Abstract
Objective
To evaluate the bi‐planar robot navigation system for insertion of cannulated screws in femoral neck fractures.
Method
Between January 2016 and December 2016, 60 patients with femoral neck fractures were separately treated using percutaneous cannulated screws assisted by the bi‐planar robot navigation system (robot group) and conventional freehand surgery (freehand group). The fluoroscopy time, the number of drilling attempts, and the operation time were recorded during operations; the dispersion and parallelism of the cannulated screws on the posteroanterior and lateral images were measured after operations. Patients were followed up for 12–24 months and the Harris scores and the final results of the two groups were compared.
Results
During bi‐planar robot navigation system‐assisted surgery, the fluoroscopy time for acquisition of images was 2.3 seconds on average, and the time for planning screws during the operation was 2.8 min on average. The average fluoroscopy time during the placement of the guide pin was 5.7 seconds and 14.14 seconds (P = 0.00), respectively. The average time of the placement of the cannulated screws was 12.7 min and 19.4 min (P = 0.00), respectively, in the robot group and the freehand group. In the robot group, only one guide pin was replaced during the operation, and the average number of adjustments for each guide pin was 2.39 in the freehand group. The screw parallelism and dispersion measured by postoperative imaging in the robot group were significantly superior to those in the freehand group. From postoperative CT it was evident that there were 5 cases of screws exiting the posterior cortex in both groups. During the follow‐up phase, 1 case of femoral head necrosis and 5 cases of femoral neck shortening of more than 10 mm occurred in the robotic navigation group; 3 cases of femoral head necrosis, 1 case of fracture nonunion, and 2 cases of shortening of more than 10 mm occurred in the freehand group. At 18 months after surgery, the average Harris scores of the patients were 85.20 and 83.45, respectively, with no significant difference.
Conclusion
Using bi‐planar robot navigation system‐assisted placement of femoral neck cannulated screws can significantly reduce the time of intraoperative fluoroscopy, drilling attempts, and operation time. The placed screws are superior to the screws placed freehand in relation to parallelism and dispersion. However, it is still necessary for surgeons to have a good reduction of the femoral neck fracture before surgery and to be proficient in the operation of the robot navigation system. In summary, the bi‐planar robot navigation system is an effective assistant instrument for surgery.
Keywords: Femoral neck fractures, Bi‐planar robot navigation system, Cannulated screw fixation
Introduction
Femoral neck fractures are common in the elderly, accounting for 3.58% of total body fractures and 54% of hip fractures. In young people, the incidence is relatively low, with fractures tending to be caused by high‐energy injuries, and accounting for only 2% to 3% of all femoral neck fractures1, 2. The treatment of femoral neck fractures often results in many complications due to poor reduction, fixation instability, and osteoporosis3. According to a meta‐analysis, treatment is associated with high incidences of avascular necrosis of the femoral head (14.3%), nonunion (9.3%), malunion (7.1%), implant failure (9.7%), and surgical site infection (5.1%)4. Femoral neck fractures have higher requirements for treatment; otherwise, complications are more likely to occur.
It is believed that precise screw placement can ensure more stable fracture fixation, thus reducing the occurrence of related complications. Some studies indicate that ideal placement of screws allows the reduction of the fracture to show a good reduction in the posteroanterior and lateral images, while reducing the number of drilling attempts can reduce the iatrogenic fractures due to multiple drilling attempts5, 6, 7. The distal screw placement point should be above the smaller trochanter to reduce the risk of subtrochanteric fractures, so the angle of the screw placement should not be too large8. It is also reported that, after the screw is placed, the head end of the cannulated screw should be located within 5‐mm below the cartilage of the femoral head; and the cannulated screws should have cortical support within 3 mm of the femoral neck cortex. However, the ideal screw placement brings great difficulty to the operation. During conventional freehand operations, the surgeon needs a wealth of experience and more accurate screw placement can be achieved by proceeding with the operation step by step under fluoroscopy. In recent years, the navigation‐assisted placement of femoral neck screws has emerged as a new technology. Studies have shown that the use of navigation can provide accurate placement of the screws, while reducing the radiation exposure of the surgeon and the number of drilling attempts9. However, it only helps the surgeon to see and surgical experience and hand stability remain critical.
The bi‐planar robot system (TINAV) is based on 2D image navigation, can determine the ideal placement of the cannulated screws based on the posteroanterior and lateral images of the hip joint after the reduction, and subsequently provide the placement channels for the screws with its mechanical arm according to the planned route. The simulation surgery experiments show that the bi‐planar robot navigation system‐assisted placement of screws can be more accurate and reduce the number of drilling attempts compared to normal navigation, and does not increase operation time10. However, little clinical data has been reported so far.
We used data from 30 cases of robot‐assisted femoral neck cannulated screw placement and 30 cases of freehand placement of cannulated screws collected in 2016. We then comprehensively evaluated the bi‐planar robot navigation system and analyzed strengths and weaknesses. First, we compared the intraoperative fluoroscopy, drilling attempts, and the operation time of the two groups to evaluate its contribution to the operation. Second, after surgery, the parallelism and dispersion of screws in posteroanterior and lateral images were measured. Third, through follow up of the patients, the Harris score of hip joints were mathematical statistics, and related complications were compared. In what follows, we analyze the advantages and related deficiencies of robot‐assisted surgery.
Materials and Methods
General Clinical Data
We selected 60 patients with femoral neck fractures in 2016 and randomly divided them into two groups. Inclusion criteria: (i) patients with femoral neck fractures; (ii) patients treated with inverted triangle cannulated screws by using the robot navigation system or in traditional method; and (iii) patients aged over 18 years. Exclusion criteria: (i) poor general condition to receive the examinations; (ii) with other lower limb fractures; and (iii) other diseases like cerebral infarction that may affect patient walking. Posteroanterior and lateral X‐ray images and CT were obtained for all patients with femoral neck fractures before surgery, and we recorded the Garden classification of femoral neck fractures. The demographic data of the patients is listed in Table 1. The patients were randomly divided into two groups, and separately treated with robotic‐assisted internal fixation and with conventional freehand fixation with cannulated screws. There were no significant statistical differences in gender, age, cause of injury, time to operation from injury, injury side, and fracture type between the two groups, and they were comparable (P > 0.05). We performed a retrospective study.
Table 1.
Patient information
| Information | Robot group | Freehand group |
|---|---|---|
| Age (years) | 56 (39–82) | 56.2 (30–84) |
| Gender (male/female) | 11/19 | 12/18 |
| Fracture type (cases) | ||
| Garden I | 8 | 10 |
| Garden II | 5 | 7 |
| Garden III | 14 | 11 |
| Garden IV | 3 | 2 |
Operative Procedure
Robot Group
Navigation Robot Surgery Method
After anesthesia, all femoral neck fractures were closed reduction. With satisfactory fluoroscopy results, three inverted triangular parallel dispersing cannulated screws were placed using a new bi‐planar navigation robot, TiRobot (TINAVI Medical Technologies,Beijing, China). The navigation robot consists of a multi‐degree‐of‐freedom robotic arm, an optical tracking device, a surgical planning and controlling system, and surgical instruments that help the robot establish spatial coordinates (Fig. 1). The bi‐planar navigation robot needs to place a specific tracking device on the patient's tibia after the fracture is reduced. This optical tracking system is a binocular camera based on infrared light, which can bring the spatial position error to less than 0.3 mm, so that the robot can track the patient in real time11. Then a positioning device is connected, appropriate posteroanterior and lateral X‐ray films of the hip joint are captured, and the patient's imaging information is collected by the robot operating system. The operator then plans the screw position on the operating platform. After planning, the operation screen will show whether the screws are parallel, together with the length of the screws (Fig. 2). The robotic arm will then run to the corresponding position according to the planning, and the screw is placed in the channel. The surgeon places the guide pins one by one according to the conventional screw placement method. After achieving satisfactory fluoroscopy results, the cannulated screw is placed.
Figure 1.

The bi‐planar robot navigation system construction (A) includes a robotic arm, an optical tracking device, and a surgery planning and controlling system. (B) The robot arm provided a guide channel for the surgeon during the operation.
Figure 2.
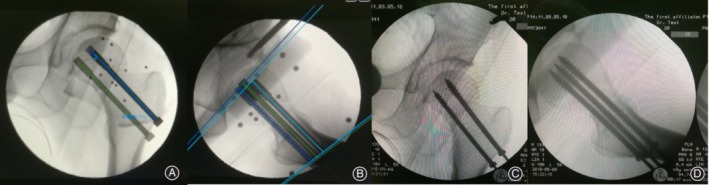
The surgeon could place the screw in the desired position through the workstation of the system (A, B). The robot arm would then provide a guide channel to help the surgeon achieve screw placement in a precise position. From the intraoperative anteroposterior (C) and lateral (D) radiographs, we can see that the screws were placed in the surgeon's planned position.
Freehand Group
In the conventional freehand fixation group, the screws were inserted with the use of standard c‐arm fluoroscopy after satisfactory closed reduction. Based on anteroposterior and lateral images, the screws were inverted in a satisfactory position.
Data Collection and Imaging Measurements
Intraoperative Related Information
After fracture reduction and satisfactory results of fluoroscopy were achieved in these two groups of patients, the number of fluoroscopy images during the insertion of screws during operation was recorded. The number of drilling attempts was also recorded. The number of drilling attempts is defined as: each time the needle is repositioned or the angle is readjusted during the insertion process12. Finally, the time from the reduction to fully placing the screws was recorded. The robot group also needs to record the time of fluoroscopy when the robot collected the patient's imaging information. After obtaining the image information, the screw position was planned and the operator's planning time was also recorded.
Imaging Measurement after Operation
After the cannulated screw was placed, anteroposterior and lateral X‐ray images of the hip joint were taken. The parallelism and dispersion of the screws was measured on the plain and lateral films using mimics 19 measurement software. The two tangential points closest to the curvature of the femoral neck were measured, by connecting the points of tangency and measuring the distance between the outer edge of the screws, and the width of the femoral neck. The dispersion percentage is defined as the ratio of the distance between the screws to the width of the femoral neck. On the anteroposterior and lateral images, the angle between the screws and the femoral shaft was determined, and the angle difference between the screw and the femur. θ = (|θ1 – θ2 | + |θ1 –θ3 | + |θ2 –θ3 |)/313°.
Postoperative Patient Follow Up
The patients in the two groups were followed up for 12–24 months. The fracture healing and related complications were observed. The Harris scores were taken in the two groups.
Statistical Analysis
Data were analyzed descriptively by using means, Student's t‐test, and Fisher's exact test. A 5% significance level was applied for all tests (P < 0.05). statistical software (IBM SPSS Statistics22; SPSS, Chicago, Illinois, USA) was used for all statistical analyses.
Results
Preparation Time of the Robot System
Finally, relevant data from the operation and postoperative imaging data were collected. In robot navigation‐assisted surgery, the fluoroscopy time for acquisition of images was 2.3 seconds on average; the time for screws planing during the operation was 2.8 min on average.
Intraoperative Fluoroscopic Time
The average fluoroscopy time during the guide pin placement was 5.7 seconds in the robot group; in the freehand group, the time was 14.14 seconds. Using the robot system can significantly decrease the fluoroscopic time (P < 0.01).
Number of Drilling Attempt
Only one guide pin was readjusted in all 30 robot assisted operations. However, in the freehand group, the average number of adjustments of guide pins was 2.39 times. Obviously, the robot system can help surgeons to insert the screw accurately in the ideal position.
Total Placement Time of Cannulated Screws
The average time for the placement of three cannulated screws was 12.7 min in the robot group and 19.4 min in the freehand group. Using the robot system can significantly decrease the operation time (P < 0.01).
All intraoperative statistics of the two groups are shown in Table 2.
Table 2.
Intraoperative data
| Groups | Number of patients | Fluoroscopy time for each screw placement (s) | Number of drilling attempt (times) | Total placement time of cannulated screws (min) |
|---|---|---|---|---|
| Robot navigation group | 30 | 5.65 | 0.01 | 12.6 |
| Freehand group | 30 | 14.14 | 2.39 | 19.4 |
| Statistics | 60 | t = −9.49, P = 0.00 | t = −12.71, P = 0.00 | t = −4.59, P = 0.00 |
Parallelism of Screws
The anteroposterior screw shaft angle was 1.08° in the robot group versus 1.2° in the freehand group (P = 0.437) and the lateral screw shaft was 1.25° in the robot group versus 1.82° in the freehand group (P = 0.028). The parallelism of the robotic group screws in the lateral image was significantly better, and there was no significant difference in the parallelism in the anteroposterior image.
Dispersion of Screws
The average anteroposterior dispersion percentage was 65.13% in the robot group versus 58.29% of the femoral neck (P < 0.01) in the freehand group; the lateral dispersion percentage was 70.08% versus 61.53% (P < 0.01). The screws inserted in the robot group have better dispersion.
Postoperative imaging measurements of the two groups are shown in Table 3.
Table 3.
Statistics of postoperative image measurements
| Groups | Number of patients | Anteroposterior dispersion percentage (%) | Lateral dispersion percentage (%) | Anteroposterior screw shaft angle (°) | Lateral screw shaft angle (°) |
|---|---|---|---|---|---|
| Robot navigation group | 30 | 65.13 | 70.08 | 1.08 | 1.25 |
| Freehand group | 30 | 58.29 | 61.53 | 1.2 | 1.82 |
| Statistics | 60 | t = −4.492, P = 0.00 | t = −5.11,P = 0.00 | t = 0.782,P = 0.437 | t = 2.259,P = 0.028 |
Follow‐up Results
During the follow‐up period of 12–24 months, we took anteroposterior and lateral X‐ray images of patients every 1–3 months. After the fracture has healed, we graded the patients’ Harris hip scores. The Harris hip scores of the navigation robot group and the freehand group were 85.20 and 83.45, respectively (P > 0.05) with no significant difference.
Complications
There was 1 case of femoral head necrosis among the 30 patients in the robot navigation group. A total of 5 patients had severe shortening of the legs after fracture healing, and the femoral neck shortened more than 10 mm. The other patients had no obvious shortening with fracture healing. In the freehand group, 3 of 30 patients underwent hip arthroplasty after femoral head necrosis; 1 patient had non‐union and a failed internal fixation; 2 patients had severe fractures after fracture healing, with the femoral neck shortening more than 10 mm.
Through postoperative CT, we found that both groups had 5 patients with screws exiting the posterior cortex. In both anteroposterior and lateral X‐rays images, the screws appear to be in the neck of the femur but actually penetrate the cortex (Fig. 3).
Figure 3.
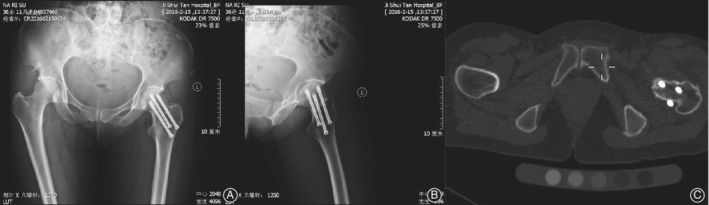
From anteroposterior (A) and lateral (B) X‐ray images, the screws appear to be in the neck of the femur, but, in fact, a screw penetrates the cortex in the posterosuperior of femoral neck (C) in the cross‐section from CT.
Discussion
Computer‐assisted orthopaedic surgery (CAOS) has been gradually recognized as a useful technique over the past few years. CAOS can improve visibility to the surgical field and operational accuracy through navigation systems and robotic devices during surgical procedures14. in vitro simulated surgery using cannulated screws to treat femoral neck fractures demonstrated that the CAOS system significantly improved the parallelism of screw placement and the dispersion of the screws in the femoral neck10. With the aging of the population, the incidence of femoral neck fractures is increasing, along with complications, so treatment requirements are becoming more stringent. Precise screw placement is believed to provide a more stable fixation. Femoral neck fracture fixation using 2D planar navigation robotic‐assisted cannulated screw placement is undertaken in this study.
Intraoperative Data
In the robot group of 30 patients, all the cannulated screws were placed in an ideal position after reduction of fractures. When using the bi‐planar robot to assist in the placement of the guide pin, only one guide pin was readjusted; the operation time of the cannulated screw insertion was 12.6 min, and the average number of drilling attempts in the freehand group was 2.39 times. The operation time was 19.4 min, and the use of the robot can achieve more precise placement of the guide pin than freehand. In addition, compared with Marcus Christian Müller's use of 3D navigation in 2012, the average operation time was 38 min, the drilling attempts was 3 times, bi‐planar robot could reduce the number of needle adjustments and the operation time12. This is due to the screw placement under 3D navigation, which still requires freehand positioning and subsequent adjustment under navigation, which is related to the experience of the operator. The robot navigation system provides more precise and fixed channels for the robot arm. It saves time in surgery and reduces the number of perspectives. At the same time, the risk of iatrogenic fractures is avoided because of the reduction in drilling attempts. Because the guide pins do not need to be adjusted repeatedly, and after the planned screws are placed, the operating platform can provide the length of the screws, which can also help to complete the screw placement and reduce fluoroscopy times.
Postoperative Imaging Measurements
Compared with the freehand group, the robot group had significant advantages in terms of the positive and lateral dispersity and lateral parallelism of the posterior cannulated screws. In this study, the third‐generation robots were used, which have an improved manipulator arm and an optical tracking system that allows minor changes in the procedure to be adjusted in time to make the surgery more accurate. Compared with Meir Liebergall's navigation screw placement study, the angle between the screws in the positive position is 1.34° versus 1.08°, and the lateral position is 1.68° versus 1.25°. The screws placed in the robotic navigation system are more parallel when placed under the navigation13. In the degree of dispersion, the robot navigation system has a greater advantage. The ratio of screw holding distance to the femoral neck in the positive position is 65.13%, which is much larger than the degree of dispersion under simple navigation. This is because when the robot‐assisted femoral neck cannulated screw is placed, the robotic arm provides a guide needle insertion channel, and the surgeon can safely place the screws tangent to the femoral neck cortex to obtain the cortical support of the screw. At the same time, because the mechanical arm provides a relatively stable passage, uncontrollable deviation of the guide needle caused by the shaking of the hand during the operation of the operator is avoided, so that the postoperative screw placement is more parallel.
Through postoperative CT we found that both groups had 5 patients with screws exiting the posterior cortex, which may decrease the stability of fixation and injure the blood supply to the femoral head15. This may have occurred because the surgeon wanted to place the screws peripherally and close to the femoral neck cortex so that the screws would obtain cortical support and better dispersion. Zhang et al.16. report that when screws appear close to the cortex on both radiographs, screws may have already perforated the cortex. The plan of where to place the screws is very important, but because of the insufficient information in 2D images, we cannot completely solve this issue at present.
Cortex support has also been shown to be more important in patients with osteoporotic femoral neck fractures. Orbel Filipov's biplane double‐supported screw fixation (BDSF) multi‐angle screw fixation has been demonstrated in biomechanical experiments and postoperative follow up as a possible effective method for the treatment of osteoporotic femoral neck17. However, the insertion angle of the screws is difficult to control, and the robot navigation system can better provide the needle guide channel due to the presence of the mechanical arm.
Clinical Outcomes
Postoperative femoral head necrosis and neck shortening after fracture healing occurred in both groups. There was no significant difference in hip Harris score between the two groups. As a unique technology to assist in operations, the navigation robot still needs to rely on the operator's preoperative reduction of the fracture and the planning of the placement of the screws. Therefore, the results of the two groups of patients after final follow‐up are similar. Shortening of the femoral neck of more than 10 mm will affect a patient's function18. Shortening may be related to the patient's fracture type, osteoporosis, and screw placement. At present, the robot can only assist in the placement of the screws, and the screw planning depends on the experience of the surgeon.
Current Defects of the Robot Navigation System
There are also shortcomings in the navigation robot system. First, because the navigation robot system needs to collect preoperative images and connect with related instruments and equipment, the preoperative preparation time is long. Second, because the ilium needs to be placed with an optical tracer, it will cause some damage to the patient. The connection between the optical camera and the tracer marker cannot be blocked during the procedure. Third, the spatial error of the bi‐planar navigation robot is 0.3 mm, but in this study, the angle of the worst parallelism of the screw is a poor 2.32°, and the lateral difference is 3.81°. This may be due to the fact that the mechanical arm is too close to the patient and the soft tissue is blocked. Fourth, because the channel provided by the mechanical arm is external, when the guide needle passes through the femoral neck cortical bone and femur, due to the harder bone barrier, the small elastic deformation may cause the guide needle to deflect in the bone, resulting in deviations in the original planning direction, which requires the surgeon to have a wealth of surgical experience and make adjustments through the surgery. Fifth, at present, robot navigation systems rely on the experience of the surgeon to conduct appropriate intraoperative planning.
The navigation robot can help the surgeon with screw planning and in precise needle positioning. However, the reduction of the fracture before surgery is very important. Only after the fracture is completely reduced can the operation achieve better curative effects. At the same time, the plan before the surgeon puts in the screws is also very important. The correct planning of screws is important for a successful operation.
Conclusion
When the bi‐planar robot navigation system is used to assist in femoral neck cannulated screw placement, the time of intraoperative fluoroscopy, drilling attempts, and operation time can be significantly reduced. In the present study, the bi‐planar robot navigation group had better screw parallelism and greater spread of screws. However, it is still necessary for the surgeons to have a good reduction of the femoral neck fracture before surgery and to be proficient in operating the robot navigation system. The bi‐planar robot navigation system is an effective assistant instrument for surgery.
Grant Sources: This work was supported by the Beijing Municipal Science and Technology Project (Z161100000116023), Capital's Funds for Health Improvement and Research: 2016–1‐2071.
References
- 1. Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma Acute Care Surg, 2010, 68: 236–242. [DOI] [PubMed] [Google Scholar]
- 2. Frihagen F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ, 2007, 335: 1251–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thiele OC, Eckhardt C, Linke B, Schneider E, Lill CA. Factors affecting the stability of screws in human cortical osteoporotic bone – A cadaver study. Bone Joint J, 2007, 89: 701–705. [DOI] [PubMed] [Google Scholar]
- 4. Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury, 2015, 46: 484–491. [DOI] [PubMed] [Google Scholar]
- 5. Booth KC, Donaldson TK, Dai QG. Femoral neck fracture fixation: a biomechanical study of two cannulated screw placement techniques. Orthopedics, 1998, 21: 1173–1176. [DOI] [PubMed] [Google Scholar]
- 6. Maurer SG, Wright KE, Kummer FJ, Zuckerman JD, Koval KJ. Two or three screws for fixation of femoral neck fractures?. Am J Orthop, 2003, 32: 438–442. [PubMed] [Google Scholar]
- 7. Zimmer WMX, Madsen PT, Teloni V, Johnson MP, Tyack PL. The complications of displaced intracapsular fractures of the hip: the effect of screw positioning and angulation on fracture healing. J Bone Joint Surg Br, 2005, 87: 1584 author reply 1584. [DOI] [PubMed] [Google Scholar]
- 8. Selvan VT, Oakley MJ, Rangan A, Al‐Lami MK. Optimum configuration of cannulated hip screws for the fixation of intracapsular hip fractures: a biomechanical study. Injury, 2004, 35: 136–141. [DOI] [PubMed] [Google Scholar]
- 9. Hamelinck HKM, Haagmans M, Snoeren MM, Biert J, van Vugt AB. Safety of Computer‐assisted Surgery for Cannulated Hip Screws. Clin Orthop Relat Res, 2007, 455: 241–245. [DOI] [PubMed] [Google Scholar]
- 10. Wang JQ, Zhao CP, Yong‐Gang SU, et al. Computer‐assisted navigation systems for insertion of cannulated screws in femoral neck fractures: a comparison of bi‐planar robot navigation with optoelectronic navigation in a Synbone hip model trial. Chin Med J, 2011, 124: 3906–3911. [PubMed] [Google Scholar]
- 11. Wang J, Yu W, Feng Y, et al. Percutaneous Sacroiliac Screw Placement: A prospective randomized comparison of robot‐assisted navigation procedures with a conventional technique. Chin Med J, 2017, 130: 2527–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Müller MC, Belei P, Pennekamp PH, et al. Three‐dimensional computer‐assisted navigation for the placement of cannulated hip screws. A pilot study. Int Orthop, 2012, 36: 1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liebergall M, Ben‐David D, Weil Y, Peyser A, Mosheiff R. Computerized Navigation for the Internal Fixation of Femoral Neck Fractures. J Bone Joint Surg Am, 2006, 88: 1748–1754. [DOI] [PubMed] [Google Scholar]
- 14. Nolte LP, Beutler T. Basic principles of CAOS. Injury, 2004, 35: 6–16. [DOI] [PubMed] [Google Scholar]
- 15. Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br, 2000, 82: 679–683. [DOI] [PubMed] [Google Scholar]
- 16. Zhang YQ, Chang SM, Huang YG, Wang X. The femoral neck safe zone: a radiographic simulation study to prevent cortical perforation with multiple screw insertion. J Orthop Trauma, 2015, 29: e178–e182. [DOI] [PubMed] [Google Scholar]
- 17. Orlin F, Boyko G. Unique stability of femoral neck fractures treated with the novel biplane double‐supported screw fixation method: A biomechanical cadaver study. Injury, 2015, 46: 218–226. [DOI] [PubMed] [Google Scholar]
- 18. Zlowodzki M, Brink O, Switzer J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi‐centre cohort study. J Bone Joint Surg Br, 2008, 90: 1487–1494. [DOI] [PubMed] [Google Scholar]


