Abstract
Objectives
To analyze the curative effect of TiRobot surgical robotic navigation and location system‐assisted percutaneous sacroiliac screw fixation and percutaneous sacroiliac screw by traditional fluoroscopy, and to summarize the safety and benefits of TiRobot.
Methods
A total of 91 patients with pelvic posterior ring fractures from December 2015 to February 2018 were included in this study. According to the surgical methods selected by the patients, the patients were divided into a TiRobot surgical robotic navigation and location system group (TiRobot group) and a percutaneous sacroiliac screw fixation group (traditional group). Statistical indicators included the number of sacroiliac screws, the time of planning the sacroiliac screw path, fluoroscopy frequency, fluoroscopy time, operation time, length of incision, blood loss, anesthesia time, the healing process of skin incisions, and fracture healing time. Fracture reduction was evaluated according to the maximum displacement degree at the inlet and outlet view X‐ray or CT. Matta standard was used to evaluate fracture reduction. At the last follow‐up, the Majeed function system was used to evaluate the function.
Results
All patients were followed up for 8 to 32 months. A total of 66 sacroiliac screws were implanted in the TiRobot group. A total of 43 sacroiliac screws were implanted in the traditional group. There were statistically significant differences in terms of fluoroscopy frequency, fluoroscopy time, operation time, incision length, anesthesia time, and blood loss between the two groups; the TiRobot group was superior to the traditional group. The healing time of the TiRobot group and the traditional group was 4.61 ± 0.68 months (range, 3.5–6.3 months) and 4.56 ± 0.78 months (range, 3.4–6.2 months), respectively, and there was no statistical difference. Postoperatively, by Matta standard, the overall excellent and good rate of fracture reduction was 89.28% and 88.57%, respectively. At the last follow‐up, by Majeed function score, the overall excellent and good rate was 91.07% and 91.43%. There was no statistical difference between the two groups.
Conclusion
Sacroiliac screw implantation assisted by TiRobot to treat the posterior pelvic ring fractures has the characteristics of less trauma, shorter operation time, and less blood loss. TiRobot has the characteristics of high safety and accuracy and has great clinical application value.
Keywords: TiRobot, Percutaneous screw, Sacroiliac joint, Sacrum, Pelvis
Introduction
Pelvic injuries are mostly caused by high‐energy injuries. Davarinos (2012) found that traffic injuries account for 72.4% and high‐fall injuries account for 27.6% of pelvic injuries1. Unstable pelvic fractures are associated with multiple injuries and hemodynamic instability, with a death rate of 21.4%2, 3, 4. The incidence of unstable posterior pelvic ring injury was 17%–30%5. After the rescue treatment, the surgical treatment had a significant effect on the functional recovery of pelvic fracture patients6. However, pelvic fractures are difficult to treat. Poor reduction and malunion are common complications, and may lead to pain, claudication, discrepancy in limb length, and other malformations; if nerve damage occurs, the consequences are serious7, 8, 9, 10, 11, 12. Effective fixation of the pelvic posterior ring injury can restore the integrity and biomechanical stability of the pelvic ring, as well as facilitate the treatment of other injured parts. However, reasonable surgical methods should be selected for different types of pelvic fractures13. Previous surgical methods involved techniques using sacrum rods, anterior plates, posterior plates, and sacroiliac screws6, 14, 15, 16, 17, 18, 19, 20, 21. The sacrum bar is largely disused due to its poor biomechanics14. Anatomic reduction can be achieved using an anterior plate under direct vision, but the trauma is large, the risk of infection is high, and the nerves are at higher risk of injury15. At the same time, because of the narrow fixation area of the medial sacral wing, only one screw can be fixed, the strength is poor, and the patient cannot bear a load early. The biomechanical stability of the posterior plate fixation is worse than that of the spinal internal fixation system, and there is considerable trauma and bleeding. As a result of the above reasons, the clinical application of anterior and posterior plates is less frequent at present10, 12, 15, 22.
At present, percutaneous sacroiliac screw fixation has become the optimal surgical method for the treatment of pelvic posterior ring fractures due to its advantage of little invasion19, 23. However, because of the complex structure, including the involvement of important blood vessels and nerves of the sacroiliac joint and sacrum, percutaneous sacroiliac screw fixation has the risk of frequent X‐rays, great radiation exposure, long operation time, high screw position error rate, and even nerve injury10, 11, 24. Determining how to treat pelvic fractures effectively in a minimally invasive fashion is the difficulty and the emphasis of current research11, 20. The era of robot‐assisted artificial intelligence surgery has been entered. Computer‐assisted orthopaedic surgery (CAOS) has been widely used in joint surgery, spine surgery, and orthopaedic trauma surgery. Therefore, the author retrospectively analyzed the data of patients with posterior pelvic ring fractures and dislocations who were treated with sacroiliac screw implantation assisted by the TiRobot surgical robotic navigation and location system, and compared the data with that of traditional percutaneous sacroiliac screw fixation. The aim of this study is to (i) analyze the safety and benefits of the technique; (ii) propose matters needing attention; and (iii) summarize the existing problems and the possible direction for further improvement.
Materials and Methods
Inclusion and Exclusion Criteria
Inclusion criteria: (i) patients with pelvic posterior ring fracture (sacral fracture and sacroiliac joint fracture dislocations); (ii) patients who were treated with the fixation method assisted by the TiRobot surgical robotic navigation and location system or percutaneous sacroiliac screw fixation without TiRobot; (iii) the main evaluation indicators include number of sacroiliac screws, the time of planning the sacroiliac screw path, fluoroscopy frequency, and fluoroscopy time; and (iv) prospective study.
Exclusion criteria: (i) preoperative vital signs were unstable and the time from injury to operation was more than 3 weeks; (ii) the patient refused surgery; (iii) patients with lower limb shaft fracture; (iv) patients with pre‐injury mobility dysfunction; (v) patients with central nervous system disorders or mental disorders; and (vi) preoperative imaging suggesting sacral dysmorphism.
Participants
Referring to inclusion and exclusion criteria, a total of 91 patients with pelvic fractures from December 2015 to February 2018 were included in this study. All patients were fully informed of their condition and treatment, and patients chose the treatment plan and signed the operation consent. According to the surgical method selected by the patient, the patients were divided into the TiRobot surgical robotic navigation and location system group (TiRobot group) and the percutaneous sacroiliac screw fixation group (traditional group). There were 56 patients in the TiRobot group and 35 patients in the traditional group.
There were 32 females and 24 males in the TiRobot group, and the age of these patients were range from 22 to 50 years. According to AO classification there were: 21 type B cases and 35 type C cases. The mechanisms of injury were traffic accident in 39 cases, falling down in 14 cases, and weight crushing in 3 cases. There were 40 patients with combined injury and 33 cases of shock at admission. The preoperative time was 3–18 days. There were 21 women and 14 men in the traditional group; the age of these patients ranged from 20 to 50 years. According to AO classification there were: 15 type B cases and 20 type C cases. The mechanisms of injury were traffic accident in 15 cases, falling down in 19 cases and weight crushing in 1 case. There were 26 patients with combined injury and 19 cases of shock at admission. The preoperative time was 4–14 days. This study was approved by the ethics committee.
Preoperative Preparation
The patients were treated according to the strategy of damage control after admission. The femoral supracondylar bone traction was performed in patients with pelvic vertical instability. To determine fracture type and displacement, preoperative examinations were completed, including radiograph of pelvis inlet view and outlet view, CT, and 3‐D reconstruction images. Patients with stable vital signs were treated with surgery, blood was prepared before surgery, and antibiotics were used 30 min before surgery to prevent infection. The TiRobot surgical robotic navigation and location system is the third generation of surgical robot by Beijing TINAVI Medical Technologies. (Model: GD‐2000, Beijing, China). The fluoroscopy equipment used was the Ziehm mobile C‐arm X‐ray machine (Ziehm8000, Nuremberg, Germany).
Operation Method of Percutaneous Sacroiliac Screw with TiRobot Assistance
The operation mode was uniform and standardized. General anesthesia is administered and the patient lies on a traction bed in dorsal position.
Device Connection and Skin Disinfection
The equipment was placed and connected; then the skin on the pelvis was sterilized. The anterior superior iliac spine of the opposite side should be exposed in the operative area. The surgeon placed a tracer on the opposite side of the anterior superior iliac spine. A sterile C‐type arm sleeve was placed on the mechanical arm and a positioning device was connected.
Fluoroscopy
Then C‐arm X‐ray machine fluoroscopy is used for pelvis inlet and outlet view, making sure all 10 markers on the positioning device are clearly visible. The position and order of all the markers were confirmed by X‐ray at the inlet and outlet view in the computer operating system.
Surgical Planning and Mechanical Arm Movement
Surgical planning was carried out based on the inlet and outlet view to design the percutaneous sacroiliac screw point, angle, and length. Method: Replace the positioning device with the pilot sleeve and simulate the movement of the manipulator arm in the computer operating system; after confirming that the movement process and direction are correct, click “movement” on the operation interface of the computer operating system; the manipulator arm moves the pilot sleeve to the surface 3 cm away from the skin according to the planned path, which is the percutaneous sacroiliac screw entry point and angle.
Screw‐setting
The surgeon made an incision approximately 1–2 cm long at the location skin, separated the fascia and muscles, and inserted the Kirschner wire along the pilot sleeve; the length exceeded the midline of the sacrum. The surgeon measured the length, inserted the sacroiliac screw along the Kirschner wire, pulled out the Kirschner wire, and washed the incision before suture. The screw position was confirmed by C‐arm X‐ray machine.
Operation Method of Percutaneous Sacroiliac Screw without TiRobot Assistance
Surgical Position and Anesthesia
The skin incision was marked approximately 1 cm below the posterior superior iliac spine and 4–5 cm laterally. General anesthesia is administered, with the patient lying on a traction bed in dorsal position.
Fluoroscopy and Insert Kirschner Wire
C‐arm fluoroscopy to confirm the vertical displacement was corrected; a small incision was made, which was approximately 2 cm long at the mark points. The fascia and muscles were separated, before inserting the Kirschner wire, inclined forward 30°–50° above the sacral foramina and the 1/3 in sacral, slowly through the ilium and sacroiliac joint into the S1 vertebral body.
Screw‐setting
The sacroiliac screw was inserted after fluoroscopy to confirm the correct position of the guide needle, then the needle was pulled out and rinsed after suture of incision.
Postoperative Management
Patients were provided symptomatic treatment, nutritional support, infection prevention, and electrolyte balance. Review was undertaken of the pelvic inlet and outlet X‐ray or CT. According to the actual situation of the patient, early functional exercise is carried out under the guidance of the Physiatrician. After the operation, the patient began isometric exercise of both lower limbs; 3–5 days after the operation, the patient started to roll over in bed with the assistance of family and practiced hip and knee flexion gradually. It is important to pay attention to the prevention of phlebothrombosis, pneumonia, pressure sores, and other complications.
Main Outcome Measures
The main statistical indicators are shown as follows.
Time of Planning Sacroiliac Screw Path
In the TiRobot group, the time of planning the sacroiliac screw path was from the beginning of fluoroscopy until the time of mechanical arm movement to the correct direction and insertion point. It represents the preparation time required under the assistance of the TiRobot and also reflects the proficiency of the operator in using the TiRobot.
Fluoroscopy Frequency
The number of intraoperative fluoroscopy images taken includes the sum of the number of pelvic inlet position, the outlet position, and the lateral position images. It can reflect the proficiency and accuracy of the operator, as well as the radiation exposure of the operator and the patient.
Fluoroscopy Time
The time of each intraoperative fluoroscopy was added, including the fluoroscopy for preoperative positioning and the fluoroscopy for verifying the correct position of the screw placement after screw‐setting. It can reflect the proficiency and accuracy of the operator, as well as the radiation exposure of the operator and the patient.
Blood Loss
Blood loss is the sum of the amount of blood through the suction apparatus and the bleeding volume at the gauzes. Similar to the length of incision, it can reflect the extent of the operation trauma.
Fracture Reduction Standard
Fracture reduction was evaluated according to the maximum displacement degree at the inlet and outlet view for X‐ray or CT. Matta standard25 was adopted: displacement less than 4 mm was excellent, displacement 4–10 mm was good, displacement 10–20 mm was general, and displacement greater than 20 mm was poor.
Functional Recovery Standard
At the last follow‐up, the Majeed function system was used to evaluate the function from five aspects: pain, work, standing, sitting, and sexual life26. The full score was 100 points, and score >85 points was excellent, 70–84 points was good, 55–69 points was general, and <55 points was poor.
Other indicators include the operation time, length of incision, anesthesia time, the number of sacroiliac screws, and the fracture healing time.
Statistical Method
All data were processed using SPSS 17.00 (SPSS, Chicago, IL, USA). The measurement data includes fluoroscopy frequency, fluoroscopy time, operation time, length of incision, blood loss, anesthesia time, the healing process of skin incisions, and fracture healing time; all of these were expressed as (mean ± standard deviation) and the t test was used to compare the measurement data between the two groups. The χ2 test or Fisher's exact test were used for the comparison of enumeration data, which includes the excellent and good cases of the Matta score and the Majeed function system. Significant level α = 0.05.
Results
General Results
All patients were followed up for 8 to 32 months. In the TiRobot group, the age was 35.95 ± 7.75 years (range, 22–50 years) and the preoperative time was 9.61 ± 3.23 days (range, 3–18 days). In the traditional group, the age was 35.68 ± 8.37 years (range, 20–50 years) and the preoperative time was 9.71 ± 2.14 days (range, 4–14 days). There was no statistical difference in general data between the two groups (Table 1).
Table 1.
Comparison of the general data between the two groups
| Variables | Cases | Age/yr. | Male/Female (case) | Preoperative time (d) | Type (B/C) (case) | Combined injury (case) | Shock (case) |
|---|---|---|---|---|---|---|---|
| TiRobot group | 56 | 35.95 ± 7.75* | 32/24 | 9.61 ± 3.23* | 21/35 | 40 | 33 |
| Traditional group | 35 | 35.68 ± 8.37* | 21/14 | 9.71 ± 2.14* | 15/20 | 26 | 19 |
| t | 0.909 | 0.072 | 0.544 | 0.259 | 0.088 | 0.190 | |
| P | 0.364 | 0.788 | 0.587 | 0.611 | 0.766 | 0.663 |
Note:
, mean ± standard deviation
A total of 66 sacroiliac screws were implanted in the TiRobot group and 43 sacroiliac screws were implanted in the traditional group. The time for planning the sacroiliac screw path was 6.71 ± 4.19 min (range, 3–26 min), which reflects the operator's proficiency with the TiRobot.
Fluoroscopy Frequency
The fluoroscopy frequency was 8.49 ± 2.37 (range, 4–15) times in the TiRobot group and 18.67 ± 4.18 (range, 11–26) times in the traditional group. The t test value is 46.105 and the P value is 0.000; there was statistically significant difference between the two groups (P < 0.05); the fluoroscopy frequency in the TiRobot group was less than in the traditional group. This means less radiation exposure for both the surgeon and the patient.
Fluoroscopy Time
The fluoroscopy time was 5.88 ± 1.29 min (range, 3.3–8.2 min) in the TiRobot group and 11.05 ± 2.98 min (range, 5.9–17.3 min) in the traditional group. The t test value is 28.384 and the P value is 0.000; there was statistically significant difference between the two groups (P < 0.05); the fluoroscopy time was less in the TiRobot group than in the traditional group. As well as the fluoroscopy frequency, it means less radiation exposure for both the surgeon and the patient.
Operation Time
The operation time was 33.25 ± 6.46 min (range, 19–51 min) in the TiRobot group and 63.55 ± 6.62 min (range, 50–83 min) in the traditional group. The t test value is 25.707 and the P value is 0.000; there was statistically significant difference between the two groups (P < 0.05) and the operation time was shorter in the TiRobot group than in the traditional group.
Length of Incision
The length of incision was 1.49 ± 0.21 cm (range, 1.0–1.9 cm) in the TiRobot group and 2.22 ± 0.49 cm (range, 1.5–3.6 cm) in the traditional group. The t test value is 11.802 and the P value is 0.000; there was statistically significant difference between the two groups (P < 0.05) and the length of incision was shorter in the TiRobot group than in the traditional group. This suggests less damage to patients and less risk of infection.
Blood Loss
The blood loss was 33.89 ± 16.4 mL (range, 15–80 mL) in the TiRobot group and 43.04 ± 12.34 mL (range, 30–80 mL) in the traditional group. The t test value is 17.356 and the P value is 0.000; there was statistically significant difference between the two groups (P < 0.05) and the blood loss was lower in the TiRobot group than in the traditional group. As well as the length of incision, this suggests less damage to patients and the use of TiRobot being more conducive to postoperative recovery.
Anesthesia Time
The anesthesia time was 43.54 ± 6.69 min (range, 30–60 min) in the TiRobot group and 75.18 ± 6.87 min (range, 30–80 min) in the traditional group. The t test value is 164.522 and the P value is 0.000; there was statistically significant difference between the two groups (P < 0.05) and the anesthesia time was shorter in the TiRobot group than in the traditional group. This suggests that the risk is lower and recovery may be faster.
Wound and Fracture Healing Results
The wounds healed well in both groups. All the sacroiliac screw positions were satisfactory in the TiRobot group. Postoperative CT indicated that 1 case had been cut by the screw in the sacral canal in the traditional group, but no neurological damage had occurred.
All fractures in both groups healed well; the healing time of the TiRobot group and the traditional group was 4.61 ± 0.68 months (range, 3.5–6.3 months) and 4.56 ± 0.78 months (range, 3.4–6.2 months). The t test value is 0.629 and the P value is 0.530; there was no statistical difference (P > 0.05) (Table 2).
Table 2.
Comparison of intraoperative and postoperative results between the two groups (mean ± standard deviation)
| Variables | Cases | Fluoroscopy frequency | Fluoroscopy time (min) | Operation time (min) | Length of incision (min) | Anesthesia time (min) | Blood loss (mL) | Fracture heal‐ ing time (m) |
|---|---|---|---|---|---|---|---|---|
| TiRobot group | 56 | 8.49 ± 2.37 | 5.88 ± 1.29 | 33.25 ± 6.46 | 1.49 ± 0.21 | 43.54 ± 6.69 | 33.89 ± 16.4 | 4.61 ± 0.68 |
| Traditional group | 35 | 18.67 ± 4.18 | 11.05 ± 2.98 | 63.55 ± 6.62 | 2.22 ± 0.49 | 75.18 ± 6.87 | 43.04 ± 12.34 | 4.56 ± 0.78 |
| t | 46.105 | 28.384 | 25.707 | 11.802 | 164.522 | 17.356 | 0.629 | |
| P | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.530 |
Matta Standard Results
Matta standard: There were 48 excellent cases (Figs 1 and 2), 2 good cases (Fig. 3), 6 general cases, and 0 poor cases in the TiRobot group; the overall excellent and good rate was 89.28%. There were 28 excellent cases, 3 good cases, 4 general cases, and 0 poor cases in the traditional group; the overall excellent and good rate was 88.57%. There was no statistical difference between the two groups.
Figure 1.
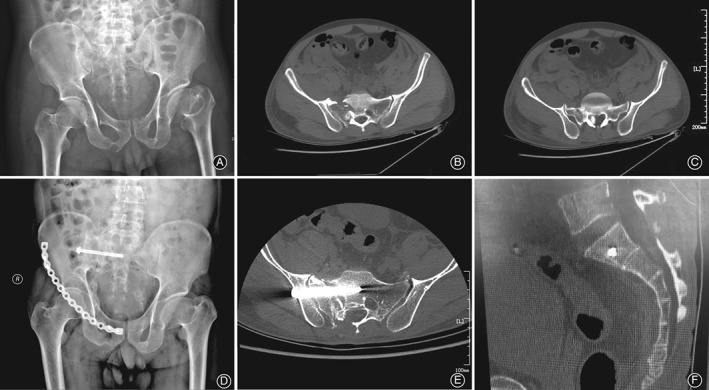
The patient was a 42‐year‐old man. Preoperative pelvic X‐ray (A) showed both pubic rami fracture and acetabular fracture, left acetabular dysplasia, the femoral neck, which is shorter than the contralateral, and the sacral fracture, which involves the sacral foramen. Preoperative CT (B, C) showed sacral fracture involving the sacral foramen and canal, and the bone fragment was displaced into the sacral canal. The postoperative X‐ray (D) and CT (E, F) showed that the sacroiliac screw position is good and the bone fragment had been removed.
Figure 2.
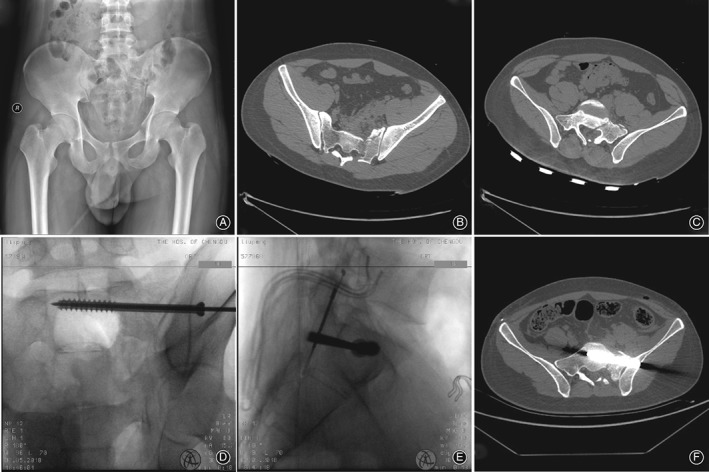
The patient was a 22‐year‐old man, with a pelvic fracture caused by falling down. Preoperative pelvic X‐ray (A) showed both pubic rami fracture and sacral fracture, and the left sacroiliac joint dislocation. Preoperative CT (B, C) showed sacral fracture involving the sacral foramen and canal, and the left sacroiliac joint dislocation. Intraoperative X‐ray (D, E) showed the sacroiliac screw implantation assisted by TiRobot. The postoperative CT (F, G) showed that the sacroiliac screw position is excellent.
Figure 3.
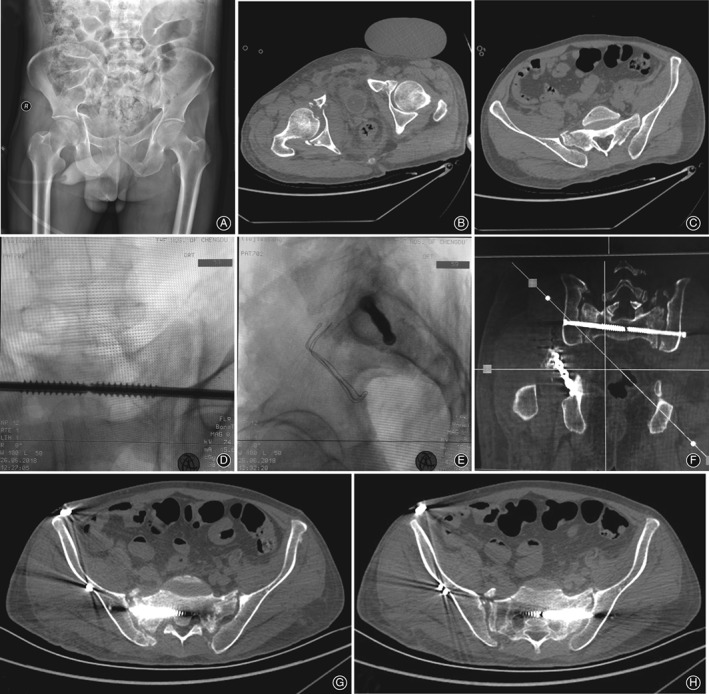
The patient was a 53‐year‐old man, pelvic fracture caused by heavy objects squeezing, concomitant hemorrhagic shock, left clavicle fracture, right humerus surgical neck comminuted fracture, flail chest, bilateral multiple rib fractures, and lung and kidney contusion. Preoperative pelvic X‐ray (A) and CT (B, C) showed that the right acetabular fracture, sacral fracture. Intraoperative X‐ray (D, E) showed the sacroiliac screw implantation assisted by TiRobot. The postoperative CT (F, G, H) showed that the sacroiliac screw position is good.
Majeed Function Score Results
At the last follow‐up, there were 49 excellent cases, 2 good cases, 5 general cases, and 0 poor cases in the TiRobot group; the overall excellent and good rate was 91.07%. There were 30 excellent cases, 2 good cases, 3 general cases, and 0 poor cases in the traditional group; the overall excellent and good rate was 91.43%. There was no statistical difference between the two groups (Table 3).
Table 3.
Comparison of functional evaluation between the two groups
| Variables | Cases | Matta standard (case) | Majeed function score (case) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Excellent | Good | General | Poor | Excellent | Good | General | Poor | ||
| TiRobot group | 56 | 48 | 2 | 6 | 0 | 49 | 2 | 5 | 0 |
| Traditional group | 35 | 28 | 3 | 4 | 0 | 30 | 2 | 3 | 0 |
| χ2 | 0.011 | 0.003 | |||||||
| P | 0.916 | 0.953 | |||||||
Discussion
The Advantages of TiRobot Over Traditional Surgical Techniques
Biomechanical studies confirmed that the stability of the anterior and posterior pelvic rings accounted for 40% and 60%27, 28, 29, 30. The stability of the posterior pelvic ring is maintained by the sacroiliac joint complex, which is composed of the bilateral ilium, the sacrum, the sacroiliac joint, and the surrounding ligaments; it also plays an important role in the stability of the pelvic ring21. With the development of minimally invasive surgery, imaging equipment and technology, sacroiliac screw fixation is the most commonly used method for the treatment of posterior pelvic ring injuries due to its central fixation and stable biomechanical properties19, 31, 32, 33, 34. Iorio et al. 7 believed that percutaneous sacroiliac screw internal fixation was suitable for the treatment of unstable posterior pelvic ring injuries, sacral fractures, sacroiliac joint fractures, and dislocation. It has the advantages of less surgical trauma, shorter operation time, fewer complications, faster recovery, and satisfactory curative effect. However, due to the special anatomical structure of the posterior pelvic ring and the numerous influencing factors during C‐arm fluoroscopy, repeated fluoroscopy is often required to confirm the anatomical structure and screw position35; there is risk of great radiation exposure, long operation times, a high screw position error rate, and even nerve injury10, 11, 31, 33. Factors such as the size of the patient and intestinal contents also affect the results36, 37. There is often variation in the sacrum, with a reported rate of 20%, which can also lead to screw misalignment. Gautier et al. 38 reported that the failure rate of sacroiliac screw implantation was 2%–13%. Ecker et al. 39 believed that preoperative determination of the nail entry point and angle was conducive to increasing the accuracy of the percutaneous sacroiliac screw, shortening the operation time, and minimizing the radiation exposure of patients and operators through cadavers’ studies. Studies have reported that both CT and C‐arm X‐ray machine‐guided placement of sacroiliac screws require repeated fluoroscopy, but CT further improved the accuracy of screw position40.
The core difficulty of traditional surgery lies in the limitations of the operator's field of vision and operation; surgical injury is inevitable. Due to the great difficulty and danger of surgery, the surgeon cannot see the internal structure, and cannot obtain real‐time 3D images of the surgical site during the operation, so there is a high risk of injury the surrounding tissue. Therefore, navigation technology has developed rapidly in orthopaedics in recent years to overcome the above disadvantages as far as possible41, 42, 43. However, the principle of navigation technology is to confirm the position of navigation tools by using the 2D images of multiple planes obtained during the operation, which have no 3D aspect and cannot be observed dynamically. In addition, there are many instruments and there is a lot of equipment in the navigation system, the operation is complex, and the cost is high. However, 3D navigation technology overcomes these shortcomings. It can not only achieve 3D imaging and real‐time imaging intraoperatively but also provides higher image quality and greater accuracy of screw placement42, 44. After analyzing the data of 2D and 3D navigation screw implantation in sacroiliac screws from four medical centers, Thakkar et al. 42 concluded that 3D navigation has obvious advantages in reducing the incidence of radiation dose exposure and the screw dislocation rate, improving accuracy45. At present, the navigation system is a photoelectric navigation system. Its advantages are conformed to suit doctors’ surgical habits, but doctors are still required to complete the operation by hand, so instability and imprecision of manual operation remain factors. Supported by the continuous development of science and technology, the concept of precision medicine and the technology of minimally invasive surgery continue to develop46, 47; surgery has entered the era of robot‐assisted artificial intelligence surgery.
The TiRobot surgical robotic navigation and location system is the third generation of surgical robot by Beijing TINAVI Medical Technologies, which is the latest generation of orthopaedic surgery robot systems independently developed in China and recognized internationally. The system adopts modular, miniaturization, and generalized design; positioning is accomplished through spatial mapping, surgical planning, and motion navigation. With the characteristics of being minimally invasive, precise, intelligent, and stable, its indication has been extended to spine surgery.
Compared with the traditional navigation system, TiRobot has the following differences. The first is that TiRobot can not only observe the change of the screw position in the sacrum bone in real time during the needle insertion process, but also timely observe the screw position deviation and prompt the surgeon to make adjustments, which has the ability of real‐time correction of screw position deviation in bone. The second is that the nailing path planning is carried out from the top according to the obtained image reconstructed by computer. TiRobot has the real‐time tracking function of an optical tracking system, which can monitor the movement of patients in real time through spatial positioning, and calculate the direction and size of the movement. Not only the injection point and direction can be adjusted in real time but also the length of the screw can be measured. The third is that the traditional navigation system requires manual nailing, and the operator's action control force is affected by many factors; the repeatability and stability error cannot be controlled.
In addition, TiRobot completes the path planning. Moving to the nail into position is a six‐axis, highly stable robotic arm; it realizes the navigation path and the surgeon does not need to look for the insertion point and angle; the error of traditional artificial nail placement is effectively avoided, and the accuracy and stability are greatly improved.
Finally, if the screw position is not satisfactory, TiRobot can be returned to the programming interface for path planning, without the need to collect images again.
Surgical Efficacy and Safety Analysis of TiRobot
In this study, there was no statistical difference in baseline data between the two groups. Because pelvic fractures are often combined with more injuries2, 3, 4, in terms of the timing of surgery, theoretically, the earlier the surgical reduction is, the easier it is. However, the earlier the operation is, the more bleeding there is and the greater the surgical risk. Connor et al. 48 believe that surgery is best performed within 1 week after injury. Percutaneous sacroiliac screw fixation can be performed after the hemodynamic stability of patients 48–72 h after injury due to its small incision trauma and bleeding. Early reduction and fixation are conducive to recovery. In this study, the earliest operation time was advanced to 3–4 days after injury, which is basically consistent with the reports in the literature.
The fluoroscopy frequency and the fluoroscopy time of the TiRobot group is significantly shorter than that of the traditional group. The traditional group requires repeated fluoroscopy during the operation to confirm the correct position. The results of this study are consistent with the results reported in other studies49. Compared with Wang50, who reported the time of sacroiliac screw under the navigation system, the TiRobot operation time is shorter; this may be associated with the reduced time for 3D scanning reconstruction. Once TiRobot gains excellent positioning images, it can be used as planning navigation image until a satisfactory planning path is obtained. Even if it is necessary to adjust the planning path, it can be returned to the programming interface without the need for perspective images. After accurate positioning, effective traction, and accurate reduction, TiRobot has a high success rate, which significantly reduces the frequency of fluoroscopy, greatly shortens the irradiation time, and reduces the damage of radiation to both doctors and patients. However, the time comparison between different studies cannot ignore the interference of the following factors: one is the proficiency of the operator and the tacit understanding of the operation team, the second is the type and severity of the fracture, and the third difference is the use of equipment50. The time of planning the sacroiliac screw path was 6.71 ± 4.19 min (range, 3–26 min), which is related to the surgeons’ inexperience, low proficiency, and poor coordination degree between team members in the early application of TiRobot. With experience, proficiency, and degree of tacit understanding of cooperation gradually increasing, the duration of operations can be significantly shortened.
In the TiRobot group, the operation time, the length of incision, the blood loss, and the anesthesia time are significantly shorter than in the traditional group. This is associated with the surgical mode of TiRobot. The TiRobot group cut the skin after the nail placement path planning was completed. Then the surgeon made an incision approximately 1–2 cm long, separated the fascia and muscles, inserted the Kirschner wire along the pilot sleeve, and inserted the sacroiliac screw along the Kirschner wire; the operation mode was “first look, then cut.” The operation time was short and the invasive operation time was short, so the blood loss was low. At the same time, TiRobot assistance can shorten the anesthesia time of patients. A study found that the infection rate after internal fixation of type C pelvic fractures was 3.4%12. In this study, there was no incisional infection, which may be related to abundant soft tissue and blood supply of the buttocks, small trauma, short operation time, and less bleeding.
Postoperative, Matta standard: The overall excellent and good rate was 89.28% in the TiRobot group and 88.57% in the traditional group. There was no statistical difference. This fully proves that the application of TiRobot to assist sacroiliac screw placement has the advantages of high accuracy and safety, strong operability, and repeatability. The author believes that good reduction is the key, and displacement greater than 1 cm can cause obvious dysfunction7.
Functional recovery after operation, Majeed function score: the overall excellent and good rate was 91.07% in the TiRobot group and 91.43% in the traditional group. There was no statistical difference. Meta‐analysis found that the superior rate of Majeed's pelvic fracture quantitative evaluation system was 88%–90% after follow up 15–33 months after the percutaneous sacroiliac screw fixation49; this is consistent with the results of this study. The author believes that the degree of comminuted and displaced fractures, whether combined with nerve injury and fracture of other parts of lower limbs, may also lead to different results among different studies. Further studies are needed to analyze and compare the effects of these factors on prognosis.
Key Technologies Used by TiRobot
TiRobot can provide accurate spatial positioning and stable path navigation, with a short operation time, excellent safety, and high efficiency. In the process of the operation, the author considers that the following key points should be noted:
Cleansing enema must be performed preoperatively and complete imaging examination is necessary to exclude sacral variation.
Sterile area protection and instrument protection: C arm sleeve is used to protect C‐arm and TiRobot. When using the tracer, attention must be paid to protect the reflective ball to avoid errors caused by friction.
Position protection: The tracer of the patient should be fixed reliably to ensure that the optical tracking camera can recognize the manipulator tracer and the patient tracer. After the ideal position of the TiRobot is determined, the protection of the ground support system should be turned on to prevent displacement. Slight changes in position may cause image errors and affect the accuracy of positioning.
Perspective points: Master the perspective angle and requirements of the standard pelvic inlet position, the outlet position, and the lateral position radiographs. The author suggests that the lateral images should be viewed first, and then the pelvic inlet and outlet X‐ray.
After the nailing path planning is completed, the motion simulation function is normally used to ensure the correct target position of the TiRobot.
When placing screws, the sleeve is close to the bone surface of the nail point. If it is found that the navigation path and the planning path have a large error, the linear motion can be selected for finetuning until the error is within the acceptable range.
Limitations of the research
There are some limitations in this study. TiRobot is a new technology in our institute and the number of cases included in the study was small. The above results are for early work, the follow‐up time was relatively short, and further experience needs to be gained in more clinical cases. Because the use of TiRobot is still in its infancy, we used single sacroiliac joint screw fixation in this study; the resistance shear and rotation were poor.
To sum up, sacroiliac screw implantation assisted by TiRobot to treat posterior pelvic ring fractures has the characteristics of being minimally invasive, safe, convenient, and accurate. In addition, it is a safe and effective method that reduces fluoroscopy frequency and radiation exposure in surgery. It is believed that with the further development of digital orthopaedics and precision medicine, more intelligent, safer, more accurate, more stable, and more convenient orthopaedics robotics will provide clinical services.
Grant Sources: This study was supported by the National Key R&D Program of China (No. 2016YFC0105806).
Disclosure: The present study was supported by the National Key Development Program of Digital Medical Equipment Research and Development Special Funding (grant 2016YFC0105806).
References
- 1. Davarinos N, Ellanti P, Morris S, Mc Elwain JP. Epidemiology of pelvic and acetabular trauma in a Dublin tertiary hospital: a 10‐year experience. Ir J Med Sci, 2012, 181: 243–246. [DOI] [PubMed] [Google Scholar]
- 2. Barrett K, Braga LH, Farrokhyar F, Davies TO. Primary realignment vs suprapubic cystostomy for the management of pelvic fracture–associated urethral injuries: a systematic review and meta‐analysis. Urology, 2014, 83: 924–929. [DOI] [PubMed] [Google Scholar]
- 3. Corrêa WO, Batista VGR, Júnior EFC, et al. Mortality predictors in patients with pelvic fractures from blunt trauma. Rev Col Bras Cir, 2017, 44: 222–230. [DOI] [PubMed] [Google Scholar]
- 4. Holstein JH, Culemann U, Pohlemann T, Working Group Mortality in Pelvic Fracture Patients . What are predictors of mortality in patients with pelvic fractures? Clin Orthop Relat Res, 2012, 470: 2090–2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dudda M, Hoffmann M, Schildhauer TA. Sacrum fractures and lumbopelvic instabilities in pelvic ring injuries: classification and biomechanical aspects. Unfallchirurg, 2013, 116: 972–978. [DOI] [PubMed] [Google Scholar]
- 6. Rommens PM, Ossendorf C, Pairon P, Dietz SO, Wagner D, Hofmann A. Clinical pathways for fragility fractures of the pelvic ring: personal experience and review of the literature. J Orthop Sci, 2015, 20: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Iorio JA, Jakoi AM, Rehman S. Percutaneous sacroiliac screw fixation of the posterior pelvic ring. Orthop Clin North Am, 2015, 46: 511–521. [DOI] [PubMed] [Google Scholar]
- 8. Shui X, Ying X, Mao C, et al. Percutaneous screw fixation of crescent fracture‐dislocation of the sacroiliac joint. Orthopedics, 2015, 38: e976–e982. [DOI] [PubMed] [Google Scholar]
- 9. Alvismiranda HR, Faridescorcia H, Alcalá Cerra G, Castellar‐Leones SM, Moscote‐Salazar LR. Sacroiliac screw fixation: a mini review of surgical technique. J Craniovertebr Junction Spine, 2014, 5: 110–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pavelka T, Salášek M, Weisová D. Complications associated with surgical treatment of pelvic ring fractures. Acta Chir Orthop Traumatol Cech, 2013, 80: 208–215. [PubMed] [Google Scholar]
- 11. Lindahl J, Hirvensalo E. Outcome of operatively treated type‐C injuries of the pelvic ring. Acta Orthop, 2009, 76: 667–678. [DOI] [PubMed] [Google Scholar]
- 12. Stover MD, Sims S, Matta J. What is the infection rate of the posterior approach to type C pelvic injuries? Clin Orthop Relat Res, 2012, 470: 2142–2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yoon HK, Oh HC, Park J, Oyunbat C, Kim T. Rupture of the deep femoral artery during proximal femoral nailing following an intertrochanteric fracture: a case report. Hip Pelvis, 2016, 28: 54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kanezaki S, Rommens PM. Bilateral nonunion of the sacrum in a long‐term paraplegic patient treated with trans‐sacral bar and spinopelvic fixation. Arch Orthop Trauma Surg, 2015, 135: 345–349. [DOI] [PubMed] [Google Scholar]
- 15. Mardanpour K, Rahbar M. The outcome of surgically treated traumatic unstable pelvic fractures by open reduction and internal fixation. J Inj Violence Res, 2013, 5: 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Acklin YP, Marco G, Sommer C. Double locking plate fixation of sacral fractures in unstable pelvic ring C‐type injuries. Oper Orthop Traumatol, 2015, 27: 74–79. [DOI] [PubMed] [Google Scholar]
- 17. Stiegervanegas SM, Senthirajah SK, Nemanic S, et al. Evaluation of the diagnostic accuracy of conventional 2‐dimensional and 3‐dimensional computed tomography for assessing canine sacral and pelvic fractures by radiologists, orthopedic surgeons, and veterinary medical students. Vet Surg, 2015, 44: 694–703. [DOI] [PubMed] [Google Scholar]
- 18. Oh HK, Choo SK, Kim JJ, Lee M. Stoppa approach for anterior plate fixation in unstable pelvic ring injury. Clin Orthop Surg, 2016, 8: 243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang L, Peng Y, Du C, Tang P. Biomechanical study of four kinds of percutaneous screw fixation in two types of unilateral sacroiliac joint dislocation: a finite element analysis. Injury, 2014, 45: 2055–2059. [DOI] [PubMed] [Google Scholar]
- 20. Wu XT, Liu ZQ, Fu WQ, Zhao S. Minimally invasive treatment of unstable pelvic ring injuries with modified pedicle screw‐rod fixator. J Int Med Res, 2018, 46: 368–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br, 2007, 89: 145–154. [DOI] [PubMed] [Google Scholar]
- 22. Bi C, Wang Q, Nagelli C, Wu J, Wang Q, Wang J. Treatment of unstable posterior pelvic ring fracture with pedicle screw‐rod fixator versus locking compression plate: a comparative study. Med Sci Monit, 2016, 22: 3764–3770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Le VH, Heckmann N, Jain N, et al. Biomechanical evaluation of supplemental percutaneous Lumbo‐Sacro‐iliac screws for Spino‐pelvic fixation following total sacrectomy. J Spinal Disord Tech, 2015, 28: E181–E185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Comai A, Zatelli M, Haglmuller T, Bonatti G. The role of transcatheter arterial embolization in traumatic pelvic hemorrhage: not only pelvic fracture. Cureus, 2016, 8: e722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hoskins W, Bucknill A, Wong J, et al. A prospective case series for a minimally invasive internal fixation device for anterior pelvic ring fractures. J Orthop Surg Res, 2016, 11: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Majeed SA. Grading the outcome of pelvic fracture. J Bone Joint Surg Br, 1989, 71: 304–306. [DOI] [PubMed] [Google Scholar]
- 27. Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg, 1996, 4: 143–151. [DOI] [PubMed] [Google Scholar]
- 28. Liu HC, Chen Y, Sang XG, Qi L. Management of lumbosacropelvic fracture‐dislocation using lumboiliac internal fixation. Injury, 2012, 43: 452–457. [DOI] [PubMed] [Google Scholar]
- 29. Shaath MK, Koury KL, Gibson PD, et al. Analysis of pelvic fracture pattern and overall orthopaedic injury burden in children sustaining pelvic fractures based on skeletal maturity. J Child Orthop, 2017, 11: 195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Grüneweller N, Raschke MJ, Zderic I, et al. Biomechanical comparison of augmented versus non‐augmented sacroiliac screws in a novel hemi‐pelvis test model. J Orthop Res, 2017, 35: 1485–1493. [DOI] [PubMed] [Google Scholar]
- 31. Mouhsine E, Garofalo R, Borens O, et al. Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury, 2005, 36: 1330–1336. [DOI] [PubMed] [Google Scholar]
- 32. Guimarães RP, de Góes Ribeiro A, Ulson O, de Ávila RB, Ono NK, Polesello GC. Supra‐acetabular fixation and sacroiliac screws for treating unstable pelvic ring injuries: preliminary results from 20 patients. Rev Bras Ortop, 2016, 51: 132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen HW, Liu GD, Fei J, et al. Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: a comparative study. J Orthop Sci, 2012, 17: 580–587. [DOI] [PubMed] [Google Scholar]
- 34. Giráldez‐Sánchez MA, Lázaro‐Gonzálvez Á, Martínez‐Reina J, et al. Percutaneous iliosacral fixation in external rotational pelvic fractures. A biomechanical analysis. Injury, 2015, 46: 327–332. [DOI] [PubMed] [Google Scholar]
- 35. Miller AN, Routt MLC. Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg, 2012, 20: 8–16. [DOI] [PubMed] [Google Scholar]
- 36. Kuo‐Ti P, Yen‐Yao L, Wei‐Hsiu H, et al. Intraoperative computed tomography with integrated navigation in percutaneous iliosacral screwing. Injury, 2013, 44: 203–208. [DOI] [PubMed] [Google Scholar]
- 37. Stockle U, Schaser K, Konig B. Image guidance in pelvic and acetabular surgery: expectations, success and limitations. Injury, 2007, 38: 450–462. [DOI] [PubMed] [Google Scholar]
- 38. Gautier E, BaChler R, Heini PF, Nolte LP. Accuracy of computer‐guided screw fixation of the sacroiliac joint. Clin Orthop Relat Res, 2001, 393: 310–317. [DOI] [PubMed] [Google Scholar]
- 39. Ecker TM, Jost J, Cullmann JL, et al. Percutaneous screw fixation of the iliosacral joint: a case‐based preoperative planning approach reduces operating time and radiation exposure. Injury, 2017, 48: 1825–1830. [DOI] [PubMed] [Google Scholar]
- 40. Smith H E, Yuan P S, Sasso R, Papadopolous S, Vaccaro AR. An evaluation of image‐guided technologies in the placement of percutaneous iliosacral screws. Spine (Phila Pa 1976), 2006, 31:234‐238. [DOI] [PubMed] [Google Scholar]
- 41. Verbeek J, Hermans E, van Vugt A, Frölke JP. Correct positioning of percutaneous iliosacral screws with computer‐navigated versus fluoroscopically guided surgery in traumatic pelvic ring fractures. J Orthop Trauma, 2016, 30: 331–335. [DOI] [PubMed] [Google Scholar]
- 42. Thakkar SC, Thakkar RS, Sirisreetreerux N, Carrino JA, Shafiq B, Hasenboehler EA. 2D versus 3D fluoroscopy‐based navigation in posterior pelvic fixation: review of the literature on current technology. Int J Comput Assist Radiol Surg, 2017, 12: 69–76. [DOI] [PubMed] [Google Scholar]
- 43. Gras F, Marintschev I, Wilharm A, Klos K, Mückley T, Hofmann GO. 2D‐fluoroscopic navigated percutaneous screw fixation of pelvic ring injuries ‐ a case series. BMC Musculoskelet Disord, 2010, 11: 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Matityahu A, Kahler D, Krettek C, et al. Three‐dimensional navigation is more accurate than two‐dimensional navigation or conventional fluoroscopy for percutaneous sacroiliac screw fixation in the dysmorphic sacrum: a randomized multicenter study. J Orthop Trauma, 2014, 28: 707–710. [DOI] [PubMed] [Google Scholar]
- 45. El‐Desouky II, Mohamed MM, Kandil AE. Percutaneous iliosacral screw fixation in vertically unstable pelvic injuries, a refined conventional method. Acta Orthop Belg, 2016, 82: 52–59. [PubMed] [Google Scholar]
- 46. D'Ambrosia RD. Precision medicine: a new frontier in spine surgery. Orthopedics, 2016, 39: 75–76. [DOI] [PubMed] [Google Scholar]
- 47. Wei WQ, Denny JC. Extracting research‐quality phenotypes from electronic health records to support precision medicine. Genome Med, 2015, 7: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Connor GS, Mcgwin G, Maclennan PA, Alonso JE, Rue LW 3rd. Early versus delayed fixation of pelvic ring fractures. Am Surg, 2003, 69: 1019–1023. [PubMed] [Google Scholar]
- 49. Zwingmann J, Konrad G, Mehlhorn AT, Südkamp NP, Oberst M. Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs conventional). J Trauma, 2010, 69:1501‐1506. [DOI] [PubMed] [Google Scholar]
- 50. Wang X‐Z, Wang G‐D, Meng C‐F, Liu X, Cai X. ISO‐C3D navigation for percutaneous sacroiliac joint screw internal fixation for treatment of pelvic posterior ring injuries. Zhong guo Xiu Fu Chong Jian Wai Ke Za Zhi, 2016, 30: 1338–1343. [DOI] [PubMed] [Google Scholar]


