To the Editor: While it is only occasionally clinical significance, multiple bilateral iridociliary cysts are commonly encountered. With the cysts progressively growing larger, they may result in vision obstruction, glaucoma, or other ocular problems.[1] Here, we reported an unusual case of multiple ciliary cysts triggering glare with the treatment of neodymium-doped yttrium aluminium garnet (Nd:YAG) laser cystectomy.
An 18-year-old man with a long-standing history of glare in both eyes visited Ophthalmology Clinic, Shanghai 9th People's Hospital for diagnosis and treatment. Before this visit, dry eye, mental aberrations, and intracranial lesions were suspected by several doctors. However, none of the previous therapies were proved to be effective. Afterwards, the patient's symptoms aggravated. No remarkable medical history or family history was noted. The patient's visual acuity, intraocular pressure, Schirmer's test, the break-up time, and appearance of pupils and iris were normal. During our clinical consultation, the test using Optical Quality Analysis System (OQAS; Visiometrics, Terrassa, Spain) was taken. The main parameters of OQAS include modulation transfer function (MTF) cutoff, Strehl ratio, and objective scattering index (OSI). The former 2 parameters are positively correlated with visual quality, while OSI is correlated negatively. OSI is indirectly associated with glare. The results of OQAS showed subnormal optical quality, the MTF cutoff, Strehl ratio, and OSI were 24.855, 0.513, and 1.6 in the right eye [Figure 1A], and 22.124, 0.141, and 1.9 in the left eye [Figure 1B], respectively. OSI value reflected worse objective scattering in both eyes than average level of his age group. Ultrasound biomicroscopy (UBM) revealed multiple non-pigmented ciliary body cysts in both eyes [Figure 1C]. Considering that no other structural abnormalities were found, the patient was diagnosed as primary iridociliary cysts associated with glare.
Figure 1.
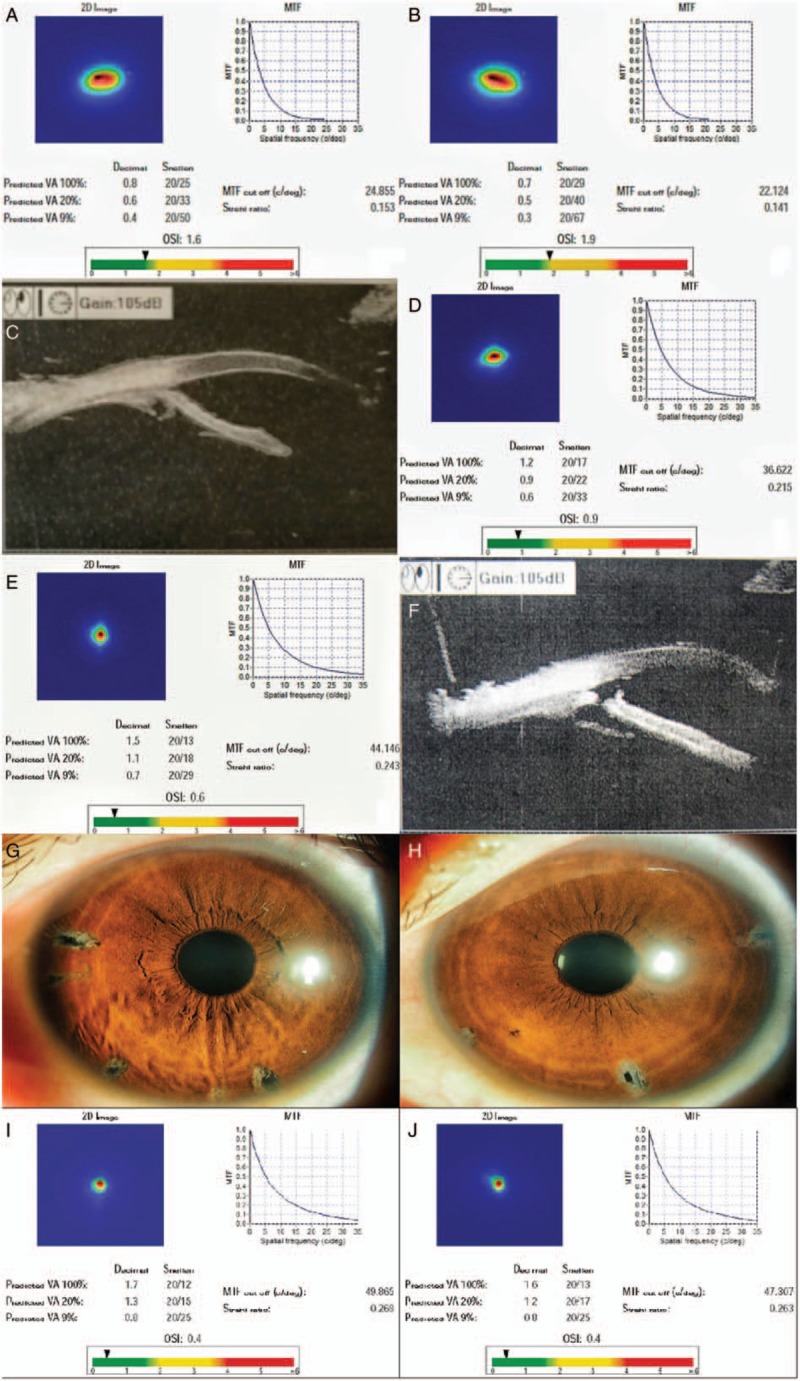
An 18-year-old man with primary iridociliary cysts associated with glare. (A and B) OQAS data of both eyes prior to laser surgery. (C and D) OQAS data of both eyes after laser treatment. (E and F) UBM of the left eye (a spot close to 3 o’clock) before and after surgery. (G and H) Slit-lamp photographs of both irises after surgery. (I and J) OQAS data of both eyes at 1-year follow-up. MTF: Modulation transfer function; OQAS: Optical quality analysis system; OSI: Objective scattering index; UBM: Ultrasound biomicroscopy.
From March to April 2016, repetitive bilateral YAG laser cystectomy through iris incision was performed. To avoid excessive hemorrhage during operation, the cystectomy was planned to be completed within 3 sessions. In the first place, we dealt with the most prominent cysts in the iris with referral to UBM results. Excitingly, the dazzling glare alleviated immediately after the treatment. The OQAS test and UBM were performed once more after surgery (on August 8, 2016); the results showed that the MTF cutoff, Strehl ratio, and OSI were 36.622, 0.215, and 0.9, in the right eye [Figure 1D], and 44.146, 0.243, and 0.6 in the left eye [Figure 1E], respectively. The increased MTF cutoff and Strehl ratio as well as the decreased OSI implied improved visual quality and light gathering power. The patient's symptom of glare has completely disappeared after the entire treatment. Laser holes were evident on UBM as well as slit-lamp microscope examination [Figure 1F–1H]. Furthermore, during the over 1-year follow-up, the last examination (on August 17, 2017) suggested that the MTF cutoff, Strehl ratio, and OSI were 49.865, 0.269, and 0.400 in the right eye [Figure 1I], and 47.307, 0.263, and 0.400 in the left eye [Figure 1J], respectively, which demonstrated a long-term stability of optical quality after treatment.
Lens coloboma or cataracts may develop when the cysts compress the lens and the zonulae.[2] Furthermore, if the cysts overlap the optical axis, visual loss, strabismus, and amblyopia may occur.[3,4] In addition, corneal injury, lens luxation, and vitreous hemorrhage are also among the complications of iridociliary cysts.[4,5] In this case, we believed that ciliary body cysts compressed the zonulae of this patient, physically disrupting lens accommodation by compromising lens regularity. Glare caused by iridociliary cysts is rarely reported. Hence, we speculated that glare might be an under-recognized complication of primary iridociliary cysts and should be evaluated clinically. At present, there is no direct method to detect what extent the lens and zonulae are influenced by the cysts, so we could only analyze the cause and mechanism in theory. To date, we have successfully diagnosed and treated three similar cases of male adolescents with long-term glare over the past decade. They all exhibited no other organic disease except iridociliary cysts and benefited from the YAG laser cystectomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Funding
This study was supported by a grant from the Science and Technology Commission of Shanghai (No. 17DZ2260100).
Conflicts of interest
None.
Footnotes
How to cite this article: He TR, Zhu Y, Zhu DQ, Zhou JB. Neodymium-doped yttrium aluminium garnet laser treating cysts of the ciliary body with glare. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000068
References
- 1.Shields CL, Kancherla S, Patel J, Vijayvargiya P, Suriano MM, Kolbus E, et al. Clinical survey of 3680 iris tumors based on patient age at presentation. Ophthalmology 2012; 119:407–414. doi: 10.1016/j.ophtha.2011.07.059. [DOI] [PubMed] [Google Scholar]
- 2.Khan AO, Assiri AA. Lens coloboma associated with a ciliary body cyst. Ophthalmic Genet 2007; 28:208–209. doi: 10.1080/13816810701531260. [DOI] [PubMed] [Google Scholar]
- 3.Holly VL, Sandmeyer LS, Bauer BS, Verges L, Grahn BH. Golden retriever cystic uveal disease: a longitudinal study of iridociliary cysts, pigmentary uveitis, and pigmentary/cystic glaucoma over a decade in western Canada. Vet Ophthalmol 2016; 19:237–244. doi: 10.1111/vop.12293. [DOI] [PubMed] [Google Scholar]
- 4.Lois N, Shields CL, Shields JA, Mercado G, De Potter P. Primary iris stromal cysts. A report of 17 cases. Ophthalmology 1998; 105:1317–1322. [DOI] [PubMed] [Google Scholar]
- 5.Rivero V, Aparicio MJ, Suárez-Leoz M, Fernández A. Vitreous hemorrhage secondary to iridociliary cyst. Arch Soc Esp Oftalmol 2015; 90:600–603. doi: 10.1016/j.oftal.2014.09.006. [DOI] [PubMed] [Google Scholar]


