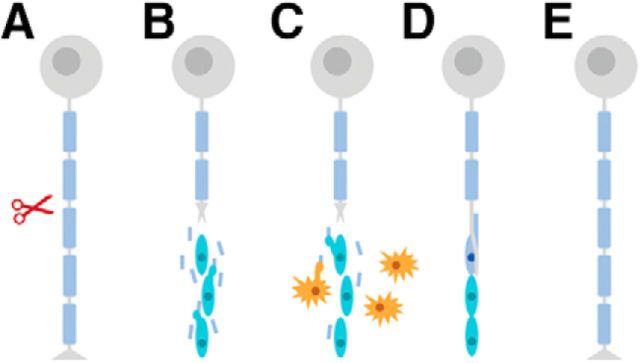
Unlike their counterparts in the CNS, neurons in the peripheral nervous system (PNS) display a remarkable regenerative capacity following injury largely due to Schwann cell (SC) activity, which provides critical support for growth and repair (Fig. 1). After injury (e.g., when the axon is cut or crushed), the distal stump of the injured axon quickly degenerates, leaving myelin ovoids behind (Jung et al., 2011). Myelinating SCs first transition from their mature state to one promoting repair (Jessen and Mirsky, 2016). Next, SCs proliferate and recruit macrophages to the injury site to aid in the clearance of debris (Martini et al., 2008; Chen et al., 2015). Third, repair SCs align along the basal lamina to form Büngner bands, which create a favorable environment for axonal regrowth, and guide the growing axon toward its target. Finally, intrinsic growth factors encourage regrowth of the proximal stump such that the newly regenerating axon makes contact with SCs, which redifferentiate and begin to remyelinate the axon (Chen et al., 2007). In just 3–4 weeks, the structure and function of a damaged neuron are restored in their entirety; yet disruption of any of these myelin functions could critically impair regeneration (Jessen and Mirsky, 2016).
Figure 1.
Schematic timeline of axon injury and regeneration. A, Crush or cut injury to axon (red scissors). B, Myelinating SCs are reprogrammed to repair SCs via downregulation of myelin genes and upregulation of repair genes that promote axon elongation and survival. C, Activation of innate immune response: SCs upregulate cytokines to recruit macrophages (orange). Both macrophages and SCs phagocytose myelin debris. D, Büngner band formation guides regrowing axon to target tissue. Contact with axon signals SCs to revert to myelinating SCs. E, SCs remyelinate axon, which reinnervates target tissue. Gray represents neurons. Blue represents myelinating mature SCs. Cyan represents repair SCs.
The molecular mechanisms by which SCs transition between phenotypes to exert these diverse functions are not fully understood, but they are likely to involve molecules implicated in the maturation of SCs during development. One such class of molecules is the adhesion G-protein coupled receptor (aGPCR) protein family (Bjarnadottir et al., 2007). aGPCRs contain extracellular N termini with multiple adhesion domains. These large adhesion domains suggest that this family of GPCRs is involved in cell–cell communication and cell adhesion, much like cadherins or integrins (Patra et al., 2014). Although aGPCRs are expressed throughout the developing and adult mammalian body, they have been particularly well studied in the context of CNS and PNS myelination (Langenhan et al., 2016). For example, Gpr126 is an evolutionarily conserved regulator of myelination. During development, Gpr126 is thought to regulate cAMP concentration in SCs via interactions with G-proteins, and elevating cAMP in SCs upregulates the expression of myelin-related molecules (Monk et al., 2009, 2011; Mogha et al. 2013; Petersen et al., 2015). These studies established Gpr126 as an essential myelin regulator during development. However, Gpr126 continues to be expressed in SCs postnatally, and its function in mature SCs remains to be determined. Mogha et al. (2016) investigated the role of Gpr126 in the adult PNS in a study recently published in The Journal of Neuroscience.
Because Gpr126 is indispensable for myelin formation during development, Mogha et al. (2016) used an SC-specific, tamoxifen-inducible system to knock out Gpr126 (Gpr126-icKO) in mature SCs. Using this system, Mogha et al. (2016) demonstrated that Gpr126 is not necessary for normal myelin maintenance; knocking out Gpr126 without injuring nerves produced no change in myelination for up to 4 months. Additionally, Gpr126-deficient and control mice showed similar levels of demyelination after injury. The authors subsequently investigated each stage of peripheral nerve degeneration and regeneration to elucidate a function for Gpr126 in the mature PNS.
First, Mogha et al. (2016) asked whether Gpr126 is involved in the transformation of SCs from their mature state to one promoting repair (Fig. 1B). c-Jun, a transcription factor upregulated in SCs after injury, is thought to mediate this transdifferentiation. c-Jun suppresses the expression of myelination-related genes and upregulates neurotrophic factors that contribute to a favorable environment for axon regeneration (Arthur-Farraj et al., 2012). To investigate whether it is Gpr126 that elevates c-Jun expression after injury, Mogha et al. (2016) visualized c-Jun-positive nuclei with immunohistochemistry in control and Gpr126-icKO mice 3 days post injury (dpi). The number of c-Jun nuclei did not differ between groups, and total c-Jun protein levels were elevated after injury in both conditions, although protein levels were significantly less elevated in Gpr126-icKO mice. This finding suggests, but does not provide conclusive evidence, that Gpr126 could be involved in regulating c-Jun levels after injury. Because the inducible knock-out in the Gpr126-icKO model is not 100% efficient, some SCs still express Gpr126. Thus, Mogha et al. (2016) repeated the experiments with an SC-specific conditional knock-out model (cKO-gpr126) in which Gpr126 is deleted in all SCs at embryonic day 12.5, well before myelination occurs (Woodhoo and Sommer, 2008). Inconsistent with the findings from the Gpr126-icKO experiments, c-Jun levels were upregulated after injury in cKO-gpr126 mutants more so than in control animals. They also found that c-Jun was elevated in uninjured cKO-gpr126 mice, indicating that Gpr126 may be important for maintaining low c-Jun levels in an uninjured context. Similar upregulation of c-Jun occurs with the early deletion of another protein necessary for peripheral myelination, Zeb2, which may negatively regulate c-Jun in support of myelin maintenance (Quintes et al., 2016). Although Gpr126 is not required for myelin maintenance, it is possible that it negatively regulates c-Jun in concert with other factors, such that c-Jun is slightly elevated in uninjured nerves and is more significantly upregulated after injury. In any case, it is difficult to interpret the findings in cKO-gpr126 mice because these SCs never form myelin. Ideally, these questions will be addressed with the advent of new methods that more efficiently knock out Gpr126 in all SCs in mature animals.
Next, Mogha et al. (2016) investigated the role of Gpr126 in SC recruitment of macrophages to the injury site (Martini et al., 2008; Chen et al., 2015) (Fig. 1C). Macrophages not only phagocytose debris and secrete factors that degrade dying cells, they also secrete factors important for nerve regeneration (Perry and Brown, 1992). To determine whether macrophage recruitment is altered in the absence of Gpr126, Mogha et al. (2016) quantified macrophages at three time points after injury in control and Gpr126-icKO mice. At 3 and 7dpi, there were significantly fewer macrophages in the Gpr126-icKO mice. By 21 dpi, similar numbers of macrophages were found in both groups of mice, indicating that macrophage recruitment was delayed rather than abolished.
Previous work has demonstrated that SCs recruit macrophages to the damaged nerve by secreting cytokines, such as TNF α, IL-1beta, leukemia inhibitory factor, and MCP-1 (Martini et al., 2008; Brosius et al., 2014). To test whether Gpr126 is required for cytokine signaling, Mogha et al. (2016) compared cytokine expression in WT and cKO-gpr126 nerve tissue at 3 dpi. Of the 84 cytokines assessed, 4 chemokines were significantly downregulated: Ccl2, Ccl3, Cxcl10, and TNF. In other contexts, Ccl2, Ccl3, and Cxcl10 have been implicated in pathways downstream of TNF (Chen et al., 2004; Wang et al., 2012; Qi et al., 2009), and these results suggest that the same might be true in this system. To more definitively establish whether SCs are secreting these factors, future experiments should profile RNA from SCs isolated from injured nerves to determine cytokine expression.
As debris is cleared, repair SCs line the basal lamina and form the Büngner band to guide regenerating axons back to their target tissue (Jessen and Mirsky, 2016) (Fig. 1D). Mogha et al. (2016) hypothesize that these bands might be disrupted in Gpr126 knock-outs because the extracellular matrix proteins laminin-211 and collagen IV are binding partners for Gpr126 (Paavola et al., 2014; Petersen et al., 2015), and proteins such as these are important for glial attachment to the basal lamina (Gao et al., 2013). Furthermore, although the basal lamina tube is not grossly disrupted in Gpr126 mutants, Mogha et al. (2016) note the presence of abnormal loops and outfoldings of basal lamina, visible by transmission electron microscopy. To investigate the possibility that bands are disrupted in the absence of Gpr126, Mogha et al. (2016) visualized regenerating axons at 3 dpi and reinnervation of neuromuscular junction at 12 dpi using immunohistochemistry in Gpr126-icKO and control mice. Axon regeneration and reinnervation were impaired in Gpr126-icKO mice. This impairment is likely independent of myelin debris interference, given that it also occurs in cKO-gpr126 mice, which lack myelin.
Impairments in axon regeneration and reinnervation in Gpr126 knock-outs suggest that Büngner band formation may be disrupted. To confirm this hypothesis, one could inhibit the ability of Gpr126 to bind laminin-211 and collagen IV and assess whether the loss of binding ability prevents axonal regeneration. Future experiments could complement rodent work by using a model system more amenable to in vivo imaging, such as zebrafish, to visualize Gpr126-deficient SCs following injury and observe whether they align into Büngner bands (Xiao et al., 2015).
Finally, Mogha et al. (2016) asked whether Gpr126 is required for remyelination, comparing remyelination in control and Gpr126-icKO mice at 21 and 35 dpi. Mutant SCs failed to remyelinate axons at either time point, a result consistent with the previous finding that Gpr126 is necessary for myelination during development (Mogha et al., 2013). SC remyelination after peripheral nerve injury may mirror developmental gene-expression patterns, and Gpr126 may play a similar role in this system (Chen et al., 2007). However, it is difficult to interpret whether the failure of Gpr126-icKO SCs to remyelinate is directly due to a lack of Gpr126 or whether it stems from problems earlier in the regeneration process, such as the misregulation of c-Jun levels or the disrupted formation of Büngner bands. Because Gpr126 influences myelination during development by regulating the concentration of cAMP in SCs (Monk et al., 2009, 2011; Mogha et al., 2013; Petersen et al., 2015), a better understanding of cAMP expression after injury could clarify the role of Gpr126 in remyelination. As Mogha et al. (2016) note, future experiments that precisely measure cAMP levels during regeneration will be critical to elucidate this process.
In conclusion, Mogha et al. (2016) demonstrate that Gpr126 is required in SCs for several aspects of peripheral nerve repair. Without Gpr126, c-Jun levels are misregulated and inappropriately elevated after injury. Additionally, macrophage recruitment is delayed, possibly due to the downregulation of several chemokines, and this may potentially impair clearance of axon debris. Finally, axon regeneration and reinnervation are impaired and remyelination is absent. These results highlight the elaborately choreographed nature of peripheral nerve repair, which involves simultaneous interactions of many molecules and diverse cell types. Future work will build off of these findings to tease apart which elements are causative. For example, does Gpr126 drive remyelination directly, or is remyelination impaired because axons fail to regrow? Can Gpr126 be targeted to promote remyelination? If so, Gpr126 could be a promising therapeutic target for peripheral neuropathies, congenital muscular dystrophy, and other myelin disorders.
Footnotes
Editor's Note: These short reviews of recent JNeurosci articles, written exclusively by students or postdoctoral fellows, summarize the important findings of the paper and provide additional insight and commentary. If the authors of the highlighted article have written a response to the Journal Club, the response can be found by viewing the Journal Club at www.jneurosci.org. For more information on the format, review process, and purpose of Journal Club articles, please see http://jneurosci.org/content/preparing-manuscript#journalclub
We thank Aaron Gitler and Nick Kramer for thoughtful comments on this review article.
The authors declare no competing financial interests.
References
- Arthur-Farraj PJ, Latouche M, Wilton DK, Quintes S, Chabrol E, Banerjee A, Woodhoo A, Jenkins B, Rahman M, Turmaine M, Wicher GK, Mitter R, Greensmith L, Behrens A, Raivich G, Mirsky R, Jessen KR (2012) c-Jun reprograms Schwann cells of injured nerves to generate a repair cell essential for regeneration. Neuron 75:633–647. 10.1016/j.neuron.2012.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjarnadóttir TK, Fredriksson R, Schioth HB (2007) The adhesion GPCRs: a unique family of G protein-coupled receptors with important roles in both central and peripheral tissues. Cell Mol Life Sci 16:2104–2119. 10.1007/s00018-007-7067-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosius Lutz A, Barres BA (2014) Contrasting the glial response to axon injury in the central and peripheral nervous system. Dev Cell 28:7–17. 10.1016/j.devcel.2013.12.002 [DOI] [PubMed] [Google Scholar]
- Chen P, Piao X, Bonaldo P (2015) Role of macrophages in Wallerian degeneration and axonal regeneration after peripheral nerve injury. Acta Neuropathol 130:605–618. 10.1007/s00401-015-1482-4 [DOI] [PubMed] [Google Scholar]
- Chen YM, Chiang WC, Lin SL, Wu KD, Tsai TJ, Hsieh BS (2004) Dual regulation of tumor necrosis factor-alpha-induced CCL2/monocyte chemoattractant protein-1 expression in vascular smooth muscle cells by nuclear factor-kappaB and activator protein-1: modulation by type III phosphodiesterase inhibition. J Pharmacol Exp Ther 309:978–986. 10.1124/jpet.103.062620 [DOI] [PubMed] [Google Scholar]
- Chen ZL, Yu WM, Strickland S (2007) Peripheral regeneration. Annu Rev Neurosci 30:209–233. 10.1146/annurev.neuro.30.051606.094337 [DOI] [PubMed] [Google Scholar]
- Gao X, Wang Y, Chen J, Peng J (2013) The role of peripheral nerve ECM components in the tissue engineering nerve construction. Rev Neurosci 24:443–453. 10.1515/revneuro-2013-0022 [DOI] [PubMed] [Google Scholar]
- Jessen KR, Mirsky R (2016) The repair Schwann cell and its function in regenerating nerves. J Physiol 594:3521–3531. 10.1113/JP270874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung J, Cai W, Lee HK, Pellegatta M, Shin YK, Jang SY, Suh DJ, Wrabetz L, Feltri ML, Park HT (2011) Actin polymerization is essential for myelin sheath fragmentation during Wallerian degeneration. J Neurosci 31:2009–2015. 10.1523/JNEUROSCI.4537-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langenhan T, Piao X, Monk KR (2016) Adhesion G protein-coupled receptors in nervous system development and disease. Nat Rev Neurosci 17:550–561. 10.1038/nrn.2016.86 [DOI] [PubMed] [Google Scholar]
- Martini R, Fischer S, López-Vales R, David S (2008) Interactions between Schwann cells and macrophages in injury and inherited demyelinating disease. Glia 56:1566–1577. 10.1002/glia.20766 [DOI] [PubMed] [Google Scholar]
- Mogha A, Benesh AE, Patra C, Engel FB, Schöneberg T, Liebscher I, Monk KR (2013) Gpr126 functions in Schwann cells to control differentiation and myelination via G-protein activation. J Neurosci 33:17976–17985. 10.1523/JNEUROSCI.1809-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogha A, Harty BL, Carlin D, Joseph J, Sanchez NE, Suter U, Piao X, Cavalli V, Monk KR (2016) Gpr126/Adgrg6 has Schwann cell autonomous and nonautonomous functions in peripheral nerve injury and repair. J Neurosci 36:12351–12367. 10.1523/JNEUROSCI.3854-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk KR, Naylor SG, Glenn TD, Mercurio S, Perlin JR, Dominguez C, Moens CB, Talbot WS (2009) A G protein-coupled receptor is essential for Schwann cells to initiate myelination. Science 325:1402–1405. 10.1126/science.1173474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk KR, Oshima K, Jörs S, Heller S, Talbot WS (2011) Gpr126 is essential for peripheral nerve development and myelination in mammals. Development 138:2673–2680. 10.1242/dev.062224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paavola KJ, Sidik H, Zuchero JB, Eckart M, Talbot WS (2014) Type IV collagen is an activating ligand for the adhesion G protein-coupled receptor GPR126. Sci Signal 7:ra76. 10.1126/scisignal.2005347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra C, Monk KR, Engel FB (2014) The multiple signaling modalities of adhesion G protein-coupled receptor GPR126 in development. Receptors Clin Investig 1:79. 10.14800/rci.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry VH, Brown MC (1992) Role of macrophages in peripheral nerve degeneration and repair. Bioessays 14:401–406. 10.1002/bies.950140610 [DOI] [PubMed] [Google Scholar]
- Petersen SC, Luo R, Liebscher I, Giera S, Jeong SJ, Mogha A, Ghidinelli M, Feltri ML, Schöneberg T, Piao X, Monk KR (2015) The adhesion GPCR GPR126 has distinct, domain dependent functions in Schwann cell development mediated by interaction with Laminin-211. Neuron 85:755–769. 10.1016/j.neuron.2014.12.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi XF, Kim DH, Yoon YS, Jin D, Huang XZ, Li JH, Deung YK, Lee KJ (2009) Essential involvement of cross-talk between IFN-gamma and TNF-alpha in CXCL10 production in human THP-1 monocytes. J Cell Physiol 220:690–697. 10.1002/jcp.21815 [DOI] [PubMed] [Google Scholar]
- Quintes S, Brinkmann BG, Ebert M, Fröb F, Kungl T, Arlt FA, Tarabykin V, Huylebroeck D, Meijer D, Suter U, Wegner M, Sereda MW, Nave KA (2016) Zeb2 is essential for Schwann cell differentiation, myelination and nerve repair. Nat Neurosci 19:1050–1059. 10.1038/nn.4321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Tang D, Shu B, Wang B, Jin H, Hao S, Dresser KA, Shen J, Im HJ, Sampson ER, Rubery PT, Zuscik MJ, Schwarz EM, O'Keefe RJ, Wang Y, Chen D (2012) Conditional activation of beta-catenin signaling in mice leads to severe defects in intervertebral disc tissue. Arthritis Rheum 64:2611–2623. 10.1002/art.34469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodhoo A, Sommer L (2008) Development of the Schwann cell lineage: from the neural crest to the myelinated nerve. Glia 56:1481–1490. 10.1002/glia.20723 [DOI] [PubMed] [Google Scholar]
- Xiao Y, Faucherre A, Pola-Morell L, Heddleston JM, Liu TL, Chew TL, Sato F, Sehara-Fujisawa A, Kawakami K, López-Schier H (2015) High-resolution live imaging reveals axon–glia interactions during peripheral nerve injury and repair in zebrafish. Dis Model Mech 8:553–564. 10.1242/dmm.018184 [DOI] [PMC free article] [PubMed] [Google Scholar]