight (n = 854; 56.7%) |
Overweight (n = 378; 25.1%) | Obese (n = 274; 18.2%) | Chi square | P value |
| Exclusive breastfeeding at 1 week | 955 (63.4) | 563 (66.0) | 236 (62.4) | 156 (56.7) | 7.92 | 0.019 |
| Exclusive breastfeeding at 3 months | 798 (53.0) | 482 (56.5) | 194 (51.3) | 121 (44.2) | 13.23 | 0.001 |
Note. BMI: body mass index.
Table 3 presents exposure to each of the Ten Steps, as reported by participants, stratified by maternal prepregnancy BMI category. Some of the Ten Steps were differentially reported by mothers across BMI categories. Obese mothers had the lowest prevalence of reporting holding their babies skin‐to‐skin the first time and being shown how to get started breastfeeding when they were ready (Step 4; 43% vs. 48% and 60% for normal/underweight and overweight mothers, respectively). Additionally, approximately 70% of obese mothers and 71% of overweight mothers reported being shown how to position their babies to reduce nipple soreness; only 62% of normal/underweight mothers reported being shown this positioning. Additionally, approximately 80% of obese mothers reported being encouraged to feed on demand; only 70% of overweight mothers and 67% of normal/underweight mothers reported the same encouragement.
Table 3.
Hospital practices used to promote breastfeeding by prepregnancy BMI statusa
| Overall | Prepregnancy BMI category n (%) | |||||
|---|---|---|---|---|---|---|
| Step | Description | n (%) | Normal/underweight | Overweight | Obese | P valuea |
| 4 | Nurses and other staff at the hospital helped you get started breastfeeding when you and your baby were ready AND the first time you held your baby you were skin‐to‐skin. | 756 (50.2) | 410 (48.1) | 227 (59.9) | 119 (43.4) | <0.001 |
| 5 | Nurses and other staff at the hospital showed you how to position your baby to limit nipple soreness. | 985 (65.4) | 525 (61.5) | 267 (70.6) | 193 (70.2) | 0.001 |
| 6 | Nurses and other staff at the hospital NEITHER provided formula or water to supplement your breast milk NOR gave you any free formula samples, coupons, or other offers. | 591 (39.2) | 347 (40.6) | 150 (39.7) | 94 (34.2) | 0.159 |
| 7 | After that first hour after your baby's birth while in the hospital, your baby stayed with you all the time (sometimes known as “rooming‐in”). | 1,028 (68.3) | 573 (67.2) | 262 (69.1) | 193 (70.4) | 0.550 |
| 8 | Nurses and other staff at the hospital encouraged you to feed whenever your baby was interested (on demand). | 1,051 (69.8) | 569 (66.6) | 263 (69.6) | 219 (79.9) | <0.001 |
| 9 | Nurses and other staff at the hospital did NOT give your baby a pacifier. | 918 (60.9) | 521 (61.1) | 231 (61.1) | 166 (60.4) | 0.975 |
| 10 | Nurses and other staff at the hospital told you about breastfeeding support resources in the community. | 792 (52.6) | 441 (51.6) | 195 (51.5) | 157 (57.1) | 0.254 |
| — | High breastfeeding support (6 or 7/7 steps) | 274 (18.3) | 152 (17.9) | 81 (21.5) | 42 (15.3) | 0.119 |
Steps 1–3 are excluded from the analysis as they concern hospitals implementing an institutional‐level policy, training staff, and providing prenatal education.
P values derived from chi‐square testing.
Other practices were reported to have been received consistently across maternal BMI categories. Overall, high breastfeeding support was reported by 18% of mothers who were underweight and of normal weight, 22% of mothers who were overweight, and 15% of obese mothers; differences across groups were not statistically significant (P > 0.05).
Table 4 shows the associations between reported exposure to each practice and exclusive breastfeeding, stratified by maternal prepregnancy BMI category. Overweight and obese mothers benefitted more than mothers of normal weight from early skin‐to‐skin (Step 4). Mothers with obesity had three times greater odds of exclusively breastfeeding at 1 week if they reported exposure to early skin‐to‐skin compared with not receiving this practice (OR = 3.18; 95% CI = 1.73, 5.85), but this exposure was not associated with exclusive breastfeeding among mothers of normal weight (OR = 1.07; 95% CI = 0.76, 1.51). Similarly, mothers who were overweight had almost two times greater odds of exclusively breastfeeding at 3 months if they reported exposure to early skin‐to‐skin compared with if they did not report this exposure (OR = 1.86; 95% CI = 1.12, 3.09); no association was found among mothers of normal weight at 3 months (OR = 0.87; 95% CI = 0.62, 1.21).
Table 4.
Multivariable logistic regression models examining the extent to which the association between practices and exclusive breastfeeding are modified by BMI status
| Practice (predictor) | Outcome | OR [95% CI] | ||
|---|---|---|---|---|
| Normal/underweight | Overweight | Obese | ||
| Model 1 | ||||
| Nurses and other staff at the hospital helped you get started breastfeeding when you and your baby were ready AND the first time you held your baby you were skin‐to‐skin. | EBF at 1 weeka | 1.07 [0.76, 1.51] | 1.62 [0.97, 2.71] | 3.18 [1.73, 5.85]** |
| EBF at 3 monthsb | 0.87 [0.62, 1.21] | 1.86 [1.12, 3.09]* | 1.66 [0.94, 2.94] | |
| Nurses and other staff at the hospital showed you how to position your baby to limit nipple soreness. | EBF at 1 week | 1.30 [0.90, 1.89] | 0.78 [0.43, 1.40] | 0.94 [0.50, 1.78] |
| EBF at 3 months | 1.00 [0.70, 1.43] | 0.71 [0.40, 1.25] | 1.26 [0.67, 2.36] | |
| Nurses and other staff at the hospital NEITHER provided formula or water to supplement your breast milk NOR gave you any free formula samples, coupons, or other offers. | EBF at 1 week | 2.44 [1.67, 3.55]** | 3.03 [1.75, 5.27]** | 1.71 [0.92, 3.20] |
| EBF at 3 months | 2.02 [1.44, 2.85]** | 1.51 [0.91, 2.50] | 1.97 [1.08, 3.60]* | |
| After that first hour after your baby's birth while in the hospital, your baby stayed with you all the time (sometimes known as “rooming‐in”). | EBF at 1 week | 1.74 [1.22, 2.50]** | 1.15 [0.67, 1.96] | 1.08 [0.58, 2.00] |
| EBF at 3 months | 1.32 [0.93, 1.86] | 1.58 [0.93, 2.68] | 1.01 [0.54, 1.90] | |
| Nurses and other staff at the hospital encouraged you to feed whenever your baby was interested (on demand). | EBF at 1 week | 1.16 [0.80, 1.69] | 1.00 [0.57, 1.77] | 2.32 [1.09, 4.56]* |
| EBF at 3 months | 1.08 [0.75, 1.56] | 0.69 [0.39, 1.20] | 2.29 [1.10, 4.78]* | |
| Nurses and other staff at the hospital did NOT give your baby a pacifier. | EBF at 1 week | 0.93 [0.65, 1.33] | 1.26 [0.75, 2.13] | 1.05 [0.58, 1.89] |
| EBF at 3 months | 1.21 [0.86, 1.70] | 1.63 [0.98, 2.71] | 0.75 [0.42, 1.33] | |
| Nurses and other staff at the hospital told you about breastfeeding support resources in the community. | EBF at 1 weeka , b | 1.61 [1.12, 2.32]** | 0.85 [0.50, 1.43] | 0.76 [0.42, 1.38] |
| EBF at 3 months | 1.32 [0.94, 1.86] | 0.74 [0.45, 1.23] | 1.00 [0.56, 1.77] | |
| Model 2 | ||||
| High breastfeeding support (≥6 of 7 steps) | EBF at 1 week | 2.54 [1.50, 4.30]** | 1.87 [0.95, 3.67] | 3.01 [1.18, 7.70]* |
| EBF at 3 months | 1.40 [0.91, 2.15] | 1.00 [0.56, 1.79] | 1.61 [0.77, 3.38] | |
Note. Models control for maternal age, race/ethnicity, insurance status, education, marital status, parity (first baby), and delivery mode. BMI: body mass index.
P value <0.05.
P value ≤0.01.
Estimates among mothers of normal weight or who are underweight are significantly different (P values <0.05) than estimates among mothers with obesity (in cases where at least one estimate is statistically significant).
Estimates among mothers of normal weight or who are underweight are significantly different (P values <0.05) than estimates among mothers who are overweight (in cases where at least one estimate is statistically significant).
Furthermore, although being encouraged to feed on demand was significantly associated with exclusive breastfeeding at 1 week and 3 months among obese mothers (OR = 2.32; 95% CI = 1.09, 4.56 and OR = 2.29; 95% CI = 1.10, 4.78, respectively), it was not associated with exclusive breastfeeding among mothers of normal weight (OR = 1.16; 95% CI = 0.80, 1.69 and OR = 1.08; 95% CI = 0.75, 1.56, respectively) or among mothers who were overweight (OR = 1.00; 95% CI = 0.57, 1.77 and OR = 0.69; 95% CI = 0.39, 1.20, respectively).
Being told about breastfeeding resources in the community (Step 10) appeared to benefit mothers of normal weight more than mothers who were overweight or mothers with obesity. Exposure to this practice was positively associated with exclusively breastfeeding among mothers of normal weight at 1 week (OR = 1.61; 95% CI = 1.12, 2.32), but there was no statistically significant relationship among overweight mothers (OR = 0.85; 95% CI = 0.50, 1.43) or among obese mothers (OR = 0.76; 95% CI = 0.42, 1.38). Similarly, rooming‐in with baby was statistically significantly associated with exclusive breastfeeding among normal‐weight mothers at 1 week (OR = 1.74; 95% CI = 1.22, 2.50) but this practice was not significant among overweight mothers (OR = 1.15; 95% CI = 0.67, 1.96) or among obese mothers (OR = 1.08; 95% CI = 0.58, 2.00).
Being shown how to position the baby for feeding and refraining from pacifier distribution were not statistically significantly associated with breastfeeding outcomes in any maternal BMI category, and refraining from the distribution of formula or related offers was statistically significantly associated with breastfeeding outcomes across all BMI categories. High breastfeeding support was associated with exclusive breastfeeding at 1 week among mothers who were underweight or normal weight (OR = 2.54; 95% CI = 1.50, 4.30) and among obese mothers (OR = 3.01; 95% CI = 1.18, 7.70). High breastfeeding support was not significantly associated with breastfeeding at 1 week among mothers who were overweight (OR = 1.87; 95% CI = 0.95, 3.67).
4. DISCUSSION
We found that the Ten Steps were associated with improved breastfeeding outcomes across all BMI categories. Interestingly, we found that Steps 4 (early breastfeeding help and skin‐to‐skin) and 8 (feeding on demand) were most beneficial for obese mothers. Of note, although the relationship among obese mothers was strongest for Step 4, this practice was also experienced significantly less frequently among these mothers. Finally, we found that high hospital breastfeeding support was generally helpful for mothers in this study regardless of prepregnancy BMI category, with the strongest positive association seen among obese mothers. Fewer than one fifth of the mothers surveyed in this study received that level of support, with the lowest prevalence reported among obese mothers.
Although increasing overall hospital breastfeeding support practices is likely to improve breastfeeding rates, certain practices appear to be more highly associated with improved exclusive breastfeeding among obese mothers, thus highlighting areas for interventions aimed at improving breastfeeding among obese mothers. Obese mothers have significantly higher odds of delivering by Caesarean section than mothers of normal weight, and those who do deliver vaginally have higher risk of difficult deliveries and complications such as birth asphyxia and shoulder dystocia (Ramoniene et al., 2017; Zhang et al., 2010). As a result, obese mothers may be at increased risk of missing early skin‐to‐skin feeding opportunities. The results of this study highlight the importance of overcoming these barriers in order to reduce breastfeeding disparities among obese mothers. Likewise, nurses and other hospital staff teaching breastfeeding on demand was very highly associated with exclusive breastfeeding at 1 week and 3 months among obese mothers and presents another area for focused breastfeeding promotion interventions.
We also note that although restricting pacifier distribution in the hospital is a relatively simple intervention, lack of exposure to a pacifier was not associated with improved exclusive breastfeeding at 1 week or 3 months among mothers in this study, contrary to the results of multiple prior observational studies (Karabulut, Yalcin, Ozdemir‐Geyik, & Karaagaoglu, 2009; Nickel et al., 2013). One prior study examined the effect of a hospital policy restricting access to pacifiers on in‐hospital exclusive breastfeeding rates and found higher rates of formula supplementation following implementation of the pacifier restriction policy (Kair, Kenron, Etheredge, Jaffe, & Phillipi, 2013). Our findings demonstrate trends in opposite directions for obese mothers compared with normal‐weight and overweight mothers. Pacifiers may be a tool for exclusively breastfeeding, obese mothers to keep their babies calm during the first few days, prior to lactogenesis II, the onset of which is delayed in obese mothers (Nommsen‐Rivers et al., 2010). Prospective research powered to examine the effect of early pacifier use on exclusive breastfeeding duration among infants born to obese mothers would be helpful to test this hypothesis.
Limitations of this study should also be considered. Data were collected retrospectively at 4 or more months post‐partum, thus allowing the potential for recall bias. Furthermore, hospital practices, breastfeeding, and BMI were all self‐reported and are subject to social‐desirability bias. The data were also collected in 2011–2012, and practices may have changed since then. Additionally, 53% of mothers in the study sample reported exclusively breastfeeding at 3 months, an estimate that differs from CDC data that show 40.7% of babies breastfed exclusively in the United States at 3 months in 2011. This difference may indicate social desirability bias or differences in the LTMIII sample populations compared with mothers in the United States overall (CDC, 2014). Our findings therefore highlight potential areas for future investigation with a prospective design that can account for some of these limitations.
5. CONCLUSIONS
Given the rise in obesity prevalence among pregnant women in the United States, a focus on improving breastfeeding rates among obese mothers is prudent. High hospital breastfeeding support is positively associated with exclusive breastfeeding at 1 week and at 3 months among mothers of all BMI categories. Efforts to decrease breastfeeding disparities among obese mothers should focus on improving early breastfeeding help and skin‐to‐skin contact between mother and baby and teaching breastfeeding on demand.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
LRK conceptualized the study, assisted with design of the analyses and interpretation of results, drafted the initial manuscript, and approves the final version to be published. NCN assisted with design of the analyses and interpretation of results, edited the manuscript, and approves the final version to be published. KJ assisted with study design and interpretation of results, edited the manuscript, and approves the final version to be published. KK assisted with data analysis and interpretation of results, edited the manuscript, and approves the final version to be published. HLS designed the study, performed the analyses, edited the manuscript, and approves the final version to be published.
ACKNOWLEDGEMENTS
The authors would like to thank participating mothers who provided their data for the Listening Mothers III survey as well as the LTMIII investigators and funders.
Kair LR, Nickel NC, Jones K, Kornfeind K, Sipsma HL. Hospital breastfeeding support and exclusive breastfeeding by maternal prepregnancy body mass index. Matern Child Nutr. 2019;15:e12783 10.1111/mcn.12783
REFERENCES
- American Academy of Pediatrics . (2012). Breastfeeding and the use of human milk. Paediatrics, 129(3), e827–e841. 10.1542/peds.2011-3552 [DOI] [PubMed] [Google Scholar]
- Amir, L. H. , & Donath, S. (2007). A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy and Childbirth, 7, 9 10.1186/1471-2393-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2014). Retrieved from https://www.cdc.gov/breastfeeding/pdf/2014breastfeedingreportcard.pdf
- Centers for Disease Control and Prevention . (2017). Healthy weight. Retrieved from https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
- Chantry, C. J. , Eglash, A. , & Labbok, M. (2015). ABM position on breastfeeding‐revised 2015. Breastfeeding Medicine, 10(9), 407–411. 10.1089/bfm.2015.29012.cha [DOI] [PubMed] [Google Scholar]
- Deputy, N. P. , Dub, B. , & Sharma, A. J. (2018). Prevalence and trends in prepregnancy normal weight—48 States, New York City, and District of Columbia, 2011‐2015. MMWR. Morbidity and Mortality Weekly Report, 66(5152), 1402–1407. 10.15585/mmwr.mm665152a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner, C. D. , Ratcliff, S. L. , Devine, C. M. , Thornburg, L. L. , & Rasmussen, K. M. (2014). Health professionals' experiences providing breastfeeding‐related care for obese women. Breastfeeding Medicine, 9(10), 503–509. 10.1089/bfm.2014.0104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal, N. , Attandasio, L. , & Kozhimannil, K. (2014). Hospital care and early breastfeeding outcomes among late preterm, early‐term, and term infants. Birth, 41(4), 330–338. 10.1111/birt.12135 [DOI] [PubMed] [Google Scholar]
- Kair, L. R. , & Colaizy, T. T. (2016). Obese mothers have lower odds of experiencing pro‐breastfeeding hospital practices than mothers of normal weight: CDC Pregnancy Risk Assessment Monitoring System (PRAMS), 2004‐2008. Maternal and Child Health Journal, 20(3), 593–601. 10.1007/s10995-015-1858-z [DOI] [PubMed] [Google Scholar]
- Kair, L. R. , Kenron, D. , Etheredge, K. , Jaffe, A. C. , & Phillipi, C. A. (2013). Pacifier restriction and exclusive breastfeeding. Paediatrics, 131(4), e1101–e1107. 10.1542/peds.2012-2203 [DOI] [PubMed] [Google Scholar]
- Karabulut, E. , Yalcin, S. S. , Ozdemir‐Geyik, P. , & Karaagaoglu, E. (2009). Effect of pacifier use on exclusive and any breastfeeding: A meta‐analysis. The Turkish Journal of Pediatrics, 51(1), 35–43. [PubMed] [Google Scholar]
- Kramer, M. S. , Chalmers, B. , Hodnett, E. D. , Sevkovskaya, Z. , Dzikovich, I. , Shapiro, S. , … Group, P. S . (2001). Promotion of Breastfeeding Intervention Trial (PROBIT): A randomized trial in the Republic of Belarus. JAMA, 285(4), 413–420. 10.1001/jama.285.4.413 [DOI] [PubMed] [Google Scholar]
- Lindhart, C. L. , Rubak, S. , Mogensen, O. , Lamont, R. F. , & Joergensen, J. S. (2013). The experience of pregnant women with a body mass index >30 kg/m2of their encounters with healthcare professionals. Acta Obstetricia et Gynecologica Scandinavica, 92(9), 1101–1107. 10.1111/aogs.12186 [DOI] [PubMed] [Google Scholar]
- Nickel, N. C. , Labbok, M. H. , Hudgens, M. G. , & Daniels, J. L. (2013). The extent that noncompliance with the Ten Steps to Successful Breastfeeding Influences Breastfeeding Duration. Journal of Human Lactation, 29(1), 59–70. 10.1177/0890334412464695 [DOI] [PubMed] [Google Scholar]
- Nommsen‐Rivers, L. A. , Chantry, C. J. , Peerson, J. M. , Cohen, R. J. , & Dewey, K. G. (2010). Delayed onset of lactogenesis among first‐time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. The American Journal of Clinical Nutrition, 92(3), 574–584. 10.3945/ajcn.2010.29192 [DOI] [PubMed] [Google Scholar]
- Oddy, W. H. , Li, J. , Landsborough, L. , Kendall, G. E. , Henderson, S. , & Downie, J. (2006). The association of maternal overweight and obesity with breastfeeding duration. The Journal of Pediatrics, 149(2), 185–191. 10.1016/j.jpeds.2006.04.005 [DOI] [PubMed] [Google Scholar]
- O'Sullivan, E. J. , Perrine, C. G. , & Rasmussen, K. M. (2015). Early breastfeeding problems mediate the negative association between maternal obesity and exclusive breastfeeding at 1 and 2 months postpartum. The Journal of Nutrition, 145(10), 2369–2378. 10.3945/jn.115.214619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl, R. M. , & Heuer, C. A. (2010). Obesity stigma: Important considerations for public health. American Journal of Public Health, 100(6), 1019–1028. 10.2105/AJPH.2009.159491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramoniene, G. , Maleckiene, L. , Nadisauskiene, R. J. , Bartuseviciene, E. , Railaite, D. R. , Maciuleviciene, R. , & Maleckas, A. (2017). Maternal obesity and obstetric outcomes in a tertiary referral center. Medicina (Kaunas, Lithuania), 53(2), 109–113. 10.1016/j.medici.2017.03.003 [DOI] [PubMed] [Google Scholar]
- Rasmussen, K. M. , Hilson, J. A. , & Kjolhede, C. L. (2001). Obesity may impair lactogenesis II. The Journal of Nutrition, 131(11), 3009S–3011S. 10.1093/jn/131.11.3009S [DOI] [PubMed] [Google Scholar]
- Rasmussen, K. M. , Hilson, J. A. , & Kjolhede, C. L. (2002). Obesity as a risk factor for failure to initiate and sustain lactation. Advances in Experimental Medicine and Biology, 503, 217–222. 10.1007/978-1-4615-0559-4_25 [DOI] [PubMed] [Google Scholar]
- Rasmussen, K. M. , & Kjolhede, C. L. (2004). Prepregnant overweight and obesity diminish the prolactin response to suckling in the first week postpartum. Paediatrics, 113(5), e465–e471. 10.1542/peds.113.5.e465 [DOI] [PubMed] [Google Scholar]
- Sipsma, H. L. , Jones, K. , & Nickel, N. C. (2017). Hospital practices to promote breastfeeding: The effect of maternal age. Birth 10.1111/birt.12284, 44, 272–280. [DOI] [PubMed] [Google Scholar]
- Sipsma, H. L. , Kornfeind, K. , & Kair, L. R. (2017). Pacifiers and exclusive breastfeeding: Does risk for postpartum depression modify the association? Journal of Human Lactation, 33(4), 692–700. 10.1177/0890334417725033 [DOI] [PubMed] [Google Scholar]
- Turcksin, R. , Bel, S. , Galjaard, S. , & Devlieger, R. (2014). Maternal obesity and breastfeeding intention, initiation, intensity and duration: A systematic review. Maternal & Child Nutrition, 10(2), 166–183. 10.1111/j.1740-8709.2012.00439.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojcicki, J. M. (2011). Maternal prepregnancy body mass index and initiation and duration of breastfeeding: A review of the literature. Journal of Women's Health (2002), 20(3), 341–347. 10.1089/jwh.2010.2248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (1998). Evidence for the Ten Steps to Successful Breastfeeding. Retrieved from Geneva:
- World Health Organization . (2018). Ten Steps to Successful Breastfeeding (revised 2018). Retrieved from http://www.who.int/nutrition/bfhi/ten-steps/en/
- Yang, S. , Platt, R. W. , Dahhou, M. , & Kramer, M. S. (2014). Do population‐based interventions widen or narrow socioeconomic inequalities? The case of breastfeeding promotion. International Journal of Epidemiology, 43(4), 1284–1292. 10.1093/ije/dyu051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, J. , Troendle, J. , Reddy, U. M. , Laughon, S. K. , Branch, D. W. , Burkman, R. , … Consortium on Safe, L . (2010). Contemporary cesarean delivery practice in the United States. American Journal of Obstetrics and Gynecology, 203(4), 326 e321–326 e310. 10.1016/j.ajog.2010.06.058 [DOI] [PMC free article] [PubMed] [Google Scholar]


