Abstract
Background:
Growing industrialization of China exposes its labor population to the risk of musculoskeletal disorders (MSDs). This study aimed to investigate the prevalence and risk factors of MSDs in a modern industrial region of Beijing.
Methods:
A cross-sectional study included 1415 employees in six industrial companies was conducted between January 2018 and May 2018 in Fangshan district, Beijng, China. Nordic Musculoskeletal Questionnaire (NMQ) was used to collect the information about MSDs. Demographic factors, lifestyle factors, health and medical factors, and work-related factors were collected as independent variables. Descriptive statistics, the chi-squared (χ2) test, and binary logistic regression analysis were used to analyze data.
Results:
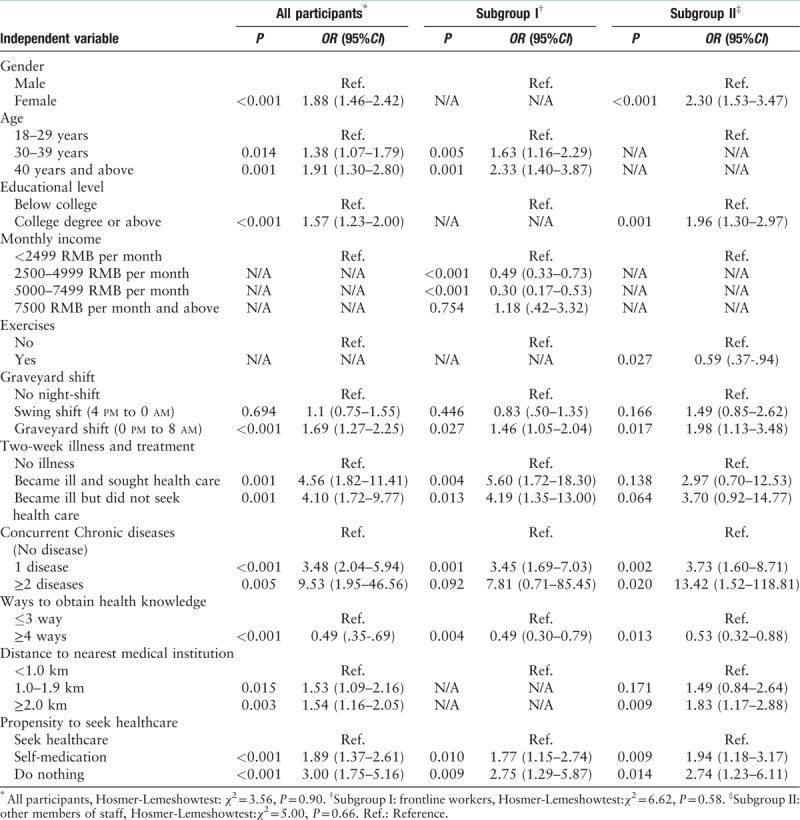
Among 1415 participants, 498 reported MSDs. The regions involved were the neck (25.16%), shoulders (17.17%), and upper back (13.29%). There was a significant statistical difference between frontline industrial workers and other staff in the prevalence of self-reported symptoms involving the shoulders (χ2 = 4.33, P = 0.037), wrists and hands (χ2 = 8.90, P = 0.003), and ankles and feet (χ2 = 12.88, P < 0.001). Increased age (P = 0.005, OR = 1.63; P = 0.001, OR = 2.33), a high or a low salary (P < 0.001, OR = 0.49; P < 0.001, OR = 0.30), night-shift (P = 0.027, OR = 1.46), two-week-history of illness and treatment (P = 0.004, OR = 5.60; P = 0.013, OR = 4.19), concurrent chronic diseases (P = 0.001, OR = 3.45; P = 0.092, OR = 7.81), limited access to health information (P = 0.004, OR = 0.49), and negative attitude towards seeking healthcare (P = 0.010, OR = 1.77; P = 0.009, OR = 2.75) were associated with MSDs in frontline workers. Female gender (P < 0.001, OR = 2.30), high education (P = 0.001, OR = 1.96), no exercises (P = 0.027, OR = 0.59), night-shift (P = 0.017, OR = 1.98), concurrent chronic diseases (P = 0.002, OR = 3.73; P = 0.020, OR = 13.42), limited access to health information (P = 0.013, OR = 0.53), far distance to medical institution (P = 0.009, OR = 1.83), and negative propensity (P = 0.009, OR = 1.94; P = 0.014, OR = 2.74) were associated with MSDs in other staffs.
Conclusions:
The prevalence of MSDs among industrial employees has changed. Frontline workers had different prevalence and risk factors for MSDs compared with other employees. Negative propensity to healthcare, limited ways to obtain health knowledge, and concomitant chronic diseases were associated with MSDs. Surprisingly, highly educated and high-income employees had a higher risk of MSDs.
Keywords: Cross-sectional study, Musculoskeletal disorders, Occupational injuries, Epidemiology
Introduction
Worldwide, musculoskeletal disorders (MSDs) commonly account for work-related health problems among industrial workers and include a wide range of inflammatory and degenerative changes affecting the joints, muscles, tendons, ligaments, nerves, and vessels.[1,2] MSDs inflict a broad range of damage upon the individual, the family unit, and the countries involved.[1] MSDs result in disability or reduced quality of life,[3] medical leave or a reduced work performance,[4] and large medical expenditure for the individual and the state.[5]
Several risk factors have been reported to be associated with MSDs among workers. Increased age and female gender have been reported to be significant risk factors for MSDs.[6,7] Smokers, and people who are overweight, also have an increased risk of MSDs.[8,9] Lower socioeconomic status, including reduced education, income, and occupation, are also associated with MSDs.[10,11] Work-related factors, including night-shifts,[12] job tenure,[7,13] and physical exposure in the working environment are also known risk factors of MSD.[14,15] Recent papers have also shown that exposure to computers and mobile phones will increase the risk of MSDs.[3,16] The impact of MSDs can be reduced by the implementation of prevention programs,[17] including ergonomic interventions[18] and physical activity.[19,20] However, the use of mechanical supports and other physical interventions are ineffective.[19] Unplanned general physical exercise is not effective[20] and excessive exercise can be counterproductive.[21] Multifactor interventions, based on a risk assessment program are most likely to be successful.[22] Therefore, it is important to assess the individual risk factors of developing MSDs prior to implementing an integrated injury prevention program.
In 2010, China overtook the United States of America and become the largest manufacturing economy and exporter of goods in the world.[23] However, growing industrialization in China exposes the labor population to the risk of work-related injuries. The prevalence of MSDs in Chinese industrial employees is high.[13,24] Recently, China's industry has witnessed several transformations to involve modern, green, intelligent, and automated processes; this is particularly the case in Beijing.[25] Previous studies have been conducted in traditional industrial areas of China, but few previous studies have made a distinction between, or compared, the prevalence and risk factors of MSDs between frontline workers and office or support industry personnel.
Therefore, this study aimed to investigate the prevalence and risk factors of MSDs in a modern industrial region of Beijing. A cross-sectional study was undertaken which included 1415 industrial employees from six equipment manufacturing companies; all of these employees completed health questionnaires.
Methods
Ethical approval
The study was approved by the Ethical Committee of Capital Medical University, Beijing, China. Because this study was an electronic survey, there was no requirement for written informed consent.
Study sites and sampling procedures
A cross-sectional study was conducted between January 2018 and May 2018 in Fangshan district. Located in southwest Beijing, Fangshan district is one of Beijing's key industrial regions, and has formed an industrial cluster that includes 3702 industrial enterprises and has generated more than 29 billion Chinese Yuan (RMB).[26]
For a variety of reasons, we used non-random sampling to select the companies. Firstly, this was because of the unknown sampling framework. Both Beijing Administration for Industry and Commerce and Beijing Bureau of Statistics were unable to provide a list of industrial companies in Fangshan district, Beijing, China. Secondly, we were unable to ascertain the operating conditions of many companies. Many companies were not in production. As a result, purposive sampling was used to select the companies to be involved in this study. In choosing the companies, we considered several factors: equipment manufacturing, production stability and a willingness to participate in the study. Finally, six modernized industrial companies were selected. We studied and compared frontline workers (production workers who engaged in processing material product) and other staffs (people who engaged in non-production work, including office staff who worked in financial management, operational and administrative technicians who engaged in engineering technology and support personal who engaged in logistics and security) from all companies. The study inclusion criteria included work experience of more than six months, and an age between 18 and 60 years. Subjects were excluded if they had undertaken long-term work outside of their company (for example long-term business trips and long-term stationing outside of the company) or refused to participate in the study.
Electronic study questionnaires
This study used electronic self-reported questionnaires to collect data from study participants. The self-reported questionnaires are commonly used in this field and some researchers believe that this practice is more informative than physical examinations, as subjective measures are better able to capture impact upon an individual.[1] Self-reported weight has also been demonstrated to be a valid measure of body mass.[27] Data from the completed questionnaires were reviewed by the authors prior to analysis. In total, 1680 employees were selected to engage in this study; 1550 questionnaires were recovered, of which 1415 were valid questionnaires.
The questionnaire consisted of two parts. The first part of the electronic questionnaire consisted of questions related to individual demographic factors, including gender, age, and body mass index (BMI) in kg/m2 (there were unified instruments to measure weight and height on the spot), educational level, monthly income (during the last 12 months), and whether the individual had Urban Employees’ Basic Medical Insurance (UEBMI). We also recorded lifestyle factors, including smoking history, a history of regular exercise (frequency of once a week or more, and exercise intensity associated with increased heart rate). Health and medical factors included a history of illness two weeks previously, the number of additional chronic diseases (diagnosed by a doctor, and excluding MSDs), a propensity to seek health care, ways to obtain health information, and the distance from their place of residence to the nearest medical institution. Work-related factors included night-shift work (during the past 12 months), and job tenure (current profession). The second part of the questionnaire included the Nordic Musculoskeletal Questionnaire (NMQ), which is a standard instrument for analyzing MSDs.[28] A Chinese version of the NMQ has been developed and has previously been shown to have good reliability and validity.[29] The NMQ consists of questions relating to musculoskeletal problems during the previous 12 months in nine anatomical areas of the human body (neck, shoulders, upper back, elbows, wrists/hands, lower back, hips/thighs, knees, and ankles/feet). Only a “yes” or “no” answer was required with regard to feeling any pain or discomfort in these regions.
Data analysis
The data from the study questionnaires were recorded using Excel spreadsheets and then analyzed using the Statistical Package of Social Sciences (SPSS) version 22 software (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to explore the individual characteristics of all employees surveyed. The chi-squared (χ2) test was performed to compare differences between the two study groups, the frontline workers and other staff. Binary logistic regression analysis was used to evaluate the independent effect of each variable on MSDs. The Hosmer-Lemeshow statistical test for goodness of fit in logistic regression models was used for its predictive (risk) value. The odds ratio (OR) was calculated to determine the strength of the association between dependent variables and independent variables (or covariates) with a 95% confidence interval (CI). A value of P < 0.05 was considered to represent statistical significance.
Results
General characteristics of the study participants
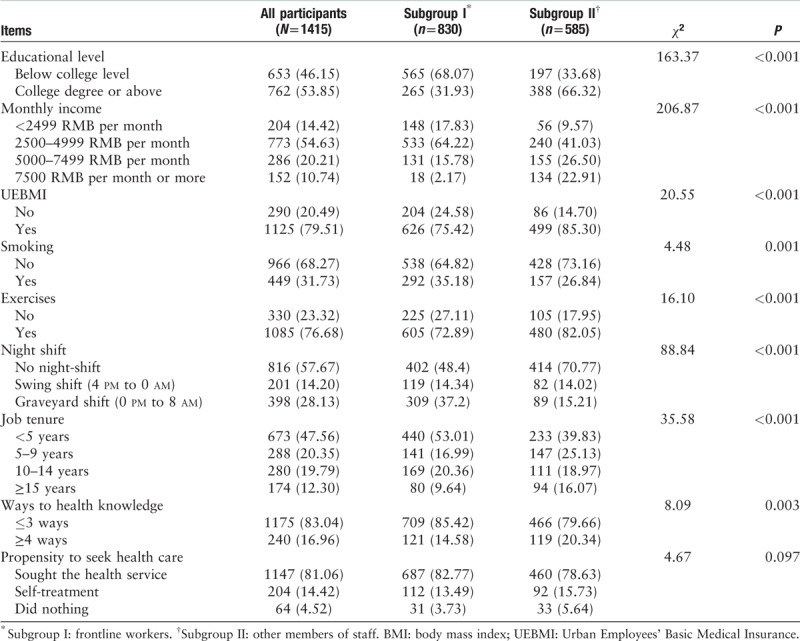
In total, 736 (52.01%) of the 1415 participants were male. The mean age was 31.8 ± 7.3 years (range: 18–60 years). Five hundred and fifty-seven subjects (39.36%) were 18 to 29 years of age, and 682 (48.20%) were aged 30 to 39 years. In 121 subjects (8.55%), BMI was below 18.5 kg/m2; in 744 subjects (52.58%) BMI was 18.5 to 23.9 kg/m2, in the remaining subjects, BMI exceeded 24 kg/m2. Most of the subjects (1358; 95.97%) reported no illness during the two weeks prior to completing the questionnaire, while 29 subjects (2.05%) became ill and sought health care and 28 subjects (1.98%) became ill but did not seek health care. Most subjects (1331; 94.06%) had no chronic disease. There were no significant differences in terms of gender, age, BMI, two-week and chronic diseases, distance to nearest medical institution and propensity to seek healthcare between frontline workers and other staff. Frontline workers had a lower educational level (χ2 = 163.37, P < 0.001), lower monthly income (χ2 = 206.87, P < 0.001), lower Urban Employee Basic Medical Insurance (UEBMI) rate (χ2 = 20.55, P < 0.001), did less exercise (χ2 = 16.10, P < 0.001), had shorter job tenure (χ2 = 35.58, P < 0.001), and more limited access to health information (χ2 = 8.09, P < 0.001) compared with other staff, and also had a higher rate of smoking (χ2 = 4.48, P = 0.001) and night-shift work (χ2 = 88.84, P < 0.001) [Table 1].
Table 1.
General characteristics of the surveyed industrial employees, n (%).
Prevalence of MSDs
The self-reported prevalence of MSDs was defined as the prevalence of MSDs in the previous 12 months, with 498 participants reporting that they had some MSDs in at least one body area during the previous 12 months. However, only 79 participants reported that they had visited a physician for the condition. Pain and discomfort were mainly reported to occur in the neck, followed by the shoulders, and upper back areas. The prevalence of MSDs in frontline workers, office clerks, support personal and technicians was 285 (34.34%), 100 (37.45%), 49 (35.00%) and 64 (35.96%), respectively. Since the small sample sizes and similar trait, office clerks, support personal and technician had been chunked into a subgroup. The prevalence of shoulder pain (P = 0.040), wrist and hand pain (P < 0.001), and ankle and foot pain (P < 0.001) were found to be significantly different in frontline workers compared with other staff [Tables 2 and 3].
Table 2.
One-year cumulative prevalence of musculoskeletal disorders (MSDs)of industrial employees, n (%).
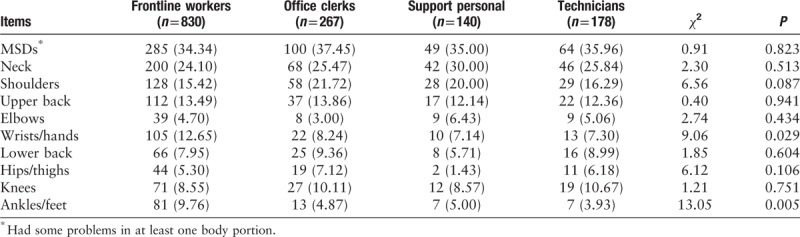
Table 3.
One-year cumulative prevalence of musculoskeletal disorders (MSDs) in two subgroups, n (%).
Factors associated with MSDs
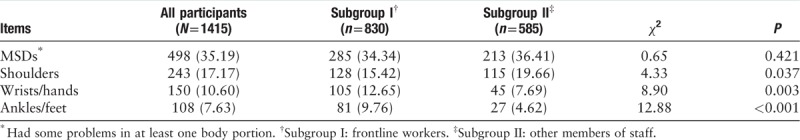
When analyzing participant questionnaires, the dependent variable was considered to be “1” if the person surveyed had suffered problems in at least one body part during the previous 12 months; otherwise, the dependent variable was considered to be “0”. Univariate analysis showed that the risk factors associated with the report of MSDs were female gender, increased age, a high level of education, a high or a low salary, lack of exercise, nightshift work, longer job tenure, at least a two-week history of illness and treatment, concurrent chronic diseases, reduced access to health information and health care, and a negative attitude towards seeking health care. The risk of MSDs increased in employees with a high BMI and in smokers, but these associations did not reach statistical significance. Education, exercise, and distance to the nearest medical institution had no effect on MSDs in front-line workers. MSDs in other staff showed no connection with age, monthly income, night-shift and job tenure [Table 4].
Table 4.
Different levels of risk factors associated with musculoskeletal disorders (MSDs)∗, n %.
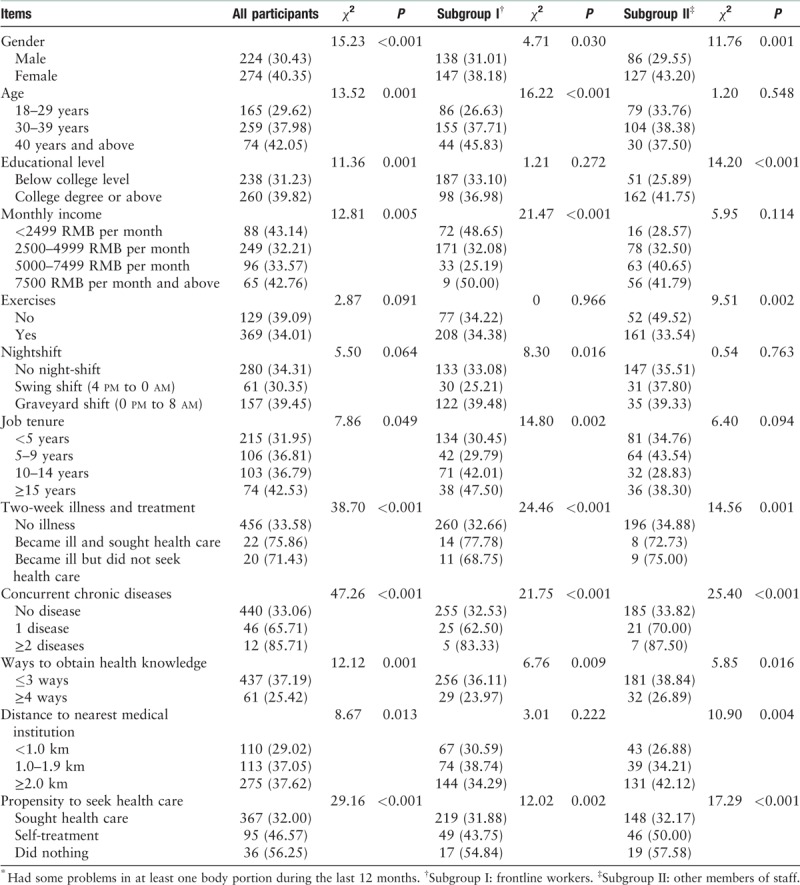
A binary logistic regression equation was established using stepwise regression analysis with variables shown in Table 3. The Hosmer-Lemeshow test showed a good fit for this model. Several risk factors for MSDs were obtained. The risk factors associated with MSDs in frontline workers were increased age (P = 0.005, OR = 1.63; P = 0.001, OR = 2.33), a high or a low salary (P < 0.001, OR = 0.49; P < 0.001, OR = 0.30), nightshift work (P = 0.027, OR = 1.46), at least a two-week history of illness and treatment (P = 0.004, OR = 5.60; P = 0.013, OR = 4.19), concurrent chronic diseases (P = 0.001, OR = 3.45; P = 0.092, OR = 7.81), reduced access to health information (P = 0.004, OR = 0.49), and a negative attitude towards seeking health care (P = 0.010, OR = 1.77; P = 0.009, OR = 2.75). Female gender (P < 0.001, OR = 2.30), education (P = 0.001, OR = 1.96), exercises (P = 0.027, OR = 0.59), night-shift (P = 0.017, OR = 1.98), concurrent chronic diseases (P = 0.002, OR = 3.73; P = 0.020, OR = 13.42), less access to health information (P = 0.013, OR = 0.53), distance to nearest medical institution (P = 0.009, OR = 1.83), and a negative attitude towards seeking health care (P = 0.009, OR = 1.94; P = 0.014, OR = 2.74) were associated with MSDs in other staff [Table 5].
Table 5.
Results of the adjusted odds ratio (OR) and 95% confidence interval (CI) of risk factors for musculoskeletal disorders (MSDs).
Discussion
The prevalence of MSDs in this study was lower than that reported by some previous studies conducted in China[8,13,24] and may be associated with improvements in the manufacturing process and the different local production environment. The consultation rate was low, which was considered to be due to the reduced concern, long working hours, high costs, long distances between home and work, lack of health information, and ineffective collaboration between local health systems and commercial enterprises.[13,30] In this study, the highest prevalence for MSDs occurred in the neck, shoulders and upper back areas. In a previous study, Yu et al[8] showed that the lower back, neck, shoulders, and wrists were the most common sites for MSDs. Liu et al[24] showed that the neck, waist, and shoulders were commonly involved in MSDs. The difference between these two earlier studies might be explained by the different study populations, but also by the increasing use of mechanization in Chinese industries. The increased use of industrial machinery over recent years has reduced the need for certain types of manual labor, which has reduced the reported prevalence of low back pain but has increased the prevalence of MSDs involving the upper body. Also, the increasing use of cell phones and computers may also be significant contributory factors in the increase in neck, shoulder, and upper back pain.[31,32] The combined results of the present study and recently published studies on work-related MSDs in China indicate that the prevalence and presentation of MSDs in the Chinese modernized industrial society have changed. As more aspects of working life become computer-based or machine-based, further studies are required to investigate the effects of this change on the musculoskeletal system and to develop methods to improve the health of individuals in the modern working environment.
In this study, there were significant differences between frontline industrial workers and other employees in the prevalence and influential factors. Frontline industrial workers had a higher rate of wrist, hand, ankle and foot pain, but a lower rate of shoulder pain compared with other staff. This finding was probably due to the different form of work between the two study groups, as the former undertake more standing for long periods and manual labor, while the second group undertakes more sedentary and computer-related work. Concerning this issue, different solutions should be considered for frontline industrial workers and other staff, which include the design of different physiotherapy or preventive practices to prevent MSDs in key areas of the body, and the provision of targeted orientation training for work that puts strain on different parts of the body, as well as improving the work environment to prevent MSDs. Educational level was associated with the rate of MSDs of other staff, and monthly income was associated with the rate of MSDs of frontline workers. This may be due to the undifferentiated manual labor of frontline workers in different educational levels; their jobs always correlated with income. Previous studies suggested that lower education and salary were the main risk factors of MSDs.[10,11] However, this study and two more previous studies conducted in China came to diametrically opposed conclusions.[8,13] Unfortunately, these studies have not attracted enough attention. The present study showed that highly-educated and high-income staffs were more likely to suffer MSDs. These discrepancies might be explained by overloaded work and unhealthy working lifestyle. Highly-educated and high-income staffs usually play important roles in the team and take on more work. This result should gain significant attention, as talented people were historically a major element of the nation's competitiveness. Further studies and countermeasures are now urgently needed. The present study showed that exercise played a minor role among frontline workers in reducing the risk of MSDs, which was possibly due to frontline workers already undertaking large amounts of physical labor in their work, or that workers were ignorant of the methods for scientific exercise. Previous studies showed that unstructured general physical exercises were less effective in preventing MSDs,[20] and that high-intensity exercises might induce injuries and other types of pain.[21] Therefore, in the future development of programs to prevent MSDs in industrial workers, individualized professional exercise plans may be necessary, which take into account individual factors such as work-related physical activity.
The findings of this study showed that a positive attitude to healthcare, accessible healthcare and rich resources to health knowledge were associated with a lower rate of MSDs. Workers who chose to self-medicate, or do nothing for their symptoms, were more likely to have MSDs compared with workers who actively sought visits to health services when they became ill. The more negative the coping style, the higher the risk of MSDs. Although the causal relationship between the propensity to seek health care and MSDs have not been previously reported, some previously published studies have concluded that higher scores for the propensity to seek health care reduces the rates of avoidable hospitalization, increases the rates of effective clinical management, and improves the control of chronic disease.[33,34] To reduce the rates of musculoskeletal pain, it is necessary to change the attitude of employees by health education and by cooperating with primary health care institutions that provide convenient high-quality health services at low cost. The findings of the present study also have implications for an approach to provide occupational health information to prevent work-related MSDs. In this study, the proportion of MSDs cases significantly decreased with the increased provision of health information. There are multiple approaches for the provision of health information in terms of content and presentation; flexible and diversified forms, along with repeat education and continuous reinforcement help to support individuals in a far better way than providing information via a single channel. Therefore, employees should be offered health information relating to MSDs through multiple channels, including lectures, training, consultation, leaflets, internet, and occupational health discussions at work. Of these, interpersonal communication should be a prioritized approach, as the interpersonal communication of health care is believed to be more trustworthy and more likely to be followed by employees.[35] Health education is supposed to improve diseases control, patient-doctor relationships, quality of life, as well as adherence to medicinal treatment plans.[36] Distance to health care providers reflects accessibility to treatment facilities, and has previously been shown to play an important role in improving health.[37,38] Increased distances from health care providers increases travel time and the cost of seeking health care, reduces the possibility of counseling and the early treatment of MSDs and results in a high prevalence of clinical symptoms. Therefore, building a cooperative relationship between industrial enterprises and relevant medical institutions, or the provision of on-site occupational health care services is an important consideration in the reduction of MSDs. Our study was consistent with early studies in that a number of factors are associated with MSDs, including female gender,[39,40] increased age, increased BMI,[41] smoking,[42] concurrent chronic diseases,[43] graveyard shift,[44,45] and increased job tenure.[7,13] Furthermore, there are some potential factors were not investigated in this study. Stress symptoms are often associated with musculoskeletal disease, and some studies indicate that stress symptoms contribute to the development of MSDs.[46] Industrial workers always suffer from high workload, low control on the job and low social support, which may cause high perceived stress. Production workers have a high utilization rate of tools which were known as important factors of musculoskeletal symptoms.[14,15] In China, people are increasingly relying on smartphones. However, it was shown to be a risk factor of MSDs.[47] Computer-based work has even become one of the most important ways in current China. With regard to ergonomic factors, computer use has shown to be risk factor of hand and upper extremity.[3,48,49]
This study has several limitations which need to be considered. This study used self-reported questionnaires to collect data, which may have resulted in data bias. To encourage participants to answer honestly, anonymous questionnaires were used. An electronic mode that no question could be skipped was used to ensure that there was no missing data. There was no security that worker reports are as precise as instrumental measurements. However, the self-reported questionnaire is widely used in the research field of MSDs and some researchers believe that it may be more accurate than other approaches, such as reviewing hospital records or performing physical examinations.[50] Also, there are some potential factors which may cause impact upon the prevalence of employee MSDs need future research.
The findings of this study on the prevalence and risk factors for MSDs in industrial employees in a modern industrial region in China showed that MSDs were common, but also that there was a low number of employees seeking treatment. The rates of upper body pain are increasing while those of low back pain are decreasing. Frontline industrial workers show a higher rate of MSD symptoms which predominantly included pain in the wrists, hands, ankles, and feet, but a lower rate of shoulder pain when compared with other staff. In industrial employees, MSDs were found to be correlated with negative propensity to healthcare, limited ways to obtain health knowledge, and concomitant chronic diseases. Surprisingly, highly educated and high-income employees had a higher risk of MSDs, and general physical exercises were less effective in preventing MSDs. Companies, employers, and health care providers might reduce the impact of MSDs by introducing an integrated injury prevention program, based on characteristics of individuals and their work. Such a program might also include support for personal fitness, smoking cessation, and weight reduction, as well as the evaluation and modification of relevant job factors, as well as improvements in medical information, counseling, and access to health services. The findings of this study provide support for the importance of assessing individual factors, including gender, age, socioeconomic status, and work status during the evaluation of individual risk for developing MSDs.
Acknowledgments
The authors would like to thank Qiang Ye, Jing He, Bo Pang, the Beijing Fangshan Commission of Economy and Information Technology, Jun-Qiang Geng, CN Care Network Limited, and the leaders of the six companies involved in this study for their support.
Funding
This study was supported by a grant from the Research Foundation for Capital General Practice, Beijing, China (No. 3500-17QK01).
Conflicts of interest
None.
Footnotes
How to cite this article: Wang T, Zhao YL, Hao LX, Jia JG. Prevalence of musculoskeletal symptoms among industrial employees in a modern industrial region in Beijing, China. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000165
References
- 1.Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol 2004; 14:13.doi: 10.1016/j.jelekin.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Zhang FR, He LH, Wu SS, Li JY, Ye KP, Wang S. Quantify work load and muscle functional activation patterns in neck-shoulder muscles of female sewing machine operators using surface electromyogram. Chin Med J 2011; 124:3731.doi: 10.3760/cma.j.issn.0366-6999.2011.22.024. [PubMed] [Google Scholar]
- 3.Ortiz-Hernández L, Tamez-González S, Martínez-Alcántara S, Méndez-Ramí́rez I. Computer use increases the risk of musculoskeletal disorders among newspaper office workers. Arch Med Res 2003; 34:331–342. doi: 10.1016/S0188-4409(03)00053-5. [DOI] [PubMed] [Google Scholar]
- 4.Lötters F, Meerding WJ, Burdorf A. Reduced productivity after sickness absence due to musculoskeletal disorders and its relation to health outcomes. Scand J Work Environ Health 2005; 31:367–374. doi: 10.5271/sjweh.920. [DOI] [PubMed] [Google Scholar]
- 5.Nagata T, Mori K, Ohtani M, Nagata M, Kajiki S, Fujino Y, et al. Total health-related costs due to absenteeism, presenteeism, and medical and pharmaceutical expenses in Japanese employers. J Occup Environ Med 2018; 60:e273.doi: 10.1097/JOM.0000000000001291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson WMS, Bertha A, Johnson P. Prevalence of upper extremity musculoskeletal disorders among workers in an industrial town in Tamilnadu. J Clin Diagn Res 2011; 5:187–190. [Google Scholar]
- 7.Coury HJCG, Porcatti IA, Alem MER, Oishi J. Influence of gender on work-related musculoskeletal disorders in repetitive tasks. Int J Ind Ergon 2002; 29:33–39. doi: 10.1016/S0169-8141(01)00047-6. [Google Scholar]
- 8.Yu S, Lu ML, Gu G, Zhou W, He L, Wang S. Musculoskeletal symptoms and associated risk factors in a large sample of Chinese workers in Henan province of China. Am J Ind Med 2012; 55:281–293. doi: 10.1002/ajim.21037. [DOI] [PubMed] [Google Scholar]
- 9.Palmer KT, Syddall H, Cooper C, Coggon D. Smoking and musculoskeletal disorders: findings from a British national survey. Ann Rheum Dis 2003; 62:33–36. doi: 10.1136/ard.62.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hagen K, Zwart JA, Svebak S, Bovim G, Jacob Stovner L. Low socioeconomic status is associated with chronic musculoskeletal complaints among 46,901 adults in Norway. Scand J Public Health 2005; 33:268–275. doi:10.1080/14034940510005699. [DOI] [PubMed] [Google Scholar]
- 11.Putrik P, Ramiro S, Chorus AM, Boonen A. People with lower education, inactive working status and female gender are more likely to have musculoskeletal disease. Ann Rheum Dis 2013; 72 suppl 3:A767–A768. doi: 10.1136/annrheumdis-2013-eular.2272. [Google Scholar]
- 12.Choobineh A, Soltanzadeh A, Tabatabaee H, Jahangiri M, Khavaji S. Health effects associated with shift work in 12-hour shift schedule among Iranian petrochemical employees. Int J Occup Saf Ergon 2012; 18:419–427. doi: 10.1080/10803548.2012.11076937. [DOI] [PubMed] [Google Scholar]
- 13.Yu W, Yu IT, Li Z, Wang X, Sun T, Lin H, et al. Work-related injuries and musculoskeletal disorders among factory workers in a major city of China. Accid Anal Prev 2012; 48:457–463. doi: 10.1016/j.aap.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Lei L, Dempsey PG, Xu JG, Ge LN, Liang YX. Risk factors for the prevalence of musculoskeletal disorders among Chinese foundry workers. Int J Ind Ergonom 2005; 35:197–204. doi: 10.1016/j.ergon.2004.08.007. [Google Scholar]
- 15.Widanarko B, Legg S, Stevenson M, Devereux J, Eng A, Mannetje AT, et al. Prevalence of musculoskeletal symptoms in relation to gender, age, and occupational/industrial group. Int J Ind Ergon 2011; 41:561–572. doi: 10.1016/j.ergon.2011.06.002. [Google Scholar]
- 16.Bau JG, Chia T, Wei SH, Li YH, Kuo FC. Correlations of neck/shoulder perfusion characteristics and pain symptoms of the female office workers with sedentary lifestyle. PLoS One 2017; 12:e0169318.doi: 10.1371/journal.pone.0169318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai SP, Gilstrap EL, Cowles SR, Waddell LC, Jr, Ross CE. Personal and job characteristics of musculoskeletal injuries in an industrial population. J Occup Med 1992; 34:606–612. doi: 10.2307/2137254. [PubMed] [Google Scholar]
- 18.Herbert R, Dropkin J, Warren N, Sivin D, Doucette J, Kellogg L, et al. Impact of a joint labor-management ergonomics program on upper extremity musculoskeletal symptoms among garment workers. Appl Ergon 2001; 32:453–460. doi: 10.1016/S0003-6870(01)00024-2. [DOI] [PubMed] [Google Scholar]
- 19.Maher CG. A systematic review of workplace interventions to prevent low back pain. Aust J Physiother 2000; 46:259–269. doi: 10.1016/S0004-9514(14)60287-7. [DOI] [PubMed] [Google Scholar]
- 20.Blangsted AK, Søgaard K, Hansen EA, Hannerz H, Sjøgaard G. One-year randomized controlled trial with different physical-activity programs to reduce musculoskeletal symptoms in the neck and shoulders among office workers. Scand J Work Environ Health 2008; 34:55–65. doi: 10.5271/sjweh.1192. [DOI] [PubMed] [Google Scholar]
- 21.Miranda H, Viikari-Juntura E, Martikainen R, Takala EP, Riihimäki H. Physical exercise and musculoskeletal pain among forest industry workers. Scand J Med Sci Sports 2001; 11:239–246. doi: 10.1034/j.1600-0838.2001.110408.x. [DOI] [PubMed] [Google Scholar]
- 22.Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup Environ Med 2003; 60:E6.doi: 10.1136/oem.60.9.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wen Yi. China's rapid rise: from backward agrarian society to industrial powerhouse in just 35 years. Reg Econ 2016; 24:8–14. [Google Scholar]
- 24.Liu J, Huang G, Li X, Wang S, Liu L, Liu X. Study on prevalence of occupational musculoskeletal disorders and their risk factors among workers in three industries in Zhongshan, China (in Chinese). Chin J Ind Hyg Occup Dis 2014; 32:415–417. doi: 10.3760/cma.j.issn.1001-9391.2014.06.004. [PubMed] [Google Scholar]
- 25.Jia P. Industry 4.0 era: the strategic breakthrough point of Beijing modern manufacturing industry. Chin Dev Obs 2017; 50–52. [Google Scholar]
- 26.Li L.X, Zuo ZG, Shi YL, Liu JF, Qi XD, Liu PS, et al. Statistical Yearbook of Fangshan District, Beijing 2017 (in Chinese). 2017; Beijing: Beijing Bureau of Statistics, 17–24. [Google Scholar]
- 27.Katz DA, Mchorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. J Gen Intern Med 2010; 15:789–796. doi: 10.1046/j.1525-1497.2000.90906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Bieringsørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987; 18:233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 29.Fang YX, Li SY, Zhang YN, Zhang P, Wu H, Wang DH. Test-retest reliability of Nordic Musculoskeletal Questionnaire in nurses (in Chinese). Chin J Ind Hyg Occup Dis 2013; 31:753–758. doi: 10.3760/cma.j.issn.1001-9391.2013.10.008. [PubMed] [Google Scholar]
- 30.Le ATK, Pham LTL, Lan HV, Schelling E. Health services for reproductive tract infections among female migrant workers in industrial zones in Ha Noi, Viet Nam: an in-depth assessment. Reprod Health 2012; 9:4.doi: 10.1186/1742-4755-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tornqvist EW, Hagberg M, Hagman M, Risberg EH, Toomingas A. The influence of working conditions and individual factors on the incidence of neck and upper limb symptoms among professional computer users. Int Arch Occup Environ Health 2009; 82:689–702. doi: 10.1007/s00420-009-0396-7. [DOI] [PubMed] [Google Scholar]
- 32.Marcus M, Gerr F, Monteilh C, Ortiz DJ, Gentry E, Cohen S, et al. A prospective study of computer users: II. Postural risk factors for musculoskeletal symptoms and disorders. Am J Ind Med 2002; 41:236–249. doi: 10.1002/ajim.10067. [DOI] [PubMed] [Google Scholar]
- 33.Loenen TV, Berg MJVD, Faber MJ, Westert GP. Propensity to seek healthcare in different healthcare systems: analysis of patient data in 34 countries. BMC Health Serv Res 2015; 15:1–10. doi: 10.1186/s12913-015-1119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loenen TV, Berg MVD, Westert GP. Propensity to seek care and avoidable hospitalization. European Journal of Public Health. Eur J Public Health 2013; 23:69.doi: 10.1093/eurpub/ckt126.161. [Google Scholar]
- 35.Valente TW, Fosados R. Diffusion of innovations and network segmentation: the part played by people in promoting health. Sex Transm Dis 2006; 33 (7 Suppl):S23.doi: 10.1097/01.olq.0000221018.32533.6d. [DOI] [PubMed] [Google Scholar]
- 36.Yang M, Rao HY, Feng B, Wu E, Wei L, Lok Anna S. Effect of a patient education intervention on asthma control and patient-doctor relationship. Chin Med J 2018; 131:1110.doi: 10.4103/0366-6999.218023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Billi JE, Pai CW, Spahlinger DA. The effect of distance to primary care physician on health care utilization and disease burden. Health Care Manage Rev 2007; 32:22–29. doi: 10.1097/00004010-200701000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Andrew B, Kevin G, Dennis O, Miriam K, Karen V, Nicole L, et al. Preventable hospitalizations and access to health care. JAMA 1995; 4:305.doi: 10.1016/1062-1458(96)81082-8. [PubMed] [Google Scholar]
- 39.Fillingim RB, King CD, Ribeiro-dasilva MC, Rahim-williams B, Riley RJ. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 2009; 10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nordander C, Ohlsson K, Balogh I, Hansson GA, Axmon A, Persson R, et al. Gender differences in workers with identical repetitive industrial tasks: exposure and musculoskeletal disorders. Int Arch Occup Environ Health 2008; 81:939–947. doi:10.1007/s00420-007-0286-9. [DOI] [PubMed] [Google Scholar]
- 41.Onyemaechi NO, Anyanwu GE, Obikili EN, Onwuasoigwe O, Nwankwo OE. Impact of overweight and obesity on the musculoskeletal system using lumbosacral angles. Patient Prefer Adherence 2016; 10:291–296. doi:10.2147/PPA.S90967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abate M, Vanni D, Pantalone A, Salini V. Cigarette smoking and musculoskeletal disorders. Muscles Ligaments Tendons J 2013; 3:63.doi: 10.11138/mltj/2013.3.2.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van der Zee-Neuen A, Putrik P, Ramiro S, Keszei A, de Bie R, Chorus A, et al. Impact of chronic diseases and multimorbidity on health and health care costs: the additional role of musculoskeletal disorders. Arthritis Care Res (Hoboken) 2016; 68:1823–1831. doi:10.1002/acr.22913. [DOI] [PubMed] [Google Scholar]
- 44.Stocks J, Tang NKY, Walsh DA, Warner SC, Harvey H, Jenkins W, et al. Bidirectional association between disturbed sleep and neuropathic pain symptoms: a prospective cohort study in post-total joint replacement participants. J Pain Res 2018; 11:1087–1093. doi:10.2147/JRS149830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matre D, Knardahl S, Nilsen KB. Night-shift work is associated with increased pain perception. Scand J Work Environ Health 2017; 43:260–268. doi:10.5271/sjweh.3627. [DOI] [PubMed] [Google Scholar]
- 46.Bongers PM, Winter CRd, Kompier MA, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health 1993; 19:297–312. doi:10.5271/sjweh.1470. [DOI] [PubMed] [Google Scholar]
- 47.Gustafsson E, Thomée S, Grimby-Ekman A, Hagberg M. Texting on mobile phones and musculoskeletal disorders in young adults: a five-year cohort study. Appl Ergon 2017; 58:208–214. doi: 10.1016/j.apergo.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 48.Fogleman M, Brogmus G. Computer mouse use and cumulative trauma disorders of the upper extremities. Ergonomics 1995; 38:2465–2475. doi: 10.1080/00140139508925280. [DOI] [PubMed] [Google Scholar]
- 49.Jong-Won K, Heon K, Soo-Hun C, Myung-Koo L, Yong-Dae K, Hong-Mei N, et al. The association of subjective stress, urinary catecholamine concentrations and PC game room use and musculoskeletal disorders of the upper limbs in young male Koreans. J Korean Med Sci 2003; 18:419.doi: 10.3346/jkms.2003.18.3.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo HR, Chang YC, Yeh WY, Chen CW, Guo YL. Prevalence of musculoskeletal disorder among workers in Taiwan: a nationwide study. J Occup Health 2004; 46:26–36. doi: 10.1539/joh.46.26. [DOI] [PubMed] [Google Scholar]


