Key Points
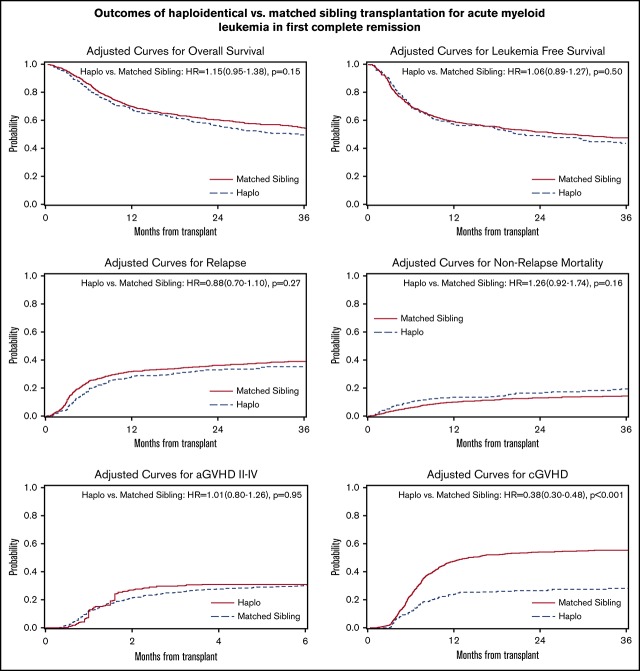
PT-Cy–based Haplo-HCT resulted in less chronic GVHD compared to matched sibling transplantation in patients with AML in CR1.
Survival, relapse, nonrelapse mortality, and acute GVHD rates were not different between the 2 approaches.
Abstract
HLA-haploidentical hematopoietic cell transplantation (Haplo-HCT) using posttransplantation cyclophosphamide (PT-Cy) has improved donor availability. However, a matched sibling donor (MSD) is still considered the optimal donor. Using the Center for International Blood and Marrow Transplant Research database, we compared outcomes after Haplo-HCT vs MSD in patients with acute myeloid leukemia (AML) in first complete remission (CR1). Data from 1205 adult CR1 AML patients (2008-2015) were analyzed. A total of 336 patients underwent PT-Cy–based Haplo-HCT and 869 underwent MSD using calcineurin inhibitor–based graft-versus-host disease (GVHD) prophylaxis. The Haplo-HCT group included more reduced-intensity conditioning (65% vs 30%) and bone marrow grafts (62% vs 7%), consistent with current practice. In multivariable analysis, Haplo-HCT and MSD groups were not different with regard to overall survival (P = .15), leukemia-free survival (P = .50), nonrelapse mortality (P = .16), relapse (P = .90), or grade II-IV acute GVHD (P = .98). However, the Haplo-HCT group had a significantly lower rate of chronic GVHD (hazard ratio, 0.38; 95% confidence interval, 0.30-0.48; P < .001). Results of subgroup analyses by conditioning intensity and graft source suggested that the reduced incidence of chronic GVHD in Haplo-HCT is not limited to a specific graft source or conditioning intensity. Center effect and minimal residual disease–donor type interaction were not predictors of outcome. Our results indicate a lower rate of chronic GVHD after PT-Cy–based Haplo-HCT vs MSD using calcineurin inhibitor–based GVHD prophylaxis, but similar other outcomes, in patients with AML in CR1. Haplo-HCT is a viable alternative to MSD in these patients.
Visual Abstract
Introduction
Allogeneic hematopoietic cell transplantation (HCT) is a potentially curative treatment modality for patients with acute myeloid leukemia (AML). Although an HLA-matched sibling donor (MSD) is considered the optimal donor,1,2 alternative donors have permitted safe and effective HCT for patients lacking an MSD. HLA-haploidentical hematopoietic cell transplantation (Haplo-HCT) is one such approach. Haplo-HCT is performed most commonly using posttransplantation cyclophosphamide (PT-Cy) as the backbone for graft-versus-host disease (GVHD) prophylaxis.3,4
Several studies have compared the outcomes of Haplo-HCT vs umbilical cord blood5-7 and matched unrelated donor (MUD) HCT.8-13 In addition, 4 large retrospective studies compared MSD vs Haplo-HCT. In 1 study comparing reduced-intensity conditioning (RIC) MSD vs PT-Cy–based Haplo-HCT in patients with lymphoma, outcomes were similar between the 2 groups, with the exception that a lower incidence of chronic GVHD was evident in the Haplo-HCT cohort.14 In another study comparing PT-Cy–based Haplo-HCT with MSD and MUD for patients with Hodgkin lymphoma, Haplo-HCT was associated with less relapse and chronic GVHD compared with MSD.11 A third study compared Haplo-HCT and MSD in patients with intermediate- or poor-risk AML in first complete remission (CR1). Among high-risk patients, no outcome differences were observed between the groups, with the exception that there was more grade II-IV acute GVHD and a trend for less relapse after Haplo-HCT.15 Among intermediate-risk patients, nonrelapse mortality (NRM), leukemia-free survival (LFS), and overall survival (OS) were worse after Haplo-HCT. Importantly, 26% of Haplo-HCT recipients in this study did not receive PT-Cy. Finally, in a study comparing MSD and PT-Cy–based Haplo-HCT in patients with AML or acute lymphoblastic leukemia,16 the incidence of chronic GVHD was lower after Haplo-HCT. Other outcomes were similar between the groups for patients younger than 55 years. In contrast, in patients aged 55 years or older, MSD yielded lower rates for graft failure, NRM, and overall mortality compared with Haplo-HCT from an offspring.
A common theme among these studies is a reduced incidence of chronic GVHD after PT-Cy–based Haplo-HCT. However, these studies have important differences in their patient-, disease-, and transplant-related characteristics, highlighting the need to analyze more homogenous cohorts. Using such cohorts would minimize confounding and increase the likelihood of detecting donor type–specific differences in outcomes. Therefore, we designed the present study to compare the outcomes of MSD with PT-Cy–based Haplo-HCT using a relatively homogenous group of patients with AML in CR1.
Methods
Data sources
The Center for International Blood and Marrow Transplant Research (CIBMTR) includes data from a voluntary working group of >450 transplant centers worldwide that contributes detailed data on allogeneic and autologous HCT. Participating centers are required to report all transplants consecutively; compliance is monitored by on-site audits, and patients are followed longitudinally. Computerized checks for discrepancies, physicians’ review of submitted data, and on-site audits of participating centers ensure data quality. Studies conducted by the CIBMTR are performed in compliance with all applicable federal regulations pertaining to the protection of human research participants. Protected health information used in the performance of such research is collected and maintained in CIBMTR's capacity as a Public Health Authority under the HIPAA Security Rule. The CIBMTR collects data at 2 levels: the transplant essential data (TED) level and the comprehensive report form (CRF) level. The TED-level data are an internationally accepted standard data set that contains a limited number of key variables for all consecutive transplant recipients. Details on CRF- and TED-level data collection have been published previously and are described in detail elsewhere.17 TED- and CRF-level data are collected pretransplant, 100 days and 6 months posttransplant, annually until year 6 posttransplant, and biannually thereafter until death.
Patients
We included all adult patients (age ≥18 years) with AML who were in CR1 at the time of their first allogeneic HCT (between 2008 and 2015) using an MSD or a haploidentical related donor (mismatched for ≥2 HLA loci among HLA-A, HLA-B, HLA-C, and HLA-DRB1). In the Haplo-HCT group, only cases receiving PT-Cy–based GVHD prophylaxis (with or without a calcineurin inhibitor [CNI] and mycophenolate mofetil) were included, whereas in the MSD group, GVHD prophylaxis was limited to CNI-based approaches. Patients receiving ex vivo (T-cell–depleted or CD34-selected grafts) or in vivo (eg, anti-thymocyte immunoglobulin) graft manipulation were excluded. Both peripheral blood and bone marrow as a graft source and myeloablative conditioning (MAC) and RIC regimens were included. The Institutional Review Board of the National Marrow Donor Program approved this study.
End points and definitions
The primary end point was OS. Secondary end points were hematopoietic recovery, relapse, LFS, NRM, and acute and chronic GVHD. OS was defined as the time from HCT to death from any cause. LFS was defined as survival with no evidence of relapse or progression. Relapse was defined as the reappearance of ≥5% blasts on morphological evaluation in bone marrow or an extramedullary site. NRM was defined as death without evidence of relapse or progression. Acute and chronic GVHD were defined according to standard criteria.18 Neutrophil engraftment was defined as achieving an absolute neutrophil count ≥ 0.5 × 109/L for 3 consecutive days, and platelet engraftment was defined as a platelet count ≥20 × 109/L for 7 days unsupported by transfusion.
Cytogenetic risk was defined according to SWOG classification.19 Minimal residual disease (MRD) information before HCT was not collected consistently or reported to the CIBMTR during the period of this study. However, given its key importance in HCT outcomes,20 we used all relevant reported variables to generate an estimate for MRD before HCT (supplemental Table 1). We classified a patient as MRD positive in the following scenarios pre-HCT: (1) answer was “no” to questions on cytogenetic, molecular, or flow cytometry-based remission; (2) answer was “yes” to the question on disease detectability in the blood or bone marrow by flow cytometry; or (3) answer was “yes” to the presence of molecular markers, such as CEBPA, FLT3 D835, FLT3-ITD, IDH1, IDH2, KIT, or NPM1 mutation. We classified a patient as MRD negative if they were not classified as MRD positive and (1) answer was “no” to the question on disease detectability in the blood or bone marrow by flow cytometry or (2) answer was “yes” to questions on cytogenetic, molecular, or flow cytometry-based remission. HCT comorbidity index (HCT-CI) was defined according to standard criteria.21
Statistical methods
Patient- and transplant-related variables were compared using the χ2 test for categorical variables and the Mann-Whitney U test for continuous variables. Kaplan-Meier curves were used to estimate the probability of OS and LFS. Cumulative incidence was used to estimate the probability of NRM, GVHD, and relapse. For GVHD and relapse, NRM was treated as a competing risk. For NRM, relapse was treated as a competing risk. For LFS and OS, patients were censored at the time of last follow-up.
Univariate analysis was performed for the main effect (donor type) in relation to outcomes. In multivariable Cox proportional-hazards models, donor type (main effect) was forced in, and a backward stepwise model selection approach using the Akaike information criterion was used to identify a priori selected potential predictors of outcomes (supplemental Table 2). Covariates significant at a 5% level were kept in the final model. The assumption of proportional hazards for each factor in the Cox model was tested by adding time-dependent covariates. Potential interactions between main effect and significant covariates were tested. Transplantation center effect was tested using the frailty model.22 Adjusted probabilities of LFS and OS, as well as adjusted cumulative incidence functions of NRM and relapse, were calculated using multivariable models, stratified on the main effect and weighted by the pooled sample proportion value for each prognostic factor.
We hypothesized that OS following PT-Cy–based Haplo-HCT is not significantly different from MSD using CNI-based GVHD prophylaxis in AML patients in CR1. Assuming that there is a ≥10% difference between the groups in 3-year OS, using a 2-sided test (allowing for the difference to be in either direction) at 5% significance level, and with the available sample size that we identified in the CIBMTR database, we had 86% power to detect this difference. All analyses were done using the statistical package SAS version 9.3 (SAS Institute, Cary, NC).
Results
Data from 1205 patients (Haplo-HCT, n = 336; MSD, n = 869) were analyzed. Patient, disease, and transplant characteristics are shown in Table 1. Patients were older and donors were younger in the Haplo-HCT group; 55% vs 38% of Haplo-HCT vs MSD recipients and 11% vs 35% of Haplo-HCT vs MSD recipients were ≥55 years of age (P < .001 for both comparisons). There were more African American patients in the Haplo-HCT group compared with the MSD group (21% vs 5%, P < .001). The Haplo-HCT group included more RIC (65% vs 30%, P < .001) and bone marrow grafts (62% vs 7%, P < .001), consistent with current practice. In addition, a smaller proportion of Haplo-HCT recipients were white (68% vs 84%, P < .001) and a smaller proportion underwent HCT within 6 months of diagnosis compared with the MSD group (69% vs 83%, P < .001). Intermediate-risk cytogenetics was more common in the MSD group (65% vs 50%, P < .001). As expected, a smaller proportion of Haplo-HCT vs MSD transplants were performed before 2011 (11% vs 49%, P < .001).
Table 1.
Patients, disease, and transplant characteristics
| Variable | Haplo (n = 336) | MSD (n = 869) | P |
|---|---|---|---|
| Patient age, y | <.001 | ||
| 18-54 | 152 (45) | 542 (62) | |
| ≥55 | 184 (55) | 327 (38) | |
| Median (range) | 57 (18-74) | 52 (18-71) | |
| Donor age, y | <.001 | ||
| 18-54 | 212 (63) | 560 (64) | |
| ≥55 | 37 (11) | 306 (35) | |
| Missing | 87 (26) | 3 (<1) | |
| Median (range) | 39 (16-68) | 51 (18-73) | |
| Sex | .42 | ||
| Male | 183 (54) | 451 (52) | |
| Female | 153 (46) | 418 (48) | |
| Race | <.001 | ||
| White | 229 (68) | 727 (84) | |
| African American | 69 (21) | 46 (5) | |
| Others | 20 (6) | 70 (8) | |
| Missing | 18 (5) | 26 (3) | |
| HCT-CI | .20 | ||
| 0 | 99 (29) | 254 (29) | |
| 1 | 53 (16) | 136 (16) | |
| 2 | 43 (13) | 124 (14) | |
| ≥3 | 133 (40) | 309 (36) | |
| Missing | 8 (2) | 46 (5) | |
| Karnofsky performance status | .78 | ||
| <90 | 112 (33) | 308 (35) | |
| ≥90 | 208 (62) | 551 (64) | |
| Missing | 16 (5) | 10 (1) | |
| Time from diagnosis to HCT, mo | <.001 | ||
| <6 | 231 (69) | 721 (83) | |
| 6-12 | 89 (26) | 131 (15) | |
| >12 | 16 (5) | 17 (2) | |
| Median (range) | 5 (2-36) | 4 (1-18) | |
| Type of AML | .05 | ||
| De novo | 244 (73) | 662 (76) | |
| Transformed from MDS/MPN | 70 (21) | 133 (15) | |
| Therapy related | 22 (6) | 74 (9) | |
| Donor/recipient cytomegalovirus serostatus | .26 | ||
| +/+ | 139 (41) | 328 (38) | |
| +/− | 29 (9) | 98 (11) | |
| −/+ | 91 (27) | 223 (26) | |
| −/− | 75 (22) | 204 (23) | |
| Missing | 2 (<1) | 16 (2) | |
| Donor/recipient sex | .47 | ||
| Male-male | 114 (34) | 256 (29) | |
| Male-female | 88 (26) | 231 (26) | |
| Female-male | 69 (21) | 195 (23) | |
| Female-female | 65 (19) | 187 (22) | |
| Cytogenetics | <.001 | ||
| Favorable | 12 (4) | 26 (3) | |
| Intermediate | 170 (50) | 560 (64) | |
| Poor: monosomal karyotype | 33 (10) | 76 (9) | |
| Poor: other | 70 (21) | 174 (20) | |
| Not tested or missing | 51 (15) | 33 (4) | |
| MRD prior to HCT | .10 | ||
| Negative | 250 (74) | 598 (62) | |
| Positive | 66 (20) | 192 (29) | |
| Missing | 20 (6) | 79 (9) | |
| Conditioning intensity | <.001 | ||
| MAC with TBI | 34 (10) | 216 (24) | |
| MAC without TBI | 83 (25) | 396 (45) | |
| RIC/nonmyeloablative | 219 (65) | 250 (30) | |
| Missing | 0 | 7 (<1) | |
| Graft source | <.001 | ||
| Bone marrow | 208 (62) | 56 (7) | |
| Peripheral blood | 128 (38) | 813 (93) | |
| GVHD prophylaxis* | <.001 | ||
| CNI + methotrexate ± others | 3 (<1) | 622 (70) | |
| CNI + mycophenolate mofetil ± others | 322 (96) | 154 (19) | |
| Others | 9 (3) | 88 (11) | |
| Missing | 2 (<1) | 5 (<1) | |
| Year of HCT | <.001 | ||
| 2008-2010 | 36 (11) | 424 (49) | |
| 2011-2015 | 300 (89) | 445 (51) | |
| Median follow-up of survivors (range), mo | 35 (3-97) | 60 (3-119) |
Unless otherwise noted, all data are n (%).
Haplo, haploidentical; MDS, myelodysplastic syndrome; MPN, myeloproliferative neoplasm.
All Haplo-HCT patients received PT-Cy, whereas all MSD patients received a CNI.
Univariate analysis
Acute and chronic GVHD.
In univariate analysis (Table 2), the Haplo-HCT group had similar rates of grade II-IV acute GVHD (32%; 95% confidence interval [95% CI], 27-37 vs 30%, 95% CI, 27-33; P = .64) and grade III-IV acute GVHD (10%; 95% CI, 7-14 vs 12%; 95% CI, 10-14; P = .54) at 6 months but lower rates of chronic GVHD (26%, 95% CI, 21-31 vs 56%; 95% CI, 53-60 at 3 years; P < .001) and extensive chronic GVHD (16%; 95% CI, 12-20 vs 47%; 95% CI, 44-50 at 3 years; P < .001).
Table 2.
Univariate analysis of outcomes
| Outcomes | Haploidentical | MSD | P |
|---|---|---|---|
| Neutrophil engraftment at 1 mo | 92 (89-95) | 99 (98-99) | <.001 |
| Platelet engraftment at 100 d | 89 (85-92) | 97 (96-98) | <.001 |
| Grade II-IV acute GVHD | .98 | ||
| 100 d | 31 (26-36) | 26 (23-29) | .09 |
| 6 mo | 32 (27-37) | 30 (27-33) | .64 |
| Grade III-IV acute GVHD | .28 | ||
| 100 d | 10 (7-14) | 10 (8-12) | .94 |
| 6 mo | 10 (7-14) | 12 (10-14) | .54 |
| Chronic GVHD | <.001 | ||
| 1 y | 22 (18-27) | 48 (45-52) | <.001 |
| 3 y | 26 (21-31) | 56 (53-60) | <.001 |
| Extensive chronic GVHD | <.001 | ||
| 1 y | 15 (11-19) | 41 (38-44) | <.001 |
| 3 y | 16 (12-20) | 47 (44-50) | <.001 |
| Relapse | .88 | ||
| 1 y | 30 (25-35) | 30 (27-34) | .92 |
| 3 y | 38 (33-44) | 38 (34-41) | .90 |
| NRM | .06 | ||
| 1 y | 13 (10-17) | 10 (8-12) | .12 |
| 3 y | 19 (15-24) | 14 (12-17) | .06 |
| LFS | .23 | ||
| 1 y | 56 (51-62) | 59 (56-63) | .34 |
| 3 y | 43 (37-48) | 48 (45-51) | .11 |
| OS | .03 | ||
| 1 y | 67 (62-72) | 70 (67-73) | .23 |
| 3 y | 48 (42-54) | 55 (52-59) | .03 |
All data are % (95% CI).
Mortality and relapse.
The Haplo-HCT group had a lower OS (48%; 95% CI, 42-54 vs 55%; 95% CI, 52-59 at 3 years; P = .03) and a trend for higher NRM (19%; 95% CI, 15-24 vs 14%; 95% CI, 12-17 at 3 years; P = .06) but similar relapse (P = .90) and LFS (P = .11). Center effect (tested for OS) was not significant (P = .08).
Engraftment.
Neutrophil and platelet engraftment rates were lower in the Haplo-HCT group (92%; 95% CI, 89-95 vs 99%; 95% CI, 98-99 for neutrophils at 1 month; P < .001 and 89%; 95% CI, 85-92 vs 97%; 95% CI, 96-98 for platelets at 100 days, P < .001).
Multivariable analysis
OS and LFS.
Haplo-HCT and MSD groups were not different with regard to OS (hazard ratio [HR], 1.15; 95% CI, 0.95-1.38; P = .15) (Figure 1). Significant predictors of worse OS included older age (P = .02), worse performance status (Karnofsky performance status < 90 vs 90+, P = .01), MRD positivity before HCT (P = .005), worse cytogenetic risk (P < .001), secondary AML (P < .001), and recipient male sex (P = .03) (Table 3).
Figure 1.
Outcomes after Haplo-HCT vs MSD in patients with AML in CR1. Adjusted curves for OS (A), LFS (B), relapse (C), NRM (D), grade II-IV acute GVHD (E), and chronic GVHD (F).
Table 3.
Multivariable analysis of outcomes
| Covariates | HR (95% CI) | P |
|---|---|---|
| OS | ||
| Main effect | .15 | |
| MSD | Reference | |
| Haplo-HCT | 1.15 (0.95-1.38) | |
| Age, y | .02 | |
| 18-54 | Reference | |
| 55+ | 1.23 (1.03-1.45) | |
| Sex | .03 | |
| Male | Reference | |
| Female | 0.84 (0.71-0.99) | |
| Karnofsky score | .03 | |
| 90+ | Reference | |
| <90 | 1.23 (1.04-1.45) | .01 |
| Missing | 0.80 (0.44-1.47) | .47 |
| Cytogenetics | <.001 | |
| Favorable | Reference | |
| Intermediate | 1.29 (0.74-2.25) | .38 |
| Poor: monosomal karyotype | 2.51 (1.39-4.54) | .002 |
| Poor: other | 1.89 (1.07-3.34) | .03 |
| Missing | 1.78 (0.96-3.31) | .07 |
| MRD at HCT | .009 | |
| Negative | Reference | |
| Positive | 1.32 (1.09-1.61) | .005 |
| Missing | 1.30 (0.97-1.73) | .07 |
| AML type | <.001 | |
| De novo | Reference | |
| Secondary | 1.38 (1.15-1.65) | |
| NRM | ||
| Main effect | .16 | |
| MSD | Reference | |
| Haplo-HCT | 1.26 (0.92-1.74) | |
| Age, y | <.001 | |
| 18-54 | Reference | |
| 55+ | 1.97 (1.43-2.70) | |
| Sex | .01 | |
| Male | Reference | |
| Female | 0.69 (0.52-0.92) | |
| HCT-CI | .005 | |
| 0 | Reference | |
| 1 | 1.36 (0.86-2.17) | .19 |
| 2 | 1.02 (0.61-1.73) | .93 |
| 3+ | 1.88 (1.31-2.71) | <.001 |
| Missing | 1.42 (0.67-3.05) | .36 |
| Conditioning | .06 | |
| MAC-TBI | Reference | |
| MAC without TBI | 0.67 (0.47-0.98) | .04 |
| RIC | 0.57 (0.38-0.86) | .008 |
| Missing | 0.56 (0.08-4.14) | .57 |
| D/R CMV status | <.001 | |
| +/+ | Reference | |
| +/− | 0.46 (0.25-0.84) | .01 |
| −/+ | 0.94 (0.67-1.31) | .70 |
| −/− | 0.67 (0.46-0.97) | .03 |
| Missing | 3.07 (1.39-6.76) | .005 |
| LFS | ||
| Main effect | .50 | |
| MSD | Reference | |
| Haplo-HCT | 1.06 (0.89-1.27) | |
| Age, y | .04 | |
| 18-54 | Reference | |
| 55+ | 1.18 (1.00-1.38) | |
| Cytogenetics | <.001 | |
| Favorable | Reference | |
| Intermediate | 1.26 (0.76-2.09) | .37 |
| Poor: monosomal karyotype | 2.37 (1.38-4.06) | .002 |
| Poor: other | 1.78 (1.06-2.99) | .03 |
| Missing | 1.62 (0.92-2.87) | .09 |
| MRD at HCT | <.001 | |
| Negative | Reference | |
| Positive | 1.41 (1.18-1.70) | <.001 |
| Missing | 1.27 (0.96-1.67) | .09 |
| AML type | .008 | |
| De novo | Reference | |
| Secondary | 1.26 (1.06-1.50) | |
| Relapse | ||
| Main effect | .27 | |
| MSD | Reference | |
| Haplo-HCT | 0.88 (0.70-1.10) | |
| Cytogenetics | <.001 | |
| Favorable | Reference | |
| Intermediate | 1.26 (0.69-2.32) | .45 |
| Poor: monosomal karyotype | 2.48 (1.30-4.72) | .006 |
| Poor: other | 2.01 (1.08-3.74) | .03 |
| Missing | 1.76 (0.88-3.50) | .11 |
| MRD at HCT | .003 | |
| Negative | Reference | |
| Positive | 1.45 (1.17-1.80) | <.001 |
| Missing | 1.19 (0.84-1.67) | .33 |
| Conditioning | .004 | |
| MAC-TBI | Reference | |
| MAC without TBI | 1.01 (0.78-1.30) | .95 |
| RIC | 1.43 (1.10-1.85) | .008 |
| Missing | 0.35 (0.05-2.50) | .29 |
| aGVHD II-IV | ||
| Main effect | .95 | |
| MSD | Reference | |
| Haplo-HCT | 1.01 (0.80-1.26) | |
| aGVHD III-IV | ||
| Main effect | .30 | |
| MSD | Reference | |
| Haplo-HCT | 0.81 (0.55-1.21) | |
| Chronic GVHD | ||
| Main effect | <.001 | |
| MSD | Reference | |
| Haplo-HCT | 0.38 (0.30-0.48) | |
| Conditioning | .04 | |
| MAC-TBI | Reference | |
| MAC without TBI | 1.24 (1.00-1.53) | .05 |
| RIC | 0.97 (0.76-1.23) | .80 |
| Missing | 0.67 (0.21-2.11) | .49 |
| D/R sex | .002 | |
| M/M | Reference | |
| M/F | 0.95 (0.75-1.19) | .64 |
| F/M | 1.38 (1.09-1.74) | .007 |
| F/F | 1.31 (1.04-1.64) | .02 |
aGVHD, acute GVHD; CMV, cytomegalovirus; D/R, donor/recipient; F, female; M, male; TBI, total body irradiation.
Haplo-HCT and MSD groups were not different with regard to LFS (HR, 1.06; 95% CI, 0.89-1.27; P = .50) (Figure 1). Significant predictors of worse LFS included older age (P = .04), MRD positivity before HCT (P < .001), worse cytogenetic risk (P < .001), and secondary AML (P = .008) (Table 3).
Relapse and NRM.
Haplo-HCT and MSD groups were not different with regard to NRM (HR, 1.26; 95% CI, 0.92-1.74; P = .16) (Figure 1). Significant predictors of higher NRM included older age (P < .001), recipient male sex (P = .01), and worse comorbidity score (P = .005). MAC with total body irradiation (TBI) was predictive of higher NRM (P = .04 vs MAC without TBI, P = .008 vs RIC). Recipient cytomegalovirus seronegativity was predictive of less NRM (P = .01 if donor seropositive, P = .03 if donor seronegative) (Table 3).
Haplo-HCT and MSD groups were not different with regard to relapse (HR, 0.88; 95% CI, 0.70-1.10; P = .27) (Figure 1). Predictors of relapse were MRD positivity before HCT (P < .001), worse cytogenetic risk (P < .001), and RIC (P = .008) (Table 3).
Acute and chronic GVHD.
Haplo-HCT and MSD groups were not different with regard to grade II-IV acute GVHD (HR, 1.01; 95% CI, 0.80-1.26; P = .98) (Figure 1). No factor other than the main effect (donor type) remained in the final model (Table 3). Similarly, the groups were not different with regard to grade III-IV acute GVHD (HR, 0.81; 95% CI, 0.55-1.21; P = .30).
However, the Haplo-HCT group had a lower rate of chronic GVHD (HR, 0.38; 95% CI, 0.30-0.48; P < .001) (Figure 1). Other factors significantly associated with an increased risk for chronic GVHD were using a female donor (P = .007 for male patient and P = .02 for female patient vs a male-to-male transplant) and MAC without TBI (compared with MAC with TBI, P = .05) (Table 3).
The interaction between MRD positivity and donor type did not influence any of the outcomes.
Subgroup analysis
Next, we performed multivariable subgroup analyses to evaluate whether the association between Haplo-HCT and less chronic GVHD is limited to MAC vs RIC or peripheral blood vs bone marrow. When the analysis was limited to the MAC subgroup, Haplo-HCT was associated with a lower risk for chronic GVHD (HR, 0.44; 95% CI, 0.31-0.61; P < .001) compared with MSD. A similar result was obtained with analysis limited to RIC cases (Haplo-HCT vs MSD: HR, 0.34; 95% CI, 0.25-0.48; P < .001). When the analysis was limited to peripheral blood cases, Haplo-HCT was associated with a lower risk for chronic GVHD compared with MSD (HR, 0.68; 95% CI, 0.50-0.91; P = .009). The association was even stronger when the analysis was limited to bone marrow grafts (HR, 0.22; 95% CI, 0.15-0.31; P < .001). These results indicate that the association between Haplo-HCT and less chronic GVHD is not limited to a specific conditioning intensity or graft source.
Causes of death
Overall, 170 deaths occurred in the Haplo-HCT group, and 425 occurred in the MSD group. The 3 most common causes of death were similar between the groups: relapse (58% vs 60%, respectively), GVHD (1% acute and 0.6% chronic vs 4% acute and 6% chronic, respectively), and infection (8% vs 10%, respectively).
Discussion
Our results from this large CIBMTR analysis of AML patients transplanted in CR1 indicate similar outcomes after current standard practices of PT-Cy–based Haplo-HCT vs MSD HCT, with the exception of less chronic GVHD after Haplo-HCT. The unique features of our study were its focus on patients with AML in CR1 and inclusion of MRD information. Because MRD was not uniformly tested or reported by CIBMTR centers, we created a logical definition of MRD using the available data. The balance between the groups using our MRD definition was important in the analysis of outcomes. Our subgroup analyses suggested that the reduced incidence of chronic GVHD in Haplo-HCT was not limited to a specific graft source or conditioning intensity.
The reduction in the incidence of chronic GVHD in our study was not associated with improved survival. Although prospective studies of Haplo-HCT vs MSD have not been performed, our finding is consistent with large randomized studies in other settings, such as matched donor transplant using peripheral blood vs bone marrow as a graft source.23 Late infections and secondary malignancies are among the causes of NRM that could offset a potential survival benefit of less chronic GVHD. However, data on these factors were not available in the present study. Similarly, reduced rates of chronic GVHD in the Haplo-HCT group in our study were not associated with increased relapse. Our analysis was strengthened by disease uniformity (AML in CR1) and balanced MRD status between the groups, 2 key factors in the analysis of relapse. A previous study comparing Haplo-HCT and MSD in patients with acute leukemia showed consistent results.16 In contrast, a recent study comparing the outcomes of Haplo-HCT and MSD in patients with relapsed/refractory AML showed worse outcomes (LFS, OS, NRM, infections) after Haplo-HCT.24
Chronic GVHD and its complications are the primary determinants of long-term quality of life after allogeneic HCT,25-27 although this relationship has not been studied after Haplo-HCT. Future research should address whether reduced chronic GVHD after Haplo-HCT results in better quality of life.
In a large study comparing PT-Cy–based Haplo-HCT with MUD in patients with AML, the incidence of acute and chronic GVHD was lower after Haplo-HCT, with no survival difference.9 Our cohorts were not different with regard to the incidence of acute GVHD, likely because of less acute GVHD in MSD compared with MUD. However, chronic GVHD results were consistent between the 2 studies, with Haplo-HCT yielding the best results. Considering our negative subgroup analyses for graft source and conditioning intensity, the lower incidence of chronic GVHD after Haplo-HCT is likely due to PT-Cy. This finding may explain negative findings for chronic GVHD in a previous large study of Haplo-HCT vs MSD in patients with intermediate- or poor-risk AML in CR1, because more than 25% of Haplo-HCT patients in that study did not receive PT-Cy.15 Most of our MSD recipients received peripheral blood stem cells, and nearly half developed chronic GVHD at 1 year. The efficacy of PT-Cy in reducing chronic GVHD rates in this setting has been demonstrated in a previous work.28
The associations between donor type and outcome in our study did not depend on MRD status before HCT. To our knowledge, only 1 previous study found differential outcomes between donor types depending on MRD status.29 In that study, patients with AML or myelodysplastic syndrome received a myeloablative cord blood or MUD transplant. The use of cord blood resulted in less relapse and higher OS compared with the use of an unrelated donor if patients were MRD positive at the time of HCT. This donor-specific association was not present in MRD-negative patients. Although prospective trials should use current and novel high-sensitivity techniques for MRD assessment, the method developed in this study may be tested in, and applied to, future CIBMTR studies of the pre-MRD era.
Donor age and relationship to the recipient in Haplo-HCT outcomes have been a subject of recent investigation. McCurdy et al showed that, among Haplo-HCT recipients, patient age (18-54 vs 55-78 years) negated the effect of donor age and relationship on survival.30 Robinson et al compared the outcomes of MSD vs Haplo-HCT in patients with acute leukemia. In their study, patients aged 18 to 54 years experienced lower rates of chronic GVHD if transplanted from a haploidentical sibling than from an MSD.16 Similarly, older patients had lower rates of chronic GVHD if transplanted from a haploidentical child than from an MSD. However, in this older group of patients (55-76 years), NRM and OS were worse after HCT from haploidentical offspring compared with an MSD. Although our study was not designed to address donor relationship in different patient age groups, the results by McCurdy et al and Robinson et al help to interpret our findings. Chronic GVHD results seem to be generalizable to different donor relationships and patient age groups, but the lack of a difference in NRM and OS between the groups in our study may be subgroup specific based on patient age and donor relationship.
Our finding of reduced chronic GVHD after Haplo-HCT compared with an MSD is consistent with previous studies, although specifics of transplant and patient populations (2 studies in lymphoma and 1 in acute leukemia) varied among studies.11,14,16 Limitations of our study include its retrospective design, the relatively small number of centers from which Haplo-HCT cases were reported, small number of MSD HCTs using bone marrow as a graft source (limiting subgroup analysis), and lack of chronic GVHD grading and MRD assessment according to the current standards. Nonetheless, the available data indicate that PT-Cy–based Haplo-HCT using bone marrow results in less chronic GVHD vs an MSD using peripheral blood and CNI-based GVHD prophylaxis. In this study, we did not consider viral reactivations and hemorrhagic cystitis, which could differ between the 2 groups.
In conclusion, a haploidentical relative is a viable alternative to an MSD in AML patients in CR1. The longer interval between diagnosis and transplant in our Haplo-HCT recipients suggests that, in some cases, centers might have spent time looking for unrelated donors before turning to haploidentical donors. Our results can help to prevent this delay in choosing a suitable donor. Choosing a haploidentical donor over a matched sibling may be necessary when stem cell collection from a matched sibling is considered risky because of comorbidities, and our results provide support for this approach. In addition, more than one fifth of our Haplo-HCT patients were African American, supporting the feasibility of using this donor type in ethnic minorities. Finally, a future study comparing Haplo-HCT with MSD, using the same graft source and PT-Cy–based GVHD prophylaxis, would be mechanistically informative about whether PT-Cy negates the effect of HLA disparity on outcomes.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank Bipin Savani and Vaibhav Agrawal.
The CIBMTR is supported primarily by the National Institutes of Health (public health service grant/cooperative agreement 5U24CA076518 from the National Cancer Institute, National Heart, Lung, and Blood Institute, and National Institute of Allergy and Infectious Diseases and grant/cooperative agreement 4U10HL069294 from the National Heart, Lung, and Blood Institute and National Cancer Institute), the Health Resources and Services Administration/Department of Health and Human Services (contract HHSH250201200016C), and the Office of Naval Research (grants N00014-17-1-2388 and N0014-17-1-2850). The CIBMTR is also supported by Actinium Pharmaceuticals, Amgen, Amneal Biosciences, Angiocrine Bioscience, an anonymous donation to the Medical College of Wisconsin, Astellas Pharma US, Atara Biotherapeutics, Be the Match Foundation, bluebird bio, Bristol Myers Squibb Oncology, Celgene Corporation, Cerus Corporation, Chimerix, the Fred Hutchinson Cancer Research Center, Gamida Cell, Gilead Sciences, HistoGenetics, Immucor, Incyte Corporation, Janssen Scientific Affairs, Jazz Pharmaceuticals, Juno Therapeutics, Karyopharm Therapeutics, Kite Pharma, Medac, MedImmune, The Medical College of Wisconsin, Mediware, Merck & Co., Mesoblast, Meso Scale Diagnostics, Millennium, Miltenyi Biotec, the National Marrow Donor Program, Neovii Biotech NA, Novartis Pharmaceuticals Corporation, Otsuka Pharmaceutical (Japan), Patient-Centered Outcomes Research Institute, Pfizer, Pharmacyclics, PIRCHE, Sanofi Genzyme, Seattle Genetics, Shire, Spectrum Pharmaceuticals, St. Baldrick’s Foundation, Sunesis Pharmaceuticals, Swedish Orphan Biovitrum, Takeda Oncology, Telomere Diagnostics, and the University of Minnesota.
The views expressed in this article do not reflect the official policy or position of the National Institutes of Health, Department of the Navy, Department of Defense, Health Resources and Services Administration, or any other agency of the US government.
Authorship
Contribution: A.R., R.R., M.H., H.-L.W., M.-J.Z., and W.S. designed the study, analyzed the data, and wrote the manuscript; and D.W., M.D.L., B.M.S., M.L., J.B.-M., J.-W.L., S.C., H.K.H., Y.K., J. Maertens, K.S.-G., A. Bajel, M.A., C.C., R.N., J.P., B.O., T.H., B.C.S., R.P.G., M. Battiwalla, S.G., S.H., N.P., C.G.K., N.H., M.R.G., L.F.V., H.S.M., V.R.B., J.R., R.O., M.A.K.-D., O.R., M.C., E.K.W., D.R., H.M.L.,M.-A.D., E.C., K.R.S., S.P., M.L.S., J.-Y.C., R. Munker, S.N., A.M.B., J. McGuirk, M.S., S.S., A.D., H.A-A., R.F.O., J.W., A. Bashey, G.C.H., N.F., N.B., M. Byrne, N.K., R. Martino, A.A., T.N., and A.S. designed the study and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Wael Saber, Division of Hematology/Oncology Medical College of Wisconsin–CIBMTR, 9200 W. Wisconsin Ave, Milwaukee, WI 53226; e-mail: wsaber@mcw.edu; and Rizwan Romee, Division of Hematologic Malignancies and Transplantation, Dana-Farber Cancer Institute, Harvard Medical School, 450 Brookline Ave, Boston, MA 02215; e-mail: rizwan_romee@dfci.harvard.edu.
References
- 1.Szydlo R, Goldman JM, Klein JP, et al. Results of allogeneic bone marrow transplants for leukemia using donors other than HLA-identical siblings. J Clin Oncol. 1997;15(5):1767-1777. [DOI] [PubMed] [Google Scholar]
- 2.Howard CA, Fernandez-Vina MA, Appelbaum FR, et al. Recommendations for donor human leukocyte antigen assessment and matching for allogeneic stem cell transplantation: consensus opinion of the Blood and Marrow Transplant Clinical Trials Network (BMT CTN). Biol Blood Marrow Transplant. 2015;21(1):4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kasamon YL, Bolaños-Meade J, Prince GT, et al. Outcomes of nonmyeloablative HLA-haploidentical blood or marrow transplantation with high-dose post-transplantation cyclophosphamide in older adults. J Clin Oncol. 2015;33(28):3152-3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bashey A, Zhang M-J, McCurdy SR, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-cell-replete haploidentical donor transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2017;35(26):3002-3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giannotti F, Labopin M, Shouval R, et al. Haploidentical transplantation is associated with better overall survival when compared to single cord blood transplantation: an EBMT-Eurocord study of acute leukemia patients conditioned with thiotepa, busulfan, and fludarabine. J Hematol Oncol. 2018;11(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Cheikh J, Crocchiolo R, Furst S, et al. Unrelated cord blood compared with haploidentical grafts in patients with hematological malignancies. Cancer. 2015;121(11):1809-1816. [DOI] [PubMed] [Google Scholar]
- 7.Brunstein CG, Gutman JA, Weisdorf DJ, et al. Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood. 2010;116(22):4693-4699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun Y, Beohou E, Labopin M, et al. ; Acute Leukemia Working Party of the EBMT . Unmanipulated haploidentical versus matched unrelated donor allogeneic stem cell transplantation in adult patients with acute myelogenous leukemia in first remission: a retrospective pair-matched comparative study of the Beijing approach with the EBMT database. Haematologica. 2016;101(8):e352-e354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciurea SO, Zhang M-J, Bacigalupo AA, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126(8):1033-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rashidi A, DiPersio JF, Westervelt P, et al. Comparison of outcomes after peripheral blood haploidentical versus matched unrelated donor allogeneic hematopoietic cell transplantation in patients with acute myeloid leukemia: a retrospective single-center review. Biol Blood Marrow Transplant. 2016;22(9):1696-1701. [DOI] [PubMed] [Google Scholar]
- 11.Martínez C, Gayoso J, Canals C, et al. ; Lymphoma Working Party of the European Group for Blood and Marrow Transplantation . Post-transplantation cyclophosphamide-based haploidentical transplantation as alternative to matched sibling or unrelated donor transplantation for Hodgkin lymphoma: a registry study of the Lymphoma Working Party of the European Society for Blood and Marrow Transplantation. J Clin Oncol. 2017;35(30):3425-3432. [DOI] [PubMed] [Google Scholar]
- 12.Kanate AS, Mussetti A, Kharfan-Dabaja MA, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors vs HLA-matched unrelated donors. Blood. 2016;127(7):938-947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lorentino F, Labopin M, Bernardi M, et al. ; Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation . Comparable outcomes of haploidentical, 10/10 and 9/10 unrelated donor transplantation in adverse karyotype AML in first complete remission. Am J Hematol. 2018;93(10):1236-1244. [DOI] [PubMed] [Google Scholar]
- 14.Ghosh N, Karmali R, Rocha V, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors versus HLA-matched sibling donors: A Center for International Blood and Marrow Transplant Research Analysis. J Clin Oncol. 2016;34(26):3141-3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salvatore D, Labopin M, Ruggeri A, et al. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103(8):1317-1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robinson TM, Fuchs EJ, Zhang M-J, et al. ; Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research . Related donor transplants: has posttransplantation cyclophosphamide nullified the detrimental effect of HLA mismatch? Blood Adv. 2018;2(11):1180-1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munker R, Brazauskas R, Wang HL, et al. ; Center for International Blood and Marrow Transplant Research . Allogeneic hematopoietic cell transplantation for patients with mixed phenotype acute leukemia. Biol Blood Marrow Transplant. 2016;22(6):1024-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flowers MED, Inamoto Y, Carpenter PA, et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood. 2011;117(11):3214-3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slovak ML, Kopecky KJ, Cassileth PA, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96(13):4075-4083. [PubMed] [Google Scholar]
- 20.Araki D, Wood BL, Othus M, et al. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual disease-based definition of complete remission? J Clin Oncol. 2016;34(4):329-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sorror ML, Maris MB, Storb R, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912-2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen PK, Klein JP, Zhang MJ. Testing for centre effects in multi-centre survival studies: a Monte Carlo comparison of fixed and random effects tests. Stat Med. 1999;18(12):1489-1500. [DOI] [PubMed] [Google Scholar]
- 23.Anasetti C, Logan BR, Lee SJ, et al. ; Blood and Marrow Transplant Clinical Trials Network . Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367(16):1487-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Battipaglia G, Boumendil A, Labopin M, et al. Unmanipulated haploidentical versus HLA-matched sibling allogeneic hematopoietic stem cell transplantation in relapsed/refractory acute myeloid leukemia: a retrospective study on behalf of the ALWP of the EBMT [published online ahead of print 4 Feb 2019]. Bone Marrow Transplant. doi:10.1038/s41409-019-0459-7. [DOI] [PubMed] [Google Scholar]
- 25.Chiodi S, Spinelli S, Ravera G, et al. Quality of life in 244 recipients of allogeneic bone marrow transplantation. Br J Haematol. 2000;110(3):614-619. [DOI] [PubMed] [Google Scholar]
- 26.Lee SJ, Kim HT, Ho VT, et al. Quality of life associated with acute and chronic graft-versus-host disease. Bone Marrow Transplant. 2006;38(4):305-310. [DOI] [PubMed] [Google Scholar]
- 27.Lee SJ, Logan B, Westervelt P, et al. Comparison of patient-reported outcomes in 5-year survivors who received bone marrow vs peripheral blood unrelated donor transplantation: long-term follow-up of a randomized clinical trial. JAMA Oncol. 2016;2(12):1583-1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mielcarek M, Furlong T, O’Donnell PV, et al. Posttransplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood. 2016;127(11):1502-1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Milano F, Gooley T, Wood B, et al. Cord-blood transplantation in patients with minimal residual disease. N Engl J Med. 2016;375(10):944-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCurdy SR, Zhang M-J, St Martin A, et al. Effect of donor characteristics on haploidentical transplantation with posttransplantation cyclophosphamide. Blood Adv. 2018;2(3):299-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.