Abstract
Background:
The mucous membrane of the maxillary sinus is very sensitive to foreign bodies and infections. Any triggering may lead to mucous membrane thickening (MMT). Residual bone thickness (RBT) is the remaining bone apical to the periodontal defect until the floor of the maxillary sinus acts as a barrier for the periodontal infections to reach the sinus. The aim of our current study was to evaluate the minimal RBT to prevent periodontal infection to reach Schneiderian membrane using cone-beam computed tomography (CBCT).
Materials and Methods:
In this descriptive study, 144 maxillary sinus exposure records of 100 patients were collected retrospectively. Patients with minimum one sinus exposure were considered. MMT and RBT were calculated with the CBCT assistance. Statistical analysis was done using Mann–Whitney U-test, Kruskal–Wallis and Chi-square test. (P < 0.05) was considered as statistically significant.
Results:
Significant difference (P < 0.001) was observed in MMT among three RBT groups. Significantly, higher mean MMT was observed with <2 mm and 2–4 mm RBT groups. The prevalence of MMT with >4 mm group is less (7%) compared to <2 mm group and 2–4 mm RBT groups (91.2% and 90.2%, respectively). Furthermore, there is no significant difference in MMT between angular and furcation defects (P = 0.890).
Conclusion:
Probability of MMT was increased if RBT is <4 mm. Early detection and prompt periodontal treatments associated with regenerative procedures can be instituted wherever possible to improve RBT and to reduce MMT. Further, microbiological studies are required to confirm the analysis.
Keywords: Cone-beam computed tomography, furcation defects, maxillary sinus, mucous membrane, periodontal diseases, periodontitis
INTRODUCTION
The maxillary sinus is one among the paranasal sinuses located within the maxillary bone. It is connected with the nasal cavity through an ostium. It maintains the airway, temperature, and balancing of the skull.[1] The Schneiderian membrane is a mucous membrane, which lines the maxillary sinus, and is quite sensitive to infectious agents of both odontogenic or nonodontogenic origin.[2] Its thickness generally ranges from 1 to 2 mm and is closely adherent to the periosteum.[2,3,4] Periodontal, periapical, and peri-implant infections which are in proximity to sinus floor may evoke inflammatory reactions in the Schneiderian membrane, further leading to the mucous membrane thickening (MMT) and sinusitis.[5,6,7,8] MMT of >2 mm is considered as pathological.[9] Thickening of the maxillary sinus membrane and chronic maxillary sinusitis may lead to pathogenesis of adjacent structures such as ethmoidal sinus.[10]
Passage of odontogenic infections through the floor of the sinus is very uncommon as the floor of the sinus is made of thick cortical bone.[11] It has also been observed that few cases (<10%) are affected due to the infection or inflammatory agents reaching the cortical bone marrow of the floor of the maxillary sinus. This can be attributed to the thick residual bone between the apical extent of the periodontal or periapical lesion and floor of the maxillary sinus which has a prime role in preventing the transmission of infections of odontogenic origin.[12] Periapical and periodontal pathology reaching the maxillary sinus is a well-known concept.[13] However, very little research evidence is available on minimal residual bone thickness (RBT) that is required apical to periodontal defect till the floor of the maxillary sinus to effectively prevent transmission of infection. Cone-beam computed tomography (CBCT) can be used to check periodontal disease extension, RBT, and MMT. CBCT overcomes the challenges such as overimposition anatomical structures and allows visualization of anatomical relations three-dimensionally.[14,15] It also helps in identifying etiology of the infection and association with dental or periodontal pathology.[16]
We hypothesized that periodontal infection leading to MMT of the maxillary sinus depends on RBT apical to periodontal defect, i.e., the distance between the floor of the maxillary sinus and apical extent of the periodontal defect. Hence, the aim of the present study was to investigate the minimum RBT to prevent odontogenic infection to reach maxillary sinus and to prevent pathological MMT with the aid of CBCT imaging. With this study, we can implicate this knowledge in periodontal regenerative procedures wherever possible to increase RBT to reduce the potential risk of maxillary sinusitis due to periodontitis.
MATERIALS AND METHODS
The current study was a retrospective, single-center descriptive study, conducted in Sri Rajiv Gandhi Dental College and Hospital, Bengaluru, India. This study included CBCT images recorded from June 2014 to May 2016 from the Department of Oral Radiology. Before starting the study, written informed consent had been obtained from the patients for checking their records and usage of their investigations for this research purpose. The study was started after the approval from an ethical committee and institutional review board.
CBCT with good quality images showing at least one tooth with an angular defect and furcation involvements in posterior region of maxilla were considered for review These radiographs were taken previously for different diagnostic and treatment purposes. A total of 258 defect sites were observed in 100 patients with 144 maxillary sinus exposures. Both male and female patients aged between 35 and 70, who were diagnosed with chronic periodontitis, were considered. Patient's previous records and periodontal charting were observed to correlate periodontal status and other histories for maxillary sinusitis.
Exclusion criteria
Categorizing odontogenic and nonodontogenic sinusitis was done according to the Abrahams guidelines.[17] Patients with preexisting maxillary sinusitis because of nonodontogenic origin, previous history of trauma, teeth with dental caries or periapical pathologies, pregnancy, nursing, history of using antibiotics in the past 2 months, patients who underwent any periodontal treatment 6 months before CBCT investigation, and edentulous areas or implants were excluded from the study.
Evaluation of images
CBCTs were taken (exposure: 90 KV, 2.5 mA, 15 s and dose: 1179 mGy.cm2), and measurements were recorded with the software (CS 3D imaging, v3.3, NY, USA) and calibrated by two dental graduates under the supervision of two oral and maxillofacial radiologists with a minimum of 2 years of experience in evaluating CBCT and the average was noted. The bias between inter-examiner calibrations was eliminated by calibrating 30% of images again.
Measuring Schneiderian membrane thickness
MMT was measured at the thickest area of the membrane perpendicularly from the underlying bone. The measuring line of MMT should be a continuation of the measuring line of RBT. Mucosal thickness grouped into two: (a) ≤2 mm as normal [Figure 1] and (b) >2 mm thickening as pathological MMT [Figure 2].[18] For each sample, measurements were taken both in coronal and sagittal sections of CBCT and the average was noted [Figure 2].[13] Rulers in the CBCT software were used for the measurements.
Figure 1.

Normal thickness of mucus membrane without periodontal infection.
Figure 2.

Measurement of residual bone thickness and mucous membrane thickening in sagittal sections of cone-beam computed tomography in relation to periodontal lesion.
Measuring residual bone thickness
Underlying RBT was measured with a line, at the thinnest area from the apical-most region of the periodontal lesion to the floor of the maxillary sinus [Figure 2]. Again, for each sample, measurements were taken both in coronal and sagittal sections of CBCT and the average was noted. RBT is grouped into three: (a) <2 mm, (b) 2–4 mm, and (c) >2 mm. All types of vertical defects (one-wall, two-wall, and three-wall defects) and all types of furcation defects were taken into consideration. Rulers in the CBCT software were used for measurements.
Statistical analysis
Statistical analysis was done, and Mann–Whitney U-test was performed for intra-group comparisons. Kruskal–Wallis test was performed for intergroup comparisons. Chi-square test was used for checking association of the prevalence of MMT with RBT groups. Statistical Package for the Social Sciences (v20.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis. P < 0.05 was taken as statistically significant.
RESULTS
A total of 144 CBCT sinus exposures of 100 patients (male 56, female 44) with 258 sites were included in the study, in which 166 sites were with angular defects and 92 were with furcation involvement. Intergroup comparisons in variations in MMT among <2 mm, 2–4 mm, and >4 mm RBT groups with the Kruskal–Wallis test show a significant difference among the groups. Mean mucosal thickness was within the range of normal mucosal thickness (<2 mm) in >4 mm RBT group and reverse was seen with <2 mm and 2–4 mm RBT groups, which come under pathological MMT range (>2 mm). These results are summarized in Table 1.
Table 1.
Intergroup comparisons of mucous membrane thickening among three residual bone thickness groups
| RBT (mm) | n | Mean mucosal thickness (mm) | SD | P# |
|---|---|---|---|---|
| <2 | 136 | 4.411a | 1.431 | <0.001** |
| 2-4 | 51 | 3.024b | 0.769 | |
| >4 | 71 | 0.951c | 0.683 |
#Kruskal-Wallis; post hoc Mann-Whitney test was used for intergroup comparison; Different alphabets in the superscript showed a significant difference among groups. SD: Standard deviation; RBT: Residual bone thickness
The prevalence of MMT in different groups is shown in Table 2. MMT is more prevalent in <2 mm and 2–4 mm RBT groups when compared to >4 mm group. A total number of pathological MMT sites in <2 mm and 2–4 mm groups are 65.89%. Greater than 4 mm RBT group showed a major number of sites with nonpathological MMT.
Table 2.
Prevalence of mucous membrane thickening in different residual bone thickness groups
| RBT (mm) | Prevalence of mucosal thickness (MMT) (%) | Total | |
|---|---|---|---|
| ≤2 mm | >2 mm | ||
| <2 | 12 (8.8) | 124 (91.2) | 136 |
| 2-4 | 5 (9.8) | 46 (90.2) | 51 |
| >4 | 66 (93) | 5 (7) | 71 |
| Total | 83 | 175 | 258 |
Chi-square test was used for association of prevalence of MMT thickness with RBT groups; χ2=165.893; df=2; P<0.001; highly significant. RBT: Residual bone thickness; MMT: Mucous membrane thickening
No significant difference was observed between the mean RBT of angular and furcation defects, as shown in Table 3. Similarly, no significant difference was observed between mean MMT in angular and furcation defects.
Table 3.
Mean residual bone thickness and mucous membrane thickening according to the type of defects
| Variable | Mean±SD | Angular versus furcation | ||
|---|---|---|---|---|
| Angular defects (n=166) | Furcation defects (n=92) | Z# | P# | |
| RBT | 2.779±2.004 | 2.643±1.916 | 0.457 | 0.647NS |
| MMT | 3.189±1.851 | 3.177±1.916 | 0.139 | 0.890NS |
#Mann-Whitney test; NS: P>0.05. NS: Not significant; RBT: Residual bone thickness; MMT: Mucous membrane thickening; SD: Standard deviation
The range of MMT values along the mean value in the three groups can be observed in Graphs 1-3. In Graph 1, we can see an extended range of observations; in fact, maximum observation of MMT when RBT is around 1 mm was noted. Furthermore, in Graph 3, minimum MMT was observed when RBT was between 4.5 mm and 6.5 mm.
Graph 1.

Range of mucous membrane thickening values above and below the mean (4.41 mm) in <2 mm residual bone thickness group.
Graph 3.
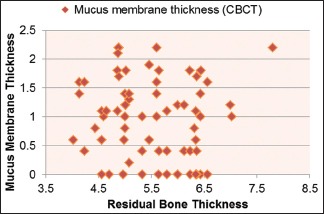
Range of mucous membrane thickening values above and below the mean (0.95 mm) in >4 mm residual bone thickness group.
Graph 2.

Range of mucous membrane thickening values above and below the mean (3.02 mm) in 2–4 mm residual bone thickness group.
DISCUSSION
With this present study results, it appears to be a significant correlation between RBT with MMT. The proportional increase in MMT was observed with a decrease in RBT; this is significant when RBT is <2 mm. Lack of significant difference in MMT between vertical defects and furcation defects supports the importance of RBT than the type of lesion.
According to our knowledge, this is the first study comparing the RBT from the apical-most part of the periodontal defect till the floor of the maxillary sinus with MMT. In previous studies, i.e. Phothikhun et al.[19] and Ren,[20] alveolar bone loss percentage and clinical parameters were used to check the severity of periodontal disease and were proportional to MMT (odds ratio = 3.2 and 4.62, respectively), found a significant association between periodontal disease severity and MMT. Bornstein et al. proposed a possible thickening of bone apical to periapical lesion and thickening of mucus membrane of the maxillary sinus due to the inflammatory reaction.[21] Some authors even proposed the MMT with marginal periodontitis.[5] However, RBT and its relation with MMT were not evaluated in any of these previous studies. In Lane et al.'s opinion, the spread of the microbiota or their toxins from the lesion to the Schneiderian membrane also depends on RBT beneath the maxillary sinus.[6] Hence, RBT and its association with MMT were evaluated.
The prevalence of MMT in this study was 175 out of 258 samples (67.8%). Again, the prevalence is more with <2 mm and 2–4 mm RBT groups (91.2% and 90.2%, respectively). Previously, a large-scale epidemiological study was conducted by Vallo et al.[22] to check MMT due to odontogenic infections, which concluded the prevalence to be 10%–12%; this low value could be attributed to the choice of imaging being orthopantomography (OPG). OPG is a two-dimensional imaging technique and is not as sensitive as CBCT, and three-dimensional imaging techniques are four times more accurate in measuring MMT than two-dimensional imaging techniques.[23] A similar study conducted by Phothikhun et al.[19] calculated periodontal bone loss by OPG and MMT by CBCT and observed the prevalence of MMT to be 42%. usingbased on The higher prevalence in these two studies might be due to the usage of three-dimensional radiographic investigations (CBCT) to check MMT. On considering evidence, in the current study, CBCT was used for assessing both RBT and MMT.
Vertical bony defects and furcation lesions are the indicators for periodontal disease severity. MMT difference between angular and furcation defects was assessed and found to be significant in previous studies.[20,22] Surprisingly, in this study, no significant difference (P = 0.890) was observed between these two groups. Perhaps, it might be because of lack of consideration of RBT in previous studies.
Limitations of the study and future research recommendations
The limitations of the present study were lack of consideration of histological evaluation which is the gold standard for the evaluation of quality of MMT. Some authors propose overemphasizing of the MMT with three-dimensional radiographs compared to histological evaluation.[24] Hence, further research is needed to concentrate on histological sections for evaluating MMT, microbial analysis to support contaminations from periodontal infections to Schneiderian membrane, and quality of the residual bone which is also crucial in preventing the spread of periodontal infection along with thickness.
CONCLUSION
Hence, with this study results, the possibility MMT of the maxillary sinus is increased if RBT is <4 mm. Early detection and prompt periodontal treatments associated with regenerative procedures can be instituted wherever possible to improve RBT beneath the sinus floor to reduce inflammatory reactions in Schneiderian membrane and MMT. Further, microbiological studies are required to confirm the analysis.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
Acknowledgment
We would like to acknowledge Dr. Rahul Dev Goswami, MDS Oral Medicine and Radiology, and Dr. Bhavana Basavaraj, MDS Oral Medicine and Radiology, for their constant support for analyzing radiographic images.
REFERENCES
- 1.Masuda S. Role of the maxillary sinus as a resonant cavity. Nihon Jibiinkoka Gakkai Kaiho. 1992;95:71–80. doi: 10.3950/jibiinkoka.95.71. [DOI] [PubMed] [Google Scholar]
- 2.Dargaud J, Cotton F, Buttin R, Morin A. The maxillary sinus: Evolution and function in aging. Morphologie. 2003;87:17–22. [PubMed] [Google Scholar]
- 3.Chanavaz M. Maxillary sinus: Anatomy, physiology, surgery, and bone grafting related to implantology – Eleven years of surgical experience (1979-1990) J Oral Implantol. 1990;16:199–209. [PubMed] [Google Scholar]
- 4.Radman WP. The maxillary sinus – Revisited by an endodontist. J Endod. 1983;9:382–3. doi: 10.1016/s0099-2399(83)80189-7. [DOI] [PubMed] [Google Scholar]
- 5.Engström H, Chamberlain D, Kiger R, Egelberg J. Radiographic evaluation of the effect of initial periodontal therapy on thickness of the maxillary sinus mucosa. J Periodontol. 1988;59:604–8. doi: 10.1902/jop.1988.59.9.604. [DOI] [PubMed] [Google Scholar]
- 6.Lane JJ, O'Neal RB. The relationship between periodontitis and the maxillary sinus. J Periodontol. 1984;55:477–81. doi: 10.1902/jop.1984.55.8.477. [DOI] [PubMed] [Google Scholar]
- 7.Moskow BS, Polson AM. Histologic studies on the extension of the inflammatory infiltrate in human periodontitis. J Clin Periodontol. 1991;18:534–42. doi: 10.1111/j.1600-051x.1991.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 8.Obayashi N, Ariji Y, Goto M, Izumi M, Naitoh M, Kurita K, et al. Spread of odontogenic infection originating in the maxillary teeth: Computerized tomographic assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:223–31. doi: 10.1016/j.tripleo.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Maloney PL, Doku HC. Maxillary sinusitis of odontogenic origin. J Can Dent Assoc (Tor) 1968;34:591–603. [PubMed] [Google Scholar]
- 10.Fadda GL, Berrone M, Crosetti E, Succo G. Monolateral sinonasal complications of dental disease or treatment: When does endoscopic endonasal surgery require an intraoral approach? Acta Otorhinolaryngol Ital. 2016;36:300–9. doi: 10.14639/0392-100X-904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brook I. Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg. 2006;135:349–55. doi: 10.1016/j.otohns.2005.10.059. [DOI] [PubMed] [Google Scholar]
- 12.Bauer WH. Maxillary sinusitis of dental origin. Am J Orthod Oral Surg. 1943;29:133–51. [Google Scholar]
- 13.Lu Y, Liu Z, Zhang L, Zhou X, Zheng Q, Duan X, et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: A retrospective study. J Endod. 2012;38:1069–74. doi: 10.1016/j.joen.2012.04.027. [DOI] [PubMed] [Google Scholar]
- 14.Ezzodini Ardakani F, Razavi SH, Tabrizizadeh M. Diagnostic value of cone-beam computed tomography and periapical radiography in detection of vertical root fracture. Iran Endod J. 2015;10:122–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Fuhrmann RA, Wehrbein H, Langen HJ, Diedrich PR. Assessment of the dentate alveolar process with high resolution computed tomography. Dento Maxilla Fac Radiol. 1995;24:50–4. doi: 10.1259/dmfr.24.1.8593909. [DOI] [PubMed] [Google Scholar]
- 16.Cymerman JJ, Cymerman DH, O'Dwyer RS. Evaluation of odontogenic maxillary sinusitis using cone-beam computed tomography: Three case reports. J Endod. 2011;37:1465–9. doi: 10.1016/j.joen.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 17.Abrahams JJ, Glassberg RM. Dental disease: A frequently unrecognized cause of maxillary sinus abnormalities? AJR Am J Roentgenol. 1996;166:1219–23. doi: 10.2214/ajr.166.5.8615273. [DOI] [PubMed] [Google Scholar]
- 18.Cagici CA, Yilmazer C, Hurcan C, Ozer C, Ozer F. Appropriate interslice gap for screening coronal paranasal sinus tomography for mucosal thickening. Eur Arch Otorhinolaryngol. 2009;266:519–25. doi: 10.1007/s00405-008-0786-6. [DOI] [PubMed] [Google Scholar]
- 19.Phothikhun S, Suphanantachat S, Chuenchompoonut V, Nisapakultorn K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J Periodontol. 2012;83:557–64. doi: 10.1902/jop.2011.110376. [DOI] [PubMed] [Google Scholar]
- 20.Ren S, Zhao H, Liu J, Wang Q, Pan Y. Significance of maxillary sinus mucosal thickening in patients with periodontal disease. Int Dent J. 2015;65:303–10. doi: 10.1111/idj.12186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bornstein MM, Wasmer J, Sendi P, Janner SF, Buser D, von Arx T, et al. Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: A comparative radiographic analysis using limited cone beam computed tomography. J Endod. 2012;38:51–7. doi: 10.1016/j.joen.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 22.Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: Results from the health 2000 health examination survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e80–7. doi: 10.1016/j.tripleo.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 23.Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:114–9. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Monje A, Diaz KT, Aranda L, Insua A, Garcia-Nogales A, Wang HL, et al. Schneiderian membrane thickness and clinical implications for sinus augmentation: A systematic review and meta-regression analyses. J Periodontol. 2016;87:888–99. doi: 10.1902/jop.2016.160041. [DOI] [PubMed] [Google Scholar]


