Abstract
Objectives
The arthroscopic “lateral gutter drive‐through” (LGDT) sign is reported to diagnose popliteus tendon (PT) injury with high sensitivity and specificity. However, no study has provided a postoperative evaluation of combined posterior cruciate ligament (PCL) and posterolateral corner (PLC) injuries using the LGDT test.
Methods
From January 2012 to January 2015, a total of 80 consecutive patients who underwent combined PCL reconstruction and PLC surgeries were identified. Fifty eligible patients were included in this study for evaluation with subjective scoring systems, physical examinations, posterior and varus stress radiographs, and second‐look arthroscopic surgeries during hardware removal operation.
Results
Forty‐nine patients were available for a mean of 31.5 ± 9.3 months follow‐up (range, 24.0–81.0 months). In terms of PLC injury pattern, there were 27 type A, 10 type B, and 12 type C patients, with 21 acute cases and 28 chronic cases. At the final follow‐up, subjective scores were all significantly improved. The side‐to‐side difference (SSD) of posterior tibial translation (PTT) improved from 18.4 ± 9.2 mm (range, 12.9–25.6 mm) to 5.2 ± 5.0 mm (range, −5.0−18.5 mm, P < 0.001), and the SSD of tibial external rotation by dial test (ER) decreased from 18.0° ± 14.4° (range, 13.0°–22.0°) to 1.2° ± 7.5° (range, −9.0°–22.0°, P < 0.001). In patients with type C injury, the SSD of the lateral opening decreased from 14.2 ± 6.6 mm (range, 22–10.2 mm) to 0.9 ± 3.1 mm (range, −4.4‐6 mm, P < 0.001). In a comparison between patients with positive and negative LGDT signs, the LGDT‐negative patients had significant superiority in subjective scores, SSD of PTT, and SSD of ER. The sensitivity and specificity of the LGDT test in detecting postoperative posterolateral rotational instability (PLRI) were calculated as 100% and 88.4%, respectively.
Conclusions
In the series of surgically treated patients with PCL and PLC injury: (i) patients had improved subjective and objective clinical outcome after combined PCL reconstruction and PLC surgery at a minimum of 24‐months follow‐up; and (ii) second arthroscopic LGDT sign testing had high sensitivity and specificity in detecting postoperative PLRI, and a positive LGDT sign was related with inferior subjective and objective results.
Keywords: Lateral gutter drive through test, Popliteal tendon, Posterior cruciate ligament reconstruction, Posterolateral corner
Introduction
The combined posterior cruciate ligament (PCL) and posterolateral corner (PLC) injuries which typically occur secondary to a forced varus moment or after knee dislocation are among the most refractory conditions in the sports medicine clinic, because not only is the optimal treatment controversial and individualized, including the timing of surgery, repair versus reconstruction, autograft versus allograft reconstruction, postoperative rehabilitation protocols, and the indications for a tibial or femoral osteotomy, but also the diagnosis and postoperative evaluation require comprehensive and meticulous physical examinations, including the dial test, the reverse pivot‐shift test, the external rotational recurvatum test, and the posterolateral drawer test1, 2, 3, 4, 5, 6. Furthermore, these subjective evaluations rely on subtleties in the physical examinations, especially when facing concurrent multi‐ligament injuries.
The anatomy of the PLC of the knee includes the lateral collateral ligament (LCL), the popliteus tendon (PT), the popliteofibular ligament (PFL), and the lateral and posterolateral capsule. According to Fanelli's study6, posterolateral rotational instability (PLRI) was classified into three types. Type A indicated increased external rotation only, corresponding to injury to the PFL, and PT only. Type B presented with increased external rotation, and mild varus of less than 10 mm increased lateral joint line opening at 30‐degree knee flexion. This type indicated injuries to the PFL and the PT, and attenuation of the fibular collateral ligament. Type C presents with increased tibial external rotation, and varus instability, more than 10 mm lateral joint line opening, without a firm end point tested at both 0° and 30° of knee flexion with varus stress. This occurs with injury to the PFL, the PT, and the fibular collateral ligament, and lateral capsular avulsion in addition to cruciate ligament disruption.
The PCL is a primary restraint to posterior tibial translation at all flexion angles. It also has a role in primary restraint for internal rotation and external tibial rotation beyond 90° of flexion3. We classified the side‐to‐side difference in posterior tibial translation into: Grade 1, 0–5 mm of side‐to‐side difference in posterior displacement constitutes a partial PCL tear; Grade 2, 6–10 mm; and Grade 3, >10 mm of posterior translation.
The arthroscopic finding of a lateral compartment joint opening greater than 1 cm has been termed the “drive‐through” sign, consistent with an acute or chronic laxity of the lateral collateral ligament. Inspired by this, the “lateral gutter drive‐through” (LGDT) was first described to indicate: (i) the presence of femoral avulsion tears of the popliteal tendon or concomitant lateral collateral ligament; (ii) the presence of repairable posterolateral corner tears; and (iii) the enablement of mini‐open surgery for the repair of these avulsion tears with a recess or reattachment procedure6, 7. Recently, the LGDT test was reported to diagnose acute and chronic “peel‐off” and non‐peel‐off lesions of PT with high sensitivity and specificity6, 7, 8. According to the literature, the sensitivity and specificity of the LGDT test were calculated as 91.4% and 93.8%, respectively. Furthermore, popliteus femoral “peel‐off” lesions were detected with a sensitivity of 100% versus 87.0% in cases of non‐peel‐off lesions8. The positive LGDT, which was defined as the arthroscope passing into the posterolateral compartment through the interval between PT and the lateral femoral condyle at 30° of knee flexion, indicated the PLRI of the knee joints7. In the literature, all LGDT‐relevant studies discuss the diagnosis of PLRI, but none of them consider the postoperative evaluation of combined PCL and PLC surgeries with LGDT tests.
In contrast, cases of grade III PCL and PLC injury are rare. In the literature, although there are few studies concerning the treatment outcome of this specific population, there is still a paucity of evidence reporting the clinical outcome of this specific severe and complicated condition5. Moulton et al.5, in a systematic review, report a great variety of PLC repair and reconstruction techniques, such as fibular sling, posterolateral capsular shift, anatomic‐based PLC reconstruction of the LCL, PT, and PFL, biceps tenodesis, and advancement of the FCL femoral origin. Therefore, the treatment of patients with grade III PCL and PLC injury is subject to great controversy and uncertainty. In the present study, identification of the LGDT test as an adjacent tool of postoperative evaluation was one of our goals; the clinical outcomes measured with conventional subjective and objective methods of patients who underwent PCL reconstruction and PLC surgery were also reported.
The purpose of this study was: (i) to report the results of clinical outcomes of patients with surgically treated combined PCL and PLC injury, including physical examinations, subjective measurement, and radiological assessments; (ii) to determine the validity of LDGT in assessing postoperative posterolateral rotational instability (PLRI). We hypothesized that: (i) the objective and subjective clinical outcome would be significantly improved at the final follow‐up; and (ii) LGDT sign could be used as an adjunctive assessment of postoperative PLRI, and that patients with a positive LGDT sign had inferior clinical outcome compared with patients with a negative LGDT sign.
Materials and Methods
Study Design
Inclusion Criteria
The patients were eligible for inclusion in this study if they: (i) had grade III PCL and PLC injury; (ii) underwent PCL reconstruction and PLC surgery from January 2012 to January 2015 in our institution; (iii) were followed for a minimum of 2 years with second‐look arthroscopic findings; and (iv) were prospectively recruited.
Exclusion Criteria
Exclusion criteria included: (i) concomitant medial collateral ligament (MCL) Grade III lesion; (ii) arcuate fracture; (iii) isolated lateral collateral ligament (LCL) lesion; (iv) bilateral PCL or PLC injuries; (v) skeletal malalignment of the lower limb (varus aligned: hip‐knee‐ankle angle>182°, valgus aligned: hip‐knee‐ankle angle<178°) at the final follow‐up; (vi) previous knee surgery; and (vii) general joint laxity. Fifty patients were included in this study.
Of the 30 excluded patients, 22 had Grade III MCL lesions and 3 cases were isolated LCL injuries; there were 2 revision cases and there was 1 arcuate avulsion fracture, 1 bilateral PCL and PLC injury, and 1 previous arthroscopic surgery (lateral partial meniscectomy). One patient was lost to follow‐up (Fig. 1).
Figure 1.
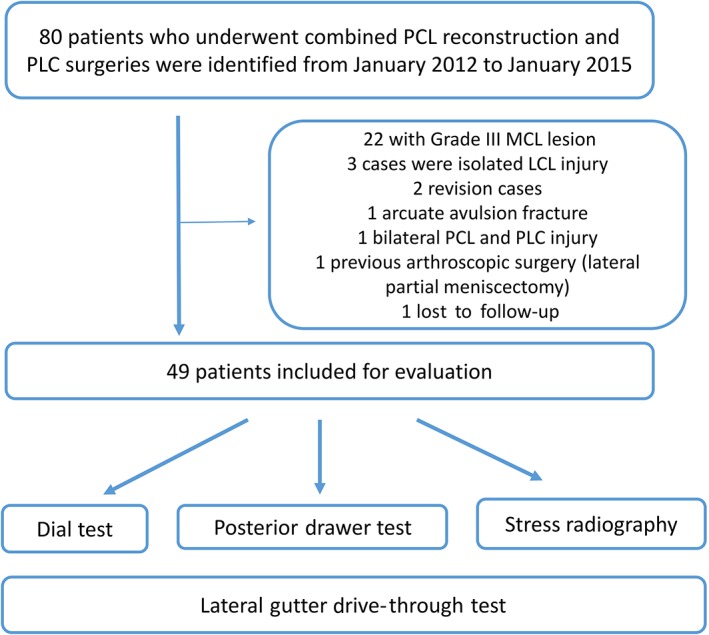
The flowchart of this study. LCL, isolated lateral collateral ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner.
Approval was obtained from the local ethics committee and all patients signed informed consent to be included in the study.
Preoperative and Postoperative Assessments
The patients were evaluated preoperatively and at postoperatively at 4 weeks, 8 weeks, 1 year, and every year thereafter until the final follow‐up.
Physical Examinations
All patients were tested with examinations under anesthesia (EUA) before the hardware removal procedure. Physical examinations included the dial test, the reverse pivot‐shift test, and the posterolateral drawer test. The range of motion was also recorded. External rotational stability was checked with a dial test at 90° of knee flexion by a single senior surgeon (Fig. 2). A photograph was taken at both initial and final positions. Using the photographs, the tibial external rotation angle was calculated, and the result was compared with the contralateral knee9. A positive dial test was defined as side‐to‐side difference (SSD) of ER > 10°.
Figure 2.
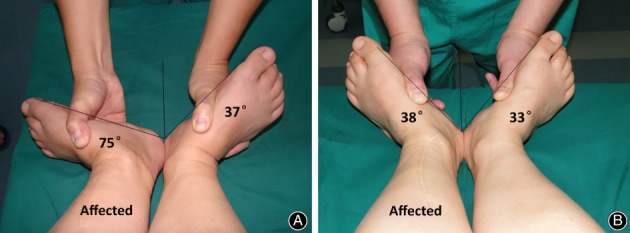
(A) A patient with positive dial test (SSD of ER: 75° − 37° = 38°). (B) The patient was treated with PT reconstruction. The SSD of ER was reduced to 38° − 33° = 5°. ER, external rotation; PT, popliteus tendon; SSD, side‐to‐side difference.
Subjective Measurement
The subjective measurement including the Lysholm score, the Tegner score, and the International Knee Documentation Committee (IKDC) subjective score were completed by an independent surgeon who was not involved during surgery.
Radiological Assessments
Radiological assessments included lower limb full‐length view and MRI scan of the knee. PCL stability was examined using a Telos stress radiographic unit (Telos, Weiterstadt, Germany) at 90° of knee flexion with a 150 N posterior load applied to the proximal tibia before and after the operations (Fig. 3). The side‐to‐side difference (SSD) of posterior tibial translation (PTT) was then calculated. LCL stability was tested with 150 N varus load applied to the knee joint. Preoperatively and at the final follow‐up, the SSD of ER and PTT, and the medial and lateral compartment opening under stress radiograph were all recorded.
Figure 3.

(A) A patient with PCL and PLC type A injury. The PTT of the injured knee under stress radiograph was 21 mm. (B) The patient was treated with transtibial PCL reconstruction. At the final follow‐up, the PTT reduced to 11.6 mm. (C) The contralateral healthy knee. The PTT was 6.1 mm. The preoperative SSD of PTT was 15.9 mm. The SSD of PTT at the final follow‐up was reduced to 5.5 mm. PCL, posterior cruciate ligament; PLC, posterolateral corner; PTT, posterior tibial translation; SSD, side‐to‐side difference
Second‐Look Arthroscopic Surgeries
Second‐look arthroscopic surgeries were performed during hardware removal surgery. The LGDT test was performed following the protocol of Feng et al.8: first, a 4‐mm 30° arthroscope with a sheath of 5.5‐mm diameter was placed in the lateral gutter with the knee at 20° to 30° of flexion with neutral tibial rotation to identify the lateral condyle and femoral insertion of PT; then, the arthroscope was moved to the lateral gutter. LGDT was defined as positive if the arthroscope could be inserted deeply into the posterolateral compartment while either internal or external rotation stress was applied to the tibia (Fig. 4).
Figure 4.
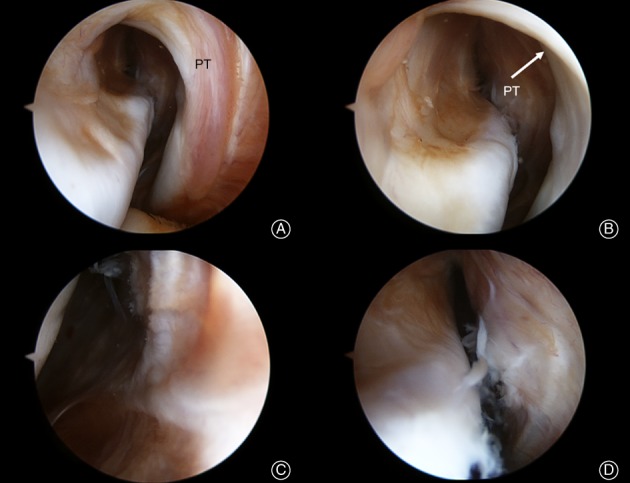
(A) The view of lateral gutter and reconstructed popliteus tendon (PT); (B) the arthroscope was inserted into the interspace between the lateral femoral condyle and the popliteus tendon; (C, D) the arthroscope was inserted deeply into the posterolateral compartment.
Surgical Technique
All surgeries were performed by the senior author. Arthroscopic assessment was conducted after all posterolateral knee injuries were identified. All patients underwent surgery under spinal epidural anesthesia. After successful anesthesia, the patient was placed in supine position.
All patients underwent arthroscopic transtibial single‐bundle PCL reconstruction with Achilles tendon allograft using a femoral outside–in technique10.
In terms of PT complex surgeries, the PT reconstruction (n = 33) was performed using open or arthroscopic posterolateral transtibial sling reconstruction. In patients with acute type I or type II PT femoral peel‐off lesions11 but without substantial stretching injury and tendon shortening at full knee extension, PT reattachment using a spiked metal washer (n = 6) was indicated and performed using the technique of Bonanzinga and Feng et al.9 Furthermore, the PT recess procedure12 was also applied in 5 patients. PFL reconstruction was performed in 3 patients according to the open method of Zhang et al.13, 14, 15. and the arthroscopic technique of Feng et al.16. In addition, 2 patients underwent anatomic‐based PT and PFL reconstruction following the technique of LaPrade et al.1, 12.
With respect to LCL management, 19 LCL reconstructions17 were completed with bone‐patellar tendon‐bone autograft and 1 LCL reattachment9 was achieved with a spiked metal washer. Other combined injuries, such as meniscal tear or chondral lesions, were treated simultaneously.
Rehabilitation Protocol
The knee was immobilized in a full‐extension padded brace with no weight bearing for 12 weeks postoperatively to protect the graft. Passive range of motion (ROM) exercise began 4 weeks after surgery. The goal was to achieve 90° of knee flexion 8 weeks postoperatively and 120° of flexion 12 weeks postoperatively. Partial weight bearing was allowed after 12 weeks, and gradually progressed to full weight bearing.
Active flexion and squatting were not allowed within the first 6 months. Sports activities without squatting were permitted after 6 months postoperatively. Patients were not allowed to participate in competitive or pivot‐type sports, such as basketball or soccer, until the involved knee stability had been specifically cleared for such activities by the surgeon 10 months after surgery9, 10.
Statistical Analysis
All analyses were performed using SPSS software for Windows, version 19.0 (Chicago, IL, USA). The normality tests demonstrated that age, the time from injury, the follow‐up time, and SSD of PTT at the final follow‐up were not normally distributed, and age and SSD of ER were normally distributed. Pearson's χ2 test was used to compare preoperative and postoperative distribution of the results of posterior drawer and varus stress tests. A binary logistic regression was also conducted to calculate the predicted probability of SSD of PTT, ER, and a combination of both. A receiver operating characteristic (ROC) curve was created to calculate the area under the curve (AUC) using the predicted probability SSD of PTT, ER, and a combination of both. The validity of the LGDT test compared with the golden standard (dial test) that determines the PLRI was also examined. The numbers of true‐positive tests, true‐negative tests, false‐positive tests, and false‐negative tests were calculated to determine sensitivity and specificity7. Based on a pilot study, assuming the clinically relevant difference of Lysholm score to detect to be 10, setting the significance level to be 0.05, and ß = 0.80, the sample size should be over 33.
Results
Demographic Data
This case series included 49 patients. The mean age was 32.0 ± 6.5 years (range, 20.0–44.0). The mean time from injury to surgery was 18.2 ± 23.7 weeks (range, 1.0–112.0). Patients were followed for a mean of 31.5 ± 9.3 months (range, 24.0–81.0) with a minimum of 24 months follow‐up. The classification of PLC injury was based on the publication of Fanelli et al.5. In the present series, there were 27 type A, 10 type B, and 12 type C patients. Among the 49 cases, there were 21 acute and 28 chronic cases.
Clinical Outcome of Posterior Cruciate Ligament and Posterolateral Corner Surgery
Physical Examinations, Subjective Measurement, and Radiological Assessments
At the final follow‐up, all results of EUA and stress radiography findings were significantly improved (Table 1, P < 0.001). The Lysholm score, the Tegner score, and IKDC the subjective score were all significantly increased (Table 2). There were 4 cases with SSD of PTT > 10 mm, and there was 1 case with SSD of PTT > 10 mm and ER > 20° at the final follow‐up.
Table 1.
Comparison of preoperative and postoperative physical examination, stress radiography, and LGDT findings
| Examinations | Preoperative (n = 49) | Postoperative (n = 49) | P‐value |
|---|---|---|---|
| PDT | 3+:40 2+:9 1+: 0 Negative: 0 |
3+:5 2+:2 1+: 22 Negative: 20 |
<0.001 |
| Varus stress test at 30° of knee flexion | 3+:11 2+:12 1+:26 Negative: 0 |
3+:1 2+:7 1+:15 Negative: 26 |
<0.001 |
| Dial test (mean ± SSD, °) | 18.0 ± 14.4 | 1.2 ± 7.5 | <0.001 |
| PTT (mean ± SSD) by stress radiography (mm) | 18.4 ± 9.2 | 5.2 ± 5.0 | <0.001 |
| LGDT | Positive: 49 Negative: 0 |
Positive: 11 Negative: 38 |
<0.001 |
LGDT, lateral‐gutter drive through; PDT, posterior drawer test; PTT, posterior tibial translation; SSD, side‐to‐side difference
Table 2.
Comparison of preoperative and postoperative subjective evaluations (mean ± SD)
| Scores | Preoperative (n = 49) | Postoperative (n = 49) | P‐value |
|---|---|---|---|
| Lysholm score | 43.8 ± 18.8 | 72.4 ± 14.8 | <0.001 |
| Tegner score | 1.9 ± 1.0 | 2.6 ± 0.7 | <0.001 |
| IKDC subjective score | 28.9 ± 9.8 | 77.1 ± 8.7 | <0.001 |
IKDC, International Knee Documentation Committee
Positive Lateral Gutter Drive‐Through Sign
Eleven patients were observed with positive LGDT sign. Among the 11 cases, there were 6 cases with SSD of ER > 10°, and 5 cases with SSD of PTT > 10 mm under the stress radiography test (Table 3). In terms of complications, there was 1 case with stiffness at 12 months, which was treated by manipulation under anesthesia.
Table 3.
Summary of 11 patients with positive LGDT sign
| No. | Age (years) | Sex | Time from injury to surgery (weeks) | PLC injury pattern | F/U time (months) | ΔPTT | ΔER | Pre‐op Lysholm | Post‐op Lysholm | Pre‐op Tegner | Post‐op Tegner | Pre‐op IKDC | Post‐op IKDC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | M | 2.0 | B | 37 | 18.5 | 8.0 | 17 | 55 | 2.0 | 1.0 | 21 | 57 |
| 2 | 26 | M | 3.0 | C | 29 | 15.6 | 9.0 | 80 | 61 | 2.0 | 2.0 | 12 | 49 |
| 3 | 39 | M | 3.0 | C | 33 | 3.5 | 10.1 | 32 | 67 | 2.0 | 1.0 | 34 | 66 |
| 4 | 26 | M | 2.0 | B | 25 | 11.1 | 2.0 | 35 | 59 | 1.0 | 2.0 | 22 | 42 |
| 5 | 36 | M | 1.0 | A | 29 | 13.0 | 4.0 | 85 | 64 | 1.0 | 1.0 | 21 | 37 |
| 6 | 35 | F | 78.0 | A | 27 | 6.9 | 14.0 | 45 | 60 | 3.0 | 1.0 | 27 | 71 |
| 7 | 38 | F | 3.0 | A | 25 | 9.9 | 10.2 | 52 | 58 | 3.0 | 1.0 | 27 | 31 |
| 8 | 26 | F | 24.0 | C | 43 | 4.3 | 10.6 | 36 | 53 | 3.0 | 1.0 | 42 | 58 |
| 9 | 33 | F | 12.0 | A | 28 | 9.9 | 6.0 | 28 | 66 | 0.0 | 2.0 | 41 | 70 |
| 10 | 35 | F | 16.0 | B | 27 | 5.2 | 12.3 | 76 | 76 | 0.0 | 2.0 | 32 | 76 |
| 11 | 29 | F | 24.0 | C | 32 | 17.5 | 22.0 | 53 | 55 | 0.0 | 2.0 | 28 | 68 |
F, female; F/U, follow‐up; IKDC, International Knee Documentation Committee; LGDT, lateral gutter drive‐through; M, male; PLC, posterolateral corner; ΔER, side‐to‐side difference of tibial external rotation; ΔPTT, side‐to‐side difference of posterior tibial translation
Validity of Lateral Gutter Drive‐Through Test as an Evaluation of Clinical Outcome
Comparison of Negative and Positive Lateral Gutter Drive‐Through Sign
In a comparison of subjective scores, SSD of PTT and ER between patients with negative and positive LGDT sign, a significant inferiority in patients with positive LGDT in all subjective and objective parameters was demonstrated (Table 4, Fig. 5). Setting the dial test as the gold standard to detect PLRI7, the sensitivity and specificity of the LGDT test were 100% and 88.4%, respectively (Table 5).
Table 4.
Comparison of objective and subjective evaluations in patients with negative and positive LGDT sign (mean ± SD)
| Evaluations | Negative LGDT (n = 38) | Positive LGDT (n = 11) | P‐value |
|---|---|---|---|
| SSD of PTT (mm) | 3.7 ± 3.6 | 10.5 ± 5.2 | <0.001 |
| SSD of ER (°) | −1.3 ± 6.1 | 9.4 ± 5.5 | <0.001 |
| Lysholm score | 75.8 ± 15.0 | 61.3 ± 6.7 | 0.003 |
| Tegner Score | 2.9 ± 0.3 | 1.4 ± 0.5 | <0.001 |
| IKDC subjective score | 83.2 ± 8.7 | 56.8 ± 15.1 | <0.001 |
ER, external rotation; IKDC, International Knee Documentation Committee; LGDT, lateral‐gutter drive through; PTT, posterior tibial translation; SSD, side to side difference
Figure 5.
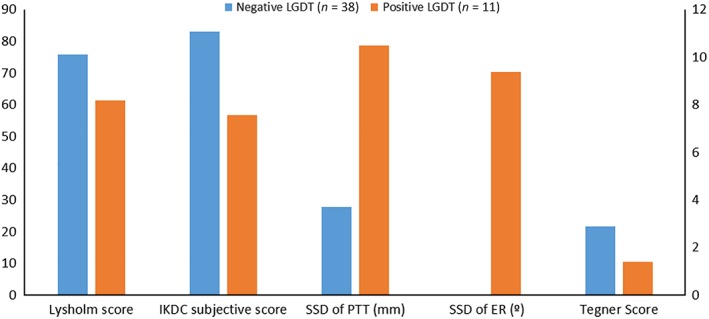
The comparison of objective and subjective outcome between patients with negative and positive LGDT sign. ER, external rotation; LGDT, lateral gutter drive‐through; PTT, posterior tibial translation.
Table 5.
Results of LGDT test in patients with negative and positive dial test (cases)
| LGDT | Dial test | Total | |
|---|---|---|---|
| Negative | Positive | ||
| Negative | 38 | 0 | 38 |
| Positive | 5 | 6 | 11 |
| Total | 33 | 6 | 49 |
LGDT, lateral‐gutter drive through; sensitivity, 100%; specificity, 88.4%
Receiver Operating Characteristic Curve
The ROC curve indicated that the SSD of ER and the SSD of ER coupled with PTT were significant predictors of positive LGDT. However, the AUC of the ROC curve of the SSD of ER coupled with PTT was 0.980 ± 0.017 (P < 0.001), which is higher than the SSD of ER (0.921 ± 0.040, P < 0.001) (Fig. 6).
Figure 6.
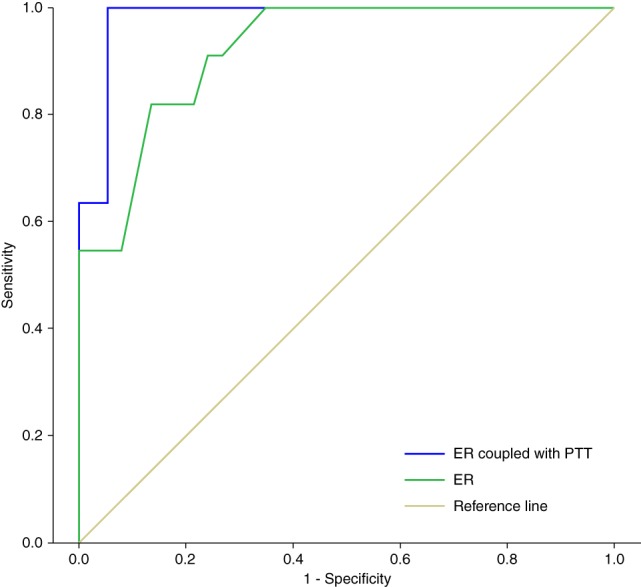
The ROC curve indicated that SSD of ER and SSD of ER coupled with PTT were significant predictors of positive LGDT. However, the AUC of the ROC curve of SSD of ER coupled with PTT was 0.980 ± 0.017 (P < 0.001), which was higher than for SSD of ER (0.921 ± 0.040, P < 0.001). AUC, area under the curve; ER, external rotation; LGDT, lateral gutter drive‐through; PTT, posterior tibial translation; ROC, receiver operating characteristic; SSD, side‐to‐side difference.
Discussion
The most important finding of this study was: (i) the improved objective and subjective clinical outcome with PCL reconstruction and PT complex surgical procedure in patients with combined PCL and PLC injury; and (ii) LGDT sign could be used as an adjunctive assessment of postoperative PLRI and patients with positive LGDT sign had inferior clinical outcome compared with patients with negative LGDT sign.
Clinical Outcome of Posterior Cruciate Ligament and Posterolateral Corner Surgery
In our cohort, 4 patients (8.2%) had SSD of PTT > 10 mm and 1 patient (2.0%) had both SSD PTT > 10 mm and ER > 20° at the final follow‐up. For PCL stability, Zorzi et al.18 reported 5 (5/19, 26%) cases with grade I step‐off sign, but no grade III posterior laxity was detected. However, consistent with the present study, Strobel et al.,19 in a study of combined one‐stage ACL, PCL, and PLC reconstruction, reported the rate of grade III posterior laxity as 11.8% (2/17). In terms of PLC surgical outcome, in a systematic review4 regarding the management of combined ACL or PCL and PLC injuries, the overall rate of undercorrection of external rotation laxity was 10%, which was comparable with the finding of the present study. Similar to our results, Sanders et al. reported3, that 88.5% (54/61) of patients had grade 0 varus laxity at 30° of knee flexion, 9.8% (6/61) had grade I laxity, and 1.7% (1/61) had grade II laxity. In another study, by Yoon et al.3, using anatomical PLC reconstruction, the varus and posterior stress radiograph showed a significant decrease to 0.9 mm and 5.3 mm, respectively.
Current Literature about Lateral Gutter Drive‐Through Test
The LGDT test was first proposed by Feng et al.8 as an arthroscopic indicator of acute femoral avulsion of the popliteus tendon. In patients with suspected PLC injuries, a positive LGDT sign usually called for a meticulous physical examination under anesthesia. The validity of the LGDT test was verified in the study of Shen et al.7, in which the sensitivity and specificity of the LGDT test to diagnose PLRI of the knee joint were calculated to be 91.4% and 93.8%, respectively. In addition, both popliteus femoral “peel‐off” lesions and “non‐peel‐off” lesions were detected with a sensitivity of higher than 85%. The mechanism of the LGDT sign was further examined in a cadaveric study6. It demonstrated that isolated sectioning of either distal PT, PFL or the LCL produced increased but insignificant external rotation angle (ETRA) with the LGDT tests was still negative, while simultaneous sectioning of PT and PFL could produce a positive LGDT sign. Confirmed by a navigation system, they reported that 2.8° of ETRA increase was the threshold of a positive LGDT sign. In summary, LGDT was proved to be a valid and accessible diagnostic tool for PLRI of the knee joint.
Lateral Gutter Drive‐Through Test is an Adjunctive Tool to Predict the Outcome of Posterolateral Corner and Posterior Cruciate Ligament Surgery
To our knowledge, there is no study on the application of the LGDT sign in the postoperative evaluation of combined PCL and PLC injury. Our hypothesis was proved to be correct in the present study. Consistent with the preoperative diagnostic findings, our results demonstrated that the LGDT test was still a reliable method with 100% sensitivity and 88.4% specificity for postoperative evaluation. Furthermore, the positive LGDT sign subgroup had inferior clinical outcome with tripled SSD of PTT, significantly higher SSD of ER, nearly 20% decrease in the Lysholm score, 30% decrease in the IKDC subjective score, and 50% decrease in the Tegner score.
In the present study, there were 11 LGDT‐positive cases. Among them, 6 cases with SSD of ER > 10° were successfully recognized by dial test. There were still another 4 cases with negative dial tests but SSD of PTT > 10 mm (11.1 mm, 13.3 mm, 15.6 mm, 18.5 mm). According to our ROC curve analysis, the AUC of coupled SSD of PTT and ER was larger than that of single SSD of ER, indicating that a compromised PCL also altered the rotational biomechanics of the knee joint. Subsequently, the tension of proximal PT was assumed to decrease and lead to positive LGDT. The assumption was supported by cadaveric biomechanical studies.19, 20, 21, 22, 23, 24 Li et al.24 reported that under 400 N of quadriceps load, after resection of PCL, the external rotation angle was significantly increased by 3.5° at 30° of knee flexion. From above, the knee joint of patients with PCL residual laxity may have increased the external rotation and subsequently led to a positive LDGT test. Therefore, according to our findings, the LGDT test seemed to provide more information than the dial test in detecting objective suboptimal cases in the first place.
Furthermore, it should be noted that, among the 6 patients with positive dial tests, 4 were upper borderline values (10.1°, 10.2°, 10.6°, 12.3°), while among the 4 dial‐test‐negative cases with positive LDGT sign, 2 were lower borderline values (8.0°, 9.0°). Given the nature of the dial test, which relies on the force and experience of the examiner, and according to the literature,25 if a repeated measure difference is lower than 8°, the difference is likely due to measurement error. Therefore, the interpretation of the six borderline values of ER may be susceptible. As well as the dial test, the LGDT test should be incorporated for a more comprehensive assessment.8 In the present study, all of the abovementioned 6 borderline cases were identified with positive LGDT sign. Comparing with LGDT‐negative cases, the Lysholm score (61.7 ± 8.6 vs 75.8 ± 15.0), the Tegner score (1.3 ± 0.5 vs. 1.4 ± 0.5), and the IKDC score (56.2 ± 15.4 vs. 83.2 ± 8.7) were lower in the 6 cases. Therefore, under the circumstances of borderline values of ER, the LGDT test was proved effective in identifying subjective suboptimal cases. As a result, the LGDT test may be used as an adjunctive tool to predict the outcome of combined PLC and PCL surgery.
There was 1 case with positive LGDT test but measured with 6° SDD of ER and 9.9 mm SSD of PTT in our series. This existence of the false‐positive phenomenon was consistent with a previous article on LGDT7 showing the rate of false‐positive cases was 4.3%.
Strengths of the Study
The strength of the study was: (i) the prospective design with high follow‐up rate (98.0%); and (ii) the objective evaluations (dial test, PTT, and lateral compartment opening measurement under stress radiograph) were all performed under anesthesia before the hardware removal procedure, providing a more accurate assessment after PCL and PLC surgery.
Limitations of the Study
There were some limitations in the present study. First, the second‐look arthroscopy was an invasive procedure which would limit the clinical application. Second, the sample size was relatively small. Although the study was not underpowered, the number of positive LGDT cases was only 11. Moreover, because this was a retrospective study, the choice of technique was based on several factors, such as the surgeon's preference, the characteristics of the injury, the concomitant lesions, and patients’ activity level and demand. This heterogeneity of surgical technique was another limitation of the present study. Finally, the LGDT test was not fully standardized by the force and direction of scope advancement.
Conclusion
This study demonstrated that in the series of surgically treated patients with PCL and PLC injury, according to the second‐look arthroscopic LGDT sign testing, subjective evaluation and EUA results: (i) patients had improved subjective and objective clinical outcomes after combined PCL reconstruction and PLC surgery at a minimum of 24‐months’ follow‐up; and (ii) the LGDT sign could be used as an adjunctive assessment of postoperative PLRI with high sensitivity and specificity and patients with a positive LGDT sign had inferior clinical outcome compared with patients with a negative LGDT sign.
Grant Sources: The study was sponsored by the Beijing Natural Science Foundation (7194276) and Beijing Municipal Administration of Hospitals Ascent Plan (DFL20180402).
Disclosure: The authors declare no conflict of interest.
References
- 1. Chahla J, James EW, Cinque ME, LaPrade RF. Midterm outcomes following anatomic‐based popliteus tendon reconstructions. Knee Surg Sports Traumatol Arthrosc, 2018, 26: 812–818. [DOI] [PubMed] [Google Scholar]
- 2. Domnick C, Frosch KH, Raschke MJ, et al Kinematics of different components of the posterolateral corner of the knee in the lateral collateral ligament‐intact state: a human cadaveric study. Art Ther, 2017, 33: 1821–1830 e1821. [DOI] [PubMed] [Google Scholar]
- 3. Lee DY, Park YJ, Kim DH, et al The role of isolated posterior cruciate ligament reconstruction in knees with combined posterior cruciate ligament and posterolateral complex injury. Knee Surg Sports Traumatol Arthrosc, 2018, 26: 2669–2678. [DOI] [PubMed] [Google Scholar]
- 4. Yoon KH, Lee SH, Park SY, Park SE, Tak DH. Comparison of anatomic posterolateral knee reconstruction using 2 different popliteofibular ligament techniques. Am J Sports Med, 2016, 44: 916–921. [DOI] [PubMed] [Google Scholar]
- 5. Moulton SG, Geeslin AG, LaPrade RF. A systematic review of the outcomes of posterolateral corner knee injuries, part 2: surgical treatment of chronic injuries. Am J Sports Med, 2016, 44: 1616–1623. [DOI] [PubMed] [Google Scholar]
- 6. Fanelli GC. Evaluation and treatment of posterolateral instability of the knee. Sports Med Arthrosc Rev, 2015, 23: 1. [DOI] [PubMed] [Google Scholar]
- 7. Feng H, Song GY, Shen JW, Zhang H, Wang MY. The "lateral gutter drive‐through" sign revisited: a cadaveric study exploring its real mechanism based on the individual posterolateral structure of knee joints. Arch Orthop Trauma Surg, 2014, 134: 1745–1751. [DOI] [PubMed] [Google Scholar]
- 8. Shen J, Zhang H, Lv Y, et al Validity of a novel arthroscopic test to diagnose posterolateral rotational instability of the knee joint: the lateral gutter drive‐through test. Art Ther, 2013, 29: 695–700. [DOI] [PubMed] [Google Scholar]
- 9. Feng H, Zhang H, Hong L, Wang XS, Zhang J. The "lateral gutter drive‐through" sign: an arthroscopic indicator of acute femoral avulsion of the popliteus tendon in knee joints. Art Ther, 2009, 25: 1496–1499. [DOI] [PubMed] [Google Scholar]
- 10. Zhang H, Hong L, Wang XS, et al Single‐bundle posterior cruciate ligament reconstruction and mini‐open popliteofibular ligament reconstruction in knees with severe posterior and posterolateral rotation instability: clinical results of minimum 2‐year follow‐up. Art Ther, 2010, 26: 508–514. [DOI] [PubMed] [Google Scholar]
- 11. Feng H, Zhang H, Hong L, Wang XS, Cheng KB, Zhang J. Femoral peel‐off lesions in acute posterolateral corner injuries: incidence, classification, and clinical characteristics. Art Ther, 2011, 27: 951–958. [DOI] [PubMed] [Google Scholar]
- 12. Geeslin AG, LaPrade RF. Outcomes of treatment of acute grade‐III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am, 2011, 93: 1672–1683. [DOI] [PubMed] [Google Scholar]
- 13. Fanelli GC, Larson RV. Practical management of posterolateral instability of the knee. Art Ther, 2002, 18: 1–8. [DOI] [PubMed] [Google Scholar]
- 14. Zhang H, Zhang J, Liu X, et al In vitro comparison of popliteus tendon and popliteofibular ligament reconstruction in an external rotation injury model of the knee: a cadaveric study evaluated by a navigation system. Am J Sports Med, 2013, 41: 2136–2142. [DOI] [PubMed] [Google Scholar]
- 15. Zhang H, Feng H, Hong L, Wang XS, Zhang J. Popliteofibular ligament reconstruction for posterolateral external rotation instability of the knee. Knee Surg Sports Traumatol Arthrosc, 2009, 17: 1070–1077. [DOI] [PubMed] [Google Scholar]
- 16. Feng H, Hong L, Geng XS, Zhang H, Wang XS, Zhang J. Posterolateral sling reconstruction of the popliteus tendon: an all‐arthroscopic technique. Art Ther, 2009, 25: 800–805. [DOI] [PubMed] [Google Scholar]
- 17. Noyes FR, Barber‐Westin SD. Posterolateral knee reconstruction with an anatomical bone‐patellar tendon‐bone reconstruction of the fibular collateral ligament. Am J Sports Med, 2007, 35: 259–273. [DOI] [PubMed] [Google Scholar]
- 18. Zorzi C, Alam M, Iacono V, Madonna V, Rosa D, Maffulli N. Combined PCL and PLC reconstruction in chronic posterolateral instability. Knee Surg Sports Traumatol Arthrosc, 2013, 21: 1036–1042. [DOI] [PubMed] [Google Scholar]
- 19. Strobel MJ, Schulz MS, Petersen WJ, Eichhorn HJ. Combined anterior cruciate ligament, posterior cruciate ligament, and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Art Ther, 2006, 22: 182–192. [DOI] [PubMed] [Google Scholar]
- 20. Apsingi S, Nguyen T, Bull AM, Unwin A, Deehan DJ, Amis AA. The role of PCL reconstruction in knees with combined PCL and posterolateral corner deficiency. Knee Surg Sports Traumatol Arthrosc, 2008, 16: 104–111. [DOI] [PubMed] [Google Scholar]
- 21. Khanduja V, Somayaji HS, Harnett P, Utukuri M, Dowd GS. Combined reconstruction of chronic posterior cruciate ligament and posterolateral corner deficiency. A two‐ to nine‐year follow‐up study. J Bone Joint Surg Br, 2006, 88: 1169–1172. [DOI] [PubMed] [Google Scholar]
- 22. Fanelli GC, Edson CJ. Combined posterior cruciate ligament‐posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2‐ to 10‐year follow‐up. Art Ther, 2004, 20: 339–345. [DOI] [PubMed] [Google Scholar]
- 23. Kennedy NI, Wijdicks CA, Goldsmith MT, et al Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med, 2013, 41: 2828–2838. [DOI] [PubMed] [Google Scholar]
- 24. Li G, Gill TJ, DeFrate LE, Zayontz S, Glatt V, Zarins B. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads‐‐an in vitro experimental study. J Orthop Res, 2002, 20: 887–892. [DOI] [PubMed] [Google Scholar]
- 25. Krause DA, Levy BA, Shah JP, Stuart MJ, Hollman JH, Dahm DL. Reliability of the dial test using a handheld inclinometer. Knee Surg Sports Traumatol Arthrosc, 2013, 21: 1011–1016. [DOI] [PubMed] [Google Scholar]


