Abstract
Objectives. To explore effects of coalitions (Community Engagement and Planning [CEP]) versus technical assistance (Resources for Services [RS]) for depression collaborative care and the effects of social determinants on long-term remission outcomes.
Methods. We randomized 95 health care and community programs in Los Angeles County, California, to CEP or RS. In 2010, 1246 depressed (Patient Health Questionnaire [PHQ-8] ≥ 10) adults enrolled and were invited for baseline and 6-, 12-, and 36-month surveys. Of 598 3-year completers, 283 participated at 4 years (2016). We examined effects of CEP versus RS, social factors (e.g., family income, food insecurity) on time to and periods in clinical (PHQ-8 < 10) and community-defined (PHQ-8 < 10 or PHQ-2 < 3; mental health composite score [MCS-12] > 40, or mental wellness) remission during the course of 3 years, and at 4 years.
Results. We found that CEP versus RS increased 4-year depression remission and, for women, community-defined remission outcomes during the course of 3 years. Social factors and clinical factors predicted remission.
Conclusions. At 4 years, CEP was more effective than RS at increasing depression remission.
Public Health Implications. Coalitions may improve 4-year depression remission, while addressing social and clinical factors associated with depression may hold potential to enhance remission.
Depressive disorders are a leading cause of disability.1 Ethnic and racial disparities persist in access to and quality of services and outcomes.2 High stigma, low access to services, and high prevalence of adverse social determinants of health increase outcome disparities.3 Collaborative care is an evidence-based approach to team-based quality improvement for depression services, mainly in primary care. It supports evidence-based treatments including medication and psychotherapy, with support for case management, team coordination, and outcomes tracking.4 While implementing collaborative care may reduce depression disparities,5 it may be unavailable in underresourced communities, where depressed persons often seek help in community sectors such as social services rather than health care settings.2,6 Multisector coalitions of health care and non–health care programs are 1 approach to promote networks across communities to address depression and underlying social factors. However, limited data exist on effects of coalitions versus alternative models to improve health.7
Community Partners in Care (CPIC) compared a multisector coalition model (Community Engagement and Planning [CEP]) versus individual program technical assistance (Resources for Services [RS]) to implement depression collaborative care across health and community sectors.6,8–11 CPIC was developed with stakeholder input on addressing depression,6,8,12 grounded in a socioecological framework that considers adverse social determinants as contributing to depression and disparities in services access. Multisector coalitions (CEP), compared with individual program trainings (RS) were hypothesized to improve access to evidence-based treatments and support for social determinants and social factors such as interpersonal stigma, relationship problems, and social support.3 In RS, participating programs were offered culturally competent technical assistance through 12 webinars and 1 site visit per primary care site to implement depression collaborative care toolkits, without support for coalition development. The CEP coalition used the same toolkits as RS but also included support to build multisector coalitions (see “Interventions” section). The CEP coalitions worked together to adapt and improve the toolkits based on community priorities as well as develop plans for training across sites, implementation, and maintenance of the intervention.
At 6-month follow-up, CEP was more effective than RS in reducing the probability of having poor mental health–related quality of life (MHRQL), behavioral health hospitalization, and homelessness risk factors. The CEP coalition increased the main community-prioritized outcome of mental wellness, defined through a participatory process as having peace of mind, energy, or some happiness with concepts matched to items from validated surveys.9 During the course of 6 to 12 months, analyses suggested that CEP relative to RS reduced having poor MHRQL and behavioral health hospitalizations.10 At 3-year follow-up, CEP improved physical health–related quality of life and reduced behavioral health hospitalization days.13 There were no intervention effects on depressive symptoms.
During participatory review of findings, stakeholders hypothesized that initial intervention benefits on MHRQL followed by physical health gains might have subsequent effects on remission of depressive symptoms or “community-defined” remission. Community-defined remission included not having either depression or poor MHRQL, or having mental wellness.9 Given evidence of long-term benefits of depression collaborative care in primary care among minorities,14 stakeholders hypothesized that CEP relative to RS would increase the chances of remission over time, periods in remission during the course of 3 years, and being in remission at 4 years.
This study provides exploratory, secondary analyses of CPIC data to estimate effects of CEP versus RS on time to and number of periods in remission during the course of 3 years,13 and primary analyses of remission at 4-year follow-up of the 3-year sample, collected through the Community and Patient Partnered Research Network.12 Because CPIC focused on underresourced groups,6 we expected modest effects of social determinant factors on outcomes, given restricted variation from high exposure in underresourced communities. We hypothesized that CEP versus RS would improve community-defined remission but not clinical remission, given previous findings.9,11,13 Because intervention effects may be mediated through social determinants, self-efficacy, and social factors, we controlled for their baseline status. For clinical remission,15 we anticipated no intervention effects, but expected to observe direct effects of social determinants.
METHODS
CPIC was a cluster-randomized trial conducted in South and Hollywood-Metro Los Angeles, California, with high representation of lower-income groups and racial/ethnic minorities.9 Funded in 2007, CPIC was not considered a clinical trial by the National Institutes of Health; study design and procedures are reported elsewhere.6,8–11,13
Study Participants and Randomization
CPIC included programs offering services considered relevant to depression by community stakeholders.8 This included mental health, primary care, public health, substance use, social services, faith-based organizations, park and recreation senior centers, hair salons, and exercise clubs.8 We included programs serving community-prioritized subgroups: homeless, seniors, African Americans, and substance misuse clients. We identified programs by using Los Angeles County directories and stakeholder nominations. We recruited programs serving adults and expected to operate at least 1 to 3 years. Of 194 identified programs, 133 were potentially eligible and randomized (65 RS, 68 CEP). After randomization, staff blinded to assignment conducted site visits to confirm participation and eligibility; 20 programs were ineligible, 18 refused, and 95 enrolled (46 RS, 49 CEP). Participating and nonparticipating programs were comparable in neighborhood demographics.9 Within programs, clients were screened for eligibility by staff blinded to intervention status. Eligible participants were English- or Spanish-speaking adults with at least moderate depression (modified Patient Health Questionnaire16 [PHQ-8] ≥ 10) and provided contact information.9
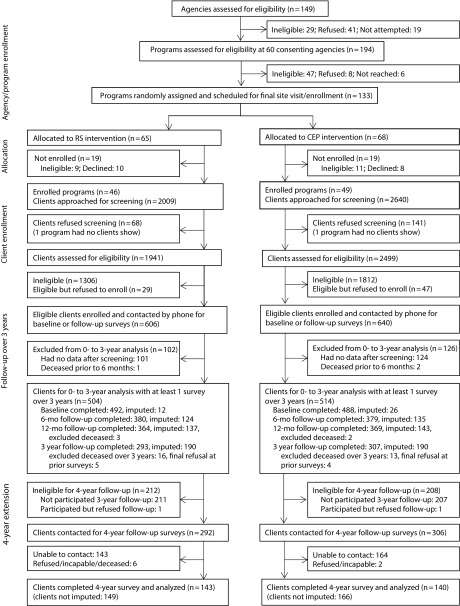
In the main study, staff approached 4649 adults for eligibility (Figure 1); 4440 (96%) agreed to participate in 93 programs. Of these, 1322 (30%) were eligible, and 1246 (94%) of the eligible adults consented. Of these, 981 (79%) completed baseline telephone surveys. Enrolled participants were invited to complete 6- and 12-month follow-up, except those whose previous survey status was ill, incarcerated, unable to contact, or deceased (see Appendix section 1, available as a supplement to the online version of this article at http://www.ajph.org).9,10 The analytic sample for the main study during the course of 12 months comprised 1018 individuals who completed 1 or more surveys at baseline, 6 months, or 12 months. For a 3-year extension study, staff attempted to contact 1004 participants who were eligible for 3-year surveys: enrolled, completed baseline or any follow-up, and neither refused follow-up nor were reported deceased at previous surveys. Of those, 600 participated (60%; RS 293, CEP 307), 24 were deceased (RS 13, CEP 11), 10 refused (RS 7, CEP 3), 3 were ill or incapable (RS 2, CEP 1), and 367 were not reached (RS 181, CEP 186).13 At 4 years, we attempted to contact 598 (RS 292, CEP 306) 3-year participants excluding 2 that declined follow-up (RS 1, CEP 1). Of those, 283 (47.3%) participated (RS 143, CEP 140), with 308 not reached (RS 143, CEP 165), 1 deceased (RS 1, CEP 0), 5 refused (RS 5, CEP 0), and 1 too ill to participate (RS 0, CEP 1). See Table A (available as a supplement to the online version of this article at http://www.ajph.org) for 4-year participation predictors.
FIGURE 1—
Study Profile: Community Partners in Care, Los Angeles County, California, 2010–2016
Notes. CEP = Community Engagement and Planning; RS = Resources for Services.
With program-level randomization within communities, intervention contamination is a potential limitation. At baseline and at 6-month and 12-month follow-up, individuals were asked to provide locations for up to 4 programs visited per sector, matched to CEP and RS sites. As reported elsewhere,13 the percentage with any visit in the opposite arm at baseline (before intervention) was 12% for RS and 19% for CEP; at 6 months: 9% for RS and 13% for CEP; at 12 months: 9% for RS and 12% for CEP. This is a moderate contamination, which could bias results toward understating CEP effects.
Interventions
Both CEP and RS supported use of depression toolkits for cognitive behavioral therapy for depression, clinician assessment, medication management, case management, lay health worker support, and team leadership.17–20 Interventions used an encouragement approach, with providers and programs able to use resources for any clients, and clients able to access services following their choices.
The RS intervention used a “train-the-trainer” approach, inviting individual programs to attend twelve 90- to 120-minute webinars in addition to a visit by trainers to primary care sites. Trainers included psychiatrists, a nurse care manager, experts in cognitive behavioral therapy, community outreach, and support staff. There was no capacity development for program collaboration.
The CEP intervention used a multisector coalition development approach. This involved inviting program administrators to attend 2-hour meetings biweekly for 4 months to plan and implement initial trainings collaboratively, followed by bimonthly meetings to monitor progress during the course of a year. Coalitions, co-led by academic and community members, reviewed and adapted toolkits to local culture and assets and developed a written training and monitoring plan. Each CEP council was provided $15 000 to support planning and innovations.13 Final plans featured half- or full-day conferences open to all staff, follow-up trainings, telephone and webinar supervision, and innovations such as training in alternative health practices and psycho-education on cognitive behavioral therapy led by lay persons. Staff participation in trainings was greater in CEP than in RS.11
Data Sources
We used data from clients’ telephone surveys at baseline, 6- and 12-month follow-up, 3-year extension study, and 4-year follow-up of 3-year participants. Survey staff were blinded to randomization status.
Measures
The CPIC study had 2 primary outcomes: poor MHRQL (12-item mental health composite score, [MCS-12] ≤ 40, and depressive symptoms (PHQ-8 ≥ 10 or PHQ-2 ≥ 3 for 4-year follow-up)16; and a community-prioritized outcome of mental wellness (a response of at least “a good bit of the time” in the previous 4 weeks to feeling calm or peaceful, having energy, or being happy), based on community input matched to the 36-item short-form health survey quality-of-life items.9,21 We developed 2 indicators: “clinical remission” (PHQ-8 < 10 or PHQ-2 < 3) and, with stakeholder input, “community-defined remission” (PHQ-8 < 10 or PHQ-2 < 3 or MCS-12 > 40 or any mental wellness). We also used a count of survey periods in remission from baseline up to 3-year follow-up. Intervention status was the client’s program assignment at enrollment to CEP or RS.
For analyses of years 0 to 3, we included baseline covariates: social determinants (family income from work of $10 000 or less in the past 12 months, food insecurity in the past 6 months)22,23; depression treatment self-efficacy (i.e., the average of 3 items on a 10-point scale of how confident respondents are in overcoming or controlling depression, taking effective action to treat depression, and managing side effects of antidepressant medications)24,25; a measure of relationship problems in past 6 months (i.e., sum of 3 items with yes-or-no response: had arguments or other difficulties with people at work in the past, a serious argument with someone, a serious problem with friends or relatives)25; a single-item social–emotional support indicator (i.e., availability of someone to have a good time with, with 6 responses from none to all of the time; correlation 0.84 with emotional support subscale in these data)26,27; and a single social-stigma item (i.e., how much relationships with friends would suffer27 if they thought you had a recent history of depression, with 4 responses from none to a lot); and clinical status (Mini-International Neuropsychiatric Interview, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)28 diagnosis of depressive disorder in past 12 months and 3 or more chronic medical conditions from 18).
Data Analyses
3-year secondary analyses.
We conducted intent-to-treat analyses with intervention status as the main independent variable. For time (survey period) to first remission, we used Cox proportional hazard models for the full sample with any survey data (n = 1018), limited to those at risk for subsequent clinical (n = 995) and community-defined (n = 408) remission at baseline. We used linear regression for number of periods in remission during the course of 3 years for the full sample (n = 1018).13 We developed models including intervention status, adding social determinants, then depression treatment self-efficacy, then social context (problems, support, stigma) and clinical indicators. The final model included intervention status and predictors significant in preliminary models at P < .05 or greater for clinical or community-prioritized remission. We report models with intervention status only and the final model. We used item-level imputation for missing data,29,30 and wave-level imputation and weights to account for nonenrollment and participation in the 3-year extension study (see Appendix sections 3 and 4, available as a supplement to the online version of this article at http://www.ajph.org).31 For all Cox regression models, predictors including intervention status met the proportionality assumption (Table B, available as a supplement to the online version of this article at http://www.ajph.org).32
For 4-year end status.
We conducted intent-to-treat analyses with intervention status as the main independent variable, using logistic regression for probability of remission (clinical, community-defined) for the sample with 4-year data (n = 298). Of 20 baseline variables tested, intervention status differed for the baseline social–emotional support item (Table 1). We conducted analyses parallel to the 3-year analyses noted previously. We included weights for enrollment and participation at 4 years (see Appendix section 2, available as a supplement to the online version of this article at http://www.ajph.org). For a sensitivity analysis, we conducted an analysis equivalent to the primary intervention analysis from the 3-year extension study,13 using the same covariates plus baseline measure of the outcome and the 1 baseline item differing by intervention status among 4-year completers (Table C, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Baseline Sociodemographic, Clinical, and Social Risk Factors: Community Partners in Care, Los Angeles County, California, 2010–2011
| Baseline Characteristics | 3-Year Analytic Sample, 2010–2014 |
At 4-Year Analytic Sample, 2016 |
||||
| Overall (n = 1018), No. (%) or Mean ±SD | RS (n = 504), No. (%) or Mean ±SD | CEP (n = 514), No. (%) or Mean ±SD | Overall (n = 283), No. (%) or Mean ±SD | RS (n = 143), No. (%) or Mean ±SD | CEP (n = 140), No. (%) or Mean ±SD | |
| Age, y | 45.8 ±12.9 | 44.9 ±12.4 | 46.6 ±13.2 | 45.3 ±11.8 | 44.7 ±11.6 | 45.9 ±11.9 |
| Female sex | 595 (57.0) | 286 (54.8) | 309 (59.1) | 185 (58.5) | 91 (56.6) | 94 (60.4) |
| Race/ethnicity | ||||||
| Hispanic/Latino | 409 (41.0) | 194 (38.8) | 215 (43.1) | 102 (38.7) | 47 (36.0) | 55 (41.2) |
| African American | 488 (46.0) | 239 (46.9) | 249 (45.0) | 142 (49.5) | 72 (51.3) | 70 (47.7) |
| Non-Hispanic White | 86 (9.2) | 45 (9.7) | 41 (8.8) | 31 (8.8) | 18 (9.6) | 13 (8.1) |
| Other | 35 (3.8) | 26 (4.6) | 9 (3.1) | 8 (3.1) | 6 (3.1) | 2 (3.0) |
| Married or living with partner | 231 (22.6) | 116 (22.6) | 115 (22.6) | 65 (25.4) | 30 (23.8) | 35 (27.0) |
| < high school education | 446 (43.6) | 221 (43.7) | 224 (43.5) | 125 (42.1) | 59 (43.3) | 66 (41.0) |
| Income under 2010 federal poverty levela | 750 (73.7) | 373 (74.5) | 377 (73.0) | 203 (74.6) | 102 (74.2) | 101 (75.0) |
| Family income from work past 12 mo ≤ $10 000 | 811 (80.1) | 404 (80.5) | 408 (79.7) | 223 (81.3) | 114 (83.1) | 109 (79.5) |
| Social determinants, self-efficacy, and social context | ||||||
| Worried that the food would not last, past 6 mo | 574 (56.8) | 284 (57.1) | 290 (56.5) | 159 (57.5) | 84 (58.2) | 75 (56.9) |
| Depression treatment self-efficacyb | 5.8 ±2.3 | 5.7 ±2.3 | 5.8 ±2.3 | 5.8 ±2.3 | 5.7 ±2.2 | 5.9 ±2.3 |
| Relationship problems subscalec | 0.9 ±0.9 | 0.9 ±0.9 | 0.9 ±0.9 | 0.9 ±0.9 | 1.0 ±0.9 | 0.8 ±0.9 |
| Relationships suffer if you had depression (stigma)d | 2.4 ±1.2 | 2.5 ±1.2 | 2.4 ±1.2 | 2.4 ±1.2 | 2.5 ±1.2 | 2.3 ±1.2 |
| Someone to have a good time with (social support)e | 3.0 ±1.7 | 2.9 ±1.7 | 3.1 ±1.7 | 3.1 ±1.8 | 2.8 ±1.7 | 3.4 ±1.8 |
| Clinical status | ||||||
| Depressive disorder in past 12 mo | 629 (61.9) | 311 (62.4) | 318 (61.4) | 178 (65.9) | 93 (67.2) | 84 (64.7) |
| Alcohol abuse or use of illicit drugs 12 mo | 398 (39.3) | 180 (36.3) | 218 (42.2) | 91 (38.6) | 35 (35.3) | 56 (41.8) |
| ≥ 3 chronic medical conditions of 18 | 548 (54.7) | 270 (54.4) | 278 (55.1) | 165 (52.2) | 89 (56.0) | 75 (48.6) |
| PHQ-8f | 15.0 ±4.1 | 15.1 ±4.2 | 14.9 ±4.1 | 14.8 ±4.0 | 15.2 ±4.2 | 14.4 ±3.8 |
| PHQ-8 < 10 or MCS-12g > 40 or wellnessh | 610 (59.9) | 301 (59.4) | 309 (60.4) | 174 (59.2) | 83 (58.0) | 91 (60.4) |
Note. CEP = Community Engagement and Planning; MCS = mental health composite score; PHQ = Patient Health Questionnaire; RS = Resources for Services or individual program technical assistance. Over 3-year sample with any survey data (n = 1018), data were multiply imputed and weighted for eligible sample for enrollment; 4-year analytic sample (n = 283) was weighted to eligible sample for 4-year survey, with item-level imputation; χ2 test was used for a comparison between the 2 groups, accounting for the design effect of the cluster randomization; intervention groups were balanced at baseline except for 4-year sample, with greater social support for CEP versus RS.
As defined by the US Census.
Possible scores range from 0 = not at all confident to 10 = extremely confident.
Sum of 3 items with yes or no response for the past 6 months: had arguments or other difficulties with people at work, a serious argument with someone, a serious problem with friends or relatives.
How much relationships with friends would suffer if they thought you had a recent history of depression with 4 responses from 1 = none to 4 = a lot.
Availability of someone to have a good time with (social support), with 6 responses from 1 = none of the time to 6 = all of the time.
Possible scores range from 0 to 24, with higher scores indicating greater depression severity.
Possible scores range from 0 to 100, with higher scores indicating better mental health–related quality of life.
At least a good bit of time on any of 3 items: feeling peaceful or calm, being a happy person, having energy.
For all analyses.
We used SUDAAN software version 11.0.1 (RTI International, Research Triangle Park, NC) to account for clustering (clients within programs) and weighting. We estimated variances via implicit Taylor linearization (a form of generalized estimating equations).33,34 We assessed significance of comparisons by using contrasts among regression coefficients. Results are presented as hazard ratios (HRs) for Cox proportional hazards, between-group difference for linear, and odds ratios (ORs) for logistic regressions, with 95% confidence intervals (CIs).9 We used 2-sided tests with P < .05 for statistical significance. Analyses were exploratory. We did not formally adjust for multiple statistical comparisons, but discuss implications. Because findings of a previous subanalysis suggested positive coalition effects among women,25 we included such subanalyses for 3-year analyses; the 4-year sample was too small.
RESULTS
The majority of clients were of racial/ethnic minority background with family incomes under 2010 US federal poverty level as defined by the US Census Bureau, and had 12-month depressive disorder and multiple chronic medical conditions. For the 3-year sample, intervention conditions were balanced in demographic factors and baseline measures of outcomes and predictors used in all models (Table 1). For the 4-year sample, participants in CEP versus RS had greater social–emotional support by the single-item measure.
Intervention Effects
The mean time to the first clinical remission during the course of 3 years was 20.6 months (SD = 14.0) and for community-defined remission was 13.1 (SD = 5; Table D, available as a supplement to the online version of this article at http://www.ajph.org). The mean number of periods in remission was 1.09 (SD = 1.0) and 2.7 (SD = 1.1) for clinical remission and community-defined remission, respectively. As shown in Table 2, there was an effect of CEP versus RS on community-defined time to remission, with an HR of 1.26 (95% CI = 1.01, 1.56) in the unadjusted model, but not significant in the final model, which had an HR of 1.23 (95% CI = 0.99, 1.52). For time to clinical remission, there were no noteworthy intervention effects. Among women, for community-defined remission, the intervention effect had an HR of 1.39 (95% CI = 1.03, 1.88). There were no significant intervention effects on the number of periods in remission for the whole sample. However, among women, CEP versus RS was associated with more periods in community-defined remission in the final model (regression b = 0.21; 95% CI = 0.01, 0.40; Table 2).
TABLE 2—
Effects of Interventions and Covariates on Remission Outcomes: Community Partners in Care, Los Angeles County, California, 2010–2014
| Whole Analytic Sample |
Female Subsample |
|||
| Clinical Remission | Community-Defined Remission | Clinical Remission | Community-Defined Remission | |
| Time to remission during the course of 3 years (not in remission at baseline), HR (95% CI)a | ||||
| Sample size | n = 995b | n = 408c | n = 584b | n = 231c |
| Model 1: intervention status (CEP vs RS) | 1.13 (0.86, 1.50) | 1.26 (1.01, 1.56) | 1.20 (0.86, 1.66) | 1.44 (1.08, 1.91) |
| Model 2: final model | ||||
| Intervention (CEP vs RS) | 1.12 (0.83, 1.50) | 1.23 (0.99, 1.52) | 1.21 (0.87, 1.69) | 1.39 (1.03, 1.88) |
| Relationships suffer if you had depression (stigma) | 0.90 (0.83, 0.97) | 0.95 (0.85, 1.06) | 1.04 (0.99, 1.09) | 1.07 (1.00, 1.13) |
| Depressive disorder in past 12 mo | 0.59 (0.48, 0.72) | 0.66 (0.51, 0.86) | 0.55 (0.45, 0.67) | 0.58 (0.42, 0.81) |
| ≥ 3 chronic medical conditions of 18 | 0.72 (0.59, 0.88) | 0.83 (0.65, 1.06) | 0.78 (0.62, 0.99) | 0.93 (0.66, 1.30) |
| Number of periods in remission during the course of 3 y, b (95% CI)a | ||||
| Sample size | n = 1018 | n = 595 | ||
| Model 1: intervention status (CEP vs RS) | 0.07 (−0.13, 0.27) | 0.14 (−0.08, 0.36) | 0.11 (−0.13, 0.34) | 0.24 (−0.01, 0.49) |
| Model 2: final model | ||||
| Intervention (CEP vs RS) | 0.05 (−0.12, 0.23) | 0.11 (−0.06, 0.29) | 0.10 (−0.10, 0.30) | 0.21 (0.01, 0.40) |
| Family income from work past 12 mo ≤ $10 000 | −0.20 (−0.38, −0.02) | −0.07 (−0.25, 0.11) | −0.23 (−0.49, 0.03) | −0.17 (−0.38, 0.05) |
| Worried that the food would not last, past 6 mo | −0.08 (−0.22, 0.05) | −0.17 (−0.30, −0.04) | −0.07 (−0.25, 0.12) | −0.25 (−0.42, −0.08) |
| Depression treatment self-efficacy | 0.03 (0.00, 0.06) | 0.05 (0.02, 0.09) | 0.04 (0.00, 0.07) | 0.06 (0.02, 0.10) |
| Relationships suffer if you had depression (stigma) | −0.07 (−0.12, −0.02) | −0.07 (−0.14, 0.00) | . . . | . . . |
| Someone to have a good time with (social support) | 0.03 (−0.01, 0.06) | 0.08 (0.04, 0.12) | 0.05 (0.00, 0.10) | 0.09 (0.03, 0.15) |
| Depressive disorder in past 12 mo | −0.41 (−0.56, −0.25) | −0.50 (−0.66, −0.34) | −0.50 (−0.67, −0.34) | −0.57 (−0.75, −0.39) |
| ≥ 3 chronic medical conditions of 18 | −0.33 (−0.48, −0.18) | −0.22 (−0.36, −0.07) | −0.26 (−0.45, −0.07) | −0.14 (−0.34, 0.05) |
Note. CEP = Community Engagement and Planning; CI = confidence interval; HR = hazard ratio; RS = Resources for Services.
Data were multiply imputed and weighted for eligible sample for enrollment and accounted for the design effect of the cluster randomization.
Sample does not include persons in clinical remission at baseline.
Sample does not include persons in community-defined remission at baseline.
For intervention effects at 4-year end status, CEP versus RS increased odds of being in both clinical and community-defined remission, with similar findings in unadjusted and final adjusted models (Table 3) and in a sensitivity analysis using the same covariate strategy as the 3-year primary analyses (Table C).13 The intervention effect was significant for clinical (OR = 1.73; 95% CI = 1.01, 2.99) and community-defined remission (OR = 2.43; 95% CI = 1.17, 5.02; Table 3).
TABLE 3—
Odds Ratios for Likelihood of Remission by Intervention Status (4-Year Sample n = 283): Community Partners in Care, Los Angeles County, California, 2010–2016
| Secondary Analyses, Adjusted for Social Determinants, Self-Efficacy, Social Context, and Clinical Status (Full Sample) | Clinical Remission (n = 130), OR (95% CI) | Community-Defined Remission (n = 227), OR (95% CI) |
| Model 1: intervention status (CEP vs RS) | 1.91 (1.11, 3.28) | 2.68 (1.32, 5.42) |
| Model 2: final model | ||
| Intervention (CEP vs RS) | 1.73 (1.01, 2.99) | 2.43 (1.17, 5.02) |
| Depression treatment self-efficacy | 1.13 (1.00, 1.28) | 1.14 (1.02, 1.27) |
| Someone to have a good time with (social support) | 1.13 (0.94, 1.36) | 1.26 (1.00, 1.59) |
| ≥ 3 chronic medical conditions of 18 | 0.46 (0.27, 0.79) | 0.85 (0.37, 1.97) |
Note. CEP = Community Engagement and Planning; CI = confidence interval; OR = odds ratio; RS = Resources for Services. Data were multiply imputed and weighted for eligible sample for enrollment and accounted for the design effect of the cluster randomization.
Effects of Covariates
For the 3-year sample, in final models, the baseline social stigma item and clinical status indicators were each associated with greater time to clinical remission, and baseline clinical status indicators were associated with time to community-defined remission (12-month depressive disorder: HR = 0.66; 95% CI = 0.51, 0.86; Table 2).
For number of periods in clinical remission, baseline predictors included low family income from work (b = −0.20; 95% CI = −0.38, −0.02), social stigma (b = −0.07; 95% CI = −0.12, −0.02), depressive disorder (b = −0.41; 95% CI = −0.56, −0.25), and 3 or more chronic medical conditions (b = −0.33; 95% CI = −0.48, −0.18). For community-defined remission, baseline predictors included food insecurity (b = −0.17; 95% CI = −0.30, −0.04), depression treatment self-efficacy (b = 0.05; 95% CI = 0.02, 0.09), social stigma (b = −0.07; 95% CI = −0.14, 0.00), social–emotional support (b = 0.08; 95% CI = 0.04, 0.12), depressive disorder (b = −0.50; 95% CI = −0.66, −0.34), and 3 or more chronic medical conditions (b = −0.22; 95% CI = −0.36, −0.07; Table 2).
For parallel analyses of 4-year end status (Table 3), final models had associations of depression treatment self-efficacy with clinical and community-defined remission (OR = 1.13; 95% CI = 1.00, 1.28; and OR = 1.14; 95% CI = 1.02, 1.27, respectively), social support with community-defined remission (OR = 1.26; 95% CI = 1.00, 1.59), and chronic medical conditions with clinical remission (OR = 0.46; 95% CI = 0.27, 0.79).
DISCUSSION
In this study, we explored secondary analyses of CPIC 3-year data9,10,13 and primary analyses of 4-year follow-up of 3-year participants.12 We compared 2 interventions to implement evidence-based toolkits for improving depression services. One (RS) provided technical assistance to individual programs and the other (CEP) supported collaboration across sectors in planning for training, monitoring, and oversight, under a community-engagement approach. The parent study was guided by community input on addressing depression and on study design. We found that CEP versus RS increased the likelihood of clinical and community-defined remission for depressed adults in underresourced communities at 4-year follow-up. For time to first remission and number of periods in remission during the course of 3 years, we observed no significant intervention effects for clinical or community-defined remission for the whole sample in final models. For women, CEP relative to RS was associated with earlier time to remission and more periods in community-defined remission, an important area for future disparities research.
The finding of an intervention effect on remission at 4 years is consistent with feedback from stakeholders that earlier intervention effects on physical health and reducing hospitalizations could lead to longer-term remission, inspiring 4-year data collection. We note that the 4-year response rate was low and participants were somewhat older, more likely to be employed, and in worse physical health than were nonparticipants. However, within this sample, intervention arms were balanced in baseline characteristics (only 1 characteristic differed out of 20 examined), and intervention effects were consistently significant.
In addition, because the 4-year sample is a follow-up of the 3-year sample, we conducted a sensitivity analysis of intervention effects on 3-year outcomes for the 4-year subsample. We found similar intervention effects on health for the full and 4-year subsample, including no significant effects on mental health at 3 years for either full or 4-year samples. This suggests that the 4-year sample is not necessarily more sensitive to mental health benefits of CEP. Nevertheless, future research should clarify intervention effects among younger, less employed, or physically healthier adults. Because 4-year follow-up was conducted 3 years after intervention support ended, even findings with these limitations may suggest potential for longer-term effects through building program capacity or client learning.
Another exploratory feature was examining associations of baseline indicators of social determinants, social contextual factors (stigma and depression treatment self-efficacy), and clinical status with remission outcomes. We found that clinical status indicators were associated with each remission outcome in 3-year analyses and with 4-year clinical remission. Social stigma was associated with greater time to clinical remission and fewer periods in clinical and community-defined remission during the course of 3 years. Family income from work was associated with periods in clinical remission, and food insecurity with periods in community-defined remission. Depression treatment self-efficacy and social–emotional support were associated with number of periods in community-defined remission during the course of 3 years and community-defined remission at 4 years, and treatment self-efficacy with clinical remission at 4 years. It is possible that enhancing interventions to address these factors could improve outcomes—an issue for future research.
Limitations
The study had important limitations. The 4-year survey was limited to 3-year survey responders, with low response rate (47.3%), but balanced groups by arm. Findings may differ for less-represented younger persons. The study was conducted in 2 Los Angeles communities with high prevalence of adverse social determinants, and replication elsewhere is important. We included some social determinant indicators, but other factors could also be predictors and are important to explore in future studies. Data were self-reported and potentially subject to recall bias. Both interventions implemented evidence-based approaches to improve depression services, as a usual-care control was considered unethical by partners.2 Thus, outcome differences may be expected to be modest. Program administrators in CEP were given participant rosters for safekeeping, which could partly explain early improvements relative to RS, but would be unlikely to explain long-term effects. We did not adjust for multiple statistical comparisons, but intervention effects on 4-year community-defined remission would survive formal adjustment for 2 primary outcomes. With program randomization within communities, contamination can be a limitation, leading to understating CEP effects relative to RS. In the parent study, contamination was moderate (> 20%), declining over time.
Public Health Implications
The findings reinforce the value of community input through a participatory process in defining relevant outcomes and hypotheses. Potential explanations for advantages of CEP include greater activation of providers in trainings, alternative sectors for case management, and networks to bridge gaps in services for depression and underlying social factors. The latter may be important because, as predicted by stakeholders, social determinants (i.e., family income, food insecurity) predicted remission. More extensive work on how communities frame and are affected by social determinants could further inform interventions. A similar coalition model supported recovery after Hurricane Katrina in New Orleans, Louisiana,20 and the authors are collaborating in a randomized trial in Louisiana of coalitions versus technical support for depression, social determinants, and disaster exposure. CPIC was noted in a Cochrane Review as a unique trial of coalitions relative to alternative approaches in minority communities.7 Therefore, these long-term findings may encourage exploration of coalition models while giving explicit attention to social determinants under a participatory, public health paradigm.
ACKNOWLEDGMENTS
This study was supported by the PCORnet Community and Patient Partnered Research Network, Patient Centered Outcomes Research Institute contract 1845 and PPRN-1501-26518 and R01MD007721 from the National Institute on Minority Health and Health Disparities. The parent Community Partners in Care (CPIC) study was supported by R01MH078853, P30MH082760, and P30MH068639 from the National Institute of Mental Health, grant 64244 from the Robert Wood Johnson Foundation, CMCH-12-97088 from the California Community Foundation, G08LM011058 from the National Library of Medicine, and UL1TR000124 from the National Institutes of Health/National Center for Advancing Translational Science UCLA Clinical and Translational Science Institute.
We acknowledge posthumously Loretta Jones, MA, ThD, who passed away during review of this manuscript.
The RAND Corporation, UCLA Semel Institute, and the Los Angeles County Departments of Mental Health, Public Health, and Health Services provided institutional support. We thank 95 participating health care and community-based agencies, the CPIC Council, and members of the Association of Clinical and Translational Science Team Science Award for CPIC (2014), and Campus–Community Partnerships for Health 2015 Annual Award. We thank Erika Orellana for support for article preparation.
The CPIC Writing Group consisted of Bowen Chung, MD, MSHS, Nichole Goodsmith, MD, PhD, Elizabeth Moore, MD, Nicolas Barcelo, MD, James Gilmore, MBA, Michael K. Ong, MD, PhD, Wayne Aoki, PhD, Thomas Belin, PhD, Elizabeth Bromley, MD, PhD, Elizabeth Dixon, RN, PhD, Megan D. Johnson, MD, MPH, Paul Koegel, PhD, Dmitry Khodyakov, PhD, Craig M. Landry, PhD, Elizabeth Lizaola, MPH, Norma Mtume, MA, LCSW, Victoria K. Ngo, PhD, Judith Perlman, MA, Esmeralda Pulido, MPH, Vivian Sauer, LCSW, Yolanda Whittington, LCSW, Pluscedia Williams, Aziza Lucas-Wright, MEd, Lily Zhang, MS, Marvin Southard, DSW, Krystal Griffith, MPH, Enrico Castillo, MD, Kristen Choi, PhD, Joseph Mango, MFA, Erika Orellana, Rosalinda Cardenas, Nancy Alfaro, Benjamin Springgate, MD, MSHS, Ashley Wennerstrom, PhD, Olivia K. Sugarman, MPH, and Kenneth Wells, MD, MPH.
CONFLICTS OF INTEREST
The authors declare no relevant conflicts of interest.
HUMAN PARTICIPANT PROTECTION
The study was approved by the RAND institutional review board.
REFERENCES
- 1.Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. doi: 10.1001/jama.2017.3826. [DOI] [PubMed] [Google Scholar]
- 2.Miranda J, McGuire T, Williams D, Wang P. Mental health in the context of health disparities. Am J Psychiatry. 2008;165(9):1102–1108. doi: 10.1176/appi.ajp.2008.08030333. [DOI] [PubMed] [Google Scholar]
- 3.Silva M, Loureiro A, Cardoso G. Social determinants of mental health: a review of the evidence. Eur J Psychiatry. 2016;30(4):259–292. [Google Scholar]
- 4.Thota AB, Sipe TA, Byard GJ et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42(5):525–538. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 5.Miranda J, Chung JY, Green BL et al. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 6.Miranda J, Ong MK, Jones L et al. Community-partnered evaluation of depression services for clients of community-based agencies in under-resourced communities in Los Angeles. J Gen Intern Med. 2013;28(10):1279–1287. doi: 10.1007/s11606-013-2480-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner‐Brown J, Krause LK. Community coalition‐driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015;6:CD009905. doi: 10.1002/14651858.CD009905.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung B, Dixon EL, Miranda J, Wells K, Jones L. Using a community partnered participatory research approach to implement a randomized controlled trial: planning Community Partners in Care. J Health Care Poor Underserved. 2010;21(3):780–795. doi: 10.1353/hpu.0.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells KB, Jones L, Chung B et al. Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med. 2013;28(10):1268–1278. doi: 10.1007/s11606-013-2484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung B, Ong M, Ettner SL et al. 12-month outcomes of community engagement versus technical assistance to implement depression collaborative care: a partnered, cluster, randomized, comparative effectiveness trial. Ann Intern Med. 2014;161(10 suppl):S23–S34. doi: 10.7326/M13-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung B, Ngo V, Ong M et al. Participation in training for depression care quality improvement: a randomized trial of community engagement or technical support. Psychiatr Serv. 2015;66(8):831–839. doi: 10.1176/appi.ps.201400099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arevian AC, Castillo EG, Chung B et al. The Community and Patient Partnered Research Network (CPPRN): application of patient-centered outcomes research to promote behavioral health equity. Ethn Dis. 2018;28(suppl):295–302. doi: 10.18865/ed.28.S2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ong MK, Jones L, Aoki W et al. A community-partnered, participatory, cluster-randomized study of depression care quality improvement: three-year outcomes. Psychiatr Serv. 2017;68(12):1262–1270. doi: 10.1176/appi.ps.201600488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherbourne CD, Edelen MO, Zhou A, Bird C, Duan N, Wells KB. How a therapy-based quality improvement intervention for depression affected life events and psychological well-being over time: a 9-year longitudinal analysis. Med Care. 2008;46(1):78–84. doi: 10.1097/MLR.0b013e318148478d. [DOI] [PubMed] [Google Scholar]
- 15.Rush AJ, Crismon ML, Toprac MG et al. Consensus guidelines in the treatment of major depressive disorder. J Clin Psychiatry. 1998;59(suppl):73–84. [PubMed] [Google Scholar]
- 16.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 17.Miranda J, Woo S, Lagomasino I, Hepner KA, Wiseman S, Muñoz R. BRIGHT Group Cognitive Behavioral Therapy for Depression. San Francisco, CA: San Francisco General Hospital, University of California, San Francisco; 2006. [Google Scholar]
- 18.Wells KB, Sherbourne C, Schoenbaum M et al. Impact of disseminating quality improvement programs for depression in managed primary care. JAMA. 2000;283(2):212–220. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 19.Unützer J, Katon W, Callahan CM et al. Collaborative care management of late-life depression in the primary care setting. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 20.Wennerstrom A, Vannoy SD, Allen C. Community-based participatory development of a community health worker mental health outreach role to extend collaborative care in post-Katrina New Orleans. Ethn Dis. 2011;21(suppl 1):S1-45–S1-51. [PMC free article] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 22.Sherbourne CD. The role of social support and life stress events in use of mental health services. Soc Sci Med. 1988;27(12):1393–1400. doi: 10.1016/0277-9536(88)90205-5. [DOI] [PubMed] [Google Scholar]
- 23.Office of Disease and Prevention and Health Promotion. Social determinants of health. 2018. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed April 4, 2019.
- 24.Ludman E, Katon W, Bush T et al. Behavioural factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychol Med. 2003;33(6):1061–1070. doi: 10.1017/s003329170300816x. [DOI] [PubMed] [Google Scholar]
- 25.Ngo VK, Sherbourne C, Chung B et al. Community engagement compared with technical assistance to disseminate depression care among low-income, minority women: a randomized controlled effectiveness study. Am J Public Health. 2016;106(10):1833–1841. doi: 10.2105/AJPH.2016.303304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 27.Roeloffs C, Sherbourne C, Unützer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. Gen Hosp Psychiatry. 2003;25(5):311–315. doi: 10.1016/s0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- 28.Sheehan DV, Lecrubier Y, Sheehan KH et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- 29.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Vol 81. New York, NY: John Wiley & Sons; 2004. [Google Scholar]
- 30.Lavori PW, Dawson R, Shera D. A multiple imputation strategy for clinical trials with truncation of patient data. Stat Med. 1995;14(17):1913–1925. doi: 10.1002/sim.4780141707. [DOI] [PubMed] [Google Scholar]
- 31.Korn EL, Graubard BI. Analysis of Health Surveys. Hoboken, NJ: Wiley-Interscience; 1999. [Google Scholar]
- 32.Lin DY, Wei L-J, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80(3):557–572. [Google Scholar]
- 33.Binder DA. On the variances of asymptotically normal estimators from complex surveys. Int Stat Rev. 1983;51(3):279–292. [Google Scholar]
- 34.Binder DA. Fitting Cox’s proportional hazards models from survey data. Biometrika. 1992;79(1):139–147. [Google Scholar]