Abstract
The evolving US opioid crisis is complex and requires myriad different interventions. These include reducing opioid overprescribing and curtailing the supply of illicit opioids, overdose rescue interventions, and treatment and recovery support services for those with opioid use disorders.
To date, more distal primary prevention strategies that have an evidence base are underutilized. Yet, the impact of early environments on later substance use disorder risk is increasingly well understood, including knowledge of the mechanistic linkages between brain development and subsequent risk behaviors. Applying this developmental framework to prevention shows promise, and some middle-school interventions have demonstrated significant reductions in prescription opioid misuse.
Reducing these risks of initial misuse of opioids may be the “ounce of prevention” that makes a substantial difference in a society now reeling from the worst drug crisis our country has seen. The challenge is to continue to develop and test promising distal interventions and to support implementation fidelity through frameworks that ensure their cultural appropriateness and sustainability. In addition, research is needed to develop new prevention strategies for adults, including patients with pain at risk for transitioning from prescription to illicit opioids.
Addressing the complex opioid public health emergency in the United States requires a range of approaches to address its multiple causes and consequences. To date, much attention has focused on prescribing practices as a key upstream driver, saving lives acutely through widespread distribution of the opioid antagonist naloxone, and expanding medication use for the treatment of opioid addiction.1 Besides improving prescribing practices, additional upstream primary prevention strategies can also play a key role. Through interventions, policies, and practices that increase protective factors and diminish risk factors, the number of persons liable to develop opioid misuse and resulting consequences, including addiction and overdose, may be reduced. That is the theme of this commentary—that attention to these childhood and adolescent prevention approaches should be considered as part of the response to the US opioid crisis. This commentary does not seek to minimize policy and practice approaches that are reducing overprescribing of opioids and other supply reduction efforts, but a full discussion of these approaches is beyond our scope. Instead we highlight a potential role for preventing the onset of opioid misuse by considering interventions that address early risk and protective factors (see the box on page S186).
KEY MESSAGES.
Previous research documents the potential for early adolescent primary prevention interventions to reduce the onset of prescription opioid misuse, and multiple studies document that primary prevention can reduce the onset of misuse of other substances. Yet, these interventions have not been widely tested regarding their long-term impact on opioid use and addiction.
There is empirical as well as theoretical rationale for preventing substance misuse and related outcomes through primary prevention aimed at addressing risk and protective factors in childhood and adolescence.
In addition to proximal prevention efforts to reduce exposure to opioids (both medical and illicit), distal primary prevention can help reduce the demand for opioids later in life and thus should be considered in efforts to address the opioid crisis.
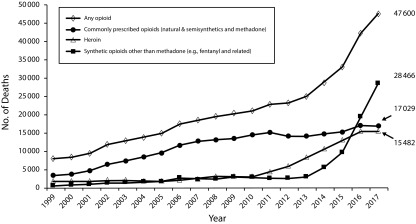
Overdoses involving prescription or illicit opioids killed 130 Americans every day in 2017, and the toll of the epidemic has escalated (Figure 1).2 Overprescribing opioid analgesics was a powerful driver, especially during the first decade of the crisis.4 Lack of caution in acute pain prescribing enabled excessive quantities of pills to become available for diversion, and long-term use of opioids to treat chronic pain led some patients to addiction.5
FIGURE 1—
Overdose Deaths Attributed to Opioids in the United States: 1999–2017
Source. Hedegaard et al.2
Note. Subcategories are not mutually exclusive.3
The opioid overdose epidemic has widened to involve and even center on illicit opioids (Figure 1). Overdoses related to prescription opioids started escalating in 1999, leveling off somewhat after 2011.2 Heroin deaths began rising in about 2007 with increases accelerating after 2010. In the last few years, potent synthetic opioids, such as illicitly made fentanyl, are now dominating the statistics on fatalities; fentanyl is often mixed in with heroin and other illicit drugs or pressed into counterfeit tablets to resemble commonly abused prescription drugs.6 The recent increase in cocaine and other psychostimulant deaths is likely attributable to illicit synthetic opioids being mixed into those drug supplies as well.3,6,7
Strategies seeking to reverse the opioid crisis must address the large cohort of people already addicted to opioids through treatment, overdose prevention, and recovery support services. Wider access to naloxone is making an impact,8 as is the gradual erosion of prejudices against use of medications in treating opioid addiction.9 Use of the medications buprenorphine, methadone, or naltrexone in patients with opioid addiction saves lives and improves outcomes.9–12 However, despite this clear evidence of effectiveness, only a subset of people with opioid use disorder seek care or receive evidence-based care,13 suggesting an important potential role for prevention.
Prevention efforts aimed at reducing the supply of prescription opioids may have already had a positive impact. The Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain improved provider education, and publicity around opioids’ hazards is changing this landscape.14 Prescriptions have been declining since 2012, and efforts are under way to modify insurance coverage and reimbursement policies to expand access to nonopioid pain treatments.15,16 There are also intensive efforts to develop new, nonaddictive pain treatments, which could reduce clinicians’ overreliance on addictive opioids.17 And with the increased role of illicit fentanyl and other synthetics, international diplomacy and law enforcement increasingly play a front-line role in curbing the supply of illicit opioids.18
The opioid crisis may in fact represent at least three separate problems: (1) individuals who started with prescriptions from their doctors, (2) individuals who got diverted prescriptions from others but were never prescribed opioids by their doctors, and (3) individuals initiating opioid use with heroin or other illicit opioids that have no connection to the medical system. Addressing the different pathways to opioid misuse and its consequences such as overdose to some extent calls for distinct types of interventions, but primary prevention strategies focusing on modifiable risk and protective factors may play a role as well.
HUMAN DEVELOPMENT-BASED PREVENTION
The science of substance use prevention is embedded in the science of human development.19 Substance use disorders arise through a combination of individuals’ environments and their unique biology, including genetic determinants. The environmental influences that contribute to risk for substance use and addiction interact in a complex way with genes as well as brain maturation.20 When one is designing prevention interventions, modifiable environmental factors are the typical targets of intervention. Knowing how and when to target prevention efforts depends on understanding the shift in balance of environmental and biological influences over the life course.
The concept of the “environment” covers a broad range of risk and protective domains. The quality of mother–child attachment or the level of stress in the family environment are crucially important early on; later, peer environments and the amount of structure experienced at school and in the neighborhood assume greater importance.21 Exposure to substances in the home environment can be important across childhood and adolescence and even prenatally. Laws and policies also can have significant impacts on families and on an individual’s behavior and so can be considered part of the environment as well.22
The risks associated with substance use begin long before an individual smokes the first cigarette, has a first drink of alcohol, or tries an illicit substance. Stressful environments in early life have been vividly shown in both animal and human research to increase later-life propensity to mental illness and to increase the likelihood of drug taking and addiction.23 In the Adverse Childhood Experiences study, a retrospective cohort study of more than 8600 adults visiting a California primary care clinic, the greater number of early childhood abuse and neglect experiences that respondents reported, the more likely they were to have used drugs as adolescents or as adults, to have a substance use disorder (SUD), and to have initiated drug use at an early age.24 Primary prevention to reduce child abuse and neglect and other forms of adverse childhood experiences may reduce a person’s risk for developing an SUD later in life.25
What is it about stressful conditions in the home of a four-year-old child that would lead that child to use drugs at age 14 or 24 years? Here is where the complex interplay of environment and biology comes into play. Epigenetic mechanisms (changes to gene expression) directly link early life stress to later stress sensitivity and associated behavioral disorders, and human studies have shown strong connections between adverse early environments and altered brain development and behavioral abnormalities,26 including evidence that some of the neurodevelopmental impacts of adverse environments can be reversed.27
One way to think about prevention is as tests of the models linking early childhood environments and experiences to later outcomes. Fostering safe, stable, nurturing relationships and environments enables children to learn empathy, impulse control, anger management, and problem solving—all skills that have a protective effect.28 Safe, stable, nurturing relationships and environments also buffer against the impact of stress and trauma.28 Parental employment, adequate housing, and access to health care and social services serve to support healthy child development too.25 One specific example is the test of a family-focused intervention in rural Georgia that found a strong correlation between number of years in poverty and diminished volume of the left dentate gyrus, the CA3 subfield of the hippocampus, and the left amygdala—structures in the brain that contribute to academic functioning, social development, learning, memory, mood, and stress reactivity—in the control group of children not receiving the intervention; the same declines were not seen in the intervention group.29 The results support the premise that prevention interventions can ameliorate what otherwise would be a toxic social environment, even without changing other aspects of that environment. Furthermore, interventions as early as the prenatal period can demonstrably improve later behavioral, cognitive, and health outcomes. Large randomized studies have shown that providing guidance to low-income, first-time mothers during pregnancy and in the first two years of a child’s life through home visitation by nurses can have a range of lasting positive impacts on the child—not only reduced abuse and neglect but also improved cognitive and behavioral outcomes that extend into the adolescent years.30
Our understanding of human neurodevelopment across the life span has also illuminated why adolescence is such a period of risk for the initiation of substance use and the development of SUDs.19,20 Brain development is characterized by uneven maturation, with the limbic structures involved in emotional responsivity and reward maturing earlier than cortical areas involved in judgment, decision-making, and impulse control.31 The prefrontal cortex, associated with the executive functions, does not mature until the mid-20s.32 This translates to a propensity for risk taking among youths.33 On one hand, that is developmentally appropriate, as it is a period when the individual needs to forge independence from parents and fashion self-identity; seeking out novel experiences and taking risks is part of this process. Unfortunately, the uneven maturation of the adolescent brain also increases susceptibility to environmental influences dominant during the adolescent years, such as peer influence.34 The hazards are compounded by the fact that, because it is not fully mature, the adolescent brain is more vulnerable to lasting effects of substance use, including increased risk of addiction.35 The risk for developing an SUD is highest for those who initiate substances in the early teens, and addiction is most likely to begin in the late teen years.36 Several prevention interventions aimed at middle- and high-school students have demonstrated effectiveness at reducing or delaying substance initiation and use, including specifically misuse of opioids (see the next section).
Across childhood and adolescence, the risk factors that predispose someone to later substance use are common and shared with a number of other negative health outcomes. Because of this, prevention interventions may affect a wide range of behavioral and health outcomes, not just substance use.28,37–39 By altering the child’s or adolescent’s trajectory at critical ages and thereby reducing many negative outcomes, such programs can thus be both effective and cost-effective, producing a large return on investment.39
The CDC has compiled a core set of evidence-based strategies at the individual, family, community, and societal levels that, when used in combination, can best ensure children reach their full potential.40 A broad implementation framework such as Communities That Care also might be relevant to addressing the opioid epidemic because it uses data to inform action at the community level and leverages existing evidence-based policies and programs for parents, caregivers, and children to achieve multiple positive outcomes.41 The Substance Abuse and Mental Health Services Administration works with states and communities to implement prevention interventions tailored to the community and target population, taking into account unique risk and protective factors, stakeholders, and local policies.
RISK- AND PROTECTION-BASED PREVENTION
With few exceptions, the direct impacts of childhood or adolescent interventions on opioid use specifically have generally been less studied, and we suggest that these approaches deserve consideration. Cross-over effects, whereby youth risk and protective factor–based interventions have been shown to affect multiple outcomes, have been reported.28,37–39 We also know that rates of opioid misuse as well as attitudes toward opioid misuse among young people are susceptible to change.
Annual data from the Monitoring the Future survey of drug use and attitudes among 8th, 10th, and 12th graders have shown significant reductions in misuse of prescription opioids since 2010.42 And some childhood and adolescent prevention interventions already have shown evidence of reducing prescription opioid misuse.43 These programs use a positive youth development and resilience approach that focuses on developmental competencies. The Strengthening Families Program 10–14 has been associated with reductions in prescription opioid misuse up to age 25 years, 13 years following the intervention.43 Communities in which seventh-graders had received a classroom-based intervention called Life Skills Training, teaching drug awareness and self-management, social, and resistance skills, showed significantly reduced prescription opioid misuse among middle- and high-school students.44 And a system for delivery of evidence-based prevention programs in sixth and seventh grade, called Promoting School–Community–University Partnerships to Enhance Resilience, has also been associated with reductions in nonmedical use of prescription drugs.45
Most recently, CDC has collaborated with the Office of National Drug Control Policy and funded 13 community-based research projects in the Combating Opioid Overdose Through Community-Level Intervention initiative. One of these programs, known as The Martinsburg Initiative, addresses adverse childhood experiences through a neighborhood school-based and community policing strategy.46 If proven effective, this might serve as a model for other communities and could be replicated through CDC’s state-based opioid overdose prevention programs.
Although positive outcomes have been demonstrated, the studies are modest in number. Thus, a challenge remains to develop and test other primary prevention approaches in preventing opioid misuse, and such work might build on the interventions that have been shown to be effective for related outcomes.39 Given the evidence from several studies that implemented the Strengthening Families Program 10–14,43 a good starting point for research that specifically tests for effects on opioid outcomes might be the rich literature on other family-based programs,47 though we caution that such research must include assessment for potential unintentional or adverse outcomes, including increased substance use in intervention groups.48
We also highlight another gap, the current lack of evidence-based preventive interventions for adults. As many people may be initiating opioid use in adulthood, the existing evidence-based preventive interventions might not be appropriate developmentally or will require other methods of delivery than via family and schools. In fact, investments in research to identify effective preventive interventions in this population are being pursued.49 In addition, the dissemination of information about the risks of opioids through traditional and new media platforms to adults and other at-risk populations and the rapid translation of emerging research on preventive interventions into practice in communities and clinical practice are needed. The forthcoming Regional Prevention Technology Transfer Centers funded by the Substance Abuse and Mental Health Services Administration could be a useful platform to advance these efforts.
CONCLUSIONS
Decades of research have shown how much can be achieved through primary prevention interventions delivered during childhood and adolescence to reduce individuals’ later risk for drug use disorders.19,28,30,37–41 Effective interventions already exist—including a few that have shown specific benefit at reducing risk of later opioid misuse43—and thus a major challenge is to test the generalizability of these interventions and to widen their culturally appropriate and sustainable adoption. More research testing the effectiveness of existing approaches in reducing opioid misuse and the ways these approaches could be modified to that end is needed, taking into account the multiple pathways into opioid misuse and addiction. Meta-analysis and other systematic reviews are needed on whether and how prevention interventions significantly reduce the onset of opioid misuse and opioid use disorders.39,50 And because some people are initiating opioid use later in life, for instance via pain treatment, research is needed to develop and test new prevention strategies for adults, including those in health care settings and those in contact with the justice system, as well as patients with pain at risk for transitioning from prescription opioid misuse to illicit opioid use.49
As the opioid crisis evolves and expands in the United States, it is necessary to approach the problem in a comprehensive manner that includes overdose prevention, measures to reduce opioid overprescribing and curtail the supply of illicit opioids, and increasing access to treatment of opioid use disorders and supporting long-term recovery.1 Reducing the risks of initiating opioid misuse by addressing modifiable childhood and adolescent risk and protective factors may be another “ounce of prevention” that makes a substantial difference in a society and health care system now reeling from one of the worst drug crises our country has seen.
CONFLICTS OF INTEREST
W. M. C. reports long-term holdings in General Electric Company, 3M Companies, and Pfizer Incorporated, unrelated to the present work.
REFERENCES
- 1.US Department of Health and Human Services. 5-point strategy to combat the opioid crisis. 2018. Available at: https://www.hhs.gov/opioids/about-the-epidemic/hhs-response/index.html. Accessed May 15, 2018. [DOI] [PubMed]
- 2. Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief, no 329. Hyattsville, MD: National Center for Health Statistics; 2018.
- 3.Seth P. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–358. doi: 10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Compton WM, Boyle M, Wargo EM. Prescription opioid abuse: problems and responses. Prev Med. 2015;80:5–9. doi: 10.1016/j.ypmed.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Paulozzi LJ, Mack KA, Hockenberry JM. Vital Signs: variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):563–568. [PMC free article] [PubMed] [Google Scholar]
- 6.Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA. 2018;319(17):1819–1821. doi: 10.1001/jama.2018.2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCall Jones C, Baldwin GT, Compton WM. Recent increases in cocaine-related overdose deaths and the role of opioids. Am J Public Health. 2017;107(3):430–432. doi: 10.2105/AJPH.2016.303627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coffin PO, Behar E, Rowe C et al. Nonrandomized intervention study of naloxone coprescription for primary care patients receiving long-term opioid therapy for pain. Ann Intern Med. 2016;165(4):245–252. doi: 10.7326/M15-2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green TC, Clarke J, Brinkley-Rubinstein L et al. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry. 2018;75(4):405–407. doi: 10.1001/jamapsychiatry.2017.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Substance Abuse and Mental Health Services Administration. Medications for opioid use disorder. Treatment Improvement Protocol (TIP) Series 63, full document. HHS Publication No. (SMA) 18-5063FULLDOC. 2018. Available at: https://store.samhsa.gov/product/TIP-63-Medications-for-Opioid-Use-Disorder-Full-Document-Including-Executive-Summary-and-Parts-1-5-/SMA18-5063FULLDOC. Accessed February 26, 2019.
- 11.D’Onofrio G, Chawarski MC, O’Connor PG et al. Emergency department–initiated buprenorphine for opioid dependence with continuation in primary care: outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660–666. doi: 10.1007/s11606-017-3993-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JD, Friedmann PD, Kinlock TW et al. Extended-release naltrexone to prevent opioid relapse in criminal justice offenders. N Engl J Med. 2016;374(13):1232–1242. doi: 10.1056/NEJMoa1505409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams AR, Nunes EV, Bisaga A, Levin FR, Olfson M. Development of a cascade of care for responding to the opioid epidemic. Am J Drug Alcohol Abuse. 2019 doi: 10.1080/00952990.2018.1546862. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bohnert AS, Guy GP, Losby JL. Opioid prescribing in the United States before and after the Centers for Disease Control and Prevention’s 2016 opioid guideline. Ann Intern Med. 2018;169(6):367–375. doi: 10.7326/M18-1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heyward J, Jones CM, Compton WM et al. Nonpharmacologic treatments for low back pain among US public and private insurers. JAMA Netw Open. 2018;1(6):e183044. doi: 10.1001/jamanetworkopen.2018.3044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin DH, Jones CM, Compton WM et al. Prescription drug coverage for low back pain among U.S. Medicaid, Medicare Advantage and commercial insurers. JAMA Netw Open. 2018;1(2):e180235. doi: 10.1001/jamanetworkopen.2018.0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volkow ND, Collins FS. The role of science in addressing the opioid crisis. N Engl J Med. 2017;377(4):391–394. doi: 10.1056/NEJMsr1706626. [DOI] [PubMed] [Google Scholar]
- 18.US Department of Justice, Drug Enforcement Administration. 2017 National Drug Threat Assessment. Available at: https://www.dea.gov/documents/2017/10/01/2017-national-drug-threat-assessment. Accessed February 26, 2019.
- 19.National Research Council and Institute of Medicine. From Neurons to Neighborhoods: The Science of Early Childhood Development. Committee on Integrating the Science of Early Childhood Development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 20.Volkow ND, Boyle M. Neuroscience of addiction: relevance to prevention and treatment. Am J Psychiatry. 2018;175(8):729–740. doi: 10.1176/appi.ajp.2018.17101174. [DOI] [PubMed] [Google Scholar]
- 21.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 22.Plunk AD, Cavazaos-Rehg P, Bierut LJ, Grucza RA. The persistent effects of minimum legal drinking age laws on drinking patterns later in life. Alcohol Clin Exp Res. 2013;37(3):463–469. doi: 10.1111/j.1530-0277.2012.01945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes K, Bellis MA, Hardcastle KA et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 24.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the Adverse Childhood Experiences study. Pediatrics. 2003;111(3):564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 25.Fortson B, Klevens J, Merrick MT, Gilbert LK, Alexander SP. Preventing child abuse and neglect: a technical package for policy, norm, and programmatic activities. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 26.Enoch M-A. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology (Berl) 2011;214(1):17–31. doi: 10.1007/s00213-010-1916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson CA, Zeanah CH, Fox NA, Marshall PJ, Smyke AT, Guthrie D. Cognitive recovery in socially deprived young children: the Bucharest Early Intervention Project. Science. 2007;318(5858):1937–1940. doi: 10.1126/science.1143921. [DOI] [PubMed] [Google Scholar]
- 28. Wilkins N, Tsao B, Hertz M, Davis R, Klevens J. Connecting the dots: an overview of the links among multiple forms of violence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; Oakland, CA: Prevention Institute; 2014.
- 29.Brody GH, Gray J, Yu T et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171(1):46–52. doi: 10.1001/jamapediatrics.2016.2988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olds DL, Kitzman HJ, Cole RE et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164(5):419–424. doi: 10.1001/archpediatrics.2010.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24(4):417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- 32.Gogtay N, Giedd JN, Lusk L et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A. 2004;101(21):8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steinberg L. Risk taking in adolescence: new perspectives from brain and behavioral science. Curr Dir Psychol Sci. 2007;16(2):55–59. [Google Scholar]
- 34.Albert D, Chein J, Steinberg L. Peer influences on adolescent decision making. Curr Dir Psychol Sci. 2013;22(2):114–120. doi: 10.1177/0963721412471347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci. 2009;40(1):31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 37.National Institute on Drug Abuse, National Institutes of Health. Principles of substance abuse prevention for early childhood, a research-based guide. 2016. Available at: https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/early_childhood_prevention_march_2016.pdf. Accessed October 1, 2018.
- 38.Monahan KC, Oesterle S, Rhew I, Hawkins JD. The relation between risk and protective factors for problem behaviors and depressive symptoms, antisocial behavior, and alcohol use in adolescence. J Community Psychol. 2014;42(5):621–638. doi: 10.1002/jcop.21642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Catalano RF, Fagan AA, Gavin LE et al. Worldwide application of prevention science in adolescent health. Lancet. 2012;379(9826):1653–1664. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.US Centers for Disease Control and Prevention. Technical packages for violence prevention: using evidence-based strategies in your violence prevention efforts. 2018. Available at: https://www.cdc.gov/violenceprevention/pub/technical-packages.html. Accessed May 14, 2018.
- 41.Hawkins JD, Catalano RF, Kuklinski MR. Encyclopedia of Criminology and Criminal Justice. New York, NY: Springer; 2014. Communities that Care; pp. 393–408. [Google Scholar]
- 42.Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future national survey results on drug use, 1975–2017: overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2018. [Google Scholar]
- 43.Spoth R, Trudeau L, Shin C et al. Longitudinal effects of universal preventive intervention on prescription drug misuse: three randomized controlled trials with late adolescents and young adults. Am J Public Health. 2013;103(4):665–672. doi: 10.2105/AJPH.2012.301209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crowley DM, Jones DE, Coffman DL, Greenberg MT. Can we build an efficient response to the prescription drug misuse epidemic? Assessing the cost effectiveness of universal prevention in the PROSPER trial. Prev Med. 2014;62:71–77. doi: 10.1016/j.ypmed.2014.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Spoth R, Redmond C, Shin C, Greenberg M, Feinberg M, Schainker L. PROSPER community–university partnership delivery system effects on substance misuse through 6 1/2 years past baseline from a cluster randomized controlled intervention trial [erratum Prev Med. 2014;69:36]. Prev Med. 2013;56(3-4):190–196. [DOI] [PMC free article] [PubMed]
- 46.Martinsburg Police Department. The Martinsburg Initiative. 2017. Available at: http://www.martinsburgpd.org/martinsburg-initiative. Accessed May 14, 2018.
- 47.Van Ryzin MJ, Kumpfer KL, Fosco GM, Greenberg MT, editors. Family-Based Prevention Programs for Children and Adolescents: Theory, Research, and Large-Scale Dissemination. New York, NY: Psychology Press; 2015. [Google Scholar]
- 48.Moos RH. Iatrogenic effects of psychosocial interventions for substance use disorders: prevalence, predictors, prevention. Addiction. 2005;100(5):595–604. doi: 10.1111/j.1360-0443.2005.01073.x. [DOI] [PubMed] [Google Scholar]
- 49.National Institutes of Health. HEAL Initiative: Preventing Opioid Use Disorder in Older Adolescents and Young Adults (ages 16–30). Available at: https://grants.nih.gov/grants/guide/rfa-files/rfa-da-19-035.html. Accessed January 31, 2019.
- 50.Cragg A, Hau JP, Woo SA, Liu C, Doyle-Waters MM, Hohl CM. Risk factors for addiction among patients receiving prescribed opioids: a systematic review protocol. Syst Rev. 2017;6(1):265. doi: 10.1186/s13643-017-0642-0. [DOI] [PMC free article] [PubMed] [Google Scholar]