The concept of brain death was 1st introduced in the 1960s, providing an essential conceptual change to medical practice,[1] and its diagnosis is based on demonstrating the complete, irreversible cessation of brainstem function. Despite medical advancement, organ transplantation remains the only hope for patients with end-stage organ failure to survive, and donation after brain death remains a main source of organs. A lack of deceased organ donors is one of the greatest obstacles to transplantation, and it remains a particular problem in the Chinese population. In 2016, the proportion of organ donors in mainland China is 3 per million population (pmp), and the number of deceased donors in Hong Kong, China in 2017 is 6 donors pmp, which are relatively low.[2] More aggressive neurosurgical intervention and better trauma and critical care management have also contributed to a substantial reduction in the number of potential organ donors. At the same time, transplant techniques are more mature, and transplantations are now offered to a group of “older and sicker” patients who were considered unsuitable recipients in the past. Every day, around 300,000 people across mainland China and more than 2000 patients in Hong Kong, China are waiting for organ transplants. Multiple studies have attempted to examine the continuing supply-demand imbalance by investigating potential influences on organ procurement, including individual cultural beliefs, beliefs about government policy, and beliefs about the health care system.[3–5] We reported a pilot cross-sectional study surveying 520 visitors at local intensive care units (ICUs) from 2014 to 2016, and their views toward the 3 aspects were investigated. Visitors under the age of 18 years were excluded. Ethics approval was granted by the relevant Research Ethics Committees.
Research has shown that donation readiness depends on cultural surroundings.[4] One of the explanations for organ shortage in the Chinese society is attributed to the Taoist and Buddhist philosophies of afterlife and sanctity of human body, which promotes keeping a body intact after death. With higher level education and Western influences, the current generation holds this traditional belief less strongly, and 61% of the study population showed a positive attitude toward the idea of body disfigurement. Meanwhile, although 94% of the participants indicated that they support organ donation, only 66% were willing to donate their organs after death [Supplementary Table 1]. This discrepancy warrants further investigation to identify factors that could be targeted in future campaigns aimed at improving organ donation rates.
Death anxiety is a general term that represents a cluster of death attitudes and is characterized by negative psychologic reactions. After-death fear and death anxiety is prevalent in the Chinese population, discussion about death or death-related issues is avoided in fear of misfortune, lowering the likelihood of talks about organ donation among family members. A previous study showed that up to one-third of the elderly Chinese population felt uncomfortable and nervous when other people talked about death.[6] In this study, only 26% of participants had ever talked to others about organ donation. Even among those who were willing to donate their organs after death, more than half (64.7%) had never conveyed their intention.
In Hong Kong, China, an “opt-in” (explicit consent, that is, only those who have given explicit consent will be donors) system was implemented in 1968. The issues of an “opt-out” (presumed consent, that is, anyone who has not clearly refused is presumed a donor) system were debated in the Legislative Council in 1998, and a final decision was made to maintain the status quo. In 2017, the Hong Kong government surveyed public views on an opt-out system and reconsidered its legislation. The population-wide survey revealed that only 33.8% supported the implementation of an opt-out system and 35.9% opposed it.[7] Based on such inconclusive finding, the existing system has remained in place, there is a need to increase public readiness before introducing an opt-out system.
The requirement of consent is another aspect of governmental policy. In Hong Kong, China, the need for familial consent to organ donation has created hurdles – including the need to reach consensus among family members, the fact that family members do not know the wishes of the deceased, and the unwillingness of relatives to make decisions on behalf of the deceased.[8] More significantly, there have been instances where patients’ consents for organ donation were posthumously overruled by their families. Data from the current study showed that 82% of the participants were unwilling to consent to organ donation on behalf of their relatives who were confirmed brain dead, with the commonest reason (91.3%) being the lack of prior approval or knowledge of the deceased one's wishes as shown in Supplementary Table 2. The relative inaccessibility to verify one's status as an organ donor in the Centralized Organ Donation Register (CODR), and the overriding status of familial consent even if the deceased patient had explicitly expressed consent have created additional hurdles. Initiatives by the government such as formal documentation of one's wish to donate organs and tissues on the identity card by designating words like “Organ Donor” may help to relieve familial anxiety in the consent process.
Public education is an important means to change attitudes toward organ donation. In the current survey, more than 90% of participants felt that government promotion and public support of organ donation were insufficient. As of April 2018, there were 282,572 names on the CODR in Hong Kong, China, which is only 3.8% of the entire population of 7.4 million. The Hong Kong government is in a leading role to promote organ donation and increase persuasiveness by health message framing.[9] The effective framing of health-related communications can elicit positive attitudes and influence decision-making.[10] The government recently established the Garden of Life to recognize the charitable acts of organ donors and their families, and to symbolize the continuation of life and kindling of hope. It also set up a Committee on the Promotion of Organ Donation to promote public discussion on the topic. A local study showed a proposed “opt-in system with organ allocation priority” may significantly increase willingness for deceased organ donation.[11] Other studies have shown that an “opt-out system with a priority system” may provide a dual-incentive for donation,[12] but this option has not been explored locally.
Finally, the awareness and promotion of organ donation should be enhanced by health care workers. Failure of health care professionals to identify potential donors is considered a major factor leading to the loss of potential organ donors.[13] A unique feature in Hong Kong, China, is that most potential deceased organ donors are identified from non-ICU wards.[13] A recent local study showed that only half of the possible organ donors were identified and referred to corresponding parties, and that one-third of unutilized potential organ donors were lost in non-ICU areas due to unstable hemodynamics or failure to complete a brain death diagnosis.[13] Previous studies showed that initiation of end-of-life care in acute settings and lack of knowledge and experience in organ donation practices outside ICUs could result in under-recognition of up to 34% potential donors.[14] Enhancing the sensitivity of frontline health care workers to identifying potential donors, and improving the support to the care of these patients may increase the organ donation rate.[15]
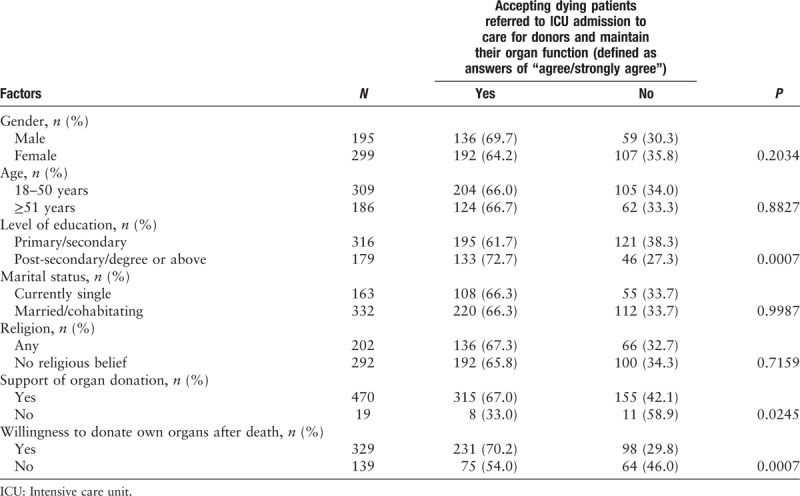
There is increasing recognition of the role of early involvement of intensive care personnel in the care of potential organ donors. Faced with inadequate health care resources, admission to the ICU traditionally occurs in the setting of acute illness with the aim to survive. There is a concern over the appropriateness and quality of palliative care provided in an ICU. Until now, there has been little information about the view of the general public regarding the utilization of scarce ICU resources for the management of potentially brain dead patients. Table 1 demonstrates the potential factors that would affect an individuals’ acceptance of referring dying patients to ICU for donor care and organ procurement. The current study showed that people accept the admission of dying patients to the ICU for various organ donation-related purposes, including the exploration and evaluation of potential organ donors (39.4%), diagnosis of brain death (58.8%), donor organ procurement (63.1%), and obtaining proxy consent for organ donation (55.2%). A proportion of participants showed a neutral response (28.7–40.8%) in this regard as shown in Supplementary Table 3. Among those who indicated the views, the acceptance of ICU admission for donor care and organ procurement was especially notable in those with a higher level of education (post-secondary or above 72.7% vs secondary or below 61.7%, P = 0.0007) [Table 1]. Personal support of organ donation and willingness to donate own organs after death were also significant factors (P = 0.0007 and 0.0245, respectively). The levels of support shown by different gender and age groups were broadly similar. Moreover, a recent study showed that this group of patients tended to have shorter ICU stays, resulting in more quality-adjusted life-years per ICU bed-day than patients admitted for management of acute illnesses, suggesting that ICU resource for this purpose may not be inappropriate.[16] These promising findings form the basis of the implementation of palliative care services and end-of-life care into routine ICU workflow. Further insights will be provided by an international multi-center study “ETHICUS II” investigating the end-of-life practices in ICUs around the world.
Table 1.
Univariate analysis of potential factors for acceptance of referring dying patients to ICU to care for donors and maintain their organ function
In conclusion, the organ donation rate has remained low in Hong Kong, China, despite continuing efforts from the government to promote organ donation. Two significant contributory factors have been identified: the attitudes of the general population, and the shortcomings of the hospital system in effective management of potential donors. While cultural beliefs and death anxiety are substantial obstacles, government-led initiatives or even legislation may facilitate identification of willing organ donors and simplify the consent process for the family. From an economic point of view, the role of palliative care and donor organ procurement in the ICU should be recognized. Further studies on the cost-effectiveness of public education methodologies and health care resource utilization are warranted.
Acknowledgements
The authors would like to thank Clinical Trials Center, The University of Hong Kong for analyzing database for this study.
Conflicts of interest
None.
Author contributions
Access to data and data analysis: Drs. Tsai NW and Chan WM had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Tsai CW, Koo J, Chan WM. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: Tsai CW, Ng PY. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: Tsai CW, Ng PY, Chan WM. Administrative, technical, or material support: Ng PY, Liong T, Lee SF, Ngai CW, Sin WC. Study supervision: Ng PY, Chan WM.
Supplementary Material
Footnotes
How to cite this article: Tsai NW, Leung YM, Ng PY, Liong T, Lee SF, Ngai CW, Sin WC, Koo J, Chan WM. Attitudes of visitors at adult intensive care unit toward organ donation and organ support. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000059
References
- 1.Wijdicks EF. The diagnosis of brain death. N Engl J Med 2001; 344 16:1215–1221. doi: 10.1056/NEJM200104193441606. [DOI] [PubMed] [Google Scholar]
- 2.International Registry in Organ Donation and Transplantation, 2017. Available from: http://www.irodat.org/ [Last accessed April 19, 2018]. [Google Scholar]
- 3.Randhawa G. Death and organ donation: meeting the needs of multiethnic and multifaith populations. Br J Anaesth 2012; 108 (Suppl 1):i88–i91. doi: 10.1093/bja/aer385. [DOI] [PubMed] [Google Scholar]
- 4.Cai Y. On the impacts of traditional Chinese culture on organ donation. J Med Philos 2013; 38:149–159. doi: 10.1093/jmp/jht007. [DOI] [PubMed] [Google Scholar]
- 5.Wu Y, Elliott R, Li L, Yang T, Bai Y, Ma W. Cadaveric organ donation in China: a crossroads for ethics and sociocultural factors. Medicine (Baltimore) 2018; 97 10:e9951.doi: 10.1097/MD.0000000000009951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu AM, Tang CS, Kwok TC. Death anxiety among Chinese elderly people in Hong Kong. J Aging Health 2002; 14 1:42–56. doi: 10.1177/089826430201400103. [DOI] [PubMed] [Google Scholar]
- 7.Thematic Household Survey Report - Report No. 63, 2017. Available from: https://www.statistics.gov.hk/pub/B11302632017XXXXB0100.pdf [Last accessed October 30, 2018]. [Google Scholar]
- 8.Yeung I, Kong SH, Lee J. Attitudes towards organ donation in Hong Kong. Soc Sci Med 2000; 50:1643–1654. doi: 10.1016/S0277-9536(99)00393-7. [DOI] [PubMed] [Google Scholar]
- 9.Chien YH, Chang WT. Effects of message framing and exemplars on promoting organ donation. Psychol Rep 2015; 117:692–702. doi: 10.2466/01.PR0.117c25z7. [DOI] [PubMed] [Google Scholar]
- 10.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol Bull 1997; 121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- 11.Cheung TK, Cheng TC, Wong LY. Willingness for deceased organ donation under different legislative systems in Hong Kong: population-based cross-sectional survey. Hong Kong Med J 2018; 24:119–127. doi: 10.12809/hkmj176831. [DOI] [PubMed] [Google Scholar]
- 12.Zuniga-Fajuri A. Increasing organ donation by presumed consent and allocation priority: Chile. Bull World Health Organ 2015; 93:199–202. doi: 10.2471/BLT.14.139535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung CY, Pong ML, Au Yeung SF, Chau KF. Factors affecting the deceased organ donation rate in the Chinese community: an audit of hospital medical records in Hong Kong. Hong Kong Med J 2016; 22:570–575. doi: 10.12809/hkmj164930. [DOI] [PubMed] [Google Scholar]
- 14.Witjes M, Kotsopoulos A, Herold IHF, Otterspoor L, Simons KS, van Vliet J, et al. The influence of end-of-life care on organ donor potential. Am J Transplant 2017; 17:1922–1927. doi: 10.1111/ajt.14286. [DOI] [PubMed] [Google Scholar]
- 15.Ramadurg UY, Gupta A. Impact of an educational intervention on increasing the knowledge and changing the attitude and beliefs towards organ donation among medical students. J Clin Diagn Res 2014; 8:JC05–JC07. doi: 10.7860/JCDR/2014/6594.4347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melville A, Kolt G, Anderson D, Mitropoulos J, Pilcher D. Admission to intensive care for palliative care or potential organ donation: demographics, circumstances, outcomes, and resource use. Crit Care Med 2017; 45:e1050–e1059. doi: 10.1097/CCM.0000000000002655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


