Abstract
Background:
Alcohol consumption has been observed to be a contributing factor in liver damage. However, very few studies have tried to decipher the correlation between patients with liver disease and alcohol consumption. Therefore, this study was planned to determine the prevalence of alcohol consumption among patients with liver disease, and to evaluate the risk factors, liver diseases, and chronic medical conditions associated with alcohol drinking.
Methods:
A cross-sectional study was conducted among patients with liver disease in 30 provinces, autonomous regions, and municipalities across China. All participants answered the questionnaire, which led to the calculation of Alcohol Use Disorders Inventory Test (AUDIT) score for each patient. Based on this score, low-risk drinkers, hazardous drinkers, and harmful drinkers were defined as having AUDIT score of <8, between 8 and 15, and ≥16, respectively.
Results:
A total of 1489 participants completed the questionnaire. Based on this information, 900 (60.44%) participants were classified as alcohol drinkers. Among these, 8.66% were ex-drinkers, 22.10% were low-risk drinkers, 17.13% were hazardous drinkers, and 12.56% were harmful drinkers. Further investigation of the association between alcohol consumption and other baseline characteristics of patients with liver disease revealed that usually men <40 years old, participants having higher family annual income, having college degree or higher education, living alone, having higher body mass index (BMI), current smokers, and ex-smokers had significant association with higher risk of alcohol consumption. In addition, among the 18.07% of the participants with cirrhosis, it was observed that risk of cirrhosis increased with higher alcohol consumption. Furthermore, harmful drinkers showed greater odds of hypertension and heart diseases, while hazardous drinkers and harmful drinkers, both had greater odds of hyperlipidemia.
Conclusions:
Overall our analyses indicated that among the patients with liver disease in China, there was high rate of alcohol consumption and dependence. Alcohol consumption usually associated with men <40 years old, higher family income, education level, living alone, high BMI, and smoking. Increased alcohol consumption not only increased the risk of cirrhosis, but also enhanced the risk of hypertension, heart diseases, and hyperlipidemia.
Keywords: Alcohol consumption, Patients with liver disease, Alcohol dependence, AUDIT, Chronic medical conditions
Introduction
According to the 2014 World Health Organization (WHO) report on alcohol and health, alcohol consumption has been estimated to result not only in 139 million disability-adjusted life years, but also contributes to 5.1% of the global burden of disease and injury.[1] Typically, alcohol drinking is normal part of daily diet, especially in rural areas of China. It is also commonly consumed during important festivals, business occasions, rituals, and special events. In this context, Chinese Health and Nutrition Survey indicated that alcohol consumption rate in the past year was around 34% in China.[2]
The hepatitis virus infection disease burden is also high in China, and usually results in liver disease. Especially patients where liver disease stems from hepatitis B virus (HBV) or hepatitis C virus (HCV) infection, the alcohol consumption has been observed to further contribute to liver damage.[3,4] In addition, alcohol intake has also been observed to independently increase the risk of cirrhosis and hepatocellular carcinoma (HCC) in patients with HBV or HCV infection.[5] Multiple studies have indicated about the interactive correlation of heavy alcohol consumption and HBV or HCV infection, with risk of cirrhosis.[6] Some earlier studies have even shown synergistic effect of alcohol drinking and HBV/HCV infection,[7,8] as a mechanism of action for HCC development.[8] Therefore, in light of high disease burden of hepatitis virus (HBV and HCV) infection, the efforts to combat liver disease development, must not only focus on primary prevention of hepatitis virus infection, but also on the other risk factors, including alcohol consumption especially in patients with hepatitis virus infection.
In parallel, alcohol consumption has also been shown to correlate with increased morbidity and mortality in certain chronic diseases.[9–11] In this regard, a recent meta-analysis study showed 2-fold increase in cardiovascular disease and cancer mortality rate, while 15-fold increase in liver cirrhosis mortality rate in individuals with alcohol use disorder (AUD), in comparison to general population.[12] Moreover, another study reported that despite drinking patterns, the all-cause mortality rate at 7-year follow-up was significantly higher in those individuals who met alcohol dependence criteria in the past year, relative to the general population.[13]
An interesting study from United Kingdom revealed that general practitioners only discussed alcohol use in less than one-third of the cases that were subsequently admitted to hospital due to alcohol-related liver disease (ALD).[14] This observation highlights an important fact that despite patients developing ALD in the community, they are not identified until they are admitted to the hospital with end stage of liver disease, and by this time, it is too late for many of them to get treatment. Similarly, the data from numerous randomized controlled trials concluded that if high-risk drinking behavior is identified early in the community or at outpatient service of hospital, then brief advice or intervention can prove to be cost-effective way to reduce drinking.[15,16] Thus, early identification of alcohol consumption behavior should be encouraged.
Importantly, little information about alcohol consumption prevalence among Chinese patients with liver disease is available. There is also a poor understanding about the effect of alcohol consumption on liver injury and chronic medical conditions among patients with liver disease in China. Therefore, in this study, we have investigated the prevalence of alcohol drinking among patients with liver disease, and identify the association of alcohol consumption with liver disease and various chronic medical conditions in China.
Methods
Ethics approval
The process of completing questionnaires, collecting and reviewing patients’ data was approved by the Institutional Review Board (IRB) of Peking University People's Hospital (IRB reference number 2018PHB038-01). All the participants provided written informed consent.
Study design
A cross-sectional study was conducted to evaluate the alcohol drinking behavior of patients with liver disease, who visited hepatology or gastroenterology outpatient department at Chinese hospitals, between March 1, 2018 and May 31, 2018. This population-based study was simultaneously conducted in 30 provinces, autonomous regions, and municipalities in China. Provincial categories included “Northern China” (Beijing, Tianjin, Hebei, Heilongjiang, Jilin, Liaoning, and Inner Mongolia), “Southern China” (Guangdong, Guangxi, Fujian, Yunnan and Hainan), “Western China” (Sichuan, Xinjiang, Chongqing, Shanxi, Shaanxi, Gansu, Ningxia, Qinghai and Guizhou), “Eastern China” (Shanghai, Shandong, Jiangxi, Jiangsu and Zhejiang), and “Central China” (Henan, Hunan, Hubei and Anhui).
The patients were excluded from the study, if they showed hepatic encephalopathy, were inebriated at the time of the interview, or had any other condition that prohibited them to properly answer the questionnaire. All the participants were interviewed face-to-face by trained investigators on the day of their regular medical appointment. All patients were explained about the goals of the study before asking them to sign the consent forms. Subsequently, these patients answered the standard general questionnaire.
Questionnaire design
Social demographics and lifestyle factors
The questionnaire included social demographic variables (age, gender, nationality, height, weight, occupation, education, family annual income, marital and living status, and area of residence) and lifestyle variables (smoking). Based on the information provided by the participants, we calculated body mass index (BMI), using height and weight (weight [kg]/height [m]2). Overweight has been defined as BMI ≥ 25 kg/m2 for Asian countries.[17] In addition, smoking cessation was defined as no smoking in 3 months prior to interview.
Liver diseases
The questionnaire asked participants if they have any of the following liver diseases, diagnosed by a competent doctor; Chronic hepatitis B (no treatment or under treatment), Chronic hepatitis C (no treatment or under treatment or cured), alcoholic liver disease, non-alcoholic fatty liver disease, drug-induced liver disease, autoimmune liver disease (ie, autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis), acute hepatitis A, acute hepatitis E, agnogenic abnormal liver function, liver cirrhosis, and HCC.
Chronic medical conditions
In addition questionnaire also required information from participants about the following 8 chronic medical conditions that had been confirmed by a competent doctor, hypertension, heart disease (myocardial infarction, angina pectoris, tachycardia, and other forms), diabetes mellitus, hyperlipidemia (ie, elevated of cholesterol or triglycerides or low density lipoproteins), hyperuricemia, gout, cerebrovascular disease (ie, cerebral infarction, cerebral hemorrhage), stomach illness (ie, gastritis, duodenal, or stomach ulcer), and renal failure.
Alcohol consumption
Finally, the participants were also asked about their alcohol consumption habits. The participants reporting consumption of any alcoholic drink in the past 12 months prior to interview were classified as alcohol drinkers, while those who have no alcohol consumption at least during the same period, but had prior history were categorized as ex-drinkers. In total, our questionnaire contained eighteen different questions about alcohol consumption. Among these, questions 1 to 10 were cited from Alcohol Use Disorders Inventory Test (AUDIT), and the answers to these questions led to the calculation of AUDIT score for each patient. The questions 1 to 3 were about exploring alcohol consumption, while questions 4 to 6 were related to alcohol dependence, and questions 7 to 10 assessed alcohol-related problems. In addition, there were 2 cut-off points, 1 for dependence (AUDIT score ≥ 16) and 1 for risky drinking (AUDIT score: 8–15).[18] In our study, low-risk drinkers were defined as those having AUDIT score of <8, while hazardous drinkers were defined as those with AUDIT score between 8 and 15. However, those with AUDIT score of ≥16 were classified as harmful drinkers.
The remaining other 8 questions were “How long have you been drinking?,” “What kind of alcohol did you usually have in recent one year,” “What is the reason you have a drink in most cases,” “Over the past year, the proportion of you involuntary having a drink (ie, business entertainment),” “Have you sought professional help or been hospitalized because of adverse effects after drinking,” “Did you try to cease drinking,” “To cease drinking successfully, do you want to go to the professional clinic of abstinence,” and “Do you know that alcohol consumption is harmful to humans.”
Data collection
To collect the complete information, each patient was interviewed during his/her regular medical appointment in an outpatient department of a hospital. All patients completed the questionnaires with the assistance of an interviewer. The information about patient's baseline characteristics (age, gender, nationality, height, weight, occupation, education, family annual income, marital and living status, and area of residence), smoking history, diagnosis of liver disease and other chronic medical conditions and alcohol consumption were collected. All the patients provided complete information, and there was no missing response. The baseline data were analyzed for information about frequency and quantity of alcohol consumption and its wide-ranging associations with sociodemographic status, liver diseases, and chronic medical conditions.
Statistical analysis
The proportions of baseline characteristics among never drinkers and drinkers were compared using Chi-squared test. Multiple logistic regression analyses were performed to estimate the odds ratios (ORs) with 95% confidence intervals (CIs), to assess association of sociodemographic and lifestyle factors, with alcohol consumption. Similar analyses were performed to assess association of liver disease and chronic medical condition among drinkers and non-drinkers. All tests were 2-sided and P-value of <0.05 represented statistical significance. All analyses were conducted using Statistical Analysis System (SAS) version 9.4 (SAS Institute, Inc., Cary, NC, USA) software.
Results
Baseline characteristics of patients with liver disease
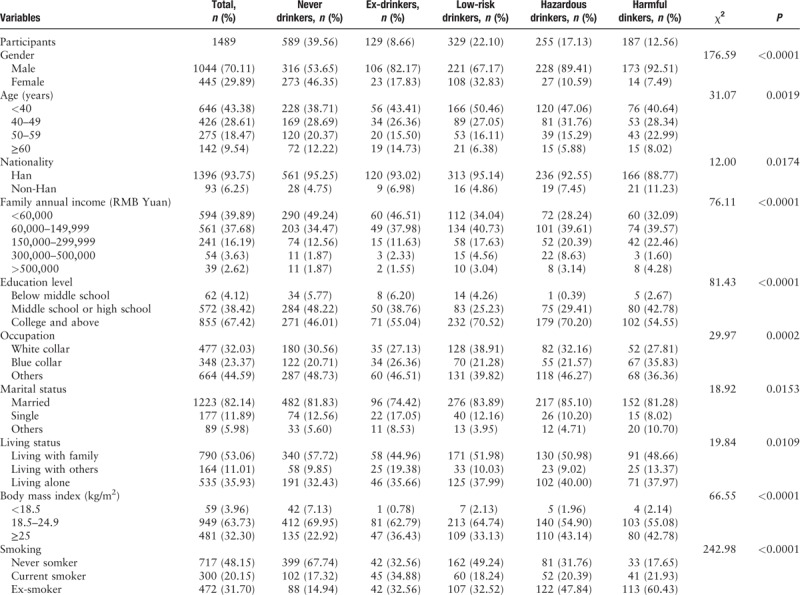
A total of 1489 participants completed the questionnaires. Among these 615 (41.30%) were from northern China, while 96 (6.45%), 397 (26.66%), 297 (19.95%), and 95 (6.38%) patients were from southern, western, eastern, and central China, respectively. The mean age of these participants was 43 years and 1044 (70.11%) were male in gender. A total of 1396 (93.75%) participants were of Chinese Han nationality. The family annual income of 594 (39.89%) participants was less than 60,000 RMB Yuan, while 561 (37.68%) had it between 60,000 RMB Yuan and 150,000 RMB Yuan. In terms of their education status, 855 (57.42%) individuals had college or higher education degree. The 477 (32.03%) participants were white collar, and 348 (23.37%) were blue collar. In addition, 1223 (82.14%) individuals were married. Analyses of the living status revealed that 790 (53.06%) patients were living with family, while 535 (35.93%) were living alone. A total of 32.30% of the participants had BMI of ≥25 kg/m2. The 717 (48.15%) participants were categorized as never smokers, while 300 (20.15%) were characterized as current smokers. The complete information about all the baseline characteristics of participants is summarized in Table 1.
Table 1.
Baseline characteristics of participants based on alcohol consumption categories.
Alcohol consumption analysis among patients with liver disease
Overall 900 (60.44%) participants were identified as alcohol drinkers, and among them, 129 (8.66%) were ex-drinkers. Alcohol drinking rate was observed to be higher among men in comparison to women (P < 0.0001). Among the 329 (22.10%) participants identified as low-risk drinkers, 67.17% were males and 32.83% were females. In contrast, among the 255 (17.13%) participants characterized as heavy drinkers, majority (84.91%) of them were male. Overall, a 187 (12.56%) participants met the criteria of alcohol dependence (harmful drinkers) [Table 1].
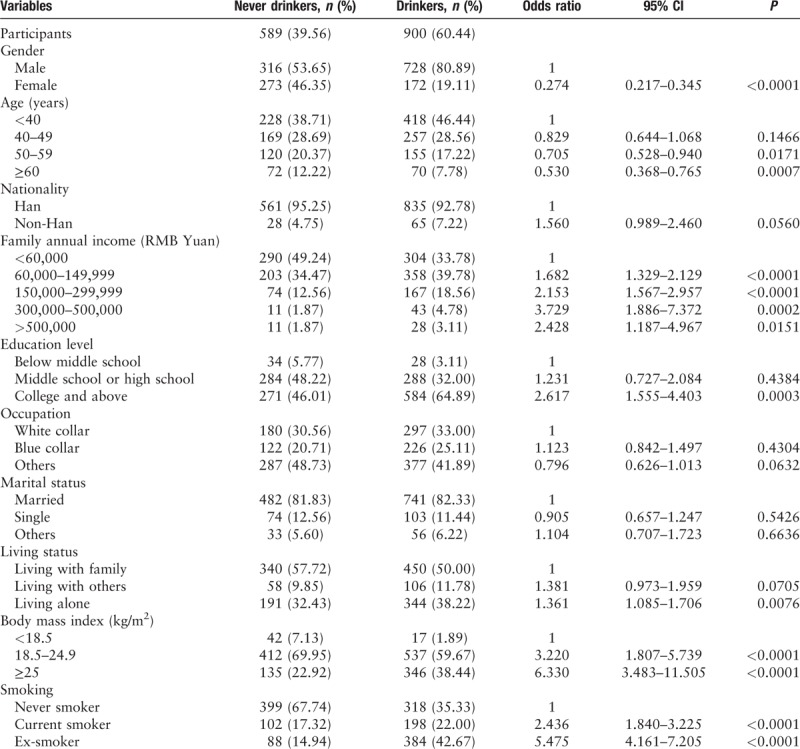
Multiple logistic regression analyses about the factors associated with alcohol consumption [Table 2], revealed that men were more likely to consume alcohol as compared to women (OR = 0.274, 95% CI = 0.217–0.345). In addition, patients younger than 40 years of age were more likely to drink alcohol than those aged between 50 and 59 years or aged older than 60 years (OR = 0.705, 95% CI = 0.528–0.940; OR = 0.530, 95% CI = 0.368–0.765, respectively). Higher family annual income (ranging from 60,000 to 500,000 RMB Yuan) also showed significant association with higher risk of alcohol consumption (OR = 1.682, 95% CI = 1.329–2.129; OR = 2.153, 95% CI = 1.567–2.957; OR = 3.729, 95% CI = 1.886–7.372, OR = 2.428, 95% CI = 1.187–4.967, respectively). Moreover, patients who have completed college or have higher education were also observed to consume higher amount of alcohol than those who had only completed middle school education (OR = 2.617, 95% CI = 1.555–4.403). The analysis of the living status revealed that patients living alone were more likely to consume alcohol than those living with family (OR = 1.361, 95% CI = 1.085–1.706). Importantly, increased BMI also showed correlation with higher risk of alcohol consumption (OR = 3.220, 95% CI = 1.807–5.739; OR = 6.330, 95% CI = 3.483–11.505, for BMI 18.5–24.9 and >25, respectively). The smoking status also showed interesting correlation, as current and ex-smokers were observed to more likely consume alcohol than never smokers (OR = 2.436, 95% CI = 1.840–3.225; OR = 5.475, 95% CI = 4.161–7.205, respectively). However, no significant relationship was found between nationality or area of residence or occupation or marital status with alcohol consumption.
Table 2.
Multiple logistic regression analyses of factors associated with alcohol consumption.
The data from AUDIT analysis are tabulated in Figure 1. A total of 43.56% of the alcohol drinking population consumed alcohol drink monthly or less, while 54.22% of them had 1 or 2 drinks on a typical day. Very small proportion (3.78%) of the patients had a drink containing alcohol 4 or more times a week, and 10 or more drinks each time [Figure 1A]. In addition, it was also noticed that 41.12% of the participants had 5 or more drinks on 1 occasion monthly. The 45.22% of them reported that they were not able to stop drinking once they had started at least monthly during the last year, and 41.44% failed to respond normally after drinking during the same time period. The 26.33% of them realized that they require a drink early in the morning to get themselves going after a heavy drinking session, at least monthly during the last year. The 44.33% of them had a feeling of guilt or remorse after drinking, while 40.89% were unable to remember what happened the night before because of their monthly drinking habit during the last year [Figure 1B]. The 21.33% reported that either they or someone else was injured due to their alcohol drinking. Interestingly, 58.56% of the participants revealed that either their relative, friend, doctor, or other health care worker were concerned about their drinking pattern and recommended to reduce alcohol consumption [Figure 1C].
Figure 1.
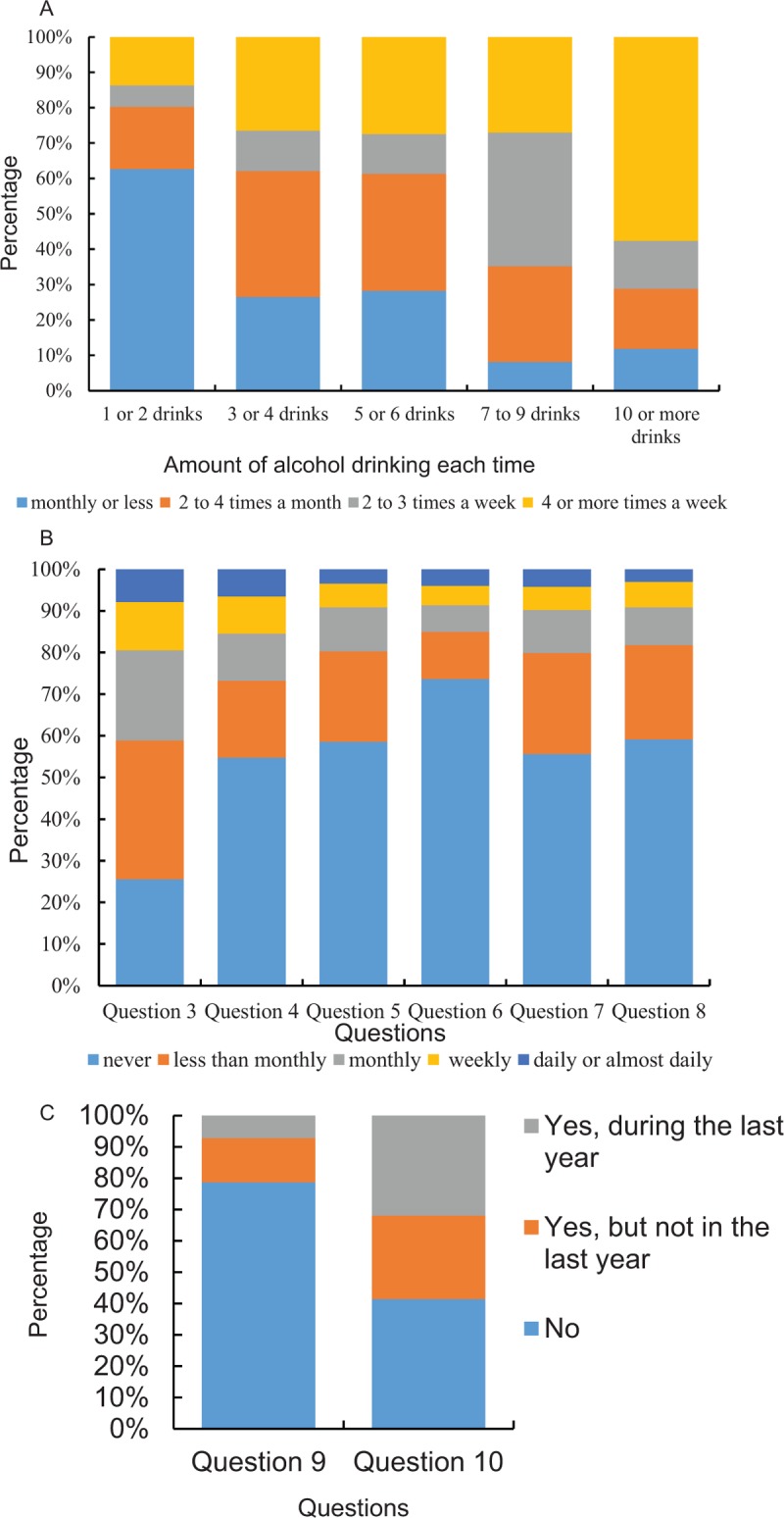
Tabulation of the results from Alcohol Use Disorders Inventory Test (AUDIT). (A) Question 1: How often do you have a drink containing alcohol? Question 2: How many drinks containing alcohol do you have on a typical day when you are drinking? (B) Question 3: How often do you have 5 or more drinks on one occasion? Question 4: How often during the last year you found that you were not able to stop drinking once you had started? Question 5: How often during the last year have you failed to do what was normally expected of you because of drinking? Question 6: How often during the last year you required a first drink in the morning to get yourself going after a heavy drinking session? Question 7: How often during the last year have you had a feeling of guilt or remorse after drinking? Question 8: How often during the last year have you been unable to remember what happened the night before because of your drinking? (C) Question 9: Have you or someone else been injured because of your drinking? Question 10: Has a relative, friend, doctor, or other health care worker been concerned about your drinking or suggested you to cut down?
Overall, total of 218 (24.22%) participants reported that they have been consuming alcohol from 1 to 5 years, while 209 (23.22%) have been doing it between 6 and 10 years. Among the type of drinks mostly consumed among these participants were white wine (50.01%) and beer (32.78%). Four hundred thirty (47.78%) patients mentioned social contact as the main reason for their alcohol consumption. A total of 519 (57.67%) participants never tried to stop drinking, while 252 (28.00%) of them tried but failed. Further, to successfully stop drinking, 387 (43.00%) patients wanted to go to the professional clinic of abstinence. However, 290 (32.22%) patients believed that moderate alcohol consumption was not harmful.
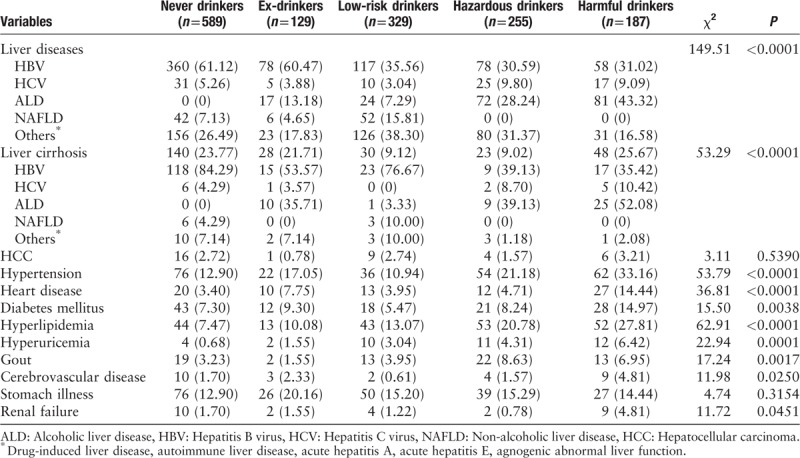
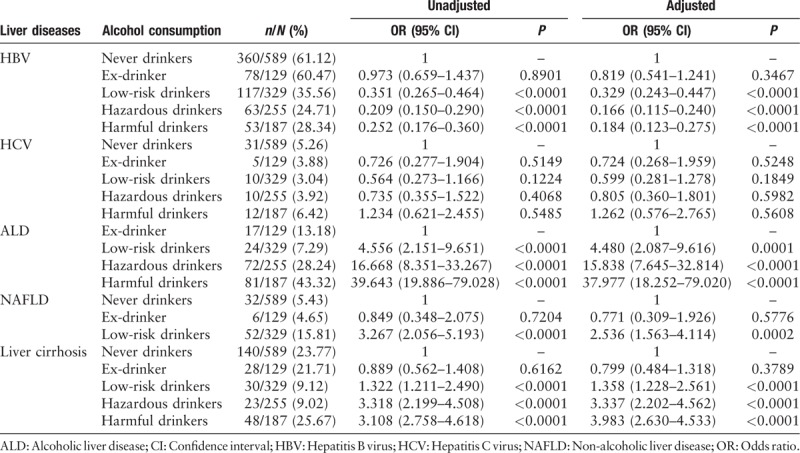
Correlation between alcohol consumption and liver diseases
We further analyzed the correlation between alcohol consumption and liver disease in these patients. It was observed that fair number of patients were primarily infected with HBV (691/1489, 46.41%). Notably, among the 269 (18.07%) participants having cirrhosis, its proportion was significantly high in harmful drinkers (P < 0.001). On the contrary, we observed no significant difference between drinkers and never drinkers in the rate of HCC among 36 (2.42%) patients with HCC [Table 3].
Table 3.
Prevalence of liver diseases and chronic medical conditions among patients categorized based on alcohol consumption, n (%).
Overall multiple logistic-regression-based analyses of association between alcohol consumption and liver diseases [Table 4], indicated that after adjustment, risk of alcoholic liver disease increased with increase in alcohol consumption (for low-risk drinkers, OR = 4.480, 95% CI = 2.087–9.616; for hazardous risk drinkers, OR = 15.838, 95% CI = 7.645–32.814; for harmful drinkers, OR = 37.977, 95% CI = 18.252–79.020, respectively). In addition, low-risk drinkers also displayed greater odds of NAFLD compared to never drinkers (OR = 2.536, 95% CI = 1.563–4.114). The risk of liver cirrhosis also increased with increase of alcohol consumption (for low-risk drinkers, OR = 1.358, 95% CI = 1.228–2.561; for hazardous risk drinkers, OR = 3.337, 95% CI = 2.202–4.562; for harmful drinkers, OR = 3.983, 95% CI = 2.630–4.533, respectively).
Table 4.
Multiple logistic regression analyses of factors associated with liver diseases.
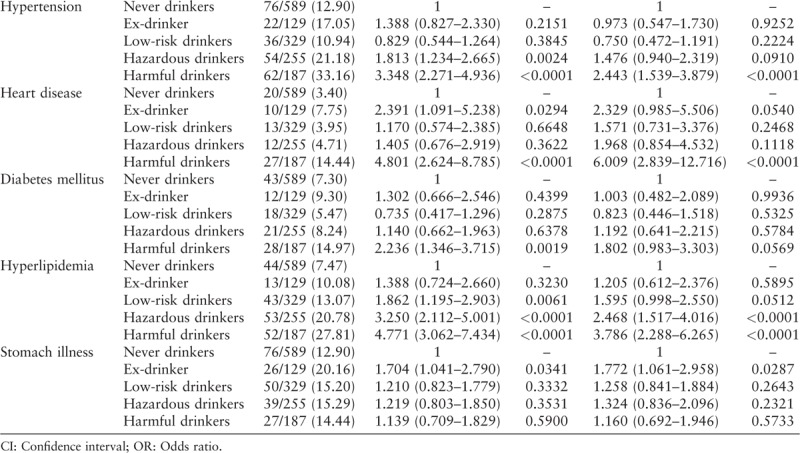
Association of alcohol consumption and chronic medical conditions
Typically, chronic medical conditions were quite common among men and women who participated in our study [Table 3]. Thus, we also analyzed the association between alcohol consumption and chronic medical conditions using multiple logistic regression analyses [Table 5]. It is important to note that we excluded several health conditions associated with alcohol consumption due to few number of cases for each of them like hyperuricemia, gout, cerebrovascular disease, and renal failure. However, after adjustment for variables, it was observed that harmful drinkers had greater odds of hypertension and heart diseases in comparison to never drinkers (OR = 2.443, 95% CI = 1.539–3.879; OR = 6.009, 95% CI = 2.839–12.716, respectively). In addition, hazardous and harmful drinkers also had greater odds of hyperlipidemia, as compared to never drinkers (OR = 2.468, 95% CI = 1.517–4.016; OR = 3.786, 95% CI = 2.288–6.265, respectively). However, no significant correlation was recorded between diabetes mellitus or stomach illness and alcohol consumption.
Table 5.
Multiple logistic regression analyses of factors associated with chronic medical conditions.
Discussion
There have been few detailed studies focused on analyzing the alcohol consumption among patients with liver disease in China. The major highlights of our study have been (1) among patients with liver disease, the alcohol drinking rate, and alcohol dependence (harmful drinking) rate in China were 60.44% and 12.56%, respectively; (2) alcohol consumption typically showed association with men younger than 40 years old, those having high family annual income, had college or higher education, living alone and higher BMI; (3) liver cirrhosis risk showed increased trend with increase in alcohol consumption; and (4) alcohol dependence (harmful drinking) enhanced the risk of hypertension, heart disease, and hyperlipidemia.
Importantly, our study noticed a higher prevalence of alcohol consumption than previously published studies,[2,19,20] and this could probably be related to the loose definition of “alcohol drinker.” However, it seems that loose definition was necessary to maximize the identification of all alcohol drinkers among patients with liver disease. More specifically, it was noticed that men had higher prevalence of alcohol consumption than women in China, and this finding was consistent with previous studies[1,19,20] and can be attributed to cultural values and norms.[21] Typically, Chinese men has a long history of alcohol consumption, in comparison to women. The proportion of female low-risk drinkers was 32.83%. As studies have demonstrated that women are more susceptible toward hepatotoxic effects of alcohol, it is advised that women should avoid alcohol drinking.
Our analysis also indicated that both current smokers and ex-smokers were more likely to consume alcohol in comparison to never smokers and was consistent with other published studies showing a direct relationship between alcohol consumption and smoking.[2,11,22,23] It has been reported that smoking exacerbates the effects of alcohol in inducing severe liver injury and favors development of HCC among patients with liver disease.[22,23]
Earlier studies have also indicated about the relationship between alcohol consumption and BMI,[24,25] and we also observed that alcohol consumption was associated with higher BMI. It has been shown that obesity is one of the most important environmental risk factor determining the risk of cirrhosis in heavy drinkers,[26] and heavy drinkers who are overweight for at least 10 years usually have a 2-fold risk of developing cirrhosis.
The association between educational level and alcohol drinking has also been explored earlier and some studies have suggested that less education directly correlates to alcohol dependence,[27,28] while other studies showed that education is related to increased daily alcohol consumption or problematic drinking.[29,30] Even some studies have indicated about no correlation between these 2 factors.[31] However, we in our study observed that patients with higher educational levels were more likely to drink alcohol.
In terms of living status and alcohol consumption, the study conducted in Norwegian women and men showed that living with a spouse or partner was positively associated with alcohol drinking.[32] However, we did not observe similar significant association in China. On the contrary, we noticed that living alone was more linked to higher alcohol consumption than living with family. These differences can be attributed to different drinking cultures. It has been observed that Chinese people drink more frequently at social occasions than with their spouse or partner at home. Another study showed that income levels were weakly associated with risk of heavy drinking.[30] However, our study revealed that increase in family annual income was significantly associated with higher risk of alcohol consumption.
Generally, NAFLD diagnosis requires exclusion of daily alcohol consumption by ≥30 g for men and 20 g for women.[33] However, the relationship between alcohol and liver injury depends on several cofactors like alcohol type, duration of exposure, drinking patterns, and individual susceptibility, thus rendering simple quantitative thresholds partly arbitrary. Specifically, patients with moderate alcohol drinking may still be predisposed to NAFLD, if they have other metabolic risk factors.[34] In our study, we found that low-risk drinkers had greater odds of developing NAFLD compared to never drinkers, thereby suggesting that it is better not to drink at all to avoid NAFLD.
Furthermore, we also identified that increased alcohol consumption led to increased risk of cirrhosis. It is very clear that there is a direct dose relationship between the amount of alcohol intake and likelihood of liver injury; yet, extensive variability exists between individuals. Only about 10% to 20% of the individuals with chronic heavy alcohol consumption usually develop advanced liver disease and cirrhosis, thereby indicating that additional disease modifiers and cofactors, such as behavioral, environmental, and genetic factors possibly play an important role.[35] The participants in our study commonly consumed white wine and beer, which seems to be consistent with local lifestyle. However due to small number of cases, the alcohol type effect could not be analyzed for the risk of cirrhosis and HCC. Previous studies also could not assess the impact of alcohol type (wine vs. beer vs. liquors) and drinking patterns (ie, binge drinking and drinking outside meals) on cirrhosis and HCC,[35] thus indicating toward large epidemiological studies.
Interestingly, alcohol consumption leads to social, family, occupational, and psychologic damage, as along with clinical comorbidities. Multiple studies have shown higher risk of hypertension,[24] cardiovascular disease,[36] and heperlipemia,[37] due to increased alcohol intake. In the present study, we also observed that alcohol dependence (harmful drinking) increased the risk of important chronic medical conditions (hypertension, heart diseases, and hyperlipidemia). However, causal relationship between alcohol consumption and chronic medical conditions could not be examined due to the cross-sectional nature of our study. But, after statistical adjustment for social-demographic factors, we indeed described the persisted association of alcohol intake with chronic medical conditions. Consistent with our data, results of another study also suggested that elevated rates of hypertension and hyperlipidemia among harmful drinkers might increase mortality rate due to coronary heart disease or cerebrovascular disease.[38] Therefore, it is always advised to reduce alcohol drinking so as to lower the risk of hypertension, heart diseases, and hyperlipidemia.
Finally, it is important to highlight some of the limitations and important implications of our study. First, cross-sectional design precluded our study from examining causal relationships, thereby indicating toward additional randomized controlled or cohort studies. Second, the information about sociodemographic status, alcohol consumption, liver diseases and chronic medical conditions was self-reported, thus more prone to information bias and/or recall bias. However, some studies have shown that self-reported information was reasonably reproducible, suggesting reliability.[39,40] Third, our study lacked precise quantification of alcohol consumption. While self-reported information/categories could be imperfect, but they do identify harmful drinkers, and our outcome data support that. Moreover, our current analytic categories of “low-risk drinkers,” “hazardous drinkers,” and “harmful drinkers” were based on the AUDIT score, a widely used internationally validated WHO tool. Fourth, participants were not chosen to directly represent Chinese population as they being younger and better educated, but it still represents a group of Chinese people, who are community embedded, and generally reflective of the Chinese population, in terms of other social and economic characteristics.
Conclusion
In summary, our study predicted that prevalence of alcohol consumption and alcohol dependence among patients with liver disease was high in China. In addition, patients with liver disease commonly acknowledged that alcohol drinking is harmful, which indicated that these individual still drank heavily despite knowing the consequences. Thus, it is imperative to devise new strategies to raise public awareness about the harmful effects of alcohol, screen alcohol drinking, and conduct brief intervention sessions in the outpatient department. It would also be helpful to set up abstinence clinics or organizations, with intent to convince patients with liver disease to stay away from alcohol consumption.
Acknowledgements
A total of 39 hospitals in 30 provinces, autonomous regions, and municipalities across China were involved. The authors thank all the investigators of these hospitals who conducted this survey.
Conflicts of interest
None.
Footnotes
How to cite this article: Xie YD, Zhao CQ, Wang JP, Cheng CS, Zhou JY, Zhang Y, Xia H, Wei L. Alcohol consumption analysis among patients with liver disease in China. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000043
References
- 1.Global status report on alcohol and health 2014. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/en/ Accessed 21 Aug 2018 [Google Scholar]
- 2.Lee YH, Wang Z, Chiang TC, Liu CT. Beverage intake, smoking behavior, and alcohol consumption in contemporary china—a cross-sectional analysis from the 2011 China Health and nutrition survey. Int J Environ Res Public Health 2017; 14:493.doi: 10.3390/ijerph14050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lam S, Mandrekar SJ, Gesthalter Y, Allen Ziegler KL, Seisler DK, Midthun DE, et al. A randomized phase IIb trial of myo-Inositol in smokers with bronchial dysplasia. Cancer Prev Res (Phila) 2016; 9:906–914. doi: 10.1158/1940-6207.CAPR-15-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calès P, Boursier J, Lebigot J, de Ledinghen V, Aubé C, Hubert I, et al. Liver fibrosis diagnosis by blood test and elastography in chronic hepatitis C: agreement or combination? Aliment Pharmacol Ther 2017; 45:991–1003. doi: 10.1111/apt.13954. [DOI] [PubMed] [Google Scholar]
- 5.Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol 2008; 48:335–352. doi: 10.1016/j.jhep.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Stroffolini T, Cotticelli G, Medda E, Niosi M, Del Vecchio-Blanco C, Addolorato G, et al. Interaction of alcohol intake and cofactors on the risk of cirrhosis. Liver Int 2010; 30:867–870. doi: 10.1111/j.1478-3231.2010.02261.x. [DOI] [PubMed] [Google Scholar]
- 7.Boccato S, Pistis R, Noventa F, Guido M, Benvegn L, Alberti A. Fibrosis progression in initially mild chronic hepatitis C. J Viral Hepat 2006; 13:297–302. doi: 10.1111/j.1365-2893.2005.00683.x. [DOI] [PubMed] [Google Scholar]
- 8.Harris DR, Gonin R, Alter HJ, Wright EC, Buskell ZJ, Hollinger FB, et al. The relationship of acute transfusion-associated hepatitis to the development of cirrhosis in the presence of alcohol abuse. Ann Intern Med 2001; 134:120–124. doi: 10.7326/0003-4819-134-2-200101160-00012. [DOI] [PubMed] [Google Scholar]
- 9.Li G, Cai AP, Mo YJ, Chen JY, Wei RB, Huang YQ, et al. Effects of guideline-based hypertension management in rural areas of Guangdong Province. Chin Med J 2015; 128:799–803. doi: 10.4103/0366-6999.152644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong SW, Linton JA, Shim JY, Kang HT. High-risk drinking is associated with a higher risk of diabetes mellitus in Korean men, based on the 2010-2012 KNHANES. Alcohol 2015; 49:275–281. doi: 10.1016/j.alcohol.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Udo T, Vásquez E, Shaw BA. A lifetime history of alcohol use disorder increases risk for chronic medical conditions after stable remission. Drug Alcohol Depend 2015; 157:68–74. doi: 10.1016/j.drugalcdep.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Roerecke M, Gual A, Rehm J. Reduction of alcohol consumption and subsequent mortality in alcohol use disorders: systematic review and meta-analyses. J Clin Psychiatry 2013; 74:e1181–e1189. doi: 10.4088/JCP.13r08379. [DOI] [PubMed] [Google Scholar]
- 13.Mirijello A, D’ Angelo C, Ferrulli A, Vassallo G, Antonelli M, Caputo F, et al. Identification and management of alcohol withdrawal syndrome. Drugs 2015; 75:353–365. doi: 10.4088/JCP.13r08379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verrill C, Smith S, Sheron N. Are the opportunities to prevent alcohol related liver deaths in the UK in primary or secondary care? A retrospective clinical review and prospective interview study. Subst Abuse Treat Prev Policy 2006; 1:16.doi: 10.1186/1747-597X-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLoS One 2011; 6:e23748.doi: 10.1371/journal.pone.0023748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaner EF, Dickinson HO, Beyer F, Crane D, Brown J, Muirhead C, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev 2009; 28:301–323. doi: 10.1111/j.1465-3362.2009.00071.x. [DOI] [PubMed] [Google Scholar]
- 17.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 18.Sheron N, Moore M, Brien WO, Harris S, Roderick P. Feasibility of detection and intervention for alcohol-related liver disease in the community: the Alcohol and Liver Disease Detection study (ALDDeS). Br J General Pract 2013; 63:e698–e705. doi: 10.3399/bjgp13X673711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu B, Mao Z-F, Rockett IR, Yue Y. Socioeconomic status and alcohol use among urban and rural residents in China. Subst Use Misuse 2008; 43:952–966. doi: 10.1080/10826080701204961. [DOI] [PubMed] [Google Scholar]
- 20.Zhou X, Su Z, Deng H, Xiang X, Chen H, Hao W, et al. A comparative survey on alcohol and tobacco use in urban and rural populations in the Huaihua District of Hunan Province. China Alcohol 2006; 39:87–96. doi: 10.1016/j.alcohol.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Bratberg GH, C Wilsnack S, Wilsnack R, Håvås Haugland S, Krokstad S, Sund ER, et al. Gender differences and gender convergence in alcohol use over the past three decades (1984–2008), The HUNT Study, Norway. BMC Public Health 2016; 16:723.doi: 10.1186/s12889-016-3384-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan TR, Mandayam S, Jamal MM. Alcohol and hepatocellular carcinoma. Gastroenterology 2004; 127:S87–S96. doi: 10.1053/j.gastro.2004.09.0.020. [DOI] [PubMed] [Google Scholar]
- 23.Daskalopoulou C, Stubbs B, Kralj C, Koukounari A, Prince M, Prina AM. Associations of smoking and alcohol consumption with healthy ageing: a systematic review and meta-analysis of longitudinal studies. BMJ Open 2018; 8:e019540.doi: 10.1136/bmjopen-2017-019540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wakabayashi I. Body weight-dependent relationships between alcohol consumption and pulse pressure in middle-aged Japanese women. J Am Soc Hypertens 2017; 11:801–810. doi: 10.1016/j.jash.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 25.Dumesnil C, Dauchet L, Ruidavets JB, Bingham A, Arveiler D, Ferrières J, et al. Alcohol consumption patterns and body weight. Ann Nutr Metab 2013; 62:91–97. doi: 10.1159/000342839. [DOI] [PubMed] [Google Scholar]
- 26.Hart CL, Morrison DS, Batty GD, Mitchell RJ, Davey Smith G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ 2010; 340:c1240.doi: 10.1136/bmj.c1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu YB, Liu L, Li YF, Chen YL. Relationship between health literacy, health-related behaviors and health status: a survey of elderly Chinese. Int J Environ Res Public Health 2015; 12:9714–9725. doi: 10.3390/ijerph120809714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grant JD, Scherrer JF, Lynskey MT, Agrawal A, Duncan AE, Haber JR, et al. Associations of alcohol, nicotine, cannabis, and drug use/dependence with educational attainment: evidence from cotwin-control analyses. Alcohol Clin Exp Res 2012; 36:1412–1420. doi: 10.1111/j.1530-0277.2012.01752.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huerta MC, Borgonovi F. Education, alcohol use and abuse among young adults in Britain. Soc Sci Med 2010; 71:143–151. doi: 10.1016/j.socscimed.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 30.Brunborg GS. Positive and negative affectivity as risk factors for heavy drinking in the second half of life: a prospective cohort study. Addiction 2017; 112:801–807. doi: 10.1111/add.13718. [DOI] [PubMed] [Google Scholar]
- 31.Schroder H, Rohlfs I, Schmelz EM, Marrugat J. REGICOR Investigators. Relationship of socioeconomic status with cardiovascular risk factors and lifestyle in a Mediterranean population. Eur J Nutr 2004; 43:77–85. doi: 10.1007/s00394-004-0443-9. [DOI] [PubMed] [Google Scholar]
- 32.Li J, Wu B, Selbæk G, Krokstad S, Helvik AS. Factors associated with consumption of alcohol in older adults - a comparison between two cultures, China and Norway: the CLHLS and the HUNT-study. BMC Geriatr 2017; 17:172.doi: 10.1186/s12877-017-0562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol 2010; 53:372–384. doi: 10.1016/j.jhep.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 34.Bellentani S, Saccoccio G, Masutti F, Croce LS, Brandi G, Sasso F, et al. Prevalence of and risk factors for hepatic steatosis in Northern Italy. Ann Intern Med 2000; 132:112–117. doi: 10.7326/0003-4819-132-2-200001180-00004. [DOI] [PubMed] [Google Scholar]
- 35.Singal AK, Bataller R, Ahn J, Kamath PS, Shah VH. ACG clinical guideline: alcoholic liver disease. Am J Gastroenterol 2018; 113:175–194. doi: 10.7326/0003-4819-132-2-200001180-00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang L, Wu YQ, Tang X, et al. Profile and correlates of health-related quality of life in chinese patients with coronary heart disease. Chin Med J 2015; 128:1853–1861. doi: 10.4103/0366-6999.160486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wakabayashi I. Difference in sensitivities of blood HDL cholesterol and LDL cholesterol levels to alcohol in middle-aged Japanese men. Alcohol 2018; 67:45–50. doi: 10.1016/j.alcohol.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 38.Fan J, Li GQ, Liu J, Wang W, Wang M, Qi Y, et al. Impact of cardiovascular disease deaths on life expectancy in Chinese population. Biomed Environ Sci 2014; 27:162–168. doi: 10.3967/bes2014.037. [DOI] [PubMed] [Google Scholar]
- 39.Ekholm O, Strandberg-Larsen K, Christensen K, Gronbaek M. Comparison of assessment methods for self-reported alcohol consumption in health interview surveys. Eur J Clin Nutr 2008; 62:286–291. doi: 10.1038/sj.ejcn.1602728. [DOI] [PubMed] [Google Scholar]
- 40.Bowlin SJ, Morrill BD, Nafziger AN, Lewis C, Pearson TA. Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: the behavioral risk factor survey. J Clin Epidemiol 1996; 49:511–517. doi: 10.1016/0895-4356(96)00010-8. [DOI] [PubMed] [Google Scholar]


