Abstract
Objective
Renal collecting system macroscopically consists of minor calyx, major calyx, renal pelvis and ureter. Stone in renal collecting system is a common presentation in everyday urological practice. The prevalence of renal calculi ranges from 4% to 20% in different geographical distribution. Anatomical variation in renal collecting system plays a significant role in formation of calculi in its parts. The large extra renal pelvis leads to stagnation of urine for longer durations and formation of stones. The stone free rate after percutaneous nephrolithotomy and extra corporeal shock wave lithotomy is significantly related to anatomical factors, particularly the type of renal pelvis and dimensions (length and width) of lower infundibulum. Previous authors described the morphology of pelvicalyceal system in a highly variable manner and the available anatomical description of pelvicalyceal system is contradictory and incomplete. Hence an attempt has been made to provide the precise anatomy of pelvicalyceal system in adult human kidneys.
Methods
We studied 196 formalin embalmed kidneys to note the number of infundibulum, major and minor calyces. The location and shape of pelvis were also studied.
Results
The intra-renal pelvis was narrow and had funnel shaped appearance in 95 of total 196 (48.5%) specimens, and the extra-renal pelvis was dilated as balloon shaped in 43 of 196 (21.9%) specimens. In 41 (20.9%) specimens, the renal pelvis was having partially intra- and extra-renal in location. Bilateral symmetry was found in only 27.1% of 196 renal collecting systems. The length of lower infundibulum was more than 22 mm in 19 (9.7%) of 196 cases which directly affects the stone clearance rate during open and endoscopic surgeries on pelvicalyceal system.
Conclusion
This study provides the accurate morphological details of the shape and dimensions of renal pelvicalyceal system to help the urologists and nephrologists.
Keywords: Renal pelvis, Morphology, Pelvicalyceal system, Urologists, Renal calculi, Intra-renal pelvis
1. Introduction
Macroscopically, the renal collecting system consists of minor and major calices, pelvis and ureter. The minor calices unite with their neighbours to form two or three larger chambers, the major calyces. The major calyces drain into infundibula. Two infundibula join to form the renal pelvis normally, one from upper pole and one from lower pole calyces, but there may be third, which drains the calyces in the midportion of kidney. The funnel shaped renal pelvis tapers towards the lower end of kidney to continue as ureter [1], [2], [3]. Standard anatomy textbooks and literature frequently describe that all branches from the renal pelvis, whether single or multiple, are termed infundibula [1], [3], [4].
The renal pelvicalyceal system is classified considering its shape, position, length, and the pattern of drainage of calyces. Didio [5] found that the renal pelvis can be classified based on length of calyces as long and brachy types. Ningthoujam et al. [6] made different groups of classifying the pelvicalyceal patterns. The different groups include multicalyceal, tricalyceal, and bicalyceal types. Those patterns that do not fit into any of the above types are grouped as unclassified type. Though previous studies provided the detail of the anatomical feature of renal pelvis, the authors used different terminology. Most of the studies were carried out on computed tomographic images. Hence, the present study was undertaken on cadavers to provide an elaborate mapping of pelvi-calyceal anatomy in cadaveric specimens as it applies to endoscopic surgeries namely extra-corporeal shock wave lithotomy (ESWL), percutaneous nephrolithotomy (PCNL) and nephron-sparing surgery.
2. Materials and methods
A total of 196 (101 right and 95 left) specimens of kidneys were included in the study from Department of Anatomy, Rural Medical College, PIMS (DU), Loni, Maharashtra, India.
Permission from the Institutional Ethical Committee of Rural Medical College (Pravara Institute of Medical Sciences, Loni, Maharashtra, India) was obtained before starting the project. The cadaver populations belong to age group 35–86 years, 65 male and 33 female cadavers of Asian origin were included in the study. The cadavers were embalmed with 10% formalin. After routine dissection of abdominal cavity by medical graduates, the specimens were used in the study. There were no signs of surgery, wound scars or trauma in the abdominal lumbar region of any of the cadavers included in the present study. Specimen having any pathology distorting the shape of kidney or renal pelvis was excluded from the study.
Kidneys were dissected out after reflecting the peritoneum of posterior abdominal wall. The fascia over the kidneys was removed. The perinephric fats around kidneys, renal vessels and ureter were cleaned and structures at the renal sinus were separated. Midsagittal section of the kidneys was taken to secure most of the part of the renal collecting system. The number of infundibulum, major and minor calyces was noted after clearing fat and fascia in the region. The location of the renal pelvis was categorized into intra-renal, extra-renal and mixed pelvis according to Bruce et al. [7] classification. Extra-renal pelvis refers to the location of the renal pelvis outside the confines of the renal hilum. Shape of renal pelvis was noted depending upon the number of major calyces joining to form the renal pelvis. Lower infundibulum length (LIL) was measured and it is the distance measured from the most distal point at the bottom of the lower calyx to a midpoint of the lower lip of the renal pelvis. Lower infundibular width (LIW) was measured at the narrowest point along their respective infundibular axis. These were the same anatomical landmarks taken by previous authors and were surgical relevant [8].
3. Results
In the present series of study on 196 specimens of adult kidneys from embalmed cadavers, a significant difference was observed in shape and location of the renal pelvis during bilateral comparison.
-
i)
Location of pelvis
The intra-renal pelvis was located within the renal sinus and presented with a narrow and funnel-shaped appearance in 95 of 196 (48.5%); the wall of extra-renal pelvis was thin and dilated in 43 of 196 (21.9%). Extra-renal pelvis was located outside the sinus and was not closed by the renal parenchyma. In 41 (20.9%) specimens, the renal pelvis was having partially intra- and extra-renal in location (Table 1). Bilateral symmetry was found in only 53 (27.0%) of 196 renal collecting systems.
-
ii)
Shape of pelvis
Table 1.
Incidence of extra-hilar and intra-hilar pelvis of 196 renal collecting systems observed.
| Location of pelvis | Total number of specimens, n (%) | Number of specimens observed |
|
|---|---|---|---|
| Right | Left | ||
| Extra-hilar | 43 (21.9) | 20 | 23 |
| Intra-hilar | 95 (48.5) | 47 | 48 |
| Mixed | 41 (20.9) | 19 | 22 |
| No pelvis | 17 (8.7) | 8 | 9 |
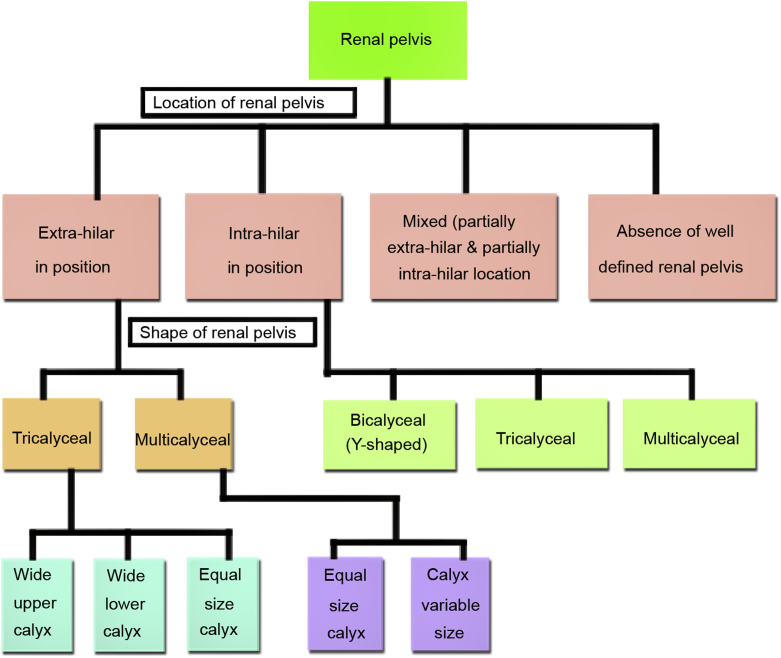
The shape of renal pelvis was classified as bicalyceal, tricalyceal, multicalyceal and absence of well-defined shape (Fig. 1, Table 2). The intra-renal pelvis was subclassified into three types depending upon the location of major calyces as shown in Fig. 2. Tricalyceal renal pelvis was classified into three types depending upon the width of major calyces as shown in Fig. 3. An absence of well-defined funnel-shaped renal pelvis was observed in 17 of 196 (8.7%) specimens where the ureter was commencing from the infundibulum of major calyx directly (Table 1, Fig. 4). Interestingly we found this type of morphology in bicalyceal renal pelvis only.
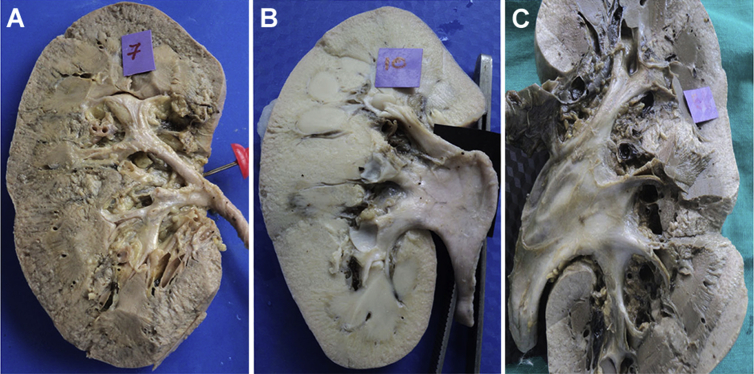
Figure 1.
Three shapes of pelvis depending upon the number of major calices joining to for pelvis. (A) Bicalyceal intra-renal pelvis; (B) Tricalyceal extra-renal pelvix; (C) Multicaliceal extra-renal pelvis.
Table 2.
Number of major calyces (shape of pelvis) in pelvi calyceal system of 196 specimens.
| Number of major calyces | Number of cases observed, n (Right and Left) | Percentage (%) |
|---|---|---|
| 2 (bicalyceal) | 116 (57 and 59) | 59.2 |
| 3 (tricalyceal) | 42 (22 and 20) | 21.4 |
| 4 and more (multicalyceal) | 33 (16 and17) | 16.8 |
| Unclassified (absence of well defined pelvis) | 5 (3 and 2) | 2.6 |
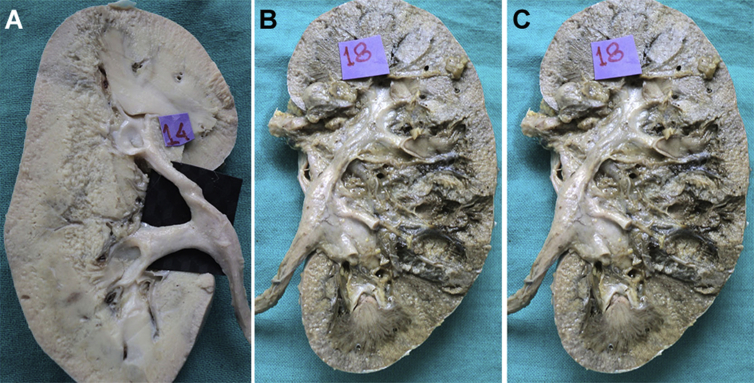
Figure 2.
Types of bicayceal pelvis depending upon the width of renal calices. (A) Bicalyceal intra-renal pelvis with equal dimensions; (B) Bicalyceal pelvis with wide upper calyx; (C) Bicalyceal renal pelvis with wide lower calyx.
Figure 3.
Types of tricalyceal pelvis depending upon the width of major calices. (A) Tricalyceal pelvis (equal dimensions of all three calyces); (B) Tricalyceal pelvis with wider middle calyx; (C) Tricalyceal pelvis with wider lower calyx.
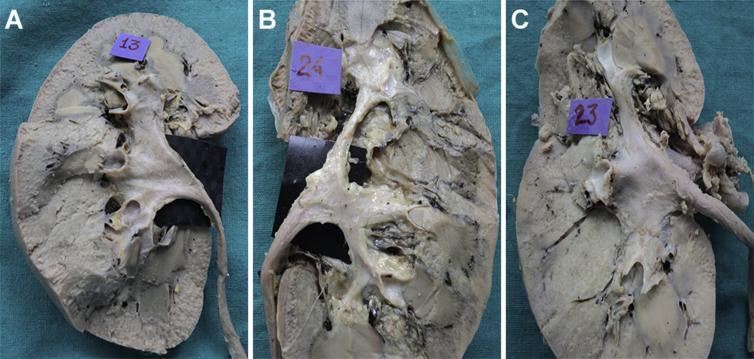
Figure 4.
The infundibula of major calyx are directly continuous with ureter and there is absence of a well defined funnel shaped renal pelvis.
iii) The level of formation of ureter was observed in relation to lower border of kidney, with 77 (39.3%) at lower border of kidney, 25 (12.7%) above lower border, and 41 (20.9%) below lower border.
iv) Interesting anatomical variations
-
a)
Urolithiasis in the form of large renal calculi in major calyx was observed in multi calyceal extrarenal pelvis. The wall of the pelvis was very thin (Fig. 5).
-
b)
Dilated renal pelvis (Megacalix) was observed in 34 (17.3%) of specimens (Fig. 1B). The observed number of major calyces and minor calices in present study is given in Table 2, Table 3, respectively. The details of dimensions (length and width) of lower infundibulum are provided in Table 4.
Figure 5.
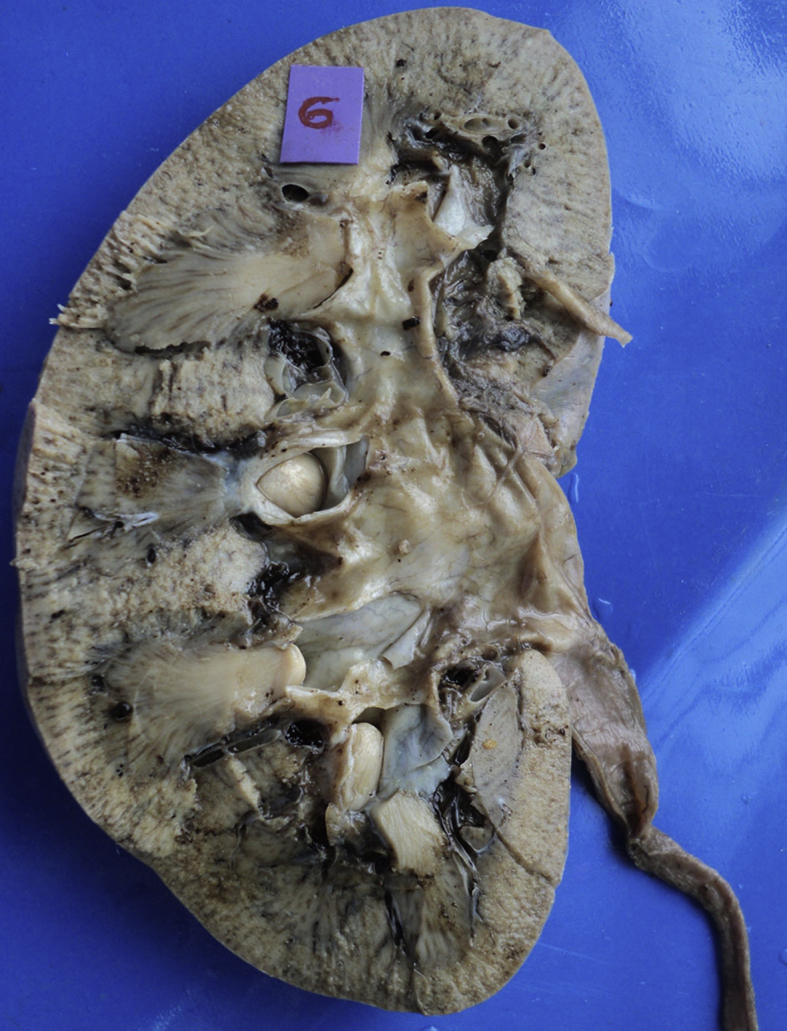
Multicalyceal renal pelvis with urolithiasis.
Table 3.
Number of minor calyces in pelvi calyceal system of 196 specimens observed.
| Number of minor calyx | Number of cases observed | Percentage (%) |
|---|---|---|
| 4 | 16 | 8.2 |
| 5 | 17 | 8.7 |
| 6 | 5 | 2.6 |
| 7 | 84 | 42.9 |
| 8 | 55 | 28.1 |
| 9 | 11 | 5.6 |
| 10 | 6 | 3.1 |
| 11 | 2 | 1.0 |
Table 4.
Length and width of lower infundibula observed in the kidneys of 196 specimens.
| Length and width of lower infundibula (mm) | Number of cases observed | Percentage (%) |
|---|---|---|
| Length | ||
| 5–10 | 32 | 16.3 |
| 11–15 | 53 | 27.0 |
| 16–21 | 92 | 46.9 |
| 22–31 | 19 | 9.7 |
| Width | ||
| More than 4 mm | 33 | 16.8 |
| Less than 4 mm | 163 | 83.2 |
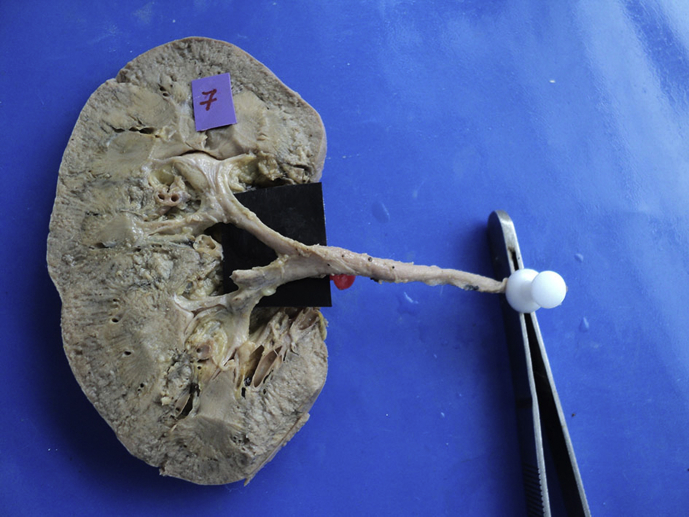
The classification of renal pelvicalyceal system depending upon the shape of minor and major calices is explained in simplified manner (Fig. 6).
Figure 6.
Classification of renal pelvi-calyceal system.
4. Discussion
Anatomical variations of renal pelvicalyceal system are as common as the variations in fingerprints of an individual. The congenital anomalies of upper urinary tract occur in almost 10% of all urinary system malformations. Calculi in lower calyceal group represent more cases in almost 24%–44% of all calculi requiring treatment because of longer stasis of urine in lower infundibulum [6], [9].
Earlier Sykes [10] in 1963 studied details of location of renal pelvis in 240 kidneys and found only 12 (5%) of these possessed extra-renal major calyces [10]. In present study, we found more percentage of extra-renal pelvis (21.9%) in comparison to previous authors (Table 1). Clinically, the extra-renal pelvis is roomier and more convenient to explore during nephron sparing surgery and partial nephrectomy than the intra-renal pelvis because it provides larger surface area away from the renal vasculature for safe surgery but the drawback is that the larger pelvic space aggravates accumulation and stasis of urine predisposing formation of renal calculi [9]. A distended renal pelvis and collecting system facilitate the puncture, placement, and maneuvering of the endourologic instruments and by providing a larger fluid chamber around a stone, enhance the efficacy of ESWL [11], [12], [13], [14]. Kupeli et al. [15] observed extra-renal distended pelvis in 27.5% of cases facilitating endourological processes. Shafik and Al-Sherif [16] in their retrospective study on 255 patients who have undergone partial nephrectomy concluded that the intra-renal pelvis is smaller and associated with longer thinner infundibula. Intra-renal pelvis was also associated with the complications as urine leak presence. A completely intra-renal pelvis is confined within renal parenchyma and thereby constrained to a smaller volume. Fluid dynamics by Pascals principle and Laplace's law explain the preferential leak rate of the intra-renal pelvis. The smaller surface area of intra-renal pelvis is responsible for increased wall tension or increased intra-renal pressure in cases of ureteral obstruction portend urinary leak following partial nephrotomy which was found in 48.4% of specimens.
The observed range of number of minor calices is 4–11 in present study (Table 3) and coincides with previous Indian authors. More number of minor calices in the operating field result in less success rate of PCNL and less invasive endoscopic procedures. Didio [5] in 1970 described mainly two types of pelvis—Longi and Brachi type. The Longi type consists of long major calices ending in a small pelvis (ramified type) and in Brachi type the major calices were short and end in large renal pelvis (ampullary type). Ningthoujam et al. [6] categorized the pelvis into three types (i) radiate or multicaliceal, (ii) triangular or tricalyceal and (iii) Y-shaped or bicalyceal depending on the number of calices which directly drains and forms the pelvis. The present study in accordance with Ningthoujam et al. [6] observed that the tricalyceal pelvis is spacious in comparision to bicalyceal renal pelvis. The bicaliceal pelvis is further subdivided depending upon the width of each limb of renal pelvis.
In present study, the renal pelvis was absent bilaterally in 8.7% of specimens while Anjana et al. [17] found absence of renal pelvis unilaterally in 3% of cases. Surgery is challenging in these type of renal pelvis because of deficiency of space and complicated relations with blood vessels. The various percutaneous procedures for treating pathologies involving the kidneys include percutaneous nephrostomy, antegrade pyelography, antegrade stent positioning, PCNL, and ureteric dilatation. All these procedures require positioning of a canula or puncturing via percutaneous approach [18]. These procedures are done under imaging guidance bearing in mind the different patterns of the pelvicalyceal system. The basic rule before gaining access into the pelvicalyceal system is that a direct puncture into the renal pelvis is dangerous because of the risk of laceration and bleeding [19], [20]. Calculi in the lower caliceal group represent almost 44% of cases requiring surgical intervention. Further calculi in upper calyx may also escape in lower calyx during fragmentation by ESWL [9]. Arzoz-Fabregas et al. [9] suggested that lower infundibular length has a great significance in the formation of calculi as the increased length leads to stagnation and retention of crystals in the inferior calyceal system which may result in formation of stones. The success rate of ESWL and removal of all fragments of stones are comparatively less in patients with long lower infundibulum. Lower infundibular length is a good measurement tool for deciding the method of treatment to obtain good outcome from lithotripsy. The height of less than 22 mm favours stone clearance [8], [9], [12], [21], [22], [23], [24]. We observed the larger LIL (22–31 mm) in 9.7% of total specimens which is higher than the reported cases which is the cause of higher incidences of renal stones. The increased length of lower calyces (22–31 mm) with a width of less than 4 mm might lead to retention of residual stones in lower caliceal group after lithotripsy as stated by Sampaio and Mandarim-de-Lacerda [24]. The number of minor and major calyces observed by previous authors is enumerated in Table 5, Table 6, respectively.
Table 5.
Reported number of minor calices by authors in different population.
| Study | Number of specimens studied | Number of minor cases observed |
|---|---|---|
| Hollinshead, 1985 [25] | – | 7–8 |
| Harrison, 1972 [26] | – | 8–9 |
| Kaye and Reinke, 1983 [27] | – | 4–12 |
| Dyson, 1995 [28] | – | 7–8 |
| Ningthoujam et al., 2005 [6] | 20 adult and 80 fetal kidneys 100 IVU |
6–12 |
| Wadekar and Gangane, 2012 [3] | 100 | 5–11 |
| Present study | 196 | 4–11 |
IVU, intravenous urography; –, not reported.
Table 6.
Reported number of major calices by authors in different population.
| Study | Country | Number of specimens studied | Number of major calyces observed | Percentage (%) |
|---|---|---|---|---|
| Fine and Keen [29] | Great Britain | 107 | 2 more than 3 | – |
| Ningthoujam et al. [6] | India | 20 adult and 80 fetal kidneys 100 IVU |
2–3 | – |
| Miller et al., 2013 [2] | United States | 100 | 3 more than 2 | – |
| Wadekar et al., 2012 [3] | India | 100 | 2 and 3 | 2 in 60% and 3 in 40% |
| Present study | India | 196 | 2–4 | 2 in 116 (59.2%) 3 in 75 (38.3%) 4 in 5 (2.5%) |
IVU, intravenous urography; –, not reported.
5. Conclusion
Present study showed that the accurate knowledge of normal and anatomical variations of pelvicalyceal system is mandatory for urologists as well as radiologists. The dimension of lower calyx of pelvicalyceal system plays a significant role in renal stone formation. The surgeon has to be cautious while performing ESWL and PCNL where the lower calyx is lengthy and narrower (less than 4 mm) which directly affects the clearance rate after these procedures. The detailed classification of pelvicalyceal system will enhance the present knowledge of this region that is mandatory for the uro-surgeons and nephrologists for safe and uncomplicated surgical procedures. Radiologists and anatomists shall also be well versed with the details of the renal collecting system to minimize the diagnosis error.
Author contributions
Study concept and design: Kusum Gandhi.
Data acquisition: Kusum Gandhi, Sushama Chavan.
Data analysis: Sushama Chavan.
Drafting of manuscript: Kusum Gandhi, Sushama Chavan.
Critical revision of the manuscript: Kusum Gandhi.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Second Military Medical University.
References
- 1.Pollack Howard M. 1st ed. W B Saunders Co; Philadelphia: 1990. Clinical urography—an atlas and textbook of urological imaging; pp. 135–178. [Google Scholar]
- 2.Miller J., Durack J.C., Sorensen M.D., Wang J.H., Stoller M.L. Renal calyceal anatomy characterization with 3-dimensional in vivo computerized tomography imaging. J Urol. 2013;189:562–567. doi: 10.1016/j.juro.2012.09.040. [DOI] [PubMed] [Google Scholar]
- 3.Wadekar P.R., Gangane S.D. Study of variations in the pelvicalyceal system of kidney and its clinical importance. NEPJOL. 2012;3:17–21. [Google Scholar]
- 4.Neil R.B., Healy J.C. Kidney. In: Standring S., Neil R.B., Patricia C., Alan R.C., Michael A.G., Healy J.C., editors. Grays anatomy. The anatomical basis of clinical practice. 40th ed. Churchill Livingstone Elsevier Limited; New York: 2008. p. 1231. [Google Scholar]
- 5.Didio L.J.A. 1st ed. The C.V. Mosby Co; Saint Louis: 1970. Urinary system in synopsis of anatomy; pp. 276–286. [Google Scholar]
- 6.Ningthoujam D.D., Chongtham R.D., Sinam S.S. Pelvi-calyceal system in foetal and adult human kidneys. J Anat Soc India. 2005;54:1–11. [Google Scholar]
- 7.Bruce Sir J., Warmsley R., Ross J.A. 5th ed. E and S Livingstone limited; Edinburg: 1967. The abdominal cavity in manual of surgical anatomy; pp. 391–403. [Google Scholar]
- 8.Wadekar P., Pundge S., Gangane S. The impact of lower infundibular length and lower infundibular width on renal stone formation. Int J Healthc Biomed Res. 2014;2:158–163. [Google Scholar]
- 9.Arzoz-Fabregas M., Ibarz-Servio L., Blasco-Casares F.J., Ramon-Dalmau M., Ruiz-Marcellan F.J. Can infundibular height predict the clearance of lower pole calyceal stone after extracorporeal shockwave lithotripsy? J Urol. 2009;35:140–150. doi: 10.1590/s1677-55382009000200003. [DOI] [PubMed] [Google Scholar]
- 10.Sykes D. The arterial supply of the human kidney with special reference to accessory renal arteries. Br J Surg. 1963;50:368–374. doi: 10.1002/bjs.18005022204. [DOI] [PubMed] [Google Scholar]
- 11.Krishnaveni C., Kulkarni R., Kishore Kumar B.N., Sanikop M.B., Venkateshu K.V. A study of renal calyces by using barium contrast. Int J Anat Res. 2014;2:369–374. [Google Scholar]
- 12.Lin C.C., Hsu Y.S., Chen K.K. Predictive factors of lower calyceal stone clearance after extracorporeal shockwave lithotripsy (ESWL): the impact of radiological anatomy. J Chin Med Assoc. 2008;71:496–501. doi: 10.1016/S1726-4901(08)70157-6. [DOI] [PubMed] [Google Scholar]
- 13.Verma A., Tomar V., Yadav S. Complex multiple renal calculi: stone distribution, pelvicalyceal anatomy and site of puncture as predictors of PCNL outcome. SpringerPlus. 2016;5:1356. doi: 10.1186/s40064-016-3017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pfeiffer E.W. Comparative anatomical observations of the mammalian renal pelvis and medulla. J Anat. 1968;102:321–331. [PMC free article] [PubMed] [Google Scholar]
- 15.Kupeli B., Tunc L., Acar C., Gurocak S., Alkibay T., Guneri C. The impact of pelvicaliceal anatomical variation between the stone-bearing and normal contralateral kidney on stone formation in adult patients with lower caliceal stones. Int Braz J Urol. 2006;32:287–294. doi: 10.1590/s1677-55382006000300005. [DOI] [PubMed] [Google Scholar]
- 16.Shafik A., Al-Sherif A. Ureteropelvic junction: a study of its Anatomical Structure and function. Ureteropelvic junction sphincter? Eur Urol. 1999;36:150–157. doi: 10.1159/000067987. [DOI] [PubMed] [Google Scholar]
- 17.Anjana T.S., Muthian E., Thiagarajan S., Shanmugam S. Gross morphological study of the renal pelvicalyceal patterns in human cadaveric kidneys. Indian J Urol. 2017;33:36–40. doi: 10.4103/0970-1591.194782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutton D. 7th ed. Elsevier Science Ltd; London: 2003. Textbook of radiology and imaging; pp. 900–903. [Google Scholar]
- 19.Sampaio F.J.B., Mandarim-de-Lacerda Anatomic classification of kidney collecting system for endourologic procedures. J Endourol. 1988;2:247–251. [Google Scholar]
- 20.Clayman R.V., Surya V., Hunter D., Castaneda-Zuniga W.R., Miller R.P., Coleman C. Renal vascular complications associated with the percutaneous removal of renal calculi. J Urol. 1984;132:228–230. doi: 10.1016/s0022-5347(17)49573-5. [DOI] [PubMed] [Google Scholar]
- 21.Gupta N.P., Singh D.V., Hemal A.K., Mandal S. Infundibulopelvic anatomy and clearance of inferior caliceal calculi with shock wave lithotripsy. J Urol. 2000;163:24–27. [PubMed] [Google Scholar]
- 22.Politis G., Griffith D.P. ESWL: stone free efficacy based upon stone size and location. World J Urol. 1987;5:255–258. [Google Scholar]
- 23.Marroig B., Favorito L.A., Fortes M.A., Sampaio F.J. Lower pole anatomy and mid-renal-zone classification applied to flexible ureteroscopy: experimental study using human three dimensional endocasts. Surg Radiol Anat. 2015;37:1243–1249. doi: 10.1007/s00276-015-1503-y. [DOI] [PubMed] [Google Scholar]
- 24.Sampaio F.J., Mandarim-de-Lacerda C.A. Three dimensional and radiologic study. In: Sampaio F.J., Uflacker R., editors. Renal anatomy applied to urology, endourology and interventional radiology. Thieme Medical Publishers; New York: 1993. pp. p1–p6. [Google Scholar]
- 25.Hollinshead W.H. 4th ed. Harper and Row Publishers; Cambridge: 1985. Textbook of anatomy in abdome; pp. 703–707. [Google Scholar]
- 26.Harrison R.G. The urogenital system. In: Romanes G.J., editor. Cunningham's textbook of anatomy. 11th ed. Oxford University Press; London: 1972. pp. 503–556. [Google Scholar]
- 27.Kaye K.W., Reinke D.B. Detailed caliceal anatomy for endourology. J Urol. 1984;132:1085–1088. doi: 10.1016/s0022-5347(17)50042-7. [DOI] [PubMed] [Google Scholar]
- 28.Dyson M. Urinary system. In: Williams P.L., Bannister L.H., Berry M.M., Collins P., Dyson M., Dussek J.E., editors. Gray's anatomy. 38th ed. Churchill Livingstone; Edinburgh: 1995. pp. 1813–1845. [Google Scholar]
- 29.Fine J., Keen E.N. The arteries of the human kidney. J Anat. 1966;100:881–894. [PMC free article] [PubMed] [Google Scholar]