Abstract
Background:
Kidney transplant is always emergent operations and frequently need to be performed at nighttime to reduce cold ischemia time (CIT). Previous studies have revealed that fatigue and sleep deprivation can result in adverse consequences of medical procedures. This study aimed to evaluate whether nighttime operation has adverse impact on kidney transplant.
Methods:
A retrospective analysis of recipients accepted kidney transplant from deceased donors in one center from 2014 to 2016 was performed. Daytime transplant was defined as operation started after 8 am or ended before 8 pm and nighttime operation was defined as operation ended after 8 pm or started before 8 am. The incidences of complications such as delayed graft function, acute rejection, surgical complications and nosocomial infections were compared between 2 groups. Student's t-test was used to analyze continuous variables such as serum creatinine (Scr) at 1-year of post-transplant. The Chi-square test was used to analyze categorical variables. Differences in recipients and graft survival were analyzed using Kaplan–Meier methodology and log-rank tests.
Results:
Among the 443 recipients, 233 (52.6%) were classified into the daytime group and the others 210 (47.4%) were in the nighttime group. The 1-year survival rate of recipients was similar for the recipients in the daytime and nighttime groups (95.3% vs. 95.2%, P = 0.981). Although the 1-year graft survival rate in the nighttime group was slightly superior to that in the daytime group, the difference was not significant (92.4% vs. 88.4%, P = 0.164). Furthermore, Scr and incidence of complications were also not significantly different between the 2 groups.
Conclusions:
Our results suggested that operation time of kidney transplant with short CIT has no significant impact on the outcome of kidney transplant. Nighttime operation of kidney transplant with short CIT could be postponed to the following day to alleviate the burden on medical staffs and avoid the potential risk.
Keywords: Kidney transplant, Delayed graft function, Donation after cardiac death, Nighttime transplant
Introduction
Kidney transplant is often an emergent procedure to keep shorter cold ischemia time (CIT). Prolonged CIT will lead to higher graft failure.[1,2] Performance of kidney transplant from deceased donor largely depends on the time of kidney donation and transport. In general, when there is a donation, there will be a transplant.
In China, doctors often overwork and are in the condition of fatigue and sleep deprivation according to the report of occupational status for Chinese doctors in 2017 from the Chinese Medical Doctor Association and a survey in the most popular bio-medical website in China.[3,4] But very few studies have focused on the relationship of adverse clinical outcomes with overwork of Chinese medical staffs. In particular, the number of organs transplant from donation after cardiac death (DCD) has dramatically increased to alleviate the organ shortage after initiation of DCD from 2010.[5,6] Undoubtedly, experts in kidney transplant will face great psychosomatic challenge from emergent operations. Therefore, we retrospectively collected data of kidney transplant after DCD from January 2014 to December 2016 in a single-center to explore whether operation time is associated with outcome of recipients and grafts in kidney transplant.
Methods
Study design and ethical approval
A single-center retrospective study was conducted in First Affiliated Hospital of Xi’an Jiaotong University, China. All courses of DCD were performed by the Organ Procurement Organization of the First Affiliated Hospital of Xi’an Jiaotong University and supervised by the Red Cross Society of Shaanxi Province. All allograft kidney transplants were approved by the Ethics Committee of the hospital. The process of DCD in China has been described previously.[7] Prospective data of donors and recipients were retrospectively collected from the Registry System of Organ Donation Database and Electronic Medical Record System. Recipients who received dual kidneys, children's kidney or combined liver transplant were excluded. At last, 443 patients received kidney transplant from DCD from January 1, 2014 to December 31, 2016 were collected. Transplant operations started after 8 am or ended before 8 pm were assigned into the daytime group. In other words, daytime operations were only performed between 8 am and 8 pm. Transplant operations that ended after 8 pm or started before 8 am were classified into the nighttime group.
Transplant procedures
All kidney transplants were operated by vice-chief or chief transplant surgeons in the Department of Kidney Transplantation of our hospital and started at skin incision and ended at skin closure. The donor's kidney was placed at iliac fossa of recipient outside the peritoneal cavity. Donor renal artery (arteries) was anastomosed to internal or external iliac artery (end-to-end or end-to-side) of the recipient. Conversely, donor renal vein was anastomosed to the external iliac vein of the recipient. Extra-vesical anti-reflexive technique was applied in the anastomosis between ureter and bladder. Routinely, suitable ureteral stent was placed to prevent stricture of uretero-vesical junction before uretero-vesical anastomosis.
Outcomes
Surgical complications after kidney transplantation within the first year were analyzed. The complications only associated with operative procedures were considered as surgical complications including vascular, urological, wound complications and hematoma around graft. Graft artery stenosis and rupture, graft vein thrombosis and rupture, and dissection of artery were considered vascular complications. Ureteral stricture, ureteral thrombosis of graft, and urine leakage were considered as urological complications.
Patient and graft survival were followed up for 1 day to 48 months or from the operation day to January 2018 by outpatient follow-up and telephone follow-up with interquartile range of 18.5 months and median of 22 months. Restart of renal replacement therapy was the hallmark of graft failure. Graft function was analyzed based on the level of serum creatinine (Scr) at 1-year of post-transplant and 1-year graft survival. Delayed graft function (DGF), acute rejection (AR) and nosocomial infections were also analyzed. DGF was defined as i) need dialysis in the first week of post-transplantation and ii) Scr >221 μmol/L (2.50 mg/dL) on the seventh day of post-transplantation. AR was diagnosed with graft tissue biopsy or clinical inference. Nosocomial infections refer to urological, respiratory, incision and catheter-associated infection after transplantation.
Statistical analysis
Continuous variables with normal distribution were compared by Student's t-test and categorical variables were compared by chi-square (χ2) test. The measurement data of skewed distribution were analyzed by nonparametric rank sum test. The survival rates of patients and grafts were estimated by Kaplan–Meier methodology and compared using log-rank tests. SPSS 18.0 (IBM Company, USA) was applied to analyze all data. The P value less than 0.05 with the 2-side tail test was considered as statistically significant.
Results
Baseline demographics
Totally 443 kidney transplant recipients from January 1, 2014 to December 31, 2016 met the enrollment criteria and their data were collected. Table 1 shows the basic characteristics of recipients and donors in the daytime and nighttime groups. Donors in daytime group were significantly older (P = 0.012) and had significantly higher body mass index (BMI) (P = 0.018) than those in the nighttime group. Male donors accounted for 79.2% in total. Expanded criteria donors (ECDs) were those >60 years old or 50 to 59 years old with two of the following conditions: hypertension, died from cerebrovascular disease, or Scr >133 μmol/L (1.50 mg/dL) before donation.[8] Non-ECDs were standard criteria donors (SCDs). In total, 20.9% kidney grafts were from ECDs, and an increasing trend was shown in the number and ratio of ECD year after year [Figure 1]. Meanwhile, kidney transplant of deceased donors increased rapidly from 2014 to 2016 [Figure 1].
Table 1.
Baseline characteristics of the kidney transplant recipients.
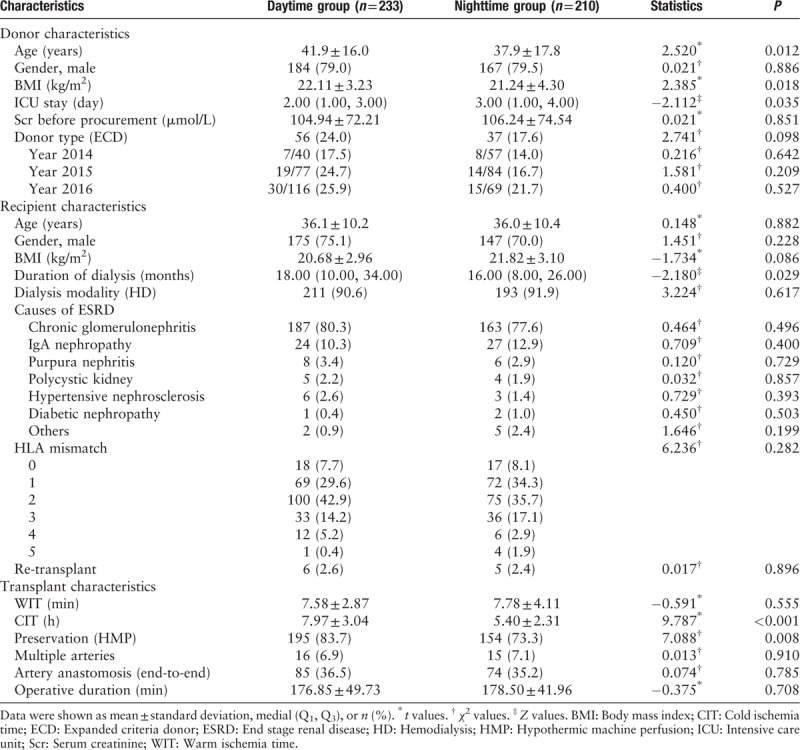
Figure 1.
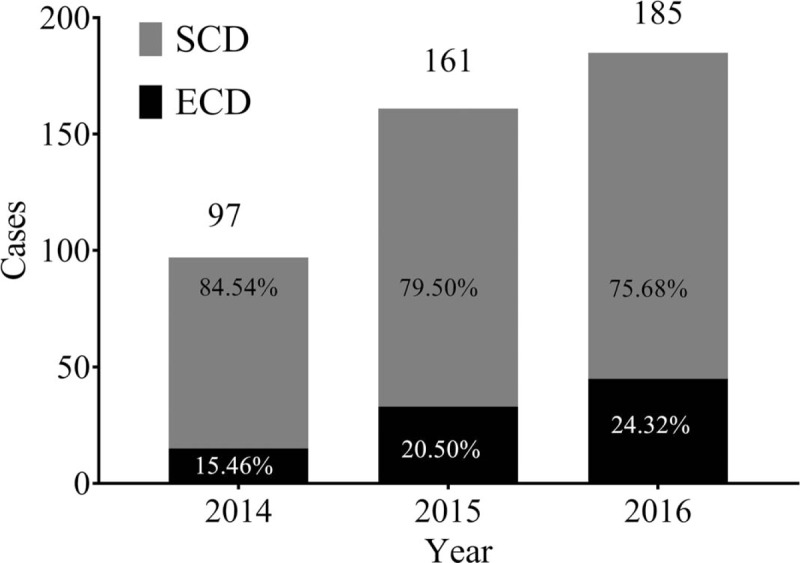
The number of DCD donors and ratio of ECD in our center from 2014 to 2016. DCD: Donation after cardiac death, ECD: Expanded criteria donor, SCD: Standard criteria donors.
Among the 443 kidney transplants, 233 (52.6%) started after 8 am and ended before 8 pm and assigned into the daytime group, while 210 (47.4%) ended after 8 pm or started before 8 am and were classified into the nighttime group. The period from 8 am to 10 am was the most frequent time period for kidney transplant [Figure 2]. Duration of dialysis of recipients in daytime group was longer than that of nighttime group (P = 0.029). The longest CIT among all graft kidneys was 16 h, and CIT was significantly shorter in nighttime group than in daytime group (P < 0.001). In addition, 78.8% kidneys were preserved by hypothermic machine perfusion (HMP) and the rest were by static cold storage. Meanwhile, HMP was more frequently used in daytime group than in nighttime group (P = 0.008). End-stage renal disease (ESRD) was developed in most recipients due to chronic glomerulonephritis (79.0%) and IgA nephropathy (11.5%). Moreover, before transplant, 404 (91.2%) recipients had undergone hemodialysis, 37 (8.4%) accepted peritoneal dialysis and 2 (0.5%) did not initiate dialysis. Totally, recipients had been treated with dialysis for approximately 23 months in average before transplant. The HLA mismatch distributed similarly in daytime and nighttime groups. No significant difference was found in operative time between the 2 groups and the mean operative duration was around 178 minutes.
Figure 2.
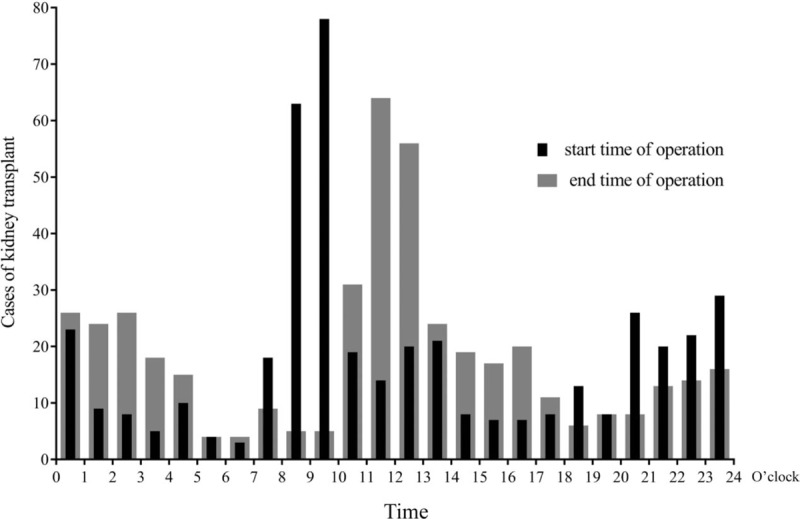
Distribution of beginning and end time of kidney transplant operation.
Complications and graft function
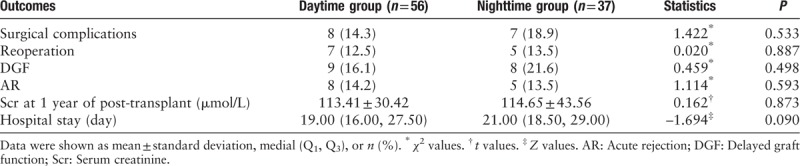
Table 2 shows outcomes of the recipients. Among all recipients, 16.5% had surgical complications, 12.4% had reoperation, 15.4% had DGF, 10.2% had AR, and 16.9% had nosocomial infection. However, the incidence of complications was not significantly different between recipients in the daytime and nighttime groups. The level of Scr at 1 year of post-transplantation was 99.0 ± 29.9 μmol/L and 104.2 ± 32.7 μmol/L for recipients in the nighttime and daytime groups, respectively, showing no significant difference (P = 0.113).
Table 2.
Outcomes of the kidney transplant recipients.
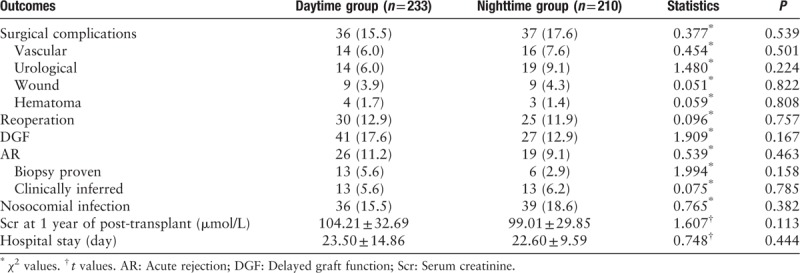
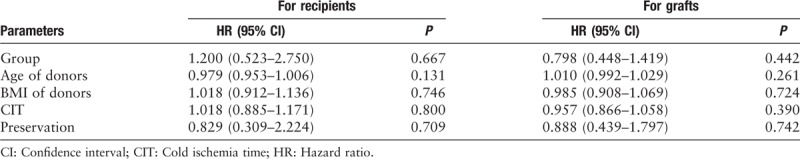
Figure 3 shows the long-term survival of recipients and grafts in the 2 groups. The difference in 1-year survival rate of recipients was not significant in the daytime and nighttime groups (95.3% vs. 95.2%, P = 0.981). The 1-year graft survival rate of recipients in the nighttime group was slightly higher than that in the daytime group by Kaplan-Meier method, but the difference did not reach statistical significance (92.4% vs. 88.4%, P = 0.164). Figure 4 shows the 1-year survival of recipients and grafts for ECDs in the two groups. Similarly, the difference did not reach the significance (92.9% vs. 94.6%, P = 0.713). For ECDs, the 1-year graft survival rate was not significant in the daytime and nighttime groups (82.1% vs. 86.5%, P = 0.555). Cox regression analyses show that no single factor had significant impacts on the survival of recipients and grafts [Table 3].
Figure 3.
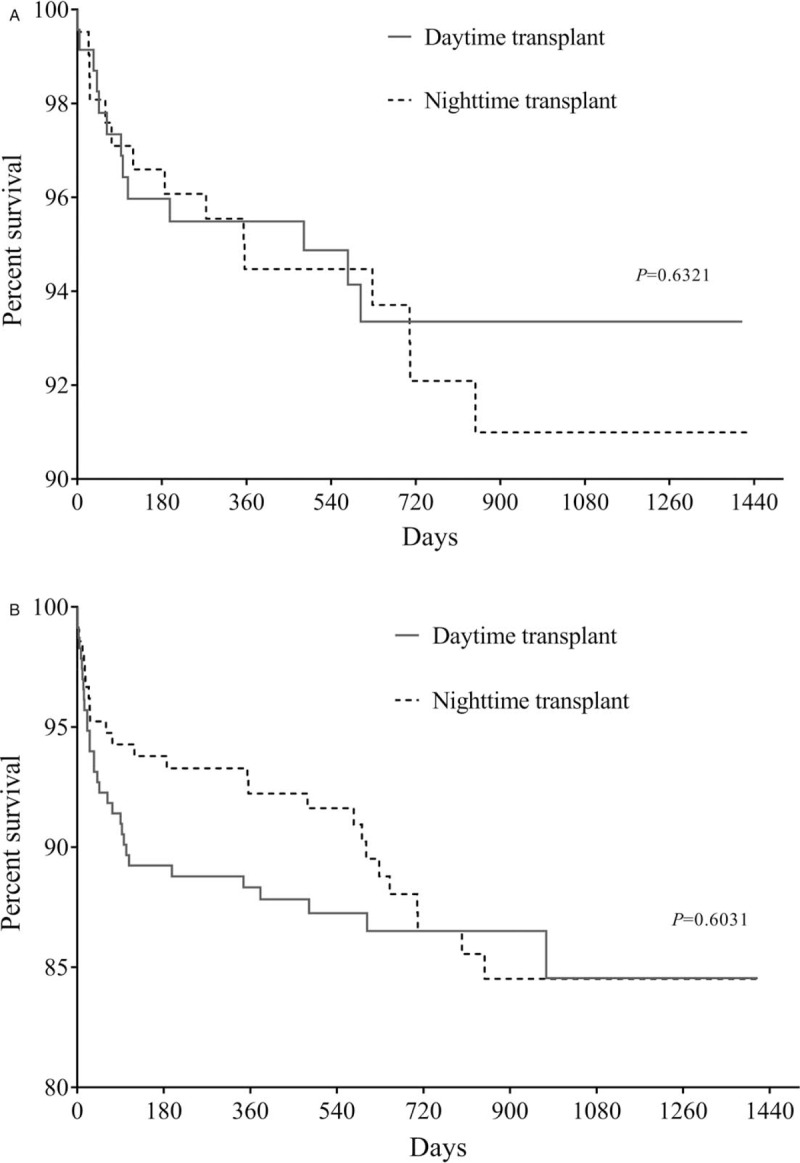
Recipient survival (A, log rank χ2 = 0.229, P = 0.632) and graft survival (B, log rank χ2 = 0.270, P = 0.603).
Figure 4.
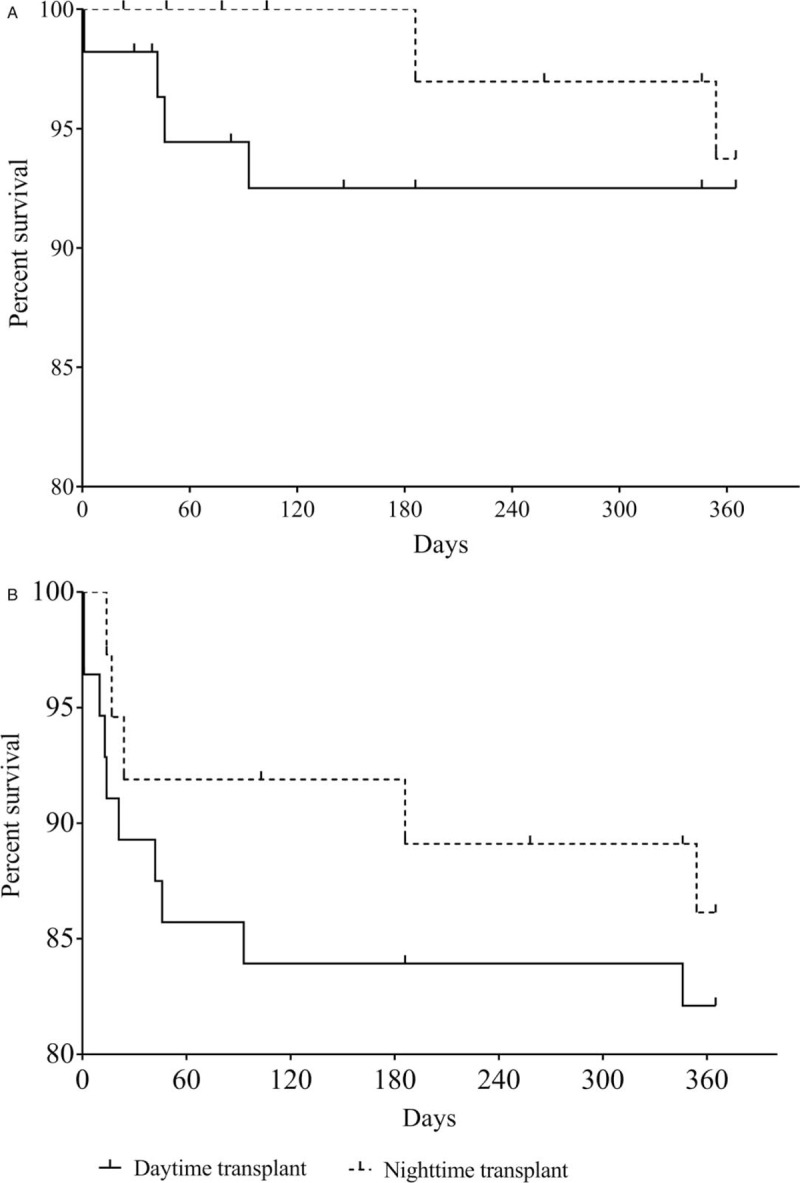
One-year survival of (A) recipients (χ2 = 0.135, P = 0.713) and (B) grafts (χ2 = 0.348, P = 0.555) from ECDs. ECD: Expanded criteria donor.
Table 3.
Cox regression analyses for recipients and grafts.
Discussion
Because of limited time for preservation of kidney grafts, kidney transplant is often an emergent operation to shorten CIT, which is considered as a key risk factor for DGF, AR and even survival in many researches.[1,2,9–13] Therefore, it has been common that kidney transplant was operated inevitably at off hours or night, especially with the number of deceased organ donation increasing in China.[5] Medical errors caused by fatigue or sleep deficiency were mostly occurred during surgical procedures, but their relationship with poor clinical outcomes and operative time was controversial.[1,14–17]
Organ procurement surgeries are usually performed during evening or night because decisions of potential organ donors and diagnosis of brain death are usually made during work hours.[18] Procedures before kidney transplantation including allocation, organ transport and recipient's preparation take much time.[19,20] Thus, 30% to 36% kidney transplantations started at nighttime (8 pm – 8 am),[1,21,22] which inevitably requires surgeons majoring in kidney transplant work for excessive duty hours. Some studies showed that sleep deprivation and fatigue result in reduced cognitive and psychomotor performance and risky decisions in doctors, drivers and pilots.[16,23,24] Moreover, 98,000 deaths resulted from medical errors annually from the report in the Institute of Medicine could be prevented.[25] It seems plausible that sleep loss and fatigue due to heavy workload may be risk factors in medical operations for surgeons. Evidences from kidney transplant, cardiothoracic, general and vascular surgeries showed that increased surgical complications were associated with after-hours or nighttime work.[16,17,22,26] However, 3 studies in kidney transplantation did not support the link between sleep deprivation and surgical complications,[1,27,28] in consistency with our results, but not with the finding of Brunschot et al[21] that less graft failure excluding non-surgical factors happened in nighttime transplant.
CIT plays a critical role in prognosis of graft and recipients in kidney transplant. In most transplant cases, 18-h-period has been considered as the safe cutoff of CIT.[1,10,29] In our cohort, although daytime transplant had significantly longer CIT, the longest CIT (16 hours) and median CIT (6 hours) were still shorter than the safe cutoff. In one hand, China has a vast territory and organ transportation largely, even completely depends on automobiles in some areas, which could lead to great variation in CIT at traffic congestion. On the other hands, China has donation policies superior to western countries for organ transplantation, which will greatly save the time spent in organ transportation. All donors in this study were from Shaanxi Province, which facilitated organ transportation and shortened CIT to some degree. Incidence of DGF in the daytime group with longer CIT did not differ significantly from that in the nighttime group (17.6% vs. 12.9%). Therefore, short CIT maybe an explanation for lower DGF incidence in our cohort than in other studies with mean CIT of 14.8 to 17.3 hours (15.35% vs. 31.1%–61.6%).[11,30] What's more, controlled DCD was performed under the circumstance that brain death was not approved by legislation in China, which had positive effects on outcome of grafts and recipients.[31]
As mentioned above, CIT limited within 18 hours would result in better outcomes. Because the longest CIT in our cohort was still shorter than 18 hours, the 2.5 hours longer CIT of the daytime group did not increase DGF and complications. Similarly, Seow et al[28] also showed that prolonged CIT did not increase the incidence of surgical complications. Besides, other studies also showed no difference in survival and complications between nighttime and daytime kidney transplants,[1,27,28] which is in discrepancy with the result of Brunschot et al[21] that less pure technical failure happened in the nighttime kidney transplant, which may had bias from experienced surgeons at night. However, studies have shown that nighttime work produced risks for patients in surgery[16,17,22] and bad effects on doctors with risk of breast cancer and obesity.[32,33] With the rapid increase in donors from citizen's death,[5] much more burden would be imposed upon transplant surgeons. Considering the issues above, it seems worthwhile to postpone transplant of organs with CIT <18 hours after elongation to the next day as a sub-emergent operation.
ESRD patients who accepted ECD kidney transplant had better outcome than those who were still in dialysis waiting for SCD even DCD kidney transplant.[8] In China, 20.99% ECD grafts were used in our transplant, which was roughly equivalent to 19% of the USA decade ago.[34] But at present, clinical use of ECD grafts has been increasing rapidly up to 43% in the United Kingdom and 50% in the USA.[8] Therefore, increasing ECDs seems an effective way to alleviate the dilemma of organ shortage in China. But actually, the majority of studies revealed worse graft survival and higher risks of DGF and AR in ECD kidney transplant.[8] Among the 47 factors associated with DGF, DCD donor, age of donor, Scr of donor, BMI of donor and recipient, cardiac function and dialysis duration of recipients were crucial.[12] HMP has been confirmed to have advantages such as offering nutrients, washing out byproducts and micro-thrombosis, and assessing graft viability according to machine parameters, which reduce DGF, AR and primary non-function.[35–40] In our center, HMP is applied to 78.78% of patients, which may be another reason to explain the low incidence of DGF. Although older donors with higher BMI had increased risk of DGF in the daytime group, HMP with protective effect on grafts was applied more in the daytime group, leading to explainable results of DGF and AR between the daytime and nighttime groups [Tables 4 and 5]. Moreover, ECD kidney transplant was often delayed to the following morning because of the poor perfusion parameters of Lifeport, indirectly leading to much longer CIT in the daytime group.
Table 4.
Characteristics of ECDs and recipients accepted ECD grafts.
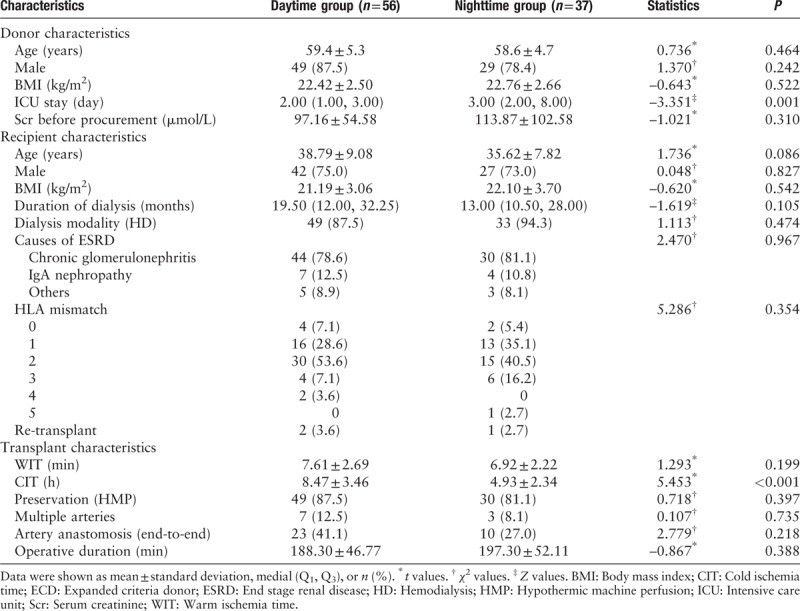
Table 5.
Outcomes of the recipients who accepted ECD grafts.
In our study, group assignment was based on both beginning and end of the operation, which was different from that of other kidney transplant cohorts, in which grouping merely depended on the beginning of the operation.[1,21,22] Elective surgery starts at 8 am on weekday, that is why we chose 8 am as the cutoff of the daytime group. The mean duration of operation in our cohort was 178 minutes, similar to about 3-h operative time in other 2 studies.[1,27] As a result, some operations started before 8 pm may continue to midnight and most operations were concluded in the period of 8 pm – 8 am Thus, the period beginning after 8 am and end before 8 pm could be more scientific for definition of daytime work from our point of view.
Our single-center retrospective study has some limitations. Some prospective studies are still needed to explore the relationship between clinical outcomes and nighttime transplant. The negative results in the association of nighttime transplant with poor clinical outcomes may be explained as follows. Firstly, the proportion of surgeons varied in each transplant, which was an indefinite factor for evaluating the impact of surgical technique between the daytime and nighttime work. Secondly, the degree of sleep deprivation for each surgeon was not described retrospectively. Rothschild et al[41] found that sleep less than 6 hours for a whole day would be detrimental for complications in surgical process. However, the duration of sleep for each surgeon was hard to know in the past. Surgeons for night surgery would always have a rest when they had obtained the reliable inform of transplant. Surgeons who stayed up late due to various reasons could take an unpredictable transplant on the next day and it was really complicated to evaluate fatigue. Thirdly, all operators were chief or vice-chief surgeons who have experienced decades’ training in kidney transplant. The beginning time of operation had little or minimal impacts on the outcome of surgeries. Meanwhile, they may have adapted to irregular work physiologically (including sleep or work at any time) to some extent. At last, due to the potential detriment of night work for doctors and patients, we have been attempting to delay transplant of some kidneys with short CIT to the following day, which explained why graft kidneys in the daytime group have significantly longer CIT than those in the nighttime group. In addition, some grafts perfused with unsatisfying parameters, especially from ECDs, were worthy to be perfused longer to achieve better perfusion,[42,43] which could explain why the mean age of donors in the daytime group significantly exceeded that in the nighttime group: that is, the proportion of ECDs was higher in the daytime group.
In conclusion, our results suggest that operation time of kidney transplant with short CIT has no significant impact on the outcome of kidney transplant. Because nighttime work predisposes adverse conditions to both doctors and patients, nighttime transplant of kidneys with short CIT could be postponed to the following day to alleviate burdens on medical staffs.
Conflicts of interest
None.
Footnotes
How to cite this article: Guo QH, Liu QL, Hu XJ, Li Y, Zheng J, Xue WJ. Comparison of nighttime and daytime operation on outcomes of kidney transplant with deceased donors: a retrospective analysis. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000056
References
- 1.Kienzl-Wagner K, Schneiderbauer S, Bösmüller C, Schneeberger S, Pratschke J, Ollinger R. Nighttime procedures are not associated with adverse outcomes in kidney transplantation. Transplant Int 2013; 26:879–885. [DOI] [PubMed] [Google Scholar]
- 2.Valdivia MAP, Gentil MA, Toro M, Cabello M, Rodriguez-Benot A, Mazuecos A, et al. Impact of cold ischemia time on initial graft function and survival rates in renal transplants from deceased donors performed in Andalusia. Transplant Proc 2011; 43:2174–2176. doi: 10.1016/j.transproceed.2011.06.047. [DOI] [PubMed] [Google Scholar]
- 3.Association CMD. Report of Occupational Status for Chinese Doctors. 2018. Accessed at http://www.cmda.net/rdxw2/11526.jhtml. [Google Scholar]
- 4.Cheng J, Tan T. What's the future of doctors in China? Stud Media Commun 2015; 3: doi: 10.11114/smc.v3i2.1151. [Google Scholar]
- 5.Sun QQ, Gao XP, Wang HB, Shiu-Chung Ko D, Li XC. A new era for organ transplantation in China. Lancet 2014; 383:1971–1972. doi: 10.1016/S0140-6736(14)60953-3. [DOI] [PubMed] [Google Scholar]
- 6.Sui W, Zheng C, Yang M, Dai Y. Organ donation in China: current status, challenges, and future development. Prog Transplant 2014; 24:375–380. doi: 10.7182/pit2014730. [DOI] [PubMed] [Google Scholar]
- 7.Xiaoming P, Xiang H, LinJuan L, Chenguang D, Li R. Preliminary results of transplantation with kidneys donated after cardiac death: a path of hope for organ transplantation in China. Nephrol Dial Transplant 2015; 30:1590–1596. doi: 10.1093/ndt/gfv049. [DOI] [PubMed] [Google Scholar]
- 8.Pérez-Sáez MJ, Montero N, Redondo-Pachón D, Crespo M, Pascual J. Strategies for an expanded use of kidneys from elderly donors. Transplantation 2017; 101:727–745. doi: 10.1097/TP.0000000000001635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SM, Ahn S, Min SI, Park D, Park T, Min SK, et al. Cold ischemic time is critical in outcomes of expanded criteria donor renal transplantation. Clin Transplant 2013; 27:132–139. doi: 10.1111/ctr.12034. [DOI] [PubMed] [Google Scholar]
- 10.Barba J, Zudaire JJ, Robles JE, Tienza A, Rosell D, Berián JM, et al. Is there a safe cold ischemia time interval for the renal graft? Actas Urol Esp 2011; 35:475–480. [DOI] [PubMed] [Google Scholar]
- 11.Tugmen C, Sert I, Kebabci E, Murat Dogan S, Tanrisev M, Alparslan C, et al. Delayed graft function in kidney transplantation: risk factors and impact on early graft function. Prog Transplant 2016; 26:172–177. doi: 10.1177/1526924816640978. [DOI] [PubMed] [Google Scholar]
- 12.Nashan B, Abbud-Filho M, Citterio F. Prediction, prevention, and management of delayed graft function: where are we now? Clin Transplant 2016; 30:1198–1208. doi: 10.1111/ctr.12832. [DOI] [PubMed] [Google Scholar]
- 13.Debout A, Foucher Y, Trebern-Launay K, Legendre C, Kreis H, Mourad G, et al. Each additional hour of cold ischemia time significantly increases the risk of graft failure and mortality following renal transplantation. Kidney Int 2015; 87:343–349. doi: 10.1038/ki.2014.304. [DOI] [PubMed] [Google Scholar]
- 14.Chan YM, Tang N, Chow SK. Surgical outcome of daytime and out-of-hours surgery for elderly patients with hip fracture. Hong Kong Med J 2018; 24:32–37. doi: 10.12809/hkmj165044. [DOI] [PubMed] [Google Scholar]
- 15.Heller JA, Kothari R, Lin HM, Levin MA, Weiner M. Surgery start time does not impact outcome in elective cardiac surgery. J Cardiothorac Vasc Anesth 2017; 31:32–36. [DOI] [PubMed] [Google Scholar]
- 16.Komen N, Dijk JW, Lalmahomed Z, Klop K, Hop W, Kleinrensink GJ, et al. After-hours colorectal surgery: a risk factor for anastomotic leakage. Int J Colorectal Dis 2009; 24:789–795. doi: 10.1007/s00384-009-0692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kelz RR, Tran TT, Hosokawa P, Henderson P, Henderson W, Paulson E, et al. Time-of-day effects on surgical outcomes in the private sector: a retrospective cohort study. J Am Coll Surg 2009; 209:434–445. e432. doi: 10.1016/j.jamcollsurg.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 18.Vacher-Coponat H, Purgus R, Indreies M, Moal V, Luciani H, Lechevallier E, et al. Cold ischemia time in renal transplantation is reduced by a timesheet in a French transplant center. Transplantation 2007; 83:561–565. doi: 10.1097/01.tp.0000253757.14344.7f. [DOI] [PubMed] [Google Scholar]
- 19.Domínguez J, Lira F, Troncoso P, Aravena C, Ortiz M, Gonzalez R. Factors that predict duration of delayed graft function in cadaveric kidney transplantation. Transplantation Proc 2009; 41:2668–2669. doi: 10.1016/j.transproceed.2009.06.076. [DOI] [PubMed] [Google Scholar]
- 20.Wolfbrandt A, Lindström K, Mjörnstedt L, Friman S, et al. What are we waiting for? Analyses of factors influencing cold ischemia time. Transplantation Proc 2010; 42:4436–4437. doi: 10.1016/j.transproceed.2010.09.109. [DOI] [PubMed] [Google Scholar]
- 21.Brunschot DM, Hoitsma AJ, van der Jagt MF, d’Ancona FC, Donders RA, van Laarhoven CJ, et al. Nighttime kidney transplantation is associated with less pure technical graft failure. World J Urol 2016; 34:955–961. doi: 10.1007/s00345-015-1679-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fechner G, Pezold C, Hauser S, Gerhardt T, Müller SC. Kidney's nightshift, kidney's nightmare? Comparison of daylight and nighttime kidney transplantation: impact on complications and graft survival. Transplant Proc 2008; 40:1341–1344. doi: 10.1016/j.transproceed.2008.02.072. [DOI] [PubMed] [Google Scholar]
- 23.Goel N, Rao H, Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol 2009; 29:320–339. doi: 10.1055/s-0029-1237117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.George TJ, Arnaoutakis GJ, Merlo CA, Kemp CD, Baumgartner WA, Conte JV, et al. Association of operative time of day with outcomes after thoracic organ transplant. JAMA 2011; 305:2193–2199. doi: 10.1001/jama.2011.726. [DOI] [PubMed] [Google Scholar]
- 25.Maurette P, Sfa CAMR. To err is human: building a safer health system. Ann Fr Anesth 2002; 21:453–454. doi: Unsp S0750765802006706/Edi Doi 10.1016/S0750-7658(02)00670-6. [DOI] [PubMed] [Google Scholar]
- 26.Thomas M, Allen MS, Wigle DA, Shen KR, Cassivi SD, Nichols FC, et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg 2012; 94:966–973. doi: 10.1016/j.athoracsur.2012.04.099. [DOI] [PubMed] [Google Scholar]
- 27.Shaw TM, Lonze BE, Feyssa EL, Segev DL, May N, Parsikia A, et al. Operative start times and complications after kidney transplantation. Clin Transplant 2012; 26:E177–E183. doi: 10.1111/j.1399-0012.2012.1622.x. [DOI] [PubMed] [Google Scholar]
- 28.Seow YY, Alkari B, Dyer P, Riad H. Cold ischemia time, surgeon, time of day, and surgical complications. Transplantation 2004; 77:1386–1389. doi: 10.1097/01.Tp.0000122230.46091.E2. [DOI] [PubMed] [Google Scholar]
- 29.Opelz G, Dohler B. Multicenter analysis of kidney preservation. Transplantation 2007; 83:247–253. doi: 10.1097/01.tp.0000251781.36117.27. [DOI] [PubMed] [Google Scholar]
- 30.Jochmans I, Moers C, Smits JM, Leuvenink HG, Treckmann J, Paul A, et al. Machine perfusion versus cold storage for the preservation of kidneys donated after cardiac death: a multicenter, randomized, controlled trial. Ann Surg 2010; 252:756–764. doi: 10.1097/SLA.0b013e3181ffc256. [DOI] [PubMed] [Google Scholar]
- 31.Xue W, Tian P, Xiang H, Ding X, Pan X, Yan H, et al. Outcomes for primary kidney transplantation from donation after Citizens’ death in China: a single center experience of 367 cases. BMC Health Serv Res 2017; 17:250.doi: 10.1186/s12913-017-2190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Theorell T, Akerstedt T. Day and night work: changes in cholesterol, uric acid, glucose and potassium in serum and in circadian patterns of urinary catecholamine excretion. A longitudinal cross-over study of railway workers. J Inter Med 2010; 200:47–53. doi: 10.1111/j.0954-6820.1976.tb08194.x. [DOI] [PubMed] [Google Scholar]
- 33.Jia Y, Lu Y, Wu K, Lin Q, Shen W, Zhu M, et al. Does night work increase the risk of breast cancer? A systematic review and meta-analysis of epidemiological studies. Cancer Epidemiol 2013; 37:197–206. doi: 10.1016/j.canep.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 34.Schold JD, Hall YN. Enhancing the expanded criteria donor policy as an intervention to improve kidney allocation: is it actually a ‘net-zero’ model? Am J Transplant 2010; 10:2582–2585. doi: 10.1111/j.1600-6143.2010.03320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taylor MJ, Baicu SC. Current state of hypothermic machine perfusion preservation of organs: the clinical perspective. Cryobiology 2010; 60 3 Suppl:S20–S35. doi: 10.1016/j.cryobiol.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jiao B, Liu S, Liu H, Cheng D, Cheng Y, Liu Y. Hypothermic machine perfusion reduces delayed graft function and improves one-year graft survival of kidneys from expanded criteria donors: a meta-analysis. PLoS One 2013; 8:e81826.doi: 10.1371/journal.pone.0081826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deng R, Gu G, Wang D, Tai Q, Wu L, Ju W, et al. Machine perfusion versus cold storage of kidneys derived from donation after cardiac death: a meta-analysis. PLoS One 2013; 8:e56368.doi: 10.1371/journal.pone.0056368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pan X, Xue W, Liu L, Xiang H, Ding C, He S, et al. Donations after cardiac death kidney transplantation in northwest China (in Chinese). J Southern Med Univ 2014; 34:414–418. [PubMed] [Google Scholar]
- 39.Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, Napieralski BP, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med 2009; 360:7–19. doi: 10.1056/NEJMoa0802289. [DOI] [PubMed] [Google Scholar]
- 40.Lo Faro ML, Akhtar MZ, Boffa C, Ploeg R. Should pulsatile preservation be the gold standard in kidney transplantation? Curr Transplant Rep 2015; 2:105–112. doi: 10.1007/s40472-015-0063-8. [Google Scholar]
- 41.Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, et al. Risks of complications by attending physicians after performing nighttime procedures. Jama-J Am Med Assoc 2009; 302:1565–1572. doi: DOI 10.1001/jama.2009.1423. [DOI] [PubMed] [Google Scholar]
- 42.Stratta RJ, Moore PS, Farney AC, Rogers J, Hartmann EL, Reeves-Daniel A, et al. Influence of pulsatile perfusion preservation on outcomes in kidney transplantation from expanded criteria donors. J Am Coll Surg 2007; 204:873–882. [DOI] [PubMed] [Google Scholar]
- 43.Matsuoka L, Shah T, Aswad S, Bunnapradist S, Cho Y, Mendez RG, et al. pulsatile perfusion reduces the incidence of delayed graft function in expanded criteria donor kidney transplantation. Am J Transplant 2010; 6:1473–1478. [DOI] [PubMed] [Google Scholar]


