Abstract
Background:
HIV pre-exposure prophylaxis (PrEP) reduces incident HIV infections, but efficacy depends on adherence and retention, among other factors. Substance use disorders, un-met mental health needs, and demographic factors are associated with non-adherence in HIV-infected patients; we studied whether these affect PrEP retention in care.
Methods:
To investigate potential risk factors for disengagement in a comprehensive HIV prevention program, we conducted a retrospective cohort analysis of individuals starting tenofovir-emtricitabine between 1/1/2015 and 11/30/2017. The primary outcome was adherence to the initial three visit schedule after PrEP initiation.
Results:
The cohort was predominantly African American (23%) and Hispanic (46%). Race, ethnicity, substance use, patient health questionnaire 9 score, insurance, and housing status were not associated with retention at the third follow-up visit. Age < 30, PrEP initiation in 2017, PrEP initiation in the sexual health clinic, and PrEP same-day start were associated with lower retention; Male gender at birth, transition from post-exposure prophylaxis (PEP) to PrEP, feeling that they could benefit from, or participating in mental health services were associated with increased retention. Overall, retention in HIV preventative care at the first follow-up visit (68%) and third follow-up visit (35%) after PrEP initiation was low.
Conclusion:
Clinic services and ancillary services (like mental health) may facilitate retention in care. In this study select social and behavioral determinants of health were not found to be linked to retention. Focused investigation of reasons for dropout may elucidate the challenges to maintaining individuals in PrEP care and direct resource allocation to those in greatest need.
Keywords: HIV Prevention, PrEP, Retention, Adherence, Risk Factors
Introduction:
HIV pre-exposure prophylaxis (PrEP) effectively reduces incident HIV infections, but its efficacy depends on adherence and retention in care, among other factors.1 Limited data on PrEP adherence in real-world settings are available; in comparable HIV-infected patients, substance use disorders, un-met mental health needs, and a variety of demographic factors are associated with non-adherence to antiretroviral therapy (ART).2 Programs designed to administer PrEP to high-risk individuals have therefore recognized the need to provide concurrent access to mental health and substance use services, preferably as part of an integrated care model. As PrEP programs expand to meet the projected need, the cost of providing these key services will be considerable. Identifying services critical to supporting PrEP adherence and identifying patients at highest risk of loss-to-follow-up is therefore essential. We investigated potential risk factors for poor retention after an initial intensive visit in a PrEP program that serves a predominantly African American and Latino patient population and offers support services including PrEP navigators, insurance benefit navigators, and mental health providers.
Methods
Program Description:
This study was performed at a large urban academic medical center consisting of inpatient and ambulatory care services in northern Manhattan. The HIV Prevention Program primarily includes two HIV/infectious disease clinics and one sexual health clinic. The program serves an area with high HIV prevalence (greater than 2%) and economic disadvantage (25% of households below the federal poverty line).3 The HIV Prevention Program provides PrEP to men who have sex with men (MSM), transgender individuals, and heterosexual men and women at risk for HIV acquisition according to New York State Department of Health (NYSDOH) PrEP guidelines.4 Comprehensive clinical services, PrEP coordination, benefits navigation, and mental health services including social work and psychiatry are provided. Same-day PrEP initiation is encouraged for eligible and interested patients. Partnerships with local pharmacies facilitate prescription pick-up immediately after an appointment. PrEP and benefit navigation is provided to help patients enroll in insurance or receive free medications through industry sponsored patient assistance programs. Patients prescribed PrEP have a one-month follow-up visit; subsequent visits are every three months.
Study Description:
We conducted a retrospective cohort analysis of individuals assessed for comprehensive HIV prevention services between 1/1/2015 and 11/30/2017. Patients were followed through 9/30/2018. Patients excluded from analysis included those who were HIV positive (n=14), had an incorrect medical record number (n=7), did not meet criteria for PrEP (n=18), were seen at an unrelated medical center (n=209) that is part of our hospital network, and patients who had been receiving HIV prevention care for greater than 60 days prior to entry into our program (n=11).
PrEP coordinators enter all screened patients into a database which contains basic demographics, HIV risk information, and PrEP start/stop dates. This data was validated and supplemented by extracting sexually transmitted infection (STI) testing, pharmaceutical prescriptions, and clinic visit data from the electronic medical record. PrEP start dates and contact information were verified through a chart review of clinician and coordinator notes. Additional questionnaires were collected from 210 patients initially evaluated at the sexual health clinic; the questionnaires included detailed information on sexual risk, substance use, and mental health.
The primary outcome was adherence to the initial three visits scheduled after PrEP initiation. PrEP initiation, the “initial visit”, could have occurred either at our program or at one of the NYC Department of Health and Mental Hygiene (DOHMH) sexual health clinics. PrEP initiation was considered day 0. To accommodate scheduling delays and missed doses, we allowed an interval of up to 60 days from initiation to first visit and 120 days between follow-up visits. Retained at a “first follow-up visit” (i.e. second overall visit), was defined as having a visit between day 14 and day 60 or documentation of enough prescription refills to last within one week of the second follow-up visit. Retained in care at a “second follow-up visit,” was defined as having a visit between day 60 and day 165, and no more than 120 days from prior visit, or documentation of having prescription refills to last within one week of the visit. Retained in care at a “third follow-up visit,” was defined as completing second follow-up visit and having a visit between day 135 and day 285, no more than 120 days from prior visit, or documentation of having prescription refills to last within one week of the visit. Demographic characteristics, visit history, STI results, and self-reported risk factors (when available) were compared between retained patients and those lost to follow up at the third follow-up visit
Results:
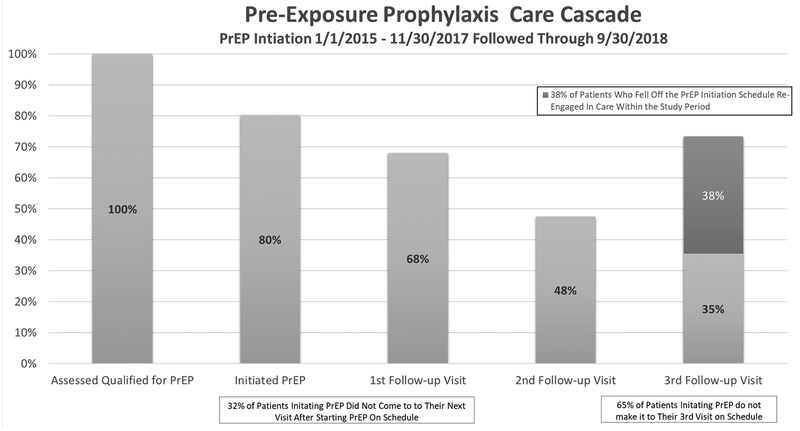
867 individuals were assessed for HIV prevention services. 696 (80%) initiated PrEP; 49.5% of those started PrEP on the same day as their initial visit. Of individuals initiating PrEP, 68% attended a first follow-up visit, 48% attended a second follow-up visit, and 35% attended a third follow-up visit on schedule. The largest drop off occurred between PrEP initiation and the first follow-up visit (32% lost to follow-up) (Figure 1).
Figure 1:
Pre-Exposure Care Cascade for Individuals Starting PrEP from 1/1/2015 through 11/30/2017 and followed through 9/30/2017 for Retention in Care Through the First Three Visits and Re-Engagement at Any Time. *”First follow-up visit” was defined as having a visit between day 14 and day 60 or documentation of enough prescription refills to last within one week of the second follow-up visit.
**”Second follow-up visit,” was defined as having a visit between day 60 and day 165, and no more than 120 days from prior visit, or documentation of having prescription refills to last within one week of the visit.
***”Third follow-up visit,” was defined as completing second follow-up visit and having a visit between day 135 and day 285, no more than 120 days from prior visit, or documentation of having prescription refills to last within one week of the visit.
Mean and median ages of individuals starting PrEP were 31 and 29 years respectively. 93% were male at birth, 23% identified as African American, and 46% identified as Hispanic. 68% of the individuals started PrEP in 2017, 30% had their first visit in the sexual health clinic, 11% transitioned from PEP to PrEP. 11.5% of patients had a known HIV-positive partner and 18% had an STI at the time of PrEP initiation. 20% of patients were uninsured. (Table 1).
Table 1:
Demographic and Clinical Characteristics of Individuals Starting PrEP from 1/1/2015 through 11/30/2017 and followed through 9/30/2018 for Retention at The Third Follow-up Visit
| Total Patients | Retention at 3rd Follow-Up Visit After Initiation | Odds Ratio (CI) | |
|---|---|---|---|
| Patients Starting PrEP | 696 | 247 (35.5%) | |
| Sex at Birth and Gender | |||
| Male at birth | 649 (93.2%) | 240 (37.0%) | 2.37 (1.02 – 5.49) |
| Female at birth | 36 (5.2%) | 7 (19.4%) | Ref (-) |
| Identify as Trans-Female | 11 (1.6%) | 5 (45.5%) | 1.53 (0.46 – 5.05) |
| Age | |||
| <30 | 377 (54.2%) | 121 (32.1%) | 0.72 (0.53 – 0.99) |
| >=30 | 319 (45.8%) | 126 (39.5%) | Ref (-) |
| Race/Ethnicity | |||
| African American | 160 (23.0%) | 53 (33.1%) | 0.87 (0.6 – 1.29) |
| Hispanic | 318 (45.7%) | 117 (36.8%) | 1.11 (0.81 – 1.52) |
| PrEP Initiation | |||
| Started in 2015 or 2016 | 223 (32.0%) | 108 (48.4%) | Ref (-) |
| Started in 2017 | 473 (68.0%) | 139 (29.4%) | 0.44 (0.32 – 0.62) |
| Started in Sexual Health Clinic | 210 (30.2%) | 61 (29.0%) | 0.66 (0.47 – 0.94) |
| PEP Transition to PrEP | 76 (10.9%) | 35 (46.1%) | 1.64 (1.02 – 2.66) |
| PrEP Same Day Start | 104 (49.5%) | 98 (30.8%) | 0.69 (0.5 – 0.94) |
| Sexual Risk Factors | |||
| STI at PrEP Start | 127 (18.2%) | 50 (39.4%) | 1.23 (0.83 – 1.82) |
| Rectal STI at PrEP Start | 53 (7.6%) | 17 (32.1%) | 1.26 (0.61 – 2.6) |
| Positive Test for Syphilis at PrEP Start | 32 (4.6%) | 13 (40.6%) | 1.08 (0.59 – 1.99) |
| Self-Reported STI prior to Starting PrEP* | 121 (57.6%) | 36 (29.8%) | 1.08 (0.59 – 1.99) |
| Considers themselves to have a current partner* | 48 (22.9%) | 15 (31.3%) | 1.15 (0.57 – 2.31) |
| Has at least one known HIV + Partner | 80 (11.5%) | 30 (37.5%) | 1.1 (0.68 – 1.79) |
| Mental Health | |||
| History of mental health counseling* | 46 (21.9%) | 15 (32.6%) | 1.24 (0.61 – 2.51) |
| Feels that they would benefit from mental health counseling at time of PrEP initiation* | 23 (11.0%) | 11 (47.8%) | 2.5 (1.04 – 6.01) |
| History of prior self-injury or suicide attempt* | 18 (8.6%) | 6 (33.3%) | 1.25 (0.45 – 3.48) |
| History of physical or sexual abuse* | 31 (14.8%) | 11 (35.5%) | 1.42 (0.63 – 3.17) |
| PHQ9 >5** | 37 (17.6%) | 8 (25.8%) | 0.82 (0.39 – 1.71) |
| Mental Health Visit After PrEP Start | 88 (12.6%) | 52 (59.1%) | 3.06 (1.94 – 4.84) |
| Substance Use | |||
| Tobacco use in the past 3 months* | 143 (68.1%) | 38 (26.6%) | 0.69 (0.37 – 1.3) |
| Alcohol use on the weekends or more in the last 3 months* | 118 (56.2%) | 31 (26.3%) | 0.74 (0.41 – 1.34) |
| Marijuana use more than monthly* | 72 (34.3%) | 15 (20.8%) | 0.53 (0.27 – 1.03) |
| Recreational drug use in the past 3 months* | 59 (28.1%) | 18 (30.5%) | 1.1 (0.57 – 2.13) |
| Insurance and Housing Status | |||
| Uninsured**** | 141 (20.3%) | 52 (36.9%) | 0.94 (0.57 – 1.57) |
| Public Insurance**** | 69 (9.9%) | 25 (36.2%) | 0.93 (0.52 – 1.65) |
| Private Insurance**** | 46 (6.6%) | 19 (41.3%) | 1.22 (0.63 – 2.33) |
| Stable Housing**** | 271 (38.9%) | 96 (35.4%) | 0.78 (0.46 – 1.35) |
| Unstable Housing**** | 11 (1.6%) | 1 (9.1%) | 0.17 (0.02 – 1.32) |
Data only available from 210 patients,
Data only available from 201 patients
Data only available from 339 patients,
Data only available from 256 patients
An additional comprehensive questionnaire was completed by 210 individuals who initially accessed PrEP through the sexual health clinic. 28.1% reported recent recreational drug use, 14.8% reported prior sexual abuse, 21.9% reported prior mental health counseling, and 17.6% reported symptoms associated with mild depression (score >5 on patient health questionnaire 9, PHQ-9) (Table 1).
Race, ethnicity, substance use, PHQ-9 score>5, insurance, and housing status were not associated with retention at the third follow-up visit. Age less than 30 (OR 0.72, CI 0.53 – 0.99), PrEP start in 2017 (OR 0.44, CI 0.32 – 0.62), PrEP start in the sexual health clinic (OR 0.66, CI 0.47 – 0.94), and PrEP same-day start (OR 0.69, CI 0.5 – 0.94) were associated with decreased retention at the third follow-up visit. Male gender at birth (OR 2.37, 1.02 – 5.49), transition from PEP to PrEP (OR 1.64, CI 1.02 – 2.66) and participating in mental health services (OR 3.136, CI 1.974 – 4.981) were associated with increased retention at the third follow-up visit.
Discussion:
Overall we observed 68% retention at the first follow-up visit after PrEP initiation and 35% retention at the third follow-up visit. While these numbers are lower than that of a sexual health clinic program that retained 74% of patients at 6 months, our data are similar to those of three US cities, where overall retention at 6 months was 60%. Retention was higher in smaller programs (Missouri and Mississippi) and lower in Rhode Island.5,6 A program in a different NYC medical center with similar demographic makeup had comparable results demonstrating a 6 month retention of only 42%.7 Our findings are also comparable, though with shorter follow-up, to programs in San Francisco and Chicago, where 47% and 43% of patients were retained at 12 months, respectively.5,8
One of the challenges of comparing retention across sites is that retention in PrEP care does not have a standard definition. In one study, disengagement was defined as failure to start PrEP, discontinued PrEP, or loss to follow-up; however, the majority of patients were lost to follow-up, and the definition of lost to follow-up was not well described.6 In another study, retention was defined as failure to return within 30 days of the scheduled follow-up visit without evidence of transferring care.5 In a third study, retention in care six months after initial PrEP prescription was defined as documentation of a renewed prescription for PrEP and a repeat HIV test at 180 ± 60 days from the initial PrEP prescription.7 A fourth paper utilized visit constancy focusing on every 3 month visits with a PrEP provider.8 Standardizing definitions for PrEP engagement and retention is essential for planning larger studies and advancing PrEP research.
While loss to follow-up was common, we found that the majority (80%) of patients eligible for PrEP started it. This is similar to what has been observed in other clinic settings.5,6,9 However, we may underestimate loss to follow up at the first follow-up visit, as we included individuals who initiated PrEP at a DOHMH clinic and presented for follow up at our program, but we do not know how many patients initiated PrEP at the DOHMH and were immediately lost to follow-up. The largest proportion of individuals (32%) were lost to follow-up in the first month after PrEP start, even though the first month in PrEP care includes the most intensive coordinator outreach, designed to remove barriers to care and access. Retention was higher in individuals who started PrEP before 2017 and in those who were not initially seen at our sexual health clinic. Notably, more than twice the number of patients started PrEP in 2017 compared to 2015 and 2016 combined. These data suggest that as our PrEP program grew, the ratio of coordinators to patients may have become insufficient for the same level of patient outreach. Furthermore, retention may have suffered as PrEP was offered to those who may previously have been less enthusiastic about starting. As PrEP rollout continues to expand, it will be cost prohibitive to provide all services to all patients. The ability to not only identify individuals at highest risk of HIV acquisition but also to accurately identify individuals at risk of loss to PrEP follow up will be critical to efficiently allocate resources to those in greatest need of targeted interventions.
Same-day PrEP initiation is an appealing model proposed in STI clinics at major urban centers10,11 and has been the focus of public health campaigns in NYS and NYC as part of the Ending the Epidemic efforts. This approach has also been explored with same-day antiretroviral initiation for HIV positive individuals to reduce loss-to-follow-up and achieve faster virologic suppression. It has been successful in some settings,12–14 but enthusiasm for this approach is somewhat tempered by concerns about logistical complexity, intensity of resources needed to sustain it, and clinical concerns related to drug resistance and side effects. In our study, 49.5% of patients had a same-day PrEP start. Same-day PrEP initiation was possible through a partnership with a pharmacy that was geographically convenient to the clinic. While same-day PrEP starts are appealing, it is unclear if this contributed to our high rates of early loss to follow-up, as other sites have reported 17–19% non-initiation after PrEP is prescribed.6,9 If not associated with retention and potentially associated with high rates of disengagement, further roll-out of same-day PrEP may not be cost effective in the long term. More studies are needed to assess the impact of same-day initiation on PrEP retention.
Sociocultural factors such as substance use are well-known risk factors for HIV acquisition and poor antiretroviral adherence, but limited data exist on the role of these factors on PrEP persistence over time.15–18 A small number of studies have shown that poor adherence to PrEP, history of STIs, history of substance abuse, younger age, and African American identification were associated with poor retention in PrEP care.5,19 However in one online survey, 50% of individuals who discontinued PrEP reported doing so because of a change in their sexual behavior and self-perceived lower HIV risk.20 These patients may be more likely to re-engage in PrEP care should their perceived risk change. We found that 38% of patients who were lost to care at any point, later re-engaged in HIV preventive care. Further research on the reasons for PrEP self-discontinuation is critical to distinguish individuals who are lost to care but remain at high risk from those whose risk profile has changed and who may not require active engagement.
In our cohort, starting with PEP treatment and mental health support were associated with improved persistence on PrEP. Combining PEP and PrEP services may play an important role in linking individuals to care at a time when they are potentially most interested in learning about PrEP, as well as supporting them through periods of fluctuations in risk. Mental health diagnoses are a known risk factor for HIV acquisition, and the presence of readily available mental health services may be an important step in retaining the highest-risk individuals in prevention services. Notably, substance use, insurance status, and housing status were not negatively associated with retention. This highlights the focus placed by NYC and our clinic on minimizing these psychosocial and structural barriers to care. However, since geographical disparities exist in the availability of public funding for PrEP services, these factors may be barriers to retention in other locations.
A limitation of this study is the low number of persons who inject drugs (PWID); this may indicate that our clinic may not serve the hardest-to-reach individuals and may limit the generalizability of our results. Another limitation is our lack of detailed data on reasons for loss of follow up. Additionally, all risk factors were collected through a self-reported questionnaire and may suffer from reporting bias. Finally, we only used data recorded as part of routine practice; we therefore have the benefit of “real world” data, but we may not have captured additional, unknown variables that affect retention.
Despite its limitations this study highlights the complexity of prevention needs and the challenges of initiating PrEP among racially and ethnically diverse individuals. Larger studies are needed. Lack of a standard definition of retention in HIV prevention care needs to be addressed as it may hinder comparisons across programs. Furthermore, drivers of loss to follow up must be explored to enable future development of interventions that will support persistence in prevention and sexual health care.
Sources of Support:
Dr. Zucker is supported by the training grant “Training in Pediatric Infectious Diseases” (National Institute of Allergy and Infectious Diseases T32AI007531) and the New York STD Prevention Training Center (Centers for Disease Control - RFA-PS14-1407).
This project was funded in part by the New York City Department of Health and Mental Hygiene through a contract with Public Health Solutions. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the funders
Contributor Information
Jason Zucker, Divisions of Infectious Diseases, Departments of Internal Medicine and Pediatrics, Columbia University Medical Center, New York, NY, USA.
Caroline Carnevale, HIV Prevention Program, New York Presbyterian Hospital’s Comprehensive Health Center, New York, NY, USA.
Paul Richards, HIV Prevention Program, New York Presbyterian Hospital’s Comprehensive Health Center, New York, NY, USA.
Jacek Slowikowski, Comprehensive Health Program (CHP), New York Presbyterian Hospital, New York, NY, USA.
Alexander Borsa, HIV Prevention Program, New York Presbyterian Hospital’s Comprehensive Health Center, New York, NY, USA.
Felix Gottlieb, Fieldston school, New York, NY, USA.
Isabella Vakkur, Bowdoin College, Brunswick, ME, USA.
Christel Hyden, Department of Family and Social Medicine, Albert Einstein College of Medicine, New York, NY, USA.
Susan Olender, Division of Infectious Diseases, Department of Internal Medicine, Columbia University Medical Center, New York, NY, USA.
Alwyn Cohall, Mailman School of Public Health & Columbia University Medical Center, New York, NY, USA.
Peter Gordon, Division of Infectious Diseases, Department of Internal Medicine, Columbia University Medical Center, New York, NY, USA.
Magdalena E. Sobieszczyk, Division of Infectious Diseases, Department of Internal Medicine, Columbia University Medical Center, New York, NY, USA.
References:
- 1.Riddell J, Amico KR, Mayer KH. HIV Preexposure Prophylaxis. Jama. 2018;319(12):1261. doi: 10.1001/jama.2018.1917 [DOI] [PubMed] [Google Scholar]
- 2.Bulsara SM, Wainberg ML, Newton-John TRO. Predictors of Adult Retention in HIV Care: A Systematic Review. AIDS Behav. 2018;22(3):752–764. doi: 10.1007/s10461-016-1644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AIDSVu (www.aidsvu.org). Emory University, Rollins School of Public Health. https://aidsvu.org/contact-us/. Accessed October 2, 2017.
- 4.New York State Dept of Health. PrEP to Prevent HIV Acquisition. Available at: https://http://www.hivguidelines.org/prep-for-prevention/prep-to-prevent-hiv/-tab_3.Published May 2018. Accessed August 1, 2018. [Google Scholar]
- 5.Hojilla JC, Vlahov D, Crouch P-C, Dawson-Rose C, Freeborn K, Carrico A. HIV Pre-exposure Prophylaxis (PrEP) Uptake and Retention Among Men Who Have Sex with Men in a Community-Based Sexual Health Clinic. AIDS Behav. 2017:1–4. doi: 10.1007/s10461-017-2009-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dombrowski JC, Golden MR, Barbee LA, Khosropour CM. Patient Disengagement from an HIV Pre-Exposure Prophylaxis Program in a Sexually Transmitted Disease Clinic. Sex Transm Dis. 2018:1. doi: 10.1097/OLQ.0000000000000823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lankowski A, Bien C, Silvera R, Patel V, Felsen U, Blackstock O. PrEP in the Real World: Predictors of 6-Month Retention in a Diverse Urban Cohort. In: IAPAC Adherence.; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rusie LK, Orengo C, Burrell D, et al. Preexposure Prophylaxis Initiation and Retention in Care Over 5 Years, 2012–2017: Are Quarterly Visits Too Much? Clin Infect Dis. 2018;67(2):283–287. doi: 10.1093/cid/ciy160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan PA, Mena L, Patel R, et al. Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc. 2016;19(1):1–8. doi: 10.7448/IAS.19.1.20903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhatia R, Modali L, Lowther M, et al. Outcomes of Preexposure Prophylaxis Referrals from Public STI Clinics and Implications for the Preexposure Prophylaxis Continuum. Sex Transm Dis. 2018;45(1):50–55. doi: 10.1097/OLQ.0000000000000690 [DOI] [PubMed] [Google Scholar]
- 11.Ridgway JP, Almirol EA, Bender A, et al. Which Patients in the Emergency Department Should Receive Preexposure Prophylaxis? Implementation of a Predictive Analytics Approach. AIDS Patient Care STDS. 2018;32(5):202–207. doi: 10.1089/apc.2018.0011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koenig SP, Dorvil N, Dévieux JG, et al. Same-day HIV testing with initiation of antiretroviral therapy versus standard care for persons living with HIV: A randomized unblinded trial. PLoS Med. 2017. doi: 10.1371/journal.pmed.1002357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosen S, Maskew M, Fox MP, et al. Initiating Antiretroviral Therapy for HIV at a Patient’s First Clinic Visit: The RapIT Randomized Controlled Trial. PLoS Med. 2016. doi: 10.1371/journal.pmed.1002015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pilcher CD, Ospina-Norvell C, Dasgupta A, et al. The Effect of Same-Day Observed Initiation of Antiretroviral Therapy on HIV Viral Load and Treatment Outcomes in a U.S. Public Health Setting. J Acquir Immune Defic Syndr. 2016. doi: 10.1097/QAI.0000000000001134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morojele NK, Kekwaletswe CT. Associations Between Alcohol Use, Other Psychosocial Factors, Structural Factors and Antiretroviral Therapy (ART) Adherence Among South African ART Recipients. 2014:519–524. doi: 10.1007/s10461-013-0583-0 [DOI] [PubMed] [Google Scholar]
- 16.Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19(8):807–814. http://www.ncbi.nlm.nih.gov/pubmed/15867495. Accessed March 2, 2019. [DOI] [PubMed] [Google Scholar]
- 17.Wrubel J, Ph D, Stumbo S, Johnson MO, Ph D. Antiretroviral Medication Support Practices among Partners of Men Who Have Sex with Men : A Qualitative Study. 2008;22(11). doi: 10.1089/apc.2008.0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stirratt MJ, Remien RH, Smith A, et al. The Role of HIV Serostatus Disclosure in Antiretroviral Medication Adherence. AIDS Behav. 2006;10(5):483–493. doi: 10.1007/s10461-006-9106-6 [DOI] [PubMed] [Google Scholar]
- 19.Whitfield THF, John SA, Rendina HJ, Grov C, Parsons JT. Why I Quit Pre-Exposure Prophylaxis (PrEP)? A Mixed-Method Study Exploring Reasons for PrEP Discontinuation and Potential Re-initiation Among Gay and Bisexual Men. AIDS Behav. 2018;22(11):3566–3575. doi: 10.1007/s10461-018-2045-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naismith K, Jaenicke T. Washington PrEP DAP Client Survey Key Findings, 2017. Washington State Department of Health Office of Infectious Disease. Available at: https://www.doh.wa.gov/Portals/1/Documents/Pubs/430-073-WAPrEPDAPClientSurveyKeyFindings2017-English.pdf. Accessed August 1, 2018.