Abstract
Objectives. To assess the impact of the 2008 Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) on mental and substance use disorder services in the private, large group employer–sponsored insurance market in the United States.
Methods. We analyzed data from the IBM MarketScan Commercial Database from January 2005 through September 2015 by using population-level interrupted time series regressions to determine whether parity implementation was associated with utilization and spending outcomes.
Results. MHPAEA had significant positive associations with utilization of mental and substance use disorder outpatient services. A spending decomposition analysis indicated that increases in utilization were the primary drivers of increases in spending associated with MHPAEA. Analyses of opioid use disorder and nonopioid substance use disorder services found that associations with utilization and spending were not attributable only to increases in treatment of opioid use disorder.
Conclusions. MHPAEA is positively associated with utilization of outpatient mental and substance use disorder services for Americans covered by large group employer–sponsored insurance.
Public Health Implications. These trends continued over the 5-year post-MHPAEA period, underscoring the long-term relationship between this policy change and utilization of behavioral health services.
Over the past 2 decades, a series of legislative initiatives have advanced parity of insurance coverage for behavioral health disorders, namely mental and substance use disorders (M/SUDs), in the United States.1,2 Parity in the context of recent federal laws means that insurance benefits for M/SUD services must be no more restrictive than those for medical and surgical treatment. To assess parity, an analysis is conducted to evaluate an array of factors, including financial limits (e.g., unequal cost sharing), quantitative treatment limits (e.g., visit and stay limits), and processes and techniques for managing care (often called nonquantitative treatment limits). Given the high rates of unmet need for behavioral health care3,4 and the continued strain to the system caused by the opioid crisis,5,6 parity in insurance coverage is one important mechanism in improving overall access to behavioral health services.
Initially, the Mental Health Parity Act of 1996 (Pub L No. 104-204) prohibited higher annual and lifetime dollar limits for mental disorder treatment benefits compared to medical and surgical benefits. However, insurance companies still could impose other restrictions on mental health coverage, such as covering only selected treatments or applying higher cost sharing for mental health visits, and parity requirements did not extend to SUD services. In 2008, the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA; Pub L No. 110-343) expanded parity in M/SUD coverage beyond the 1996 law to a broader set of financial and treatment limits and to SUD services. This law—interacting with the Patient Protection and Affordable Care Act (Pub L No. 111-148), which expands parity to the individual market, small group insurance market, and those covered via Medicaid expansion—was expected to expand access to M/SUD insurance coverage for 62 million people.7
Research on M/SUD benefits suggests that parity laws, including MHPAEA, have affected quantitative treatment limits. Most plans substantially reduced or eliminated treatment limits after MHPAEA, and no evidence has indicated that the law led plans to drop M/SUD coverage rather than redress possible parity violations.8–10 Parity laws also have been found to shift most, but not all, financial requirements for M/SUD treatment coverage to a level that is comparable to that for medical and surgical treatment.10–12 However, findings regarding MHPAEA’s impact on nonquantitative treatment limits are mixed and suggest that these limits still are being applied in a manner inconsistent with MHPAEA.9,11,13
Early analyses of these changes in coverage on utilization and spending attributable to parity laws found modest increases in utilization of behavioral health services.14,15 Some studies also found positive utilization impacts on specific disorder categories considered more vulnerable to noncomparable benefit limits before MHPAEA, including increased mental health visits for autism spectrum disorder16 and increased psychotherapy visits for eating disorders.17 Others focused on cost concerns, finding decreased out-of-pocket costs for bipolar disorder, adjustment disorder, and major depression diagnosis.18 None of these studies tracked the impact of MHPAEA beyond 2012. The 2010 interim final rule implementing the law provided explicit guidance on how to conduct parity analyses by treatment category and extended parity to include nonquantitative treatment limits, applicable for all plans as of January 2011.
We examined the relationship between MHPAEA in the large group employer–sponsored insurance market and M/SUD service utilization and spending on outpatient services, extending the follow-up period through September 2015. Because most M/SUD services are provided in an outpatient setting, we focused our evaluation on this setting. Given that the implementation of MHPAEA also coincided with the current opioid crisis in the United States, increased demand for behavioral health services resulting from the crisis may confound the law’s impact on SUD service utilization and spending. Therefore, we evaluated opioid use disorder (OUD) and nonopioid SUD services separately.
METHODS
We estimated the association of MHPAEA with changes in utilization and spending by using a population-level interrupted time series (ITS) design. Time-series designs are robust quasi-experimental designs for evaluating population-level public health policy interventions19,20 and have been widely used to assess parity impacts.11,16,18 They control for selection bias, confounding attributable to group differences, short-term fluctuations, secular trends, and regression to the mean but remain vulnerable to threats attributable to history (or concurrent events) and instrumentation.19,20 Because the concurrent opioid crisis is a significant potential threat to the relationship between parity and SUD treatment, we stratified our analysis according to OUD and nonopioid SUD services.
Data
We used data in the IBM MarketScan Commercial Database from January 2005 through September 2015. The database contains private insurance claims from approximately 150 large employers for employees, their dependents, and early retirees, encompassing roughly 50 million lives per year. Although MarketScan data are a convenience sample that has fluctuated in size and contributors over time, the database has maintained the same age and sex distribution as reported by the US Census Bureau for individuals with employer-sponsored insurance.
Study Sample
The sample consisted of enrollees younger than 65 years with continuous enrollment in a large group employer–sponsored insurance plan for all 12 months in each calendar year (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org, for attrition table and detailed methods). We excluded enrollees covered under plans that were not fully insured by the employer and plans that did not include prescription drug data. We used International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM; Hyattsville, MD: National Center for Health Statistics; 1980) diagnosis codes to identify M/SUD services, including OUD and nonopioid SUD services. Non–behavioral health services were identified by the absence of an M/SUD diagnosis code on the service claim, similar to other studies that have used claims-based data sets.21,22 We included a total of 24.1 million enrollees from 2005 to 2010 (before MHPAEA implementation) and 25.9 million enrollees from 2011 to 2015 (after implementation) in the analysis.
Outcomes
Our population-level ITS analysis required monthly measures of utilization and spending on outpatient services. Outpatient services in this study comprised all behavioral health services broadly delivered in an outpatient setting, including physician and psychiatrist office visits and intensive outpatient, partial hospitalization, and outpatient residential services. In addition to excluding inpatient services, we excluded emergency department visits, prescription drugs, and laboratory and radiology services. We defined all outcome measures separately for M/SUD and non–behavioral health services. We defined OUD and nonopioid SUD outcomes for the subanalysis of SUD services. For utilization outcomes, we included any use of outpatient services as well as the average frequency of services used per service user. For spending outcomes, we examined average insurer spending per service user, average insurer reimbursement per visit, average out-of-pocket spending per service user, and average out-of-pocket amount paid per visit.
Analytic Approach
We defined the preparity period for our study as January 2005 through December 2010 and the postparity period as January 2011 through September 2015. Although the interim final rule was passed in 2010, it did not become effective for most plans that use a calendar year system until 2011. We did not include data from the last quarter of 2015 because the ICD-9-CM classification system of diseases was updated in October 2015. Therefore, we had 72 months of preparity data and 57 months of postparity data.
We used Stata version 14 (StataCorp LP, College Station, TX) for the ITS regression analysis with the user command ITSA.23 We included 3 predictor variables in the analysis: (1) a linear time variable (month), (2) a binary variable (parity [pre–post indicator]; 0 = 2005–2010; 1 = 2011–2015), and (3) an interaction variable (parity∗month). In addition to the 3 predictor variables, we controlled for seasonality by including indicator variables for each month. In all spending-related outcomes, we controlled for inflation by including a quarterly measure of inflation—the gross domestic product deflator.
We tested all regression analyses for first-order serial correlation by using a Durbin–Watson test statistic and estimated a full set of corrected ITS regressions. All coefficient signs and magnitudes were very similar across the models, and we present the unadjusted results here. We also performed a full set of regression analyses that included an additional indicator for the interim period, years 2009 to 2010, and an additional month∗interim period variable. This alternative specification revealed little evidence of changes in outcomes in the 2-year interim period before the 2011 effective interim rule compliance date (results not shown).
Because MHPAEA affected all large group employer–sponsored insurance plans nationally, finding a suitable comparison population would be difficult. Instead, we compared trends in behavioral health services with trends in non–behavioral health services because MHPAEA was expected to influence M/SUD outcomes but not necessarily medical or surgical outcomes. This approach was taken in previous studies and proved useful in distinguishing behavioral health trends from other broader health care trends.21,24,25 To further confirm that our findings were not a result of changes in the sample of employers from year to year, we ran analyses on a subset of 65 employers that continuously contributed to the database in the study period.
RESULTS
Table 1 presents the average number and percentage of enrollees with at least 1 health care service who accessed behavioral health services per year before and after parity—separated by mental health and SUD services—with SUD services separated into any OUD services and any nonopioid SUD services. On average, in each preparity year, about a quarter of enrollees (25.2%) with at least 1 health care service also had at least 1 behavioral health claim, increasing to 26.9% per year after parity. Behavioral health service use was driven primarily by use of mental health services. Only an average of 0.8% of enrollees used any SUD services during each preparity year, and 1.2% after parity (Appendix B, available as a supplement to the online version of this article at http://www.ajph.org, for year-specific values).
TABLE 1—
Enrollees in Employer-Sponsored Insurance in the United States Who Accessed Health Care Services in the Preparity (2005–2010) and Postparity (2011–2015) Periods by Types of Services Used, Average Annual Percentage
| Type of Service Used | Preparity (2005–2010), No. (%) | Postparity (2011–2015), No. (%) |
| ≥ 1 health care service (average across years) | 10 737 695 | 14 233 282 |
| Any behavioral health service | 2 705 157 (25.2) | 3 823 844 (26.9) |
| Any mental health service | 2 677 421 (24.9) | 3 767 138 (26.5) |
| Any SUD service | 82 200 (0.8) | 173 300 (1.2) |
| Any nonopioid SUD service | 72 097 (0.7) | 147 130 (1.0) |
| Any OUD service | 10 949 (0.1) | 27 638 (0.2) |
Note. OUD = opioid use disorder; SUD = substance use disorder. Enrollees were excluded if they did not have at least 1 calendar year of continuous enrollment. See Appendix B (available as a supplement to the online version of this article at http://www.ajph.org) for annual percentages.
Tables 2 and 3 present the results from the ITS analysis, which captured trends in monthly population outcomes over the study period, with control for the general linear trend, seasonal variation, and inflation where applicable. For each regression, the total sample size was 129—the number of months in our study period. The parity (pre–post indicator) variable is a measure of the associated change in the level of the outcome variable; regression results for this variable can be interpreted as a more immediate, 1-time impact of MHPAEA. The parity∗month interaction variable is a measure of the associated change in the slope of the outcome variable; regression results for this variable can be interpreted as a more gradual impact of MHPAEA over the postparity period.
TABLE 2—
Interrupted Time Series Regression of Mental Health Parity and Addiction Equity Act Impact on Utilization of and Spending on Mental and Substance Use Disorder Outpatient Services in Employer-Sponsored Insurance: United States, 2005–2015
| Variable | Non–Behavioral Health Services, b (95% CI) | Mental Health Services, b (95% CI) | Substance Use Disorder Services, b (95% CI) |
| Any use of outpatient services, percentage points | |||
| Parity (pre–post indicator) | −0.483 (−1.301, 0.335) | 0.093 (−0.081, 0.268) | 0.011 (0.006, 0.017) |
| Parity*month | −0.025 (−0.048, −0.003) | −0.001 (−0.006, 0.003) | 0.001 (0.0007, 0.001) |
| Month (linear time variable) | 0.012 (−0.001, 0.025) | 0.016 (0.013, 0.019) | 0.001 (0.001, 0.002) |
| Average frequency of monthly outpatient service use per service user, no. of services | |||
| Parity (pre–post indicator) | −0.025 (−0.101, 0.050) | < 0.001 (−0.052, 0.052) | −0.059 (−0.161, 0.042) |
| Parity*month | 0.001 (−0.002, 0.003) | 0.005 (0.004, 0.007) | 0.054 (0.051, 0.057) |
| Month (linear time variable) | 0.006 (0.005, 0.007) | 0.002 (0.001, 0.003) | −0.005 (−0.006, −0.003) |
| Average monthly insurer spending per service user, $ | |||
| Parity (pre–post indicator) | −18.303 (−45.120, 8.513) | −3.674 (−12.444, 5.150) | 47.674 (23.495, 71.853) |
| Parity*month | −0.320 (−1.061, 0.420) | 0.348 (0.105, 0.591) | 6.879 (6.211, 7.547) |
| Month (linear time variable) | 1.646 (−0.110, 3.402) | 1.519 (0.943, 2.095) | 0.372 (−1.211, 1.955) |
| Average insurer reimbursement paid per visit, $ | |||
| Parity (pre–post indicator) | 4.982 (3.241, 6.722) | 2.548 (0.435, 4.661) | 5.954 (−2.788, 14.697) |
| Parity*month | −0.297 (−0.345, −0.249) | −0.072 (−0.131, −0.014) | −0.074 (−0.315, 0.168) |
| Month (linear time variable) | 0.102 (−0.012, 0.216) | 0.273 (0.135, 0.412) | 0.851 (0.279, 1.424) |
| Average monthly outpatient out-of-pocket spending, $ | |||
| Parity (pre–post indicator) | 9.091 (−3.326, 21.508) | 4.223 (−3.789, 12.236) | 16.781 (0.323, 33.239) |
| Parity*month | 0.158 (−0.185, 0.501) | 0.070 (−0.152, 0.291) | 0.757 (0.303, 1.212) |
| Month (linear time variable) | 0.437 (−0.376, 1.250) | 0.164 (−0.361, 0.686) | −0.150 (−1.227, 0.928) |
| Average out-of-pocket paid per visit, $ | |||
| Parity (pre–post indicator) | 1.812 (−1.005, 4.628) | 1.781 (−0.822, 4.385) | 1.156 (−1.691, 4.004) |
| Parity*month | 0.018 (−0.060, 0.095) | 0.017 (−0.055, 0.088) | −0.030 (−0.109, 0.048) |
| Month (linear time variable) | −0.036 (−0.220, 0.149) | −0.064 (−0.235, 0.106) | −0.060 (−0.246, 0.126) |
Note. CI = confidence interval. All regressions had a total no. of 129 and included month indicators for seasonal variation. Insurer and enrollee spending regressions adjusted for inflation by using the gross domestic product deflator.
TABLE 3—
Interrupted Time Series Regression of Mental Health Parity and Addiction Equity Act Impact on Utilization and Spending for Opioid Use Disorder and Nonopioid Substance Use Disorder Services in the Employer-Sponsored Insurance Market: United States, 2005–2015
| Variable | OUD Services, b (95% CI) | Nonopioid SUD Services, b (95% CI) |
| Any use of outpatient services, percentage points | ||
| Parity (pre–post indicator) | 0.006 (0.004, 0.009) | 0.006 (0.002, 0.011) |
| Parity*month | < 0.001 (0.0002, 0.0004) | < 0.001 (0.0006, 0.0009) |
| Month (linear time variable) | 0.001 (0.0009, 0.001) | 0.001 (0.0005, 0.0006) |
| Average frequency of monthly outpatient service use per service user, no. of services | ||
| Parity (pre–post indicator) | 0.008 (−0.137, 0.153) | −0.052 (−0.163, 0.059) |
| Parity*month | 0.062 (0.058, 0.066) | 0.050 (0.047, 0.053) |
| Month (linear time variable) | −0.005 (−0.007, −0.003) | −0.003 (−0.005, −0.001) |
| Average monthly insurer spending per service user, $ | ||
| Parity (pre–post indicator) | 65.316 (34.556, 96.075) | 47.362 (20.484, 74.240) |
| Parity*month | 9.584 (8.734, 10.434) | 6.710 (5.968, 7.453) |
| Month (linear time variable) | 3.323 (1.309, 5.336) | 0.879 (−0.880, 2.639) |
| Average insurer reimbursement paid per visit, $ | ||
| Parity (pre–post indicator) | 2.655 (−21.444, 26.753) | 6.381 (−3.807, 16.569) |
| Parity*month | 0.554 (−0.112, 1.219) | −0.211 (−0.493, 0.070) |
| Month (linear time variable) | 0.267 (−1.311, 1.845) | 0.947 (0.280, 1.614) |
| Average monthly outpatient out-of-pocket spending, $ | ||
| Parity (pre–post indicator) | 18.211 (1.842, 34.580) | 17.126 (−0.030, 34.281) |
| Parity*month | 0.741 (0.289, 1.193) | 0.769 (0.295, 1.243) |
| Month (linear time variable) | 0.190 (−0.882, 1.262) | −0.157 (−1.280, 0.966) |
| Average out-of-pocket paid per visit, $ | ||
| Parity (pre–post indicator) | 1.781 (−3.467, 7.028) | 1.064 (−2.098, 4.225) |
| Parity*month | 0.092 (−0.053, 0.237) | −0.069 (−0.156, 0.018) |
| Month (linear time variable) | 0.130 (−0.214, 0.473) | −0.073 (−0.280, 0.134) |
Note. CI = confidence interval; OUD = opioid use disorder; SUD = substance use disorder. All regressions had a total no. of 129, included month indicators for seasonal variation, and were adjusted for inflation by using the gross domestic product deflator for spending outcomes.
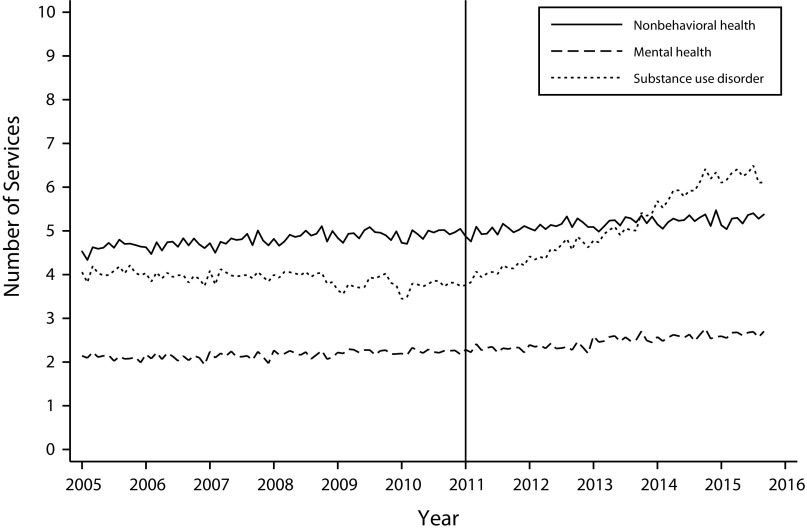
Table 2 shows the association between MHPAEA and utilization of mental health and SUD outpatient services. There was no change in any use of mental health outpatient services (the percentage of enrollees who used ≥ 1 service). However, the law did have a positive, though small, association with any SUD outpatient service use (parity [pre–post indicator] = 0.011; P < .01; parity∗month = 0.001; P < .01). This means that parity increased the percentage of enrollees with any use of outpatient SUD services by 0.023 percentage points in the first postparity year and 0.068 percentage points by the end of the 2015 postparity period. MHPAEA was positively associated with the frequency of services used for both mental health and SUD services (parity∗month = 0.005; P < .01 for mental health; parity∗month = 0.054; P < .01 for SUD services). However, the magnitude of this association was much larger for SUD services (Figure 1). The associated increase of average monthly SUD service use was 0.59 services per month per service user in the first postparity year and 3.0 services by the end of the postparity period. For non–behavioral health services, results were not significant or the coefficient was negative, increasing our confidence that changes were associated with MHPAEA and not unobserved factors.
FIGURE 1—
Average Number of Outpatient Services Used per Service User by Non–Behavioral Health, Mental Health, and Substance Use Disorder Service Categories Before and After Implementation of the Mental Health Parity and Addiction Equity Act: United States, 2005–2015
Table 2 also presents the regression results showing the association between MHPAEA and insurer and enrollee spending. The law was associated with increased average monthly insurer spending for both mental health and SUD services; however, the impact on mental health services was comparatively small. For SUD services, the associated impact was large and statistically significant (parity [pre–post indicator] = 47.674; P < .01; parity∗month = 6.879; P < .01). This translates into an estimated increase in insurer spending of $130 per month per SUD service user in the first postparity year and $440 by the end of the postparity period. Yet there was no statistically significant association of MHPAEA with the average reimbursement paid per SUD outpatient visit. This finding suggests that MHPAEA’s relationship with SUD insurer spending was not because it affected price paid per SUD visit but was instead driven by increased utilization of SUD services. For mental health, we found a moderate though statistically significant increase in reimbursement rates paid per service, but because we found a similar result for non–behavioral health services, we cannot be confident that this change was attributable to MHPAEA and not to general health care trends (Appendix C, available as a supplement to the online version of this article at http://www.ajph.org, for trend graphs).
MHPAEA was not associated with M/SUD enrollee out-of-pocket costs paid per visit but was associated with an increase in average monthly out-of-pocket enrollee spending for SUD services (parity [pre–post indicator] = 16.781; P = .05; parity∗month = 0.757; P < .01). This amounts to an increase of $26 per month in SUD out-of-pocket costs after the first year after parity and $60 by the end of the postparity period. Because the enrollee cost per visit did not increase with parity, this increase in out-of-pocket spending can be attributed to parity’s association with the frequency of SUD service use and not increased enrollee cost sharing.
Table 3 shows the regression results regarding the associated impact of MHPAEA on SUD services, stratified into OUD services and nonopioid SUD services. Our results demonstrate that MHPAEA had a similar impact on both OUD and nonopioid SUD service utilization and spending. For both OUD and nonopioid SUD services, there was an associated increase in the average frequency of monthly service use per service user (OUD services: parity∗month = 0.062; P < .01; nonopioid SUD services: parity∗month = 0.050; P < .01), an associated increase in average monthly insurer spending (OUD services: parity [pre–post indicator] = 65.32; P < .01; parity∗month = 9.58; P < .01; nonopioid SUD services: parity [pre–post indicator] = 47.36; P < .01; parity∗month = 6.71; P < .01), and an associated increase in out-of-pocket spending (OUD services: parity [pre–post indicator] = 18.211; P = .03; parity∗month = 0.741; P < .01; nonopioid SUD services: parity [pre–post indicator] = 17.126; P = .05; parity∗month = 0.769; P < .01). However, there was no increase in the per-visit average insurer reimbursement paid or out-of-pocket amount paid for either OUD or nonopioid SUD services.
DISCUSSION
In this study, we found a positive association between implementation of MHPAEA and utilization of outpatient behavioral health services. For SUD outpatient visits, the association was particularly strong, which is not surprising given that it was the first federal law to apply parity to SUD treatment. However, our finding that the law also was positively associated with the average frequency of mental health outpatient visits is noteworthy. Before the law was implemented, most individuals used mental health services below the preparity quantitative treatment limits.21 Hence, our expectations were that any reductions in treatment limits attributable to MHPAEA were not likely to affect average use. Yet we still observed a modest relationship between the law’s implementation and the frequency of outpatient mental health services at the mean.
MHPAEA also was positively associated with insurer and enrollee average spending per service user, especially for SUD services. However, consistent with earlier studies on the short-term impact of the law on SUD services,26 we found no association with provider reimbursement amount paid per visit or enrollee out-of-pocket amount paid per visit. Our findings suggest that the increase in behavioral health spending can be attributed to increased utilization, not higher reimbursement rates or higher out-of-pocket amounts for enrollees. It is important to note that SUD treatment services represented only 1.2% of total health care services after parity. Thus, despite the increase in spending on and utilization of SUD services in the employer-sponsored insurance market, the overall impact of MHPAEA on total spending by insurers was modest—consistent with other recent research.27
We found that MHPAEA had similar positive associations for OUD and nonopioid SUD services, increasing our confidence that the overall growth in utilization and spending for SUD treatment was not driven by more demand attributable to the opioid crisis. A recent analysis found that OUD coverage by commercial insurers has shifted over time and that, in particular, prior authorization requirements for OUD treatment have decreased.6 The results of this study and previous research suggest that MHPAEA is an important piece of the ongoing efforts to combat the opioid crisis. However, the rates of service use for individuals with SUD and OUD, in particular, remain extremely low and highlight the need for a multifaceted approach to improving access to care.
One provision of MHPAEA requires insurers to apply parity regulations to out-of-network outpatient visits and inpatient visits. Recent research that used MarketScan data found that the law was associated with a 4.3% increase in use of out-of-network outpatient SUD services compared with what would have been expected without parity by 2012.28 Extending similar analyses to September 2015, we found that the shift to out-of-network providers continued throughout the study period and that this shift occurred for both OUD and nonopioid SUD outpatient services (Appendix D, available as a supplement to the online version of this article at http://www.ajph.org).
Understanding the dramatic shift in out-of-network service use requires disentangling the impacts of MHPAEA from those of provider supply limitations and other barriers to health care access overall. The demand for SUD treatment exceeds the supply of treatment providers,29 particularly for OUD treatment.5,30 Though important, parity in insurance coverage alone will not solve ongoing problems with access to behavioral health services.2 More research is necessary to understand how the increased protections afforded by MHPAEA interact with potential provider shortages, possibly leading to increased use of out-of-network care and costs for consumers.
A methodological advantage of this study is that it extended the postparity period to the third quarter of 2015. Our analyses demonstrated that in the large group employer–sponsored insurance market, the associated impact of parity continued throughout the postparity period and was particularly evident for SUD outpatient services. In our descriptive analyses, the trend lines show no evidence that they were leveling off, and effects on these services were evident into 2015 (Appendix C, available as a supplement to the online version of this article at http://www.ajph.org).
One possible explanation for these trends is that, although insurers were initially delayed in addressing nonquantitative treatment limits,2,9 enforcement of these limits may have improved in more recent years. Federal education and guidance on nonquantitative treatment limits may help support this trend,31,32 and varied systems for monitoring and enforcing compliance with parity are increasingly evident at the state level.33 However, nonquantitative treatment limits are difficult to regulate, particularly in a managed care environment, and other adjustments to financing structures may be necessary to avoid adverse selection for those with behavioral health conditions.34 Although federal policy alone is not sufficient to redress stigma,35 the ongoing effect of parity may improve overall attitudes, further facilitating access to care.
Limitations
One limitation of this study was that, although MarketScan represents many individuals, it is a convenience sample, and plans contributing data shift from year to year. To account for this limitation, we ran parallel analyses with only continuously enrolled plans and found similar results. Another limitation was that identifying a suitable comparison group to study a policy change that affected the entire US population with employer-sponsored insurance would be difficult. We partially mitigated this limitation by comparing our findings with utilization and spending for non–behavioral health services, but this is not a perfect comparison group. In addition, because the study excluded enrollees with less than 12 months of enrollment in each calendar year, our results may not be generalizable to enrollees with partial enrollment. We also did not consider whether insurers might adjust physical health benefits in response to MHPAEA, but there is a growing consensus that insurers did not respond to MHPAEA in this way.5 Our total mental health and SUD groups were not mutually exclusive, so it is possible that those with co-occurring SUDs could contribute to our modest findings in the mental health group. Finally, as noted previously, time-series designs are always vulnerable to validity threats attributable to concurrent historical events (e.g., changes to provider guidelines and policies) or instrumentation effects (e.g., systematic variations in how providers code outpatient visits).
Public Health Implications
MHPAEA is associated with improved access to and utilization of behavioral health outpatient services, and subsequent increases in spending were driven primarily by overall increases in utilization. This study demonstrates the influence that broad policy changes can have on the delivery of behavioral health services at the population level. Although spending on SUD services increased, SUD services make up a small fraction of behavioral health services and are unlikely to affect overall health care spending. More research is needed on the additional burden of out-of-pocket spending for those with OUD, which is attributed to the increased service use that parity has facilitated. Given the opioid crisis, it is critical to assess whether this out-of-pocket spending is a barrier to receipt of SUD outpatient treatment for those with OUD and those with co-occurring mental disorders and SUDs.
ACKNOWLEDGMENTS
This study was conducted under contract to the Office of the Assistant Secretary for Planning and Evaluation (ASPE), US Department of Health and Human Services.
Findings from the study were previously presented at the Academy Health Research Meeting on June 25, 2018, in Seattle, Washington.
The authors would like to thank D. E. B. Potter and Laurel Fuller of ASPE and Timothy Creedon of IBM Watson Health for their helpful input, and Mary Beth Schaefer for editing support.
CONFLICTS OF INTEREST
None of the authors have any conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study did not meet the regulatory definition of research involving human participants, and institutional review board approval was not required.
REFERENCES
- 1.Barry CL, Huskamp HA, Goldman HH. A political history of federal mental health and addiction insurance parity. Milbank Q. 2010;88(3):404–433. doi: 10.1111/j.1468-0009.2010.00605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterson E, Busch S. Achieving mental health and substance use disorder treatment parity: a quarter century of policy making and research. Annu Rev Public Health. 2018;39(1):421–435. doi: 10.1146/annurev-publhealth-040617-013603. [DOI] [PubMed] [Google Scholar]
- 3.Roll JM, Kennedy J, Tran M, Howell D. Disparities in unmet need for mental health services in the United States, 1997–2010. Psychiatr Serv. 2013;64(1):80–82. doi: 10.1176/appi.ps.201200071. [DOI] [PubMed] [Google Scholar]
- 4.Mojtabai R, Chen LY, Kaufmann CN, Crum RM. Comparing barriers to mental health treatment and substance use disorder treatment among individuals with comorbid major depression and substance use disorders. J Subst Abuse Treat. 2014;46(2):268–273. doi: 10.1016/j.jsat.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am J Public Health. 2015;105(8):e55–e63. doi: 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reif S, Creedon TB, Horgan CM et al. Commercial health plan coverage of selected treatments for opioid use disorders from 2003 to 2014. J Psychoactive Drugs. 2017;49(2):102–110. doi: 10.1080/02791072.2017.1300360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frank RG, Beronio K, Glied SA. Behavioral health parity and the Affordable Care Act. J Soc Work Disabil Rehabil. 2014;13(1-2):31–43. doi: 10.1080/1536710X.2013.870512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thalmayer AG, Friedman SA, Azocar F, Harwood JM, Ettner SL. The Mental Health Parity and Addiction Equity Act (MHPAEA) evaluation study: impact on quantitative treatment limits. Psychiatr Serv. 2017;68(5):435–442. doi: 10.1176/appi.ps.201600110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horgan CM, Hodgkin D, Stewart MT et al. Health plans’ early response to federal parity legislation for mental health and addiction services. Psychiatr Serv. 2016;67(2):162–168. doi: 10.1176/appi.ps.201400575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hodgkin D, Horgan CM, Stewart MT et al. Federal parity and access to behavioral health care in private health plans. Psychiatr Serv. 2018;69(4):396–402. doi: 10.1176/appi.ps.201700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goplerud EN. Consistency of large employer and group health plan benefits with requirements of the Paul Wellstone and Pete Domenici Mental Health Parity and Addition Equity Act of 2008. Washington, DC: Assistant Secretary for Planning and Evaluation; 2013. [Google Scholar]
- 12.Friedman SA, Thalmayer AG, Azocar F et al. The Mental Health Parity and Addiction Equity Act evaluation study: impact on mental health financial requirements among commercial “carve‐in” plans. Health Serv Res. 2018;53(1):366–388. doi: 10.1111/1475-6773.12614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berry KN, Huskamp HA, Goldman HH, Barry CL. A tale of two states: do consumers see mental health insurance parity when shopping on state exchanges? Psychiatr Serv. 2015;66(6):565–567. doi: 10.1176/appi.ps.201400582. [DOI] [PubMed] [Google Scholar]
- 14.Beronio K, Glied S, Frank R. How the Affordable Care Act and Mental Health Parity and Addiction Equity Act greatly expand coverage of behavioral health care. J Behav Health Serv Res. 2014;41(4):410–428. doi: 10.1007/s11414-014-9412-0. [DOI] [PubMed] [Google Scholar]
- 15.Grazier KL, Eisenberg D, Jedele JM et al. Effects of mental health parity on high utilizers of services: pre–post evidence from a large, self-insured employer. Psychiatr Serv. 2016;67(4):448–451. doi: 10.1176/appi.ps.201400586. [DOI] [PubMed] [Google Scholar]
- 16.Stuart EA, McGinty EE, Kalb L et al. Increased service use among children with autism spectrum disorder associated with Mental Health Parity Law. Health Aff (Millwood) 2017;36(2):337–345. doi: 10.1377/hlthaff.2016.0824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huskamp HA, Samples H, Hadland SE et al. Mental health spending and intensity of service use among individuals with diagnoses of eating disorders following federal parity. Psychiatr Serv. 2018;69(2):217–223. doi: 10.1176/appi.ps.201600516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Busch AB, Yoon F, Barry CL et al. The effects of mental health parity on spending and utilization for bipolar, major depression, and adjustment disorders. Am J Psychiatry. 2013;170(2):180–187. doi: 10.1176/appi.ajp.2012.12030392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lopez Bernal J, Soumerai S, Gasparrini A. A methodological framework for model selection in interrupted time series studies. J Clin Epidemiol. 2018;103:82–91. doi: 10.1016/j.jclinepi.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 21.Mark TL, Vandivort-Warren R, Miller K. Mental health spending by private insurance: implications for the Mental Health Parity and Addiction Equity Act. Psychiatr Serv. 2012;63(4):313–318. doi: 10.1176/appi.ps.201100312. [DOI] [PubMed] [Google Scholar]
- 22.Mark TL, Hodgkin D, Levit KR, Thomas CP. Growth in spending on and use of services for mental and substance use disorders after the Great Recession among individuals with private insurance. Psychiatr Serv. 2016;67(5):504–509. doi: 10.1176/appi.ps.201500034. [DOI] [PubMed] [Google Scholar]
- 23.Linden A. ITSA: Stata module to perform interrupted time series analysis for single and multiple groups. Statistical Software Components S457793. Boston College Department of Economics. 2014. Available at: https://ideas.repec.org/c/boc/bocode/s457793.html. Accessed May 3, 2018.
- 24.Mark TL, Yee T, Levit KR et al. Insurance financing increased for mental health conditions but not for substance use disorders, 1986–2014. Health Aff (Millwood) 2016;35(6):958–965. doi: 10.1377/hlthaff.2016.0002. [DOI] [PubMed] [Google Scholar]
- 25.Levit KR, Mark TL, Coffey RM et al. Federal spending on behavioral health accelerated during recession as individuals lost employer insurance. Health Aff (Millwood) 2013;32(5):952–962. doi: 10.1377/hlthaff.2012.1065. [DOI] [PubMed] [Google Scholar]
- 26.Busch SH, Epstein AJ, Harhay MO et al. The effects of federal parity on substance use disorder treatment. Am J Manag Care. 2014;20(1):76–82. [PMC free article] [PubMed] [Google Scholar]
- 27.Harwood JM, Azocar F, Thalmayer A et al. The Mental Health Parity and Addiction Equity Act evaluation study: impact on specialty behavioral healthcare utilization and spending among carve-in enrollees. Med Care. 2017;55(2):164–172. doi: 10.1097/MLR.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McGinty EE, Busch SH, Stuart EA et al. Federal parity law associated with increased probability of using out-of-network substance use disorder treatment services. Health Aff (Millwood) 2015;34(8):1331–1339. doi: 10.1377/hlthaff.2014.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vestal C. How severe is the shortage of substance abuse specialists? The Pew Charitable Trusts. 2015. Available at: http://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2015/4/01/how-severe-is-the-shortage-of-substance-abuse-specialists. Accessed May 3, 2018.
- 30.Rosenblatt RA, Andrilla CH, Caitlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13(1):23–26. doi: 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Executive Office of the President of the United States. The Mental Health and Substance Use Disorder Parity Task Force. Final report. October 2016. Available at: https://www.hhs.gov/sites/default/files/mental-health-substance-use-disorder-parity-task-force-final-report.PDF. Accessed May 3, 2018.
- 32. Substance Abuse and Mental Health Services Administration. Consumer guide to disclosure rights: making the most of your mental health and substance use disorder benefits. HHS Publication No. SMA-16-4992. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016.
- 33. Approaches in implementing the Mental Health Parity and Addiction Equity Act: best practices from the states. HHS Publication No. SMA-16-4983. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016.
- 34.McGuire TG. Achieving mental health care parity might require changes in payments and competition. Health Aff (Millwood) 2016;35(6):1029–1035. doi: 10.1377/hlthaff.2016.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cummings JR, Lucas SM, Druss BG. Addressing public stigma and disparities among persons with mental illness: the role of federal policy. Am J Public Health. 2013;103(5):781–785. doi: 10.2105/AJPH.2013.301224. [DOI] [PMC free article] [PubMed] [Google Scholar]