To the Editor: Nowadays, most infants with tetralogy of Fallot (TOF) survive the initial surgical repair; however, they continue to experience residual hemodynamic and physiologic abnormalities in the follow-up.[1] Pulmonary regurgitation (PR) is still recognized as the most common complication that determines late outcomes. PR may result in right ventricular (RV) dilatation and, ultimately, cardiac dysfunction. Indicators of deterioration of clinical status such as impaired exercise tolerance, ventricular arrhythmia, and sudden cardiac death have all been associated with chronic PR. The degree of PR is one of the most important factors determining RV dysfunction; thus, pulmonary valve replacement becomes necessary to retain lower RV volumes, increase the RV systolic function, and lower the mortality rates.[2] Cardiac magnetic resonance (CMR) imaging is now recommended as the optimal method to use in the follow-up of patients with TOF.[3] It has been proven to be more accurate than transthoracic echocardiography for the evaluation of RV function due to the irregular RV cavity.[4,5] Indexed PR volume (PRVi) and PR fraction (PRF) are the two main markers to be measured; however, the optimal method for PR quantification remains controversial. Previous studies have recommended the use of PRVi and hypothesized that this marker is better than PRF in reflecting RV preload. However, PRVi is not widely used in clinical practice and has not been the diagnostic standard for PR classification. Accordingly, our study aimed to discover the optimal index for the assessment of the degree of PR.
This retrospective study included 57 consecutive patients with repaired TOF who had undergone CMR evaluations from June 2008 to September 2017, and had evidence of PR on echocardiography. All patients underwent transthoracic echocardiography within 1 week of CMR. Each patient or their guardians provided written informed consent for participation in this study, and the institutional ethics committee approved the review of medical records. The exclusion criteria included: (i) percutaneous or surgical pulmonary valve replacement, (ii) more than mild regurgitation of other cardiac valves except the pulmonary valve, and (iii) intra- or extra-cardiac residential shunts. Patient characteristics including age, sex, age at TOF repair, and type of surgical repair were recorded.
All CMR studies were performed using a commercially available 1.5-T scanner (Avanto; Siemens, Erlangen, Germany) with an 8-element phased-array surface coil. Volumetric analysis and two-dimensional phase-contrast (PC) sequence in the main pulmonary artery were performed as previously reported.[6] The following parameters were calculated: end-diastolic volume, end-systolic volume, and ejection fraction of the right and left ventricles. The volume parameters of the right and left ventricles were indexed using the body surface area. RV dilatation was classified using indexed RV end-diastolic volume (RVEDVi): mild RV dilatation (RVEDVi = 110–140 mL/m2), medium RV dilatation (RVEDVi = 141–170 mL/m2), and severe RV dilatation (RVEDVi > 170 mL/m2).[7]
The clinical characteristics and CMR results of all remaining 57 patients are presented in Table 1. The median PRVi and PRF were 27.09 ± 18.67 mL·beat−1·m−2 and 32.98 ± 16.17%, respectively. The correlation between PRVi and PRF was proved (r = 0.690). Although a strong correlation was seen between PRF and PRVi, we also observed that significant variability existed in individual patients. For instance, a PRF of 40% could represent a PRVi of 18 or 38 mL·beat−1·m−2. On the contrary, a PRVi of 48 mL·beat−1·m−2 could represent a PRF of between 22% and 56%.
Table 1.
Characteristics of the study population and CMR results.

Both RVEDVi and RVESVi had moderate correlation with PRVi (r = 0.400/0.327, P = 0.002/0.013); however, PRF did not show a significant correlation with RVEDVi and RVESVi (r = 0.105/0.081, P = 0.439/0.551). The correlation of PRVi or PRF with RV ejection fraction was slight.
When RV dilatation was classified into three subgroups, mild (n = 39), medium (n = 5), and severe (n = 13), a considerably higher difference among the 3 groups was noted in PRVi than in PRF (F = 11.177, P < 0.001 vs. F = 16.525, P < 0.001). PRVi showed the ability to differentiate mild from medium RV dilatation, whereas PRF did not have this ability [Figure 1].
Figure 1.
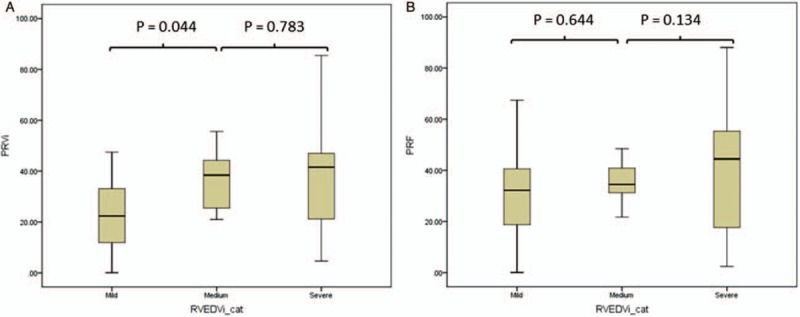
PRVi (A) and PRF (B) compared by RVEDVi criterion. PRF: Pulmonary regurgitation fraction; PRVi: Indexed pulmonary regurgitation volume; RVEDVi: Indexed right ventricular end-diastolic volume.
Patients with severe RVEDVi, PRVi showed better ability to identify severe RV dilatation (area under the ROC curve [AUC] of PRVi = 0.705 vs. AUC of PRF = 0.601, P = 0.026). The cutoff value of PRVi was 37 mL/beat/m2, whereas the sensitivity and specificity were 0.615 and 0.818, respectively.
During the past decade, several studies have investigated the indices of PR and proved a close correlation between PRF and PRVi; however, which is the better index remains debated. PRF has been commonly used in published TOF studies and recommended for decision making on pulmonary valve replacement; however, this parameter has some limitations. The expression of a percentage cannot reflect the exact volume backward. Henkens proved that PRF was not related to RV dimensions; thus, the timing of pulmonary valve replacement should be based on RVESV and RV ejection fraction rather than PRF.[4] Wald et al found that PRVi was better than PRF for the identification of severe RV dilatation (AUC 0.83 vs. 0.71, P = 0.003).[7] Meanwhile, PRF and PRVi are not interchangeable. Wald et al suggested that PRF may remain the same with different PRVis due to different RV volumes.[7] This phenomenon was also seen in our study.
The impact of PR overload on the RV relies on its grade and duration. Chronic PR of more than a moderate degree will increase RVEDV. Spiewak et al showed that PRVi showed better ability than PRF in evaluating RV dilatation, both in populations with and without RV outflow tract obstruction (RVOTO).[8] Sakrana et al and Gorter et al proposed that PRVi was better correlated with RVEDV than was PRF.[9,10] Similar to previous reports, our study showed that PRVi showed a good correlation with RV volume measurements (RVEDVi and RVESVi) and may be preferable to PRF. Meanwhile, PRVi also performed superior to PRF in discriminating between different extents of RV dilatation and is more appropriate for the quantification of RV dilatation. Furthermore, based on ROC analysis in patients with significant RVEDVi, PRVi was a better predictor of significant RV dilatation than PRF, with high sensitivity and specificity.
The indications for pulmonary valve replacement in repaired TOF are variable, including severe PR, abnormal cardiac function, decreased exercise intolerance, heart failure symptoms, and severe arrhythmia.[3] Numerous reports have extensively discussed about this topic, and some indications remain debated.[11] Nevertheless, the accurate evaluation of PR and RV dilatation is always the most important factor overall, and it is prudent to use the most reliable index in assessing the volume load on the heart. We believe that PRVi can fulfill these criteria, rather than PRF, especially for patients with larger RV. In addition, an RV to left ventricular (LV) interaction can cause subsequent LV dysfunction. At long-term follow-up, about 25% of patients with repaired TOF had LV dysfunction, and some researchers recommended the use of the RV/LV ratio instead of RVEDVi.[6] It has been proven that PRVi could also be used with the RV/LV ratio, as the optimal combination for TOF evaluation.[12]
In conclusion, PRVi and PRF have a good correlation with each other; however, they are not interchangeable. PRVi has a statistically significantly higher correlation with the RV volume and can be a better marker of RV dilatation than PRF. Now in our institution, we both check the PRF and PRVi for RV function evaluation in reaired patients with TOF, especially in those patients with large RV. We thought PRVi could be a valuable supplement for a TOF patient's follow-up.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Funding
This study was supported by a grant from the National Key Research and Development Program of China (No. 2016YFC1000500).
Conflicts of interest
None.
Footnotes
How to cite this article: Yao Q, Shen QL, Hu XH, Qiao ZW, Huang GY. Evaluation of pulmonary regurgitation by using different cardiac magnetic resonance indices in children with repaired tetralogy of Fallot. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000154
References
- 1.Nollert G, Fischlein T, Bouterwek S, Böhmer C, Klinner W, Reichart B. Long-term survival in patients with repair of tetralogy of Fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. J Am Coll Cardiol 1997; 30:1374–1383. doi: 10.1016/s0735-1097(97)00318-5. [DOI] [PubMed] [Google Scholar]
- 2.Ferraz Cavalcanti PE, Sá MP, Santos CA, Esmeraldo IM, de Escobar RR, de Menezes AM, et al. Pulmonary valve replacement after operative repair of tetralogy of Fallot: meta-analysis and meta-regression of 3,118 patients from 48 studies. J Am Coll Cardiol 2013; 62:2227–2243. doi: 10.1016/j.jacc.2013.04.107. [DOI] [PubMed] [Google Scholar]
- 3.Geva T. Repaired tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support. J Cardiovasc Magn Reson 2011; 13:9.doi: 10.1186/1532-429X-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henkens IR, van Straten A, Schalij MJ, Hazekamp MG, de Roos A, van der Wall EE, et al. Predicting outcome of pulmonary valve replacement in adult tetralogy of Fallot patients. Ann Thorac Surg 2007; 83:907–911. doi: 10.1016/j.athoracsur.2006.09.090. [DOI] [PubMed] [Google Scholar]
- 5.Mercer-Rosa L, Yang W, Kutty S, Rychik J, Fogel M, Goldmuntz E. Quantifying pulmonary regurgitation and right ventricular function in surgically repaired tetralogy of Fallot: a comparative analysis of echocardiography and magnetic resonance imaging. Circ Cardiovasc Imaging 2012; 5:637–643. doi: 10.1161/CIRCIMAGING.112.972588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao Q, Hu XH, Shen QL, Qiao ZW, Pa ME, Qian B, et al. Differential effect of the ratio of right ventricular volume to left ventricular volume in children with repaired tetralogy of Fallot. Cardiology 2016; 133:135–140. doi: 10.1159/000441291. [DOI] [PubMed] [Google Scholar]
- 7.Wald RM, Redington AN, Pereira A, Provost YL, Paul NS, Oechslin EN, et al. Refining the assessment of pulmonary regurgitation in adults after tetralogy of Fallot repair: should we be measuring regurgitant fraction or regurgitant volume? Eur Heart J 2009; 30:356–361. doi: 10.1093/eurheartj/ehn595. [DOI] [PubMed] [Google Scholar]
- 8.Spiewak M, Biernacka EK, Małek ŁA, Miśko J, Kowalski M, Miłosz B, et al. Quantitative assessment of pulmonary regurgitation in patients with and without right ventricular tract obstruction. Eur J Radiol 2011; 80:e164–e168. doi: 10.1016/j.ejrad.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Sakrana AA, Al-Zubaidi SA, Nasr MM, Helmy EM, Al Ghamdi SS, Tahlawi ME. Cardiac magnetic resonance indices reflecting pulmonary regurgitation burden after tetralogy of Fallot repair. Clin Radiol 2017; 72:900–909. doi: 10.1016/j.crad.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Gorter TM, van Melle JP, Freling HG, Ebels T, Bartelds B, Pieper PG, et al. Pulmonary regurgitant volume is superior to fraction using background-corrected phase contrast MRI in determining the severity of regurgitation in repaired tetralogy of Fallot. Int J Cardiovasc Imaging 2015; 31:1169–1177. doi: 10.1007/s10554-015-0670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geva T. Indications for pulmonary valve replacement in repaired retralogy of Fallot: the quest continues. Circulation 2013; 128:1855–1857. doi: 10.1161/CIRCULATIONAHA.113.005878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Śpiewak M, Małek ŁA, Petryka J, Mazurkiewicz Ł, Miłosz B, Biernacka EK, et al. The ratio of right ventricular volume to left ventricular volume reflects the impact of pulmonary regurgitation independently of the method of pulmonary regurgitation quantification. Eur J Radiol 2012; 81:e977–e981. doi: 10.1016/j.ejrad.2012.06.026. [DOI] [PubMed] [Google Scholar]


