Abstract
Background
The effect of laparoscopic fundoplication on reflux-related chronic cough is unpredictable, the aim of the study is to investigate the predictive effect of positive reflux-cough correlation on the resolution of reflux-related chronic cough after anti-reflux surgery.
Methods
A 5 years retrospective review was performed. Logistic regression analysis was used to determine the independent predictors on the cure of chronic cough.
Results
Seventy-nine patients were included in this study, among which chronic cough was cured in 47 (59.5%) and significantly improved in 10 (12.7%) patients. Present of typical symptoms (odds ratio = 6.435,95% confidence interval [CI] = 1.427–29.032, p = 0.015) and number of Reflux episodes (impedance) ≥73 (odds ratio = 0.306, 95% confidence interval [CI] = 0.107–0.874, p = 0.027) were significantly associated with the cure of chronic cough.
Conclusions
laparoscopic fundoplicaiton is effective for the management of reflux-related chronic cough, particularly with the present of typical symptoms.
Trial registration
(Trial registration number: ChiCTR1800016444; Trial registration date: June 01, 2018)
Keywords: Gastroesophageal reflux disease, Cough, Fundoplication
Background
Gastroesophageal reflux disease (GERD) is a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications [1, 2]. The typical symptoms of GERD are heartburn and regurgitation, while the atypical symptoms of GERD include non-cardiac chest pain and extraesophageal symptoms such as chronic cough, chronic asthma, chronic laryngitis and dental erosions [3–5]. The prevalence of GERD in East Asia is about 2.5–7.8% [6]. Chronic cough defined as cough that persisits for > 8 weeks, affects 11–20% of the adult population and significantly impairs health-related quality of life [7]. GERD symptom response rates for anti-reflux surgery varies based on 1) evidence for GERD, such as ambulatory pH monitoring metrics, PPI response and GERD phenotypes, and 2) the particular symptom [3]. while laproscopic fundoplication (LF) can control typical symptoms in about 90% of patients [8–13], the resolution of chronic cough is less predictive (about 51–96%) [9, 10, 14, 15]. Impedance-pH monitoring is widely used in the diagnosis of GERD, and its ability to simultaneously record symptoms allows evaluation of reflux-symptom correlation [16]. The aim of this study was to investgate if positive reflux-cough correlation predicts resolution of chronic cough after antireflux surgery.
Methods
Study population
We retrospectively analysis information from patients who underwent LF in The General Hospital of the PLA Rocket Force from January 2013 to December 2017. Inclusion criteria (all of the two): chronic cough persists for more than 8 weeks; complete 24-h multichannel intraluminal impedance pH (24-h MII-pH) monitoring and at least one cough was recorded. Exclusion criteria [17] (at least one): present smoker; use of angiotensin-converting-enzyme inhibitors (ACEI); abnormal chest radiograph; recently upper respiratory infection; upper airway cough syndrome; previous upper gastrointestinal surgery; malignancy; major disorders of peristalsis (absent contractility, distal esophageal spasm, and jackhammer esophagus). The following information was collected form each patient eligible for this study: demographics factors (gender, age, body mass index (BMI), hypertension, diabetes and coronary heart disease), symptoms (heartburn, regurgitation, chronic cough, chronic asthma), response of chronic cough to proton pump inhibitor (PPI), hiatal hernia presence (endoscopic and/or high resolution manometry), endoscopic factors (esophagitis, barrett’s esophagus, reflux of bile), impedance-pH monitoring factors [DeMeester score, acid exposure time (AET), bolus exposure time (BET), symptom index (SI), symptom association probability (SAP)] and high resolution manometry (HRM) determined ineffective esophageal motility (50% or more ineffective esophageal swallows).
24-h MII-pH monitoring
All reflux events were collected from pH-impedance monitoring, and all impedance-pH monitoring were performed off PPI for at least 7 days as previously described [18]. Symptoms were considered related to reflux events if they occurred within 2 min after the reflux event. The symptom index (SI) was defined as the ratio of reflux-related symptoms to the total number of symptoms [19], the sympton-association probability was calculated as Weusten [20] described. Positive reflux-cough correlation defined as SI > 50% and/or SAP > 95%.
Outcome
Eligible subjects were contacted for a telephone interview to determine symptomatic outcome of chronic cough and typical symptoms. Symptomatic outcome was considerd cured if the patient was symptom-free or minor complaints remained but required no medication (PPI, H2 receptor antagonists, prokinetic agents, antacids and antitussive); excellent if symptoms were significantly improved but required on-demand medication; fair if reflux symptoms were slightly improved and required daily dose of medication; poor if the symptoms were not improved and required more than daily dose of medication or refractory to medical therapy.
Statistical analysis
All statistical tests were performed using IBM SPSS Statistics (Version 20). The chi-square test or Fisher’s exact test was performed to evaluate univariate effects of each predictor variable on outcome (chronic cough cured or not cured). A stepwise forward logistic regression was performed to determine independent predictors of outcome (chronic cough cured or not cured). statistical significance was considered at the p < 0.05 level.
Results
Between January 2013 and December 2017, a total of 1636 patients underwent laparoscopic fundoplication, among which 97 patients meet the criteria for further follow up (Fig. 1). Fourteen patients couldn’t be reached and 4 patients died (1 for leukemia, 1 for pulmonary fibrosis and two unclear), thus 79 patients were included in this study. Among which 30 patients underwent Nissen-Rossetti procedure, 34 underwent Nissen procedure, 14 under Toupet procedure, and 1 underwent Dor procedure.
Fig. 1.
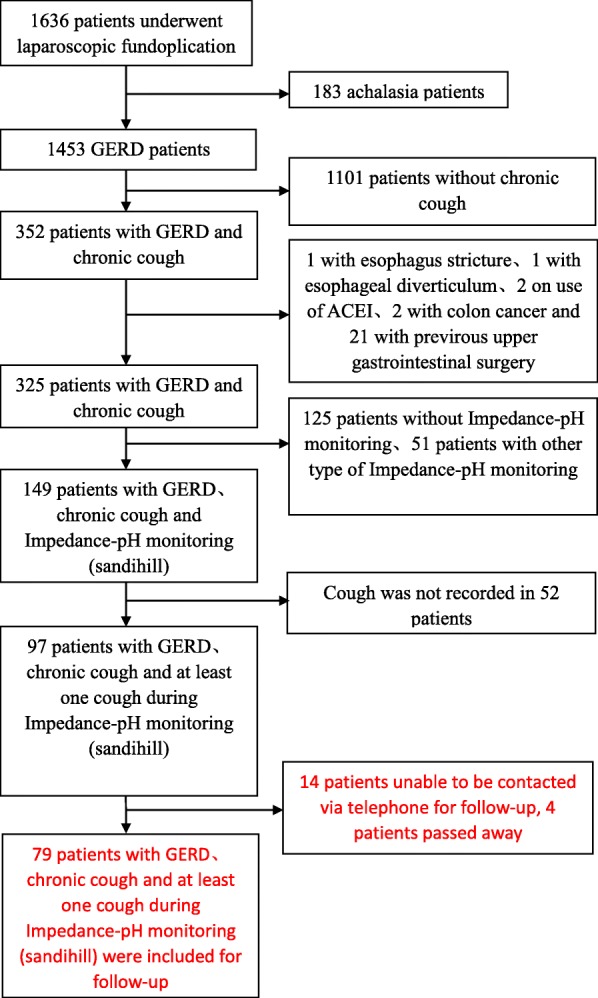
Study flow diagram
The demographics factors and symptomatic outcomes among the 79 patients were listed in Table 1 and Table 2, respectively. At a median follow-up time of 35 months after surgery (range 7–65 months), symptomatic outcome of chronic cough was rated cured in 47 (59.5%) and excellent in 10 (12.7%) of the 79 patients. Heartburn was rated cured in 47 (79.7%) and excellent in 5 (8.5%) of the 59 patients. Regurgitation was rated cured in 46 (74.2%) and excellent in 7 (11.3%) of the 62 patients.
Table 1.
Demographics factors of the study population (N = 79)
| Median age (year) | 60(range14–79) |
|---|---|
| Male | 43 (54.4%) |
| Body mass index | |
| normal(18.5–24.99) | 43 (54.4%) |
| overweight(25–29.99) | 30 (38.0%) |
| obesity(≥30) | 6 (7.6%) |
| Hypertension | 20 (25.3%) |
| Diabetes | 3 (3.8%) |
| Coronary heart disease | 3 (3.8%) |
Table 2.
symptomatic outcomes among 79 patients
| Cured | Excellent | Fair | Poor | Total | |
|---|---|---|---|---|---|
| Chronic cough | 47 (59.5%) | 10 (12.7%) | 4 (5.1%) | 18 (22.7%) | 79 |
| Heartburn | 47 (79.7%) | 5 (8.5%) | 1 (1.7%) | 6 (10.1%) | 59 |
| Regurgitation | 46 (74.2%) | 7 (11.3%) | 2 (3.2%) | 7 (11.3%) | 62 |
| Asthma | 9 (39.1%) | 4 (17.4%) | 7 (30.4%) | 3 (13%) | 23 |
At the univariate level (Table 3), three factors were significantly associated with the cure rate of chronic cough. These included typical symptoms, Number of Reflux episodes (impedance) and Ineffective esophageal motility. At the multivariate level, all the factors listed in Table 3 together with BMI (overweight, obesity vs normal) and type of surgery (Nissen-Rossetti, Nissen vs Toupet) were offered to the regression procedure. Present of typical symptoms (OR = 6.435, 95%CI = 1.427–29.032, p = 0.015) and number of Reflux episodes (impedance) ≥73 (OR = 0.306, 95%CI = 0.107–0.874, p = 0.027) were independently associated with the cure of chronic cough (Table 4). we also performed the same analysis procedure on cure+excellent vs fair+poor and cure vs fair+poor of chronic cough, and found that only present of typical symptoms was the independent predictor (OR = 4.114, 95%CI = 1.091–15.522, p = 0.037; OR = 5.857, 95%CI = 1.290–26.590, p = 0.022).
Table 3.
Univariate association with outcome
| Variable | Outcome | P value | |
|---|---|---|---|
| Cured | Not cured | ||
| Age | |||
| ≥ 60 | 25 (61%) | 16 (39%) | |
| < 60 | 22 (57.9%) | 16 (42.1%) | 0.78 |
| Sex | |||
| Male | 25 (58.1%) | 18 (41.9%) | |
| Femal | 22 (61.1%) | 14 (38.9%) | 0.789 |
| Hypertension | |||
| Yes | 11 (55%) | 9 (45%) | |
| No | 36 (61%) | 23 (39%) | 0.636 |
| Diabetes | |||
| Yes | 3 (100%) | 0 (0%) | |
| No | 44 (57.9%) | 32 (42.1%) | 0.391 |
| Coronary heart disease | |||
| Yes | 1 (33.3%) | 2 (66.7%) | |
| No | 46 (60.5%) | 30 (39.5%) | 0.733 |
| Heartburn | |||
| Yes | 38 (64.4%) | 21 (35.6%) | |
| No | 9 (45.0%) | 11 (55.0%) | 0.127 |
| Regurgitation | |||
| Yes | 40 (64.5%) | 22 (35.5%) | |
| No | 7 (41.2%) | 10 (58.8%) | 0.082 |
| Typical symptoms | |||
| Yes | 44 (64.7%) | 24 (35.3%) | |
| No | 3 (27.3%) | 8 (72.7%) | 0.044 |
| Asthma | |||
| Yes | 17 (73.9%) | 6 (26.1%) | |
| No | 30 (53.6%) | 26 (46.4%) | 0.094 |
| Hiatal hernia | |||
| Yes | 35 (60.3%) | 23 (39.7%) | |
| No | 12 (57.1%) | 9 (42.9%) | 0.798 |
| Esophagitis | |||
| Yes | 21 (56.8%) | 16 (43.2%) | |
| No | 26 (61.9%) | 16 (38.1%) | 0.642 |
| Barrett’s esophagus | |||
| Yes | 7 (77.8%) | 2 (22.2%) | |
| No | 40 (57.1%) | 30 (42.9%) | 0.409 |
| Reflux of bile | |||
| Yes | 6 (40%) | 9 (60%) | |
| No | 41 (64.1%) | 23 (35.9%) | 0.088 |
| DeMeester scores | |||
| ≥ 14.7 | 22 (55%) | 18 (45%) | |
| < 14.7 | 25 (64.1%) | 14 (35.9%) | 0.41 |
| Acid exposure time | |||
| ≥ 4.2% | 22 (56.4%) | 17 (43.6%) | |
| < 4.2% | 25 (62.5%) | 15 (37.5%) | 0.581 |
| Bolus exposure time | |||
| ≥ 1.4% | 29 (53.7%) | 25 (46.3%) | |
| < 1.4% | 18 (72%) | 7 (28%) | 0.123 |
| Number of Reflux episodes (impedance) | |||
| ≥ 73 | 18 (47.4%) | 20 (52.6%) | |
| < 73 | 29 (70.7%) | 12 (29.3%) | 0.035 |
| SI of chronic cough | |||
| > 50% | 17 (58.6%) | 12 (41.4%) | |
| ≤ 50% | 30 (60%) | 20 (40%) | 0.904 |
| SAP of chronic cough | |||
| > 95% | 22 (56.4%) | 17 (43.6%) | |
| ≤ 95% | 25 (62.5%) | 15 (37.5%) | 0.581 |
| Reflux-cough correlation | |||
| Positive | 26 (56.5%) | 20 (43.5%) | |
| Negative | 21 (63.6%) | 12 (36.4%) | 0.525 |
| Ineffective esophageal motility | |||
| Yes | 9 (40.9%) | 13 (59.1%) | |
| No | 36 (69.2%) | 16 (30.8%) | 0.023 |
Table 4.
Stepwise logistic regression resluts
| predictor | Adjusted odds ratio (95% confidence interval) |
P value |
|---|---|---|
| Typical symptoms | ||
| Yes | 6.435 (1.427–29.032) | 0.015 |
| No | – | – |
| Number of Reflux episodes (impedance) | ||
| ≥ 73 | 0.306 (0.107–0.874) | 0.027 |
| <73 | – | – |
Among the 79 patients, 19 patients didn’t have pathologic AET and positive reflux-cough association. Fourteen of which had their cough cured or significantly improved (Table 5).
Table 5.
Detailed information of 19 patients without pathologic AET and positive reflux-cough association
| Hiatal hernia | Typical symptoms | No. of reflux episodes ≥73 | DeMeester scores ≥14.7 | No response to PPI | Partial response to PPI | Complete response to PPI | No use of PPI | No. of patients | Cough cured or significantly improved |
|---|---|---|---|---|---|---|---|---|---|
| yes | yes | yes | 5 | 5 | |||||
| yes | yes | yes | 2 | 2 | |||||
| yes | yes | yes | 1 | 1 | |||||
| yes | yes | yes | 1 | 1 | |||||
| yes | yes | yes | yes | 1 | 0 | ||||
| yes | yes | yes | yes | 1 | 1 | ||||
| yes | yes | 1 | 0 | ||||||
| yes | yes | 1 | 0 | ||||||
| yes | yes | yes | 1 | 1 | |||||
| yes | yes | yes | 1 | 1 | |||||
| yes | yes | 1 | 1 | ||||||
| yes | yes | 2 | 0 | ||||||
| yes | yes | yes | yes | 1 | 0 |
Discussion
Seventy-nine patients with chronic cough under LF were included in our study, At a median follow-up time of 35 months after surgery, chronic cough, heartburn and regurgitation were cured or significantly improved in 57(72.2%), 52(88.1%) and 53(85.5%) patients. By using multivariate model, we found that present of typical symptoms (OR = 6.435) and number of Reflux episodes (impedance) ≥73 (OR = 0.306) but not AET and reflux-cough association were independently associated with the cure of chronic cough. GERD, Asthma, and Postnasal drip syndrome, alone or in combination, were responsible for 93.6% of the cases of chronic cough [21, 22]. The 2016 ACCP guidelines recommended a clinical profile to excluding other potential chronic cough causes, and the clinical profile was estimated to be 91% predicive that a patient’s cough would respond to anti-reflux treatment [23]. In our study, asthma and non-asthmatic eosinophilic bronchitis were not excluded, so the respond rate was lower (72.2%).
Francis [24] found that preoperative heartburn with or without regurgitation and esophageal acid exposure of greater than 12% at baseline were significant predictors of response of the primary extraesophageal reflux symptom to anti-reflux surgery. In our study, present of typical symptoms was consistently significantly associated with good outcome in three different multivariate analysis. Number of Reflux episodes (impedance) ≥ 73 was only significantly associated with the cure of chronic cough. Thus we believed that typical symptoms was the only predictor in our study. We utilized a favorable response (cure+excellent) to LF as the “gold standard” test for comparison with present of typical symptoms (consistency test) and found that the consistency was poor (κ value:0.219, p = 0.033), thus although typical symptoms can predict better outcome, its ability to diagnose GERD-related cough is poor.
The recent Lyon consensus on ambulatory reflux monitoring illustrated that SI and SAP have a predictive value for the effect of medical and surgical treatment of reflux disease, and this is independent of AET [2]. While data about predictive role of SI and SAP on outcome of LF for chronic cough is still limited and controversial. Marco [9] found that even single time of correlation between cough and reflux could improve cure rate of chronic cough, but the sample size was too small (8 patients in one group and 10 in the other). Michael [25] found that positive SAP independently predicted good outcome of chronic cough, but most patients were under PPI therapy and only pH mornitoring was used. In contrary, Francis [24] found that no difference in response to surgery based on SI/SAP parameters, but the sample size was small too (12 cough patients). Thus our study is basically the first one to investigate the role of reflux-cough correlation on outcome of chronic cough after anti-reflux surgery. We found that positive SI/SAP was not significantly associated with the cure rate of chronic cough. The following two studies may provide a perspective on the reason. Paterson and Murat [26] showed that using a diary or event marker for determination of cough is inadequate because patients underestimate the frequency of cough events or misreport their timing. Sifrim and Dupont [27] found that the number of cough bursts detected by manometry was significantly higher than by patients using the event marker, and the delay was 28 (7–80) seconds, most of all, they found that the delay could change cough-reflux pattern to reflux-cough pattern. Thus correctly calculation of SI/SAP was impossible, not to mention using them as predictive factor for better outcome of LF.
DeMeester scores and AET were also not significantly associated with good outcome of chronic cough. The reason may be that pathologic AET are not the only implication for considering LF. In our center, other evidence of GERD such as hiatal hernia, typical symptoms, No. of reflux episodes, DeMeester scores and PPI response are under consideration. Thus symptomatic outcome of patients without pathological AET may similar to those with pathological AET. As we can see that 14 of 19 patients without pathologic AET and positive reflux-cough association had their cough cured or significantly improved after LF.
There were several limitations in our study. First, as the dose of PPI, duration of PPI, and response of chronic cough to PPI was not standardized in our medical record, thus PPI response was not included. Since a positive response to initial empiric PPI therapy is the best indicator for eventual resolution of gastroesophageal reflux-related chronic cough [28, 29], thus the lack of this part may have an impact on the results. Further, this is a retrospective study and the symptomatic outcome were relied on telephone interview, the patients may misunderstood what we asked, as the cure of chronic cough was easy to judge, thus we adopted cure of chronic cough as the outcome metrics to minimize the impact.
Conclusion
The clinical profile to excluding other potential chronic cough causes is useful in selecting patients most like to benefit from LF, and present of typical symptoms but not postitive reflux-cough correlation predicts cure of chronic cough. Futher prospective study using manometry to detect cough is needed to illustrate the association between reflux-cough correlation and symptomatic outcome of chronic cough after LF.
Acknowledgments
Not applicable.
Abbreviations
- 24-h MII-pH monitoring
24-h multichannel intraluminal impedance pH monitoring
- ACEI
Angiotensin-converting-enzyme inhibitors
- AET
Acid exposure time
- BET
Bolus exposure time
- BMI
Body mass index
- GERD
Gastroesophageal reflux disease
- HRM
High resolution manometry
- LF
Laproscopic fundoplication
- PPI
Proton pump inhibitor
- SAP
Symptom association probability
- SI
Symptom index
Authors’ contributions
ZGW, DC, ZWH, and JMW designed the study. DC, YL, and FX collected the data. DC, ZWH, YL, and FX analysis and interpreted the data. ZGW, DC, ZWH drafted the manuscript. ZGW, DC, ZWH, JMW revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study protocol was approved by the Institutional Review Board of the General Hospital of the PLA Rocket Force (Beijing, China) (reference number: KY2018021), and together with the prospective part,were registrated in chinese clinical trail registry center. Oral informed consent was achieved from each patient through telephone interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dong Chen, Email: 739353406@qq.com.
Zhonggao Wang, Email: zgwang82@163.com.
Zhiwei Hu, Email: Higherrife@163.com.
Yan Liang, Email: 335231422@qq.com.
Fei Xiao, Email: 971335445@qq.com.
Jimin Wu, Email: drwujimin@qq.com.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Group GC The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1125–1140. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Roman S, Gyawali CP, Savarino E, Yadlapati R, Zerbib F, Wu J, et al. Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: update of the Porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil. 2017;29(10):1–15. doi: 10.1111/nmo.13067. [DOI] [PubMed] [Google Scholar]
- 3.Tolone S, Gualtieri G, Savarino E, Frazzoni M, Bortoli ND, Furnari M, et al. Pre-operative clinical and instrumental factors as antireflux surgery outcome predictors. World J Gastrointest Surg. 2016;8(11):719–728. doi: 10.4240/wjgs.v8.i11.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savarino E, Bredenoord AJ, Fox M, Pandolfino JE, Roman S, Gyawali CP. Expert consensus document: Advances in the physiological assessment and diagnosis of GERD. Nat Rev Gastroenterol Hepatol. 2017;14(11):665–76. doi: 10.1038/nrgastro.2017.130. [DOI] [PubMed] [Google Scholar]
- 5.Gyawali C. P., Roman S., Bredenoord A. J., Fox M., Keller J., Pandolfino J. E., Sifrim D., Tatum R., Yadlapati R., Savarino E. Classification of esophageal motor findings in gastro-esophageal reflux disease: Conclusions from an international consensus group. Neurogastroenterology & Motility. 2017;29(12):e13104. doi: 10.1111/nmo.13104. [DOI] [PubMed] [Google Scholar]
- 6.El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63(6):871–880. doi: 10.1136/gutjnl-2012-304269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kahrilas PJ, Howden CW, Hughes N, Molloy-Bland M. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest. 2013;143(3):605–612. doi: 10.1378/chest.12-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD. Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc. 2007;21(11):1978–1984. doi: 10.1007/s00464-007-9490-7. [DOI] [PubMed] [Google Scholar]
- 9.MG P, M A, A T, U D, CV F, B S, et al. Effect of laparoscopic fundoplication on gastroesophageal reflux disease-induced respiratory symptoms. J Gastrointest Surg. 2000;4(2):143–149. doi: 10.1016/S1091-255X(00)80050-5. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman JA, Houghland JE, Quiroga E, Cahill M, Pellegrini CA, Oelschlager BK. Long-term outcomes of laparoscopic antireflux surgery for gastroesophageal reflux disease (GERD)-related airway disorder. Surg Endosc Other Interv Tech. 2006;20(12):1824–1830. doi: 10.1007/s00464-005-0329-9. [DOI] [PubMed] [Google Scholar]
- 11.Granderath FA, Kamolz T, Schweiger UM, Pasiut M., Jr WH, Pointner R. quality of life and symptomatic outcome three to five years after laparoscopic Toupet fundoplication in gastroesophageal reflux disease patients with impaired esophageal motility. Am J Surg. 2002;183(2):110–116. doi: 10.1016/S0002-9610(01)00868-6. [DOI] [PubMed] [Google Scholar]
- 12.Dallemagne B, Weerts J, Markiewicz S, Dewandre JM, Wahlen C, Monami B, et al. Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc Other Interv Tech. 2006;20(1):159–165. doi: 10.1007/s00464-005-0174-x. [DOI] [PubMed] [Google Scholar]
- 13.Brillantino A, Schettino M, Torelli F, Marano L, Porfidia R, Reda G, et al. Laparoscopic Nissen-Rossetti fundoplication is a safe and effective treatment for both acid and bile gastroesophageal reflux in patients poorly responsive to proton pump inhibitor. Surg Innov. 2011;18(4):387. doi: 10.1177/1553350611409593. [DOI] [PubMed] [Google Scholar]
- 14.Iqbal M, Batch AJ, Spychal RT, Cooper BT. Outcome of surgical fundoplication for extraesophageal (atypical) manifestations of gastroesophageal reflux disease in adults: a systematic review. J Laparoendosc Adv Surg Tech A. 2008;18(6):789. doi: 10.1089/lap.2007.0165. [DOI] [PubMed] [Google Scholar]
- 15.Lugaresi M, Aramini B, Daddi N, Baldi F, Mattioli S. Effectiveness of Antireflux surgery for the cure of chronic cough associated with gastroesophageal reflux disease. World J Surg. 2015;39(1):208–215. doi: 10.1007/s00268-014-2769-7. [DOI] [PubMed] [Google Scholar]
- 16.Hirano I, Richter JE. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol. 2007;102(3):668–685. doi: 10.1111/j.1572-0241.2006.00936.x. [DOI] [PubMed] [Google Scholar]
- 17.Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):80s–94s. doi: 10.1378/chest.129.1_suppl.80S. [DOI] [PubMed] [Google Scholar]
- 18.Du X, Wang F, Hu Z, Wu J, Wang Z, Yan C, et al. The diagnostic value of pepsin detection in saliva for gastro-esophageal reflux disease: a preliminary study from China. BMC Gastroenterol. 2017;17(1):107. doi: 10.1186/s12876-017-0667-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiener GJ, Richter JE, Copper JB, Wu WC, Castell DO. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988;83(4):358–361. [PubMed] [Google Scholar]
- 20.Weusten BL, Roelofs JM, Akkermans LM, Van Berge-Henegouwen GP, Smout AJ. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology. 1994;107(6):1741–1745. doi: 10.1016/0016-5085(94)90815-X. [DOI] [PubMed] [Google Scholar]
- 21.Palombini B, Villanova CE, Gastal O, Alt D, Stolz D, Palombini C. A pathogenic triad in chronic cough: asthma, postnasal drip syndrome, and gastroesophageal reflux disease. Chest. 1999;116(2):279. doi: 10.1378/chest.116.2.279. [DOI] [PubMed] [Google Scholar]
- 22.Sidhwa F, Moore A, Alligood E, Fisichella PM. Diagnosis and treatment of the Extraesophageal manifestations of gastroesophageal reflux disease. Ann Surg. 2017;265(1):63. doi: 10.1097/SLA.0000000000001907. [DOI] [PubMed] [Google Scholar]
- 23.Kahrilas PJ, Altman KW, Chang AB, Field SK, Harding SM, Lane AP, et al. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest. 2016;150(6):1341. doi: 10.1016/j.chest.2016.08.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Francis DO, Goutte M, Slaughter JC, Garrett CG, Hagaman D, Holzman MD, et al. Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope. 2011;121(9):1902–1909. doi: 10.1002/lary.21897. [DOI] [PubMed] [Google Scholar]
- 25.Hersh MJ, Sayuk GS, Gyawali CP. Long-term therapeutic outcome of patients undergoing ambulatory pH monitoring for chronic unexplained cough. J Clin Gastroenterol. 2010;44(4):254–260. doi: 10.1097/MCG.0b013e3181b8e97b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paterson WG, Murat BW. Combined ambulatory esophageal manometry and dual-probe pH-metry in evaluation of patients with chronic unexplained cough. Dig Dis Sci. 1994;39(5):1117. doi: 10.1007/BF02087567. [DOI] [PubMed] [Google Scholar]
- 27.Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54(4):449–454. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naik RD, Vaezi MF. Extra-esophageal manifestations of GERD: who responds to GERD therapy? Curr Gastroenterol Rep. 2013;15(4):318. doi: 10.1007/s11894-013-0318-4. [DOI] [PubMed] [Google Scholar]
- 29.Baldi F, Cappiello R, Cavoli C, Ghersi S, Torresan F, Roda E. Proton pump inhibitor treatment of patients with gastroesophageal reflux-related chronic cough: a comparison between two different daily doses of lansoprazole. World J Gastroenterol. 2006;12(1):82. doi: 10.3748/wjg.v12.i1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


