Abstract
Background:
The precise pathophysiology of venous erectile dysfunction (VED) was still unclear. Dynamic infusion cavernosometry and cavernosography (DICC) was the gold standard approach for the diagnoses of VED. However, a standard operative procedure of DICC was needed and it was unclear whether DICC could show promise in accurate assessment and treatment of VED. The aim of this study was to establish an optimized operation process of DICC and evaluate the efficacy of DICC in the diagnoses and therapy of VED.
Methods:
One hundred and forty-seven VED patients identified by the color doppler duplex ultrasonography (CDDU) were included. Then the method of DICC was adopted to assess the severity of VED and all patients were divided into 4 groups, including (1) non-VED; (2) mild VED; (3) moderate VED and (4) severe VED. All patients received the treatment of psychotherapy. Drug therapy, the intervention embolism of corpus cavernosum and the implantation of penile prosthesis were applied if psychotherapy was ineffective for patients. The international index of erectile function (IIEF-5) scores of patients were collected and compared before and after treatment.
Results:
IIEF-5 score of non-VED group after psychotherapy (19.35 ± 3.59) and drug therapy (23.31 ± 0.75) was higher than that before psychotherapy (15.30 ± 2.72, t = −4.31, P < 0.01) and drug therapy (16.62 ± 1.50, t = −19.13, P < 0.01). IIEF-5 scores of mild VED (18.25 ± 2.60) and moderate VED group (14.83 ± 4.17) after treatment was improved significantly by intervention embolism of corpus cavernosum when compared with those before treatment (mild: 15.50 ± 2.14, t = −2.31, P < 0.05; moderate: 11.83 ± 2.86, t = −1.45, P < 0.05). However, drug therapy and intervention embolism (IE) of corpus cavernosum showed poor effects on patients with moderate and severe VED patients (P > 0.05). IIEF-5 score of severe VED group was increased under the treatment of implantation of penile prosthesis (23.25 ± 0.71) compared with that before treatment (8.00 ± 0.39, t = −53.25, P < 0.05).
Conclusion:
DICC was a valid diagnostic tool that could identify patients with VED. And DICC had great effect on the diagnosis and individual therapy for patients with VED in varying degrees. Moreover, the manipulation of DICC needed uniform standards.
Keywords: Venous erectile dysfunction, Dynamic infusion cavernosometry and cavernosography, Diagnosis, Treatment
Introduction
Venous erectile dysfunction (VED) accounted for most of vasculogenic ED, including arterial insufficiency or venoocclusive dysfunction.[1] Treatment options for VED included first-line treatment (drug therapy, such as PDE-5 inhibitors), second-line treatment (intracavernous injection) and third line treatment (the implantation of penile prosthesis).[2–4] However, the limited effectiveness of oral administration of PDE-5 inhibitors for patients with VED had imperatively called for alternative treatments. Recently, other treatments had been described that include penis prosthesis implantation and negative pressure device for impotence.[5] To obtain the greatest therapeutic effect, VED patients with different severity might need different treatment.
The blood flow volume of penis could be assessed by the color doppler duplex ultrasonography (CDDU), which was considered as an accurate tool to evaluate venous leakage.[6–9] Nevertheless, CDDU actually had some limitations in the diagnostic evaluation of VED with a high percentage of false positive diagnoses of VED.[10] Dynamic infusion cavernosometry and cavernosography (DICC) provided an ideal approach to the diagnosis of VED.[11] Previous study showed that DICC had diagnostic values for VED and it could be used to classify patients with VED.[3]
A standard operative procedure of DICC had already been proposed by us. However, its application in the diagnosis and classification of VED was unclear. And its significance for individual treatment was also unclear. In our study, all patients with VED were divided into 4 groups (non-VED, mild VED, moderate VED, severe VED) by the method of DICC. Then, drug therapy, the intervention embolism (IE) of corpus cavernosum and the implantation of penile prosthesis were applied to improve erectile function of VED patients. The aim of this study was to investigate the efficiency of DICC for classifying venous erectile dysfunction and its significance for individual treatment.
Methods
Ethical approval
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital. And all participants provided written informed consent.
Subjects
From January, 2012 to January 2015, 147 erectile dysfunction (ED) patients aged between 19 and 48 years old were included in the study. All patients had persistent inability to achieve or maintain an erection sufficient for sexual intercourse. The courses of disease ranged from 6 months to 6 years. All patients were in a stable heterosexual relationship for at least 6 months. Then, a detailed medical history and relevant drug history, and basic laboratory tests were carried to exclude patients with serious physical disorders. Sexual functioning of patients were assessed by the international index of erectile function (IIEF). All patients enrolled in this study had abnormal morning and nocturnal penile erection rated by RigiScan test. CDDU was used to evaluate penile hemodynamics. For all patients, the peak systolic velocity (PSV) of corpus cavernosum of penis >25 cm/s and the end diastolic velocity (EDV) of corpus cavernosum >5.0 cm/s rated by CDDU.
Lastly, DICC was applied to assess the severity of patients with VED. Then patients were divided into 4 groups, including (1) non-VED; (2) mild VED; (3) moderate VED and (4) severe VED.
DICC
The DICC examination was carried out in the digital subtraction angiography (DSA) room of Nanjing Drum Tower Hospital. The patients were maintained at supine position during the test. Nerve block anesthesia was conducted in the base of penis with 10 mL 2% lidocaine. Then the base of penis was tied with a rubber band. Ten microgram (2 mL) of alprostadil was injected at 9 o’clock of the middle part of right corpus cavernosum with a skin test needle (not injure the corpus cavernosum). Then a skin test needle was punctured at 3 o’clock of the middle part of left corpus cavernosum and a pressotransducer (the maximum pressure: 300 mmHg; 1 mmHg = 0.133 kpa) was connected with the other end of the needle. A blood taking needle (21G) was punctured at 9 o’clock of the middle part of right corpus cavernosum and the other end of the needle was connected with an injection pump via an extension tube. It was important to note that the needle head should be fixed on the penis well.
The first stage of DICC
Firstly, intracavernous pressure (ICP) under the softening condition of penis was measured. Under a softening condition, 60 mL normal saline +20 mL ioversol were injected via an injection pump with a speed of 0.4 mL/s. The erection of penis was observed under this process. And the normotopia, left and right oblique views were taken for later comparison.
The second stage of DICC
Two hundred mL ioversol and normal saline with a ratio of 1:4 was injected into corpus cavernosum of patients at different speeds of 2.5, 3.5, 4.5, and 4.9 mL/s. The infusion was stopped when the patient complained about penis distending pain with an IV degree and with ICP of 150 mmHg. The speed was reduced to 2.0, 1.5, 1.0, 0.5, 0.3, and 0.1 mL/s respectively to maintain infusion (in order to keep a good condition of the erected penis, ICP was controlled within 150 ± 20 mmHg). The speed of infusion was recorded as flow to maintain (FTM).[3] If ICP decreased gradually, ICP decay (pressure decay, PD) within 30 second since the stop of infusion was being recorded.[4] In addition, digital images of the normotopia, left and right oblique views at each speed were taken. The patient could be diagnosed with vein leakage if the reflux vein development of cavernous veins was found.
Therapy
All patients received psychological therapy. The patient would receive drug therapy if the psychological therapy was ineffective. Moreover, the patient would receive interventional embolism therapy or prosthesis implantation therapy if the drug therapy was ineffective.
Psychological therapy
All patients received psychological counseling, which helped them establish the confidence of treatment.
Drug therapy
Ten to twenty milligram of Tadalafil (Cialis) was orally administrated every other day for 3 to 4 weeks.
Intervention embolism
Intervention embolism was performed in the DSA room of our hospital. The 4F cobra catheter was embedded in the internal iliac vein by puncturing 4F vagina vasorum into the femoral vein of the patient. And then a micro-catheter was punctured into the junction of deep dorsal veins of penis and prostatic venous plexus. The location of micro-catheter was identified by cavernosography. According to the return blood flow velocities and flows, 4 to 10 mL mixture (20%–25% of glubran–2 glue) were prepared with glubran-2 glue and ultra liquid iodized oil in accordance with ratios between 1:3 and 1:4. To embolize, the glue was slowly injected through the micro-catheter under fluoroscopy, which was washed by the 5% glucose injection. Adequate diffusion and solidification of the prostatic venous plexus and related collateral reflux veins were conducted. During glue injection, diffusion and reflux distances of glue should be controlled strictly. We stopped the injection until the embolism was quickly inserted into the internal iliac vein, and quickly pulled out the microcatheter. Finally, effects of embolization were evaluated by cavernosonography.
Penile prosthesis implantation
Longitudinal incision of the scrotum in the middle of the base of the penis was conducted. The penis membrane of the base of the penis was exposed. A hagar expander was inserted into the cavernous. A tunnel was formed from the incision of albuginea penis to the glans. Then the length of the tunnel was measured and a penile prosthesis whose length matched with the tunnel was chosen. The penile prosthesis was inserted into the tunnel and reached the end of corpus cavernosum. After confirming that there was no mechanical failure, skin was sutured layer by layer.
Statistical analysis
The follow-up period was 3 to 12 months. The definition of effective treatment was: (1) intervention treatment was successful if the embolism was in the target vessel; (2) the implanted prosthesis worked well; (3) IIEF-5 scores of patients were collected before and after treatment. Statistical analyses were performed using the SPSS 20 software (SPSS Inc., USA). A t test was performed to evaluate differences of IIEF-5 scores before and after treatment. The difference was statistically significant if P < 0.05.
Results
Different groups according to DICC
Among 147 patients receiving DICC examination, 23 patients had non-VED and the other 124 patients were divided into different groups according to FTM and ICP [Table 1 and Figure 1].
Table 1.
Different groups of patients divided by DICC.
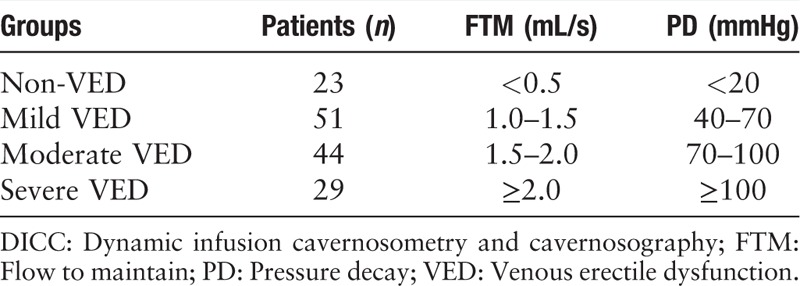
Figure 1.
Patients divided by DICC. (A) No venous ED on cavernosography: ICP = 165 mmHg; flow-to-maintain = 0.1 mL/s; PD = 0 mmHg. (B) Mild venous ED on cavernosography: ICP = 141 mmHg; flow-to-maintain = 1.0 mL/s; PD = 44 mmHg. (C) Moderate venous ED on cavernosography: ICP = 139 mmHg; flow-to-maintain = 1.5 mL/s; PD = 72 mmHg. (D) Severe venous ED on cavernosography: ICP = 90 mmHg; flow-to-maintain = 2.0 mL/s; PD = 118 mmHg. DICC: Dynamic infusion cavernosometry and cavernosography; ED: Erectile dysfunction; ICP: Intracavernous pressure; PD: Pressure decay.
Twenty-three patients with non-VED showed FTM < 0.5 mL/s or PD < 20 mmHg. No venous return shadow was observed on digital images of all patients. Their FTMs were low, ranging from 0.1 to 0.3 mL/s. The erection was normal with PD more than 150 mmHg during maintenance of erection. Fifty-one patients with mild VED showed 1.0 mL/s ≤ FTM < 1.5 mL/s or 40 mmHg ≤ PD < 70 mmHg. Forty-four patients with moderate VED showed 1.5 mL/s ≤ FTM < 2.0 mL/s or 70 mmHg ≤ PD < 100 mmHg. Twenty-nine patients with severe VED showed FTM ≥ 2.0 mL/s or PD ≥ 100 mmHg.
Technique success
All embolisms of 19 patients (9 mild, 6 moderate, and 5 severe patients) receiving therapy of corpus cavernosum vein intervention embolism showed that the embolism was in the target vessel. The prosthesis of 1 patient was taken out due to infection, all other 12 patients showed successful prosthesis implantation.
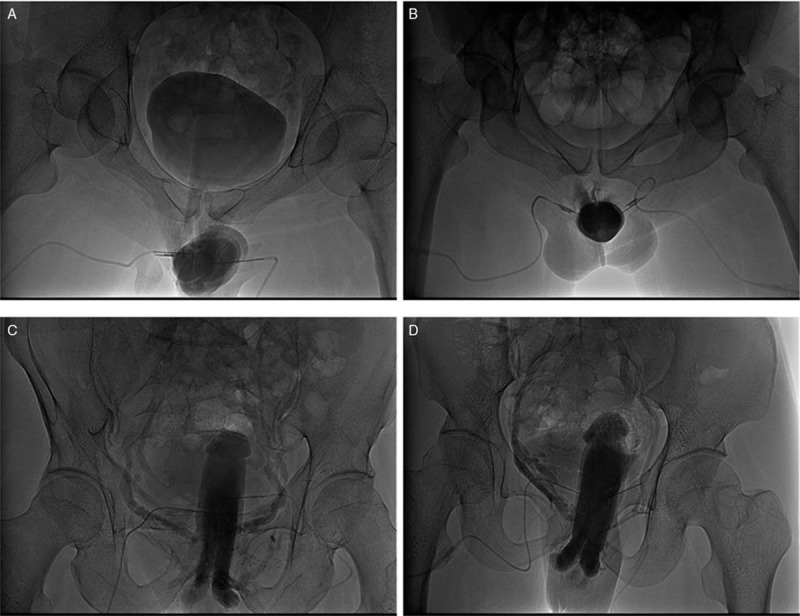
IIEF of all patients before and after treatment
For non-VED group, the psychotherapy and drug therapy could obtain satisfying effects, which was also consistent with the results of DICC. In the mild group, some patients showed good effects after taking drugs orally [Table 2].
Table 2.
IIEF scores among patients before and after the psychotherapy and drug therapy.
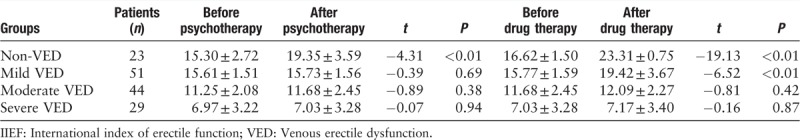
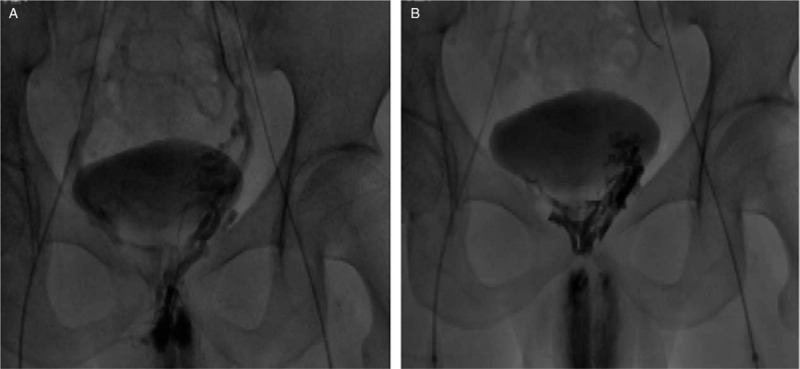
In the moderate and severe groups, the drug therapy showed no effect for patients [Table 2]. Then they received the intervention embolism therapy or prosthesis implantation. The cavernosonography for patients who had an intervention embolism therapy showed that all operations were successful with exact cavernosum reflux vein embolism [Figure 2]. The intervention embolism therapy showed good effects for patients with mild VED (P < 0.05) and had poor effects on patients with moderate and severe VED [Table 3].
Figure 2.
Intervention embolism was successful with embolism in the target vessel. (A) Cavernosonography before intervention embolism showed internal pudendal veins of both sides; (B) Cavernosonography after intervention embolism showed exact embolism and non-development of internal pudendal veins of both sides.
Table 3.
IIEF scores of mild, moderate, and severe groups before and after intervention embolism.
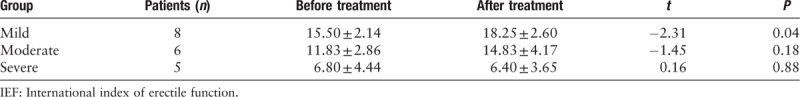
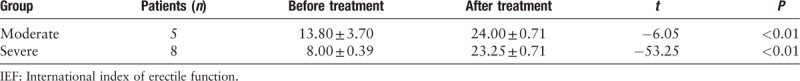
For patients with mild VED, drug therapy could be added if they had an intervention embolism therapy with poor effects. Among patients with moderate VED, the intervention embolism therapy showed poor effects and there was no obvious improvement after a drug therapy. However, the intervention embolism therapy basically had no effect on patients with severe VED. In addition, prosthesis implantation was effective for patients with moderated and severe VED [Table 4].
Table 4.
IIEF scores moderate and severe groups before and after prosthesis implantation.
Discussion
This study divided VED patients into different groups by the results of DICC, including mild, moderate and severe groups. Oral administration of PDE-5 inhibitors was effective for most patients, however, it had poor effects on moderate and severe patients. An intervention embolism therapy or prosthesis implantation was conducted on moderate and severe patients. Severe patients could not get adequate erection even if the maximal infusion velocity was 4.9 mL/s. And obvious cavernous venous reflux was found in the digital images of these patients. Though sufficient artery blood supply (injection pumping) was found in these patients, the venous return still existed. Therefore, VED were not related to the insufficient blood supply of artery but related to other factors (such as the dysfunction of cavernosum smooth muscle cell and the dysfunction of albuginea penis).
Now therapeutic methods of VED mainly included oral administration of PDE-5 inhibitors, contraction of corpus cavernosum and albuginea,[12] ligation/decollement/insertion of corpus cavernosum veins and prosthesis implantation.[13–15] The oral drug therapy had certain effects for mild VED, however, it had poor effects on moderate and severe VED. The prosthesis implantation had good effects for moderate and severe VED.
However, this surgery was not accepted by some patients for high costs. The prosthetic device should be taken out if infection could occur. The surgical therapy of VED was the ligation of deep dorsal veins of penis by increasing obstruction of blood return.[16] Previous study showed that sildenafil might improve the erection of VED patients after surgery. Shafik reported that a new therapy of vein leakage, which improved the vein closing mechanism by overlapping of albuginea.[17] After 6 months, the erection of 8 patients after operation was improved significantly. In the tissue biopsy of albuginea under microscope, collagen fiber atrophy was observed.[17] Zhang et al[18] reported that the surgery of embedding deep dorsal vein of penis had achieved good effects for treatment of vein leakage ED, and 14 out of 17 patients obtained satisfying effects. Popken G reported that 122 patients who had received ligation of deep dorsal vein of penis with a total effective rate of 33%.[19]
In 2000, Peskircioglu et al[20] firstly attempted to apply embolism of deep dorsal veins of penis with 5 mL tissue glue, N-butyl - cyanoacrylate and iodine oil mixture for the treatment of VED. Nakata et al[21] used embolism of deep dorsal veins of penis with 50% ethyl alcohol to treat 23 patients with VED with 20 effective cases (87%) and 18 effective cases (78%) after 6 months. According to previous results, we chose the interventional operation, namely embolization of the corpus cavernosum vein system via femoral veins, and the embolism point was located in the junction of proximal deep dorsal veins of penis, prostatic venous plexus and internal pudendal veins.[22] The injection of liquid embolic agent in the junction could be rapidly diffused to peripheral veins. An effect of embolism could be built within veins and spread to the most part of reflux vessels of corpus cavernosum veins. According to imaging, its blocking effect on venous return was better than that of pure blockage of deep dorsal veins of penis and penile crural veins. In addition, this operation was an invasive surgery, which could be operated under local anesthesia.
Our results suggested that this operation was proper for patients with mild and moderate VED diagnosed by DICC. Long-term oral administration of Cialis could be utilized for patients with poor postoperative effects. However, it was not suitable for patients with severe VED, which might be related to severe damage of vascular endothelial cells, failure of embolic agents or possible insufficiency of albuginea. However, it is still an enormous challenge about the ectopic veins and the right route to the ectopic veins during interventional embolization.
Conclusion
Our results showed that DICC was a valid diagnostic tool, which could identify patients with VED. Patients with VED could be divided into 4 groups by DICC, including non-VED, mild VED, moderate VED and severe VED. This found has great effect on the individual therapy for patients with VED. However, more studies about the operating procedure and the significance of DICC for the diagnosis of patients with VED are needed.
Funding
The work was supported by the grants from the National Natural Science Foundation of China (No. 81701433), the Project of Nanjing Municipal Bureau of Health (No. YKK17098), the Fundamental Research Funds for the Central Universities (No. 021414380134).
Conflicts of interest
None.
Footnotes
How to cite this article: Gao QQ, Chen JH, Chen Y, Song T, Dai YT. Dynamic infusion cavernosometry and cavernosography for classifying venous erectile dysfunction and its significance for individual treatment. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000099
Qing-Qiang Gao and Jian-Huai Chen contributed equally to this work.
References
- 1.Vlachopoulos C, Rokkas K, Ioakeimidis N, Aggeli C, Michaelides A, Roussakis G, et al. Prevalence of asymptomatic coronary artery disease in men with vasculogenic erectile dysfunction: a prospective angiographic study. Eur Urol 2005; 48:996–1003. doi: 10.1016/j.eururo.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Hellstrom WJG, Montague DK, Moncada I, Carson C, Minhas S, Faria G, et al. Implants, mechanical devices, and vascular surgery for erectile dysfunction. J Sex Med 2010; 7:501–523. doi: 10.1111/j.1743-6109.2009.01626.x. [DOI] [PubMed] [Google Scholar]
- 3.Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol 2010; 57:804–814. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 4.Aschenbach R, Steiner T, Kerl MJ, Zangos S, Basche S, Vogl TJ. Endovascular embolisation therapy in men with erectile impotence due to veno-occlusive dysfunction. Eur J of Radiol 2013; 82:504–507. doi: 10.1016/j.ejrad.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 5.Song WD, Yuan YM, Cui WS, Wu AK, Zhu YC, Liu J, et al. Penile prosthesis implantation in Chinese patients with severe erectile dysfunction: 10-year experience. Asian J Androl 2013; 15:658–661. doi: 10.1038/aja.2013.78. DOI: 10.1038/aja.2013.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shafik A, Shafik I, El Sibai O, Shafik AA. On the pathogenesis of penile venous leakage: role of the tunica albuginea. BMC Urol 2007; 7:14.doi: 10.1186/1471-2490-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferrini MG, Kovanecz I, Sanchez S, Umeh C, Rajfer J, Gonzalez-Cadavid NF. Fibrosis and loss of smooth muscle in the corpora cavernosa precede corporal veno-occlusive dysfunction (CVOD) induced by experimental cavernosal nerve damage in the rat. J Sex Med 2009; 6:415–428. doi: 10.1111/j.1743-6109.2008.01105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavallini G, Maretti C. Unreliability of the duplex scan in diagnosing corporeal venous occlusive disease in young healthy men with erectile deficiency. Urology 2018; 113:91–98. doi: 10.1016/j.urology.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Sikka SC, Hellstrom WJG, Brock G, Morales AM. Standardization of vascular assessment of erectile dysfunction: standard operating procedures for duplex ultrasound. J Sex Med 2013; 10:120–129. doi: 10.1111/j.1743-6109.2012.02825.x. [DOI] [PubMed] [Google Scholar]
- 10.Caretta N, De Rocco Ponce M, Minicuci N, Palego P, Valente U, Garolla A, et al. Penile doppler ultrasound predicts cardiovascular events in men with erectile dysfunction. Andrology 2018; doi: 10.1111/andr.125/61. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Wespes E, Amar E, Hatzichristou D, Hatzimouratidis K, Montorsi F, Pryor J, et al. EAU Guidelines on erectile dysfunction: an update. Eur Urol 2006; 49:806–815. doi: 10.1016/j.eururo.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 12.el-Sibai O, Shafik AA, Shafik IA. Tunica albuginea reefing: a novel technique for the treatment of erectile dysfunction. J Invest Surg 2011; 24:44–48. doi: 10.3109/08941939.2010.526682. [DOI] [PubMed] [Google Scholar]
- 13.Hsu GL, Chen HS, Hsieh CH, Lee WY, Chen KL, Chang CH. Salvaging penile venous stripping surgery. J Androl 2010; 31:250–260. doi: 10.2164/jandrol.109.008409. [DOI] [PubMed] [Google Scholar]
- 14.Hsu GL, Chen HS, Hsieh CH, Ling PL, Wen HS, Liu LJ, et al. Insufficient response to venous stripping surgery: is the penile vein recurrent or residual? J Androl 2006; 27:700–706. doi: 10.2164/jandrol.106.000737. [DOI] [PubMed] [Google Scholar]
- 15.Hsu GL, Chen HS, Hsieh CH, Lee WY, Chen KL, Chang CH. Clinical experience of a refined penile venous stripping surgery procedure for patients with erectile dysfunction: is it a viable option? J Androl 2010; 31:271–280. doi: 10.2164/jandrol.109.008532. [DOI] [PubMed] [Google Scholar]
- 16.Wen HS, Hsieh CH, Hsu GL, Kao YC, Ling PY, Huang HM, et al. The synergism of penile venous surgery and oral sildenafil in treating patients with erectile dysfunction. Int J Androl 2005; 28:297–303. doi: 10.1111/j.1365-2605.2005.00554.x. [DOI] [PubMed] [Google Scholar]
- 17.Shafik A, Shafik I, Sibai OE, Shafik AA. Tunica albuginea overlapping: a novel technique for the treatment of erectile dysfunction. Andrologia 2005; 37:180–184. doi: 10.1111/j.1439-0272.2005.00678.x. [DOI] [PubMed] [Google Scholar]
- 18.Zhang B, Chen J, Xiao H, Zhang Y, Cai L, Tao X, et al. Treatment of penile deep dorsal venous leakage of erectile dysfunction by embedding the deep dorsal vein of the penis: a single center experience with 17 patients. J Sex Med 2009; 6:1467–1473. doi: 10.1111/j.1743-6109.2008.01080.x. [DOI] [PubMed] [Google Scholar]
- 19.Popken G, Katzenwadel A, Wetterauer U. Long-term results of dorsal penile vein ligation for symptomatic treatment of erectile dysfunction. Andrologia 1999; 31:77–82. [DOI] [PubMed] [Google Scholar]
- 20.Peşkircioğlu L, Tekin I, Boyvat F, Karabulut A, Ozkardeş H. Embolization of the deep dorsal vein for the treatment of erectile impotence due to veno-occlusive dysfunction. J Urol 2000; 163:472–475. [DOI] [PubMed] [Google Scholar]
- 21.Nakata M, Takashima S, Kaminou T, Koda Y, Morimoto A, Hamuro M, et al. Embolotherapy for venous impotence: use of ethanol. J Vasc Interv Radiol 2000; 11:1053–1057. [DOI] [PubMed] [Google Scholar]
- 22.Rebonato A, Auci A, Sanguinetti F, Maiettini D, Rossi M, Brunese L, et al. Embolization of the periprostatic venous plexus for erectile dysfunction resulting from venous leakage. J Vasc Interv Radiol 2014; 25:866–872. doi: 10.1016/j.jvir.2014.01.015. [DOI] [PubMed] [Google Scholar]


