To the Editor: In recent years, as marriage and childbearing have been delayed, the ages of primiparous women have, in general, increased. In addition, with changes in the dietary habits of pregnant women, the body mass index (BMI) during pregnancy, and birth weight of newborns have also increased. A retrospective multi-center study demonstrated the effects of obstetric characteristics (increased maternal age and the BMI) and clinical treatment (labor induction and painless delivery) on labor duration: cervical dilatation was slower than that described previously, especially during cervical dilatation of 4 to 6 cm. This new information on labor duration could provide new research directions pre-pregnancy. That is, whether the BMI can become an indicator of the optimization and management of labor duration. This research aimed to assess the effects of pre-pregnancy body mass index (BMI) and gestational weight gain (GWG) on primipara duration of labor.
This research undertook a retrospective assessment of 6786 pregnant women who had full-term, cephalic presentation, and single pregnancies delivered in Beijing Obstetrics and Gynecology Hospital from September 1st, 2014 to August 31st, 2015 to explore the association between pre-pregnancy BMI and gestational weight gain (GWG) with the duration of labor. Exclusion criteria were: age <18 years; multipara; complications during pregnancy (including diseases of the heart, brain, lungs, liver or kidneys); chronic hypertension during pregnancy; gestational diabetes mellitus; preeclampsia; uterine scarring; placenta previa; severe fetal malformations; stillbirth, among them, 6361 women had vaginal deliveries (93.32%) and 425 underwent cesarean section (CS; 6.68%).
The indices that we evaluated were pregnancy age, height, education level, pre-pregnancy weight, pregnancy weight, weight at birth, gravidity history, gestational age, complications during pregnancy, birth mode, duration of labor, and neonatal data (childbirth complications and newborn condition).
Based on the classification standardset by the World Health Organization (WHO), “low” and “normal” body weights were reflected by a BMI <18.5 kg/m2 and 18.5 kg/m2 ≤ BMI <24.9 kg/m2, respectively, whereas “overweight” and “obesity” were reflected by 25.0 kg/m2 ≤ BMI <29.9 kg/m2 and BMI ≥30.0 kg/m2, respectively. Besides, six groups were obtained according to GWG at the interval of 5.0 kg (<10.0 kg; 10.0–14.9 kg; 15.0–19.9 kg; 20.0–24.9 kg; 25.0–29.9 kg; and ≥30.0 kg).
According to the required variables, EpiData (Copenhagen, Denmark) was used to establish a database (including an EpiData quality-control file). Physicians or medical graduates with clinical experience in obstetrics within our hospital entered the data, after thorough training. Then, the obtained data were checked by readjustment of medical records for missing items, rechecking and correction of medical records for cases with logical errors, rechecking medical records for extreme values, and random selection of 10% of cases for a final check of data.
SPSS version 20 (IBM, Armonk, NY, USA) was used for statistical analyses. Continuous variables with a normal distribution are the mean ± standard deviation (SD), and assessed by one-way analysis of variance (ANOVA) with post-hoct-test. Continuous variables with a non-normal distribution were presented as the median and interquartile range and compared by the rank sum test. Count data were expressed as frequency and percentage, and compared by the Pearson χ2 test or Fisher exact test. Binary logistic regression was used to determine odds ratios (ORs), adjusted ORs, and 95% confidence intervals (95% CIs) for CS risk during delivery in women with different levels of pre-pregnancy BMI and GWG. Covariates in the regression equation were maternal age, education level, pre-pregnancy BMI, and GWG. A P < 0.05 was considered significant.
A total of 6786 women who attempted vaginal delivery were included in this study, of whom 6361 had successful vaginal delivery and 425 (6.26%) did not. At the first stage of labor, 400 women underwent CS (90 due to fetal distress) and 25 cases underwent CS at the second stage of labor (4 resulting from fetal distress). All 6361 cases were grouped according to pre-pregnancy BMI: BMI <18.5 kg/m2, 1139 cases (17.33%); 18.5 kg/m2 ≤ BMI <24.9 kg/m2, 4650 cases (73.11%); 25 kg/m2 ≤BMI <29.9 kg/m2, 2507 cases (8.47%); BMI ≥30 kg/m2, 265 (1.09%) cases [Table 1].
Table 1.
Demographics and gestational characteristics of all study cases (n = 6786).

In addition, the duration of labor in each stage increased gradually with the pre-pregnancy BMI, with significant differences in the first and total stages of labor (P = 0.02) being documented [Table 2]. Then, the result shows that in women with a pre-pregnancy BMI <18.5 kg/m2, there were no significant differences in the duration of labor in the first, second or total stages among groups with different GWG levels. For those with 18.5 kg/m2 ≤BMI <24.9 kg/m2, the duration of labor increased significantly in the first, second and total stages with GWG (P < 0.001, 0.015, and <0.001, respectively). For those with a BMI ≥ 25.0 kg/m2, there were no significant differences in the duration of labor in the first, second or total stages among groups with different GWG levels [Table 3]. Further, CS risk during labor was calculated according to the pre-pregnancy BMI and GWG during pregnancy. Multivariate logistic regression analysis showed that the higher the pre-pregnancy BMI and the higher the GWG, the higher the CS risk during labor [Tables 4 and 5].
Table 2.
Correlation between the pre-pregnancy BMI and duration of labor.

Table 3.
Correlation between gestational weight gain (GWG) and labor duration.

Table 4.
Correlation between the pre-pregnancy BMI and CS during labor.
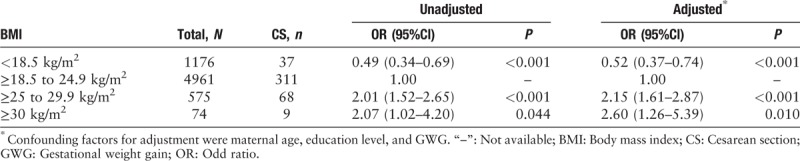
Table 5.
Correlation between GWG and CS during labor.

It is well known that the BMI is a good indicator for describing the degree of obesity and posture. Obesity and a sedentary lifestyle during pregnancy can reduce the contractility of abdominal muscles, resulting in suboptimal use of abdominal pressure during labor as well as lack of productive force, which can lead to prolonged labor.[1] Fat accumulation in pelvic and genital regions in obese pregnant women can increase resistance within the birth canal and affect fetal delivery directly. If macrosomia occurs in excessively obese pregnant women, the difficulty of vaginal delivery is increased further, and is an important reason for prolonged labor.
Ellekjaer et al[2] conducted a retrospective multiple linear regression analysis of 1885 cases. They found that the median active labor phase lasted 5.83 hour for women with a normal pre-pregnancy BMI, 6.08 hour for overweight women, and 5.90 hour for obese women, demonstrating that the pre-pregnancy BMI did not affect the active phase of labor significantly. However, in terms of CS implementation during the active period, there was a significant difference between pre-pregnant obese women and pre-pregnant women of normal weight. Maged and colleagues,[3] in a prospective study carried out in Egypt, discovered a different prevalence of cervical dilatation and duration of labor in pregnant women with different BMI values. Carlhalland co-workers demonstrated that, with a pre-pregnancy BMI >30 kg/m2, the probability of prolonged latency, active-phase stagnation, and prolonged active phase increased, whereas the duration of the second phase of labor was not significantly different from that of low and normal body weight group. These findings suggested that the impact of obesity was limited to the first stage of labor, and did not result in abnormal progression to the second stage. The authors mentioned above proposed that an increase in the BMI affects uterine contraction, and impacts the first stage of labor mainly. Carpenter JR agrees that the labor process is longer in obese women confined to the first stage of labor. In the context of the determination of the status of the fetus and the mother, the time for progress in the first stage of Labour should be allowed to increase.[4]
A study by Somprasit and colleagues[5] of Asian pregnant women found that individuals with a pre-pregnancy BMI ≥23 kg/m2 tended to have prolonged duration of the second phase of labor (relative risk = 1.41, 95%CI 1.04–1.90). Chin and colleagues showed that in women who had a vaginal delivery, obese individuals had a longer duration of the first phase of labor (597 vs. 566 min, P = 0.03), compared with those with a normal BMI, and that CS risk in obese women was significantly higher than in those with a normal BMI (OR = 2.4; 95%CI 1.9–3.1).
Based on the classification standard set by the WHO, this study revealed a significant difference in the duration of the first phase of labor (P = 0.002). Women with a pre-pregnancy BMI ≥30 kg/m2 showed the longest duration of the first stage of labor, with a median of 630 min. Meanwhile, no significant differences were found in the second stage of labor among groups (P = 0.179). Although the first stage of labor in overweight women lasted 40 minute less than in those with a normal BMI (440 vs. 480 minute), the difference was not significant. With the pre-pregnancy BMI, the duration of the first stage of labor, as well as the total duration of labor, increased gradually. Therefore, management of the pre-pregnancy BMI should be controlled over an appropriate range, especially for overweight and obese pregnant women. This strategy would reduce the impact on labor duration as well as CS prevalence.
In addition, accumulation of fatty tissue in the birth canal increases birth resistance and reduces muscle contraction in pregnant women, and can lead to cephalopelvic disproportion, abnormal labor, and obstruction of labor. Thus, the risk of assisted vaginal delivery and CS also increases. Robinson and colleagues revealed that GWG is not related to the duration of the second stage of labor, with values of 1.1 hour, 1.1 hour and 1.0 hour (P = 0.13), respectively, in women with a normal pre-pregnancy BMI, overweight women, and obese women; in addition, GWG did not increase CS risk. The recommended weight gain during pregnancy in China follows the Guideline for weight gain during pregnancy[6] from the US National Academy of Medicine. According to that publication, the growth range of pregnant women with low weight during pregnancy is 12.5 to 18 kg, mean body-weight gain during mid and late pregnancy is 0.51 kg/w (0.44–0.58 kg/w); the growth range of pregnant women of normal weight is 11.5 to 16 kg during pregnancy, and mean weight gain during mid and late pregnancy is 0.42 kg/w (0.35–0.50 kg/w); for overweight women, 7 to 11 kg is added during pregnancy, with a mean weight gain of 0.28 kg/w (0.23–0.33 kg/w) in mid and late pregnancy; for obese women, 5 to 9 kg is added during pregnancy, with a mean weight gain of 0.28 kg/w (0.17–0.27 kg/w) in mid and late pregnancy. We grouped women according to GWG at an interval of 5 kg. As shown above, in women with a pre-pregnancy BMI of 18.5 to 24.9 kg/m2, GWG was associated significantly with the duration of the first stage of labor (P < 0.001), and correlated positively and significantly with the duration of the second stage of labor (P = 0.015), suggesting that attention should also be paid to GWG in addition to the pre-pregnancy BMI. Even in women with a normal pre-pregnancy BMI, excessive weight gain during pregnancy could result in poor birth outcomes. Therefore, in women with pre-pregnancy obesity and excessive weight gain during pregnancy, contractions, duration of labor, and changes in the fetal heart rate should be monitored closely during delivery. It is particularly important to strengthen management of dietary nutrition during pregnancy and control GWG to a suitable range.
Moreover, pre-pregnancy overweight or obese women, and those with excessive GWG, are prone to complications such as hypertension and gestational diabetes mellitus (and even fetal distress and neonatal asphyxia), which would increase CS risk.[7] If they undergo vaginal delivery, prolonged labor may increase the risk of poor delivery outcomes (especially fetal distress) as well as the burden on women, resulting in excessive physical exertion, electrolyte imbalance, postnatal uterine contractions, postpartum hemorrhage, and puerperal infections. Young and co-workers demonstrated that excessive GWG doubles the prevalence of cephalopelvic disproportion in non-obese women, with a significant effect on CS prevalence. We showed that CS prevalence in primipara with a pre-pregnancy BMI >30 kg/m2 was 6-times that of counterparts with a BMI <20 kg/m2. Cedergren and colleagues reported a significant correlation between ineffective uterine contractility and the maternal BMI. Due to fetal distress, the risk of non-selective CS increases significantly with the maternal BMI, reaching fourfold in overweight women. Gunatilake and co-workers[8] found the BMI to be a predictor of conversion of failed vaginal delivery to CS, with a 3.5-fold increase if the BMI during pregnancy increased by 10 kg/m2. In the current study, pre-pregnancy overweight and obese women accounted for 7.97% (507/6361) and 1.02% (35/6361), respectively, and 8.99% altogether. After adjustment for confounding factors such as maternal age, education level, and GWG, CS prevalence in overweight women was 2.01-times higher than that of women with a normal BMI, whereas obese women showed a CS prevalence 2.69-times greater than that for women with a normal BMI pre-pregnancy. CS prevalence increased gradually with GWG; for GWG of 20 to 25 kg, CS prevalence during labor was increased twofold; GWG of 25 to 30 kg resulted in a 3.69-fold increase in CS prevalence, whereas there was no significant difference for women with GWG ≥30 kg.
In summary, the present study indicated that pre-pregnancy BMI and GWG affect labor duration and CS prevalence during delivery. Even in women with a normal BMI pre-pregnancy, the duration of labor was prolonged significantly with an increase in GWG >20 kg, with a notably increased CS prevalence. Therefore, to reduce CS prevalence and obtain better pregnancy outcomes, pre-pregnancy overweight and obese women should select optimal lifestyles for weight control as well as balanced nutritional diets for a reasonable weight increase during pregnancy. This approach would prevent overweight and obesity at delivery, and reduce CS prevalence, thereby resulting in good delivery outcomes.
Funding
This study was supported by a grant from the Capital Characteristics Project (Beijing Municipal Science and Technology Commission No.151100004015182).
Conflicts of interest
None.
Footnotes
How to cite this article: Zhou L, Yang HX, Zhao RF, Zhang WY. Association of pre-pregnancy body mass index and gestational weight gain with labor stage. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000093
References
- 1.WHO Obesity: Preventing, Managing the Global Epidemic. Report of a WHO consultation. WHO, Geneva; 2000: 1–253. [PubMed] [Google Scholar]
- 2.Ellekjaer KL, Bergholt T, Løkkegaard E. Maternal obesity and its effect on labor duration in nulliparous women: a retrospective observational cohort study. BMC Pregnancy Childbirth 2017; 17:222.doi: 10.1186/s12884-017-1413-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maged AM, Belal DS, Marie HM, Rasjwan H, Abdelaziz S, Gabr AA, et al. Prospective study of the effect of maternal body mass index on labor progress in nulliparous women in Egypt. Int J Gynaecol Obstet 2017; 139:329–335. doi: 10.1002/ijgo.12322. [DOI] [PubMed] [Google Scholar]
- 4.Carpenter JR. Intrapartum Management of the Obese Gravida. Clin Obstet Gynecol 2016; 59:172–179. doi: 10.1097/GRF.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 5.Somprasit C, Tanprasertkul C, Rattanasiri T, Saksiriwutth P, Wongkumn J, Kovavisarach E, et al. High pre-pregnancy body mass index and the risk of poor obstetrics outcomes among Asian women using BMI criteria for Asians by World Health Organization Western Pacific Region(WPRO): a large cohort study. J Med Assoc Thai 2015; 98 Suppl 2:S101–S107. [PubMed] [Google Scholar]
- 6.Institute of Medicine (US), National Research Council (US) Committee to reexamine IOM pregnancy weight guidelines, Rasmussen KM, Yaktine AL, editors Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US); 2009. doi: 10.17226/12584. [PubMed] [Google Scholar]
- 7.Harvey MW, Braun B, Ertel KA, Pekow PS, Markenson G, Chasan-Taber L. Prepregnancy Body Mass Index, gestational weight gain, and odds of cesarean delivery in Hispanic women. Obesity (Silver Spring) 2017; 26:185–192. doi: 10.1002/oby.22048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gunatilake RP, Smrtka MP, Harris B, Harris B, Kraus DM, Small MJ, et al. Predictors of failed trial of labor among women with an extremely obese body mass index. Am J Obstet Gynecol 2013; 209:1–5. doi: 10.1016/j.ajog.2013.07.023. [DOI] [PubMed] [Google Scholar]


