Abstract
Aim
To in detail delineate sex differences in non-small cell lung cancer outcome and investigate possible underlying drivers.
Methods
We performed a nationwide, population-based cohort study using data on all incident cases of lung squamous cell carcinoma (n = 10,325) and adenocarcinoma (n = 23,465) recorded in the Swedish Lung Cancer Register in 2002–2016. Flexible parametric models were applied to compute adjusted female-to-male hazard ratios (aHRs) and standardized survival proportions over follow-up including age, calendar year, education, marital status, birth country, health care region, performance status, smoking history, comorbidities, and tumor location in the final model.
Results
Women presented with better performance status, were younger, and more often never-smokers. Women with adenocarcinoma also had lower comorbidity burden, less advanced stage, and were more often EGFR positive. Men with adenocarcinoma had a consistently poorer lung cancer-specific survival across stage; HR 0.69; 95% CI 0.63–0.76 (stage IA-IIB) to 0.94; 95% CI 0.88–0.99 (stage IIIB-IV), remaining largely unchanged after adjustments; aHR 0.74; 95% CI 0.66–0.82 to 0.84; 95% CI 0.81–0.87. The same pattern was observed in squamous cell carcinoma, except in stage IIIA disease, where we found no sex differences in survival.
Conclusions
Men with non-small cell lung cancer have a consistently poorer prognosis, even after careful adjustments for a wide range of prognostic factors. While the pattern was similar in both squamous cell and adenocarcinoma, it was larger and more consistent in the latter.
Introduction
Converging evidence from studies conducted in different geographic regions demonstrate that men with non-small cell lung cancer (NSCLC) have a poorer prognosis compared to women [1–11]. The inferior male survival in NSCLC appears to be consistent over calendar time and across the two major histological types; squamous cell and adenocarcinoma. It has become increasingly apparent that these two subtypes represent separate clinical entities with different epidemiology, treatment, and prognosis [12].
Prognostic factors in NSCLC encompass stage, tumor location, number of examined lymph nodes, nodal station involvement, tumor biology and molecular characteristics (histology, grade, proliferation rate, pleural and vascular invasion, mutational status), number and location of metastasis, treatment, age, smoking history, socioeconomic status, ethnicity, comorbidity, performance status, presence of pulmonary symptoms, and weight loss [1, 2, 5, 8, 13–16]. The underlying reasons behind the male excess mortality remain incompletely understood [6, 17, 18].
The aim of the present study was firstly to in detail characterize and quantify sex differences in non-small cell lung cancer outcome. Secondly, to investigate a wide range of possible factors contributing to these differences.
Materials and methods
Data sources and covariates
We performed a population-based cohort study using prospectively collected data from the Lung Cancer DataBase Sweden (LcBaSE) from 2002 until 2016. LcBaSE is a research database containing detailed patient-level data from several nationwide registers, including the Swedish National Lung Cancer Register (NLCR), the Swedish Cancer Register, the National Patient Register, the Prescribed Drug Register, the Longitudinal Integration Database for Health Insurance and Labor Market Studies (LISA), the Cause of Death Register, and the Total Population Register [19, 20]. The national registration number, a personal identifier assigned to all residents of Sweden, enabled individual-level record linkages between registers [21].
The NLCR started in 2002 and aims to include all Swedish residents diagnosed with invasive lung cancer according to the International Classification of Diseases for Oncology code C34. Postmortem diagnoses, carcinoma in situ, tracheal, and pleural tumors are not included. The completeness compared to the mandatory Swedish Cancer Register is 96% [19, 20]. The NLCR records clinicopathological factors at diagnosis as well as diagnostic investigations and primary treatment [19]. We applied the Elixhauser method to assess comorbidity burden using data on main and secondary diagnoses at discharge from hospital from the National Patient Register and data on other malignancies from the Swedish Cancer Register, 15 years—1 month before lung cancer diagnosis [20, 22]. Coding was according to the International Classification of Diseases revision 9 (year 1987–1996) and 10 (year 1997–2016). The Elixhauser approach is considered valid and reliable and was applied in its original form, treating the 31 comorbidity groups as independent, binary variables [22, 23]. Additional measures of comorbidity, including number of medications prescribed 6–18 months before NSCLC diagnosis, grouped according to the first three positions of the Anatomical Therapeutic Chemical Classification, number of in- and outpatient visits 6–18 months before diagnosis, and the Charlson Comorbidity Index, were explored. Educational level and marital status were acquired from the LISA database. Date and cause of death were retrieved from the Cause of Death register. Information on emigration was ascertained from the Total Population Register.
Inclusion criteria included a first record of lung cancer, squamous cell or adenocarcinoma histopathology, year of diagnosis 2002–2016, and age at diagnosis 20 years or older (n = 34,003). More rare histologic types of non-small cell lung cancer (large cell carcinomas, carcinoid tumors, adenosquamous carcinomas, sarcomatoid carcinomas, salivary gland-type tumors, and unclassified carcinomas) were not included. Histologically unverified cases (n = 110) and cases with missing date of birth (n = 102) were excluded. This way, the final study population encompassed 33,790 men and women with NSCLC (S1 Fig). Staging was based on the tumor-node-metastasis (TNM) system by the American Joint Committee on Cancer, the 6th revision up until 2010 when the 7th revision was introduced in clinical practice [24].
Statistical analyses
All analyses were stratified on histology. Analyses on treatment and mortality were additionally stratified into early (IA-IIB), locally advanced (IIIA), and late (IIIB-IV) stage disease, based on treatment guidelines.[25] Numbers and percentages of missing data were low (0–3.7%) and similar between sexes; the missing indicator approach was applied to not exclude these cases from multivariable analyses.
The frequency of clinicopathological characteristics at diagnosis, including calendar period, level of education, age, ECOG performance status, smoking history, Elixhauser comorbidities, TNM stage, and EGFR mutation status (advanced stage adenocarcinoma, years 2010–2016) were calculated for men and women. The Pearson chi-square test was applied to compare distributions.
To quantify sex differences in diagnostic and treatment intensity, we used logistic regression with robust standard errors to compute odds ratios (OR) with 95% confidence intervals (CI) for each modality. Treatment-on-time was defined as treatment initiation or decision within 28 days from referral to specialist care. For each diagnostic/treatment modality we ran two models, the first included age and year of diagnosis (OR), and the second (aOR) also incorporated educational level, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidities, TNM stage, and primary tumor location.
Date of diagnosis was defined as the date of histopathological or cytological sample collection. Survival time was calculated from date of diagnosis until date of death, emigration, or end of follow-up (December 31, 2017), whichever occurred first. Lung cancer-specific death was defined as C34 according to the 10th revision of the International Classification of Diseases. Flexible parametric models were applied to estimate female-to-male hazard ratios (HR) with 95% confidence intervals (CI) [26]. As a sensitivity analysis we explored the effects of several confounders by including them sequentially, evaluating the effect on the HR. All survival models included age and year of diagnosis (HR), the fully adjusted model (aHR) also included level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location. We performed a subgroup analysis of patients diagnosed with lung adenocarcinoma in 2010–2016 tested for EGFR, and fitted a third model, additionally adjusted for EGFR mutational status. Further sensitivity analyses were employed to explore effect modification and model fit including interaction between sex and selected covariates.
In addition to Kaplan-Meier survival curves, we estimated standardized survival proportions for men and women over follow-up including the absolute difference (women-men) in survival at 1, 3 and 5 years after diagnosis, with 95% CI, using fully-adjusted flexible parametric models [26]. This approach predicts one survival curve for each individual in the strata under study and averages these to create two standardized survival curves were the only differences is that in one everyone is exposed (male sex) and in the other one unexposed (female sex) [27]. The baseline hazard function was fitted using restricted cubic splines with 5 degrees of freedom, generating 4 interior knots placed at the 20th, 40th, 60th, and 80th percentile. To allow for non-proportional hazards, the time-dependent effect of sex was fitted using restricted cubic splines with 3 degrees of freedom.
All statistical analyses were performed using Stata Intercooled version 15.1 (StataCorp LP). The Stata commands stpm2 and stpm2_standsurv were used when applying flexible parametric models [26]. This study was approved by the regional Ethical Review Committee in Stockholm (2012/1162-31/4; 2016/1137-32; 2017/445-32).
Results
We identified 33,790 men and women with a diagnosis of lung squamous cell (n = 10,325) or adenocarcinoma (n = 23,465). Table 1 summarizes clinicopathological factors by histology and sex (S1 Table summarizes all investigated factors). While the incidence of lung adenocarcinoma increased overall, the incidence of squamous cell carcinoma decreased in men and increased in women. In both subtypes, women had a higher education, were more often never-smokers, younger, and presented with better performance status at diagnosis, compared to men. In adenocarcinoma, women also had a lower comorbidity burden, presented with less advanced stage, and more often had EGFR positive tumors. In general sex differences were less pronounced in squamous cell than in adenocarcinoma.
Table 1. Clinical characteristics at diagnosis.
| Squamous cell carcinoma | Adenocarcinoma | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | p-value | Men | Women | p-value | |||||
| n | % | n | % | n | % | n | % | |||
| All cases | 6556 | 100.0 | 3769 | 100.0 | 10795 | 100.0 | 12670 | 100.0 | ||
| Calendar period | ||||||||||
| 2002–2006 | 2225 | 33.9 | 1119 | 29.7 | 2695 | 25.0 | 2882 | 22.7 | ||
| 2007–2011 | 2200 | 33.6 | 1262 | 33.5 | 3671 | 34.0 | 4241 | 33.5 | ||
| 2012–2016 | 2131 | 32.5 | 1388 | 36.8 | <0.001 | 4429 | 41.0 | 5547 | 43.8 | <0.001 |
| Education | ||||||||||
| Low | 3235 | 49.3 | 1751 | 46.5 | 4559 | 42.2 | 4808 | 37.9 | ||
| Middle | 2383 | 36.3 | 1495 | 39.7 | 4230 | 39.2 | 5427 | 42.8 | ||
| High | 762 | 11.6 | 452 | 12.0 | 1809 | 16.8 | 2273 | 17.9 | ||
| missing | 176 | 2.7 | 71 | 1.9 | <0.001 | 197 | 1.8 | 162 | 1.3 | <0.001 |
| Age | ||||||||||
| 0–59 | 659 | 10.1 | 445 | 11.8 | 1551 | 14.4 | 2344 | 18.5 | ||
| 60–69 | 2002 | 30.5 | 1168 | 31.0 | 3702 | 34.3 | 4571 | 36.1 | ||
| 70–79 | 2711 | 41.4 | 1521 | 40.4 | 3966 | 36.7 | 4106 | 32.4 | ||
| 80–89 | 1148 | 17.5 | 612 | 16.2 | 1501 | 13.9 | 1562 | 12.3 | ||
| 90+ | 36 | 0.5 | 23 | 0.6 | 0.04 | 75 | 0.7 | 87 | 0.7 | <0.001 |
| ECOG performance status | ||||||||||
| 0 | 1126 | 17.2 | 629 | 16.7 | 2501 | 23.2 | 3514 | 27.7 | ||
| 1 | 2528 | 38.6 | 1553 | 41.2 | 3998 | 37.0 | 4829 | 38.1 | ||
| 2 | 1502 | 22.9 | 875 | 23.2 | 2183 | 20.2 | 2276 | 18.0 | ||
| 3 | 886 | 13.5 | 465 | 12.3 | 1256 | 11.6 | 1264 | 10.0 | ||
| 4 | 272 | 4.1 | 139 | 3.7 | 455 | 4.2 | 448 | 3.5 | ||
| missing | 242 | 3.7 | 108 | 2.9 | 0.02 | 402 | 3.7 | 339 | 2.7 | <0.001 |
| Smoking history | ||||||||||
| Smoker | 3120 | 47.6 | 1976 | 52.4 | 4109 | 38.1 | 5120 | 40.4 | ||
| Former smoker | 3160 | 48.2 | 1470 | 39.0 | 5336 | 49.4 | 4957 | 39.1 | ||
| Never-smoker | 165 | 2.5 | 253 | 6.7 | 1147 | 10.6 | 2384 | 18.8 | ||
| missing | 111 | 1.7 | 70 | 1.9 | <0.001 | 203 | 1.9 | 209 | 1.6 | <0.001 |
| Elixhauser comorbidities | ||||||||||
| 0 | 2261 | 34.5 | 1386 | 36.8 | 4196 | 38.9 | 5557 | 43.9 | ||
| 1–2 | 2628 | 40.1 | 1469 | 39.0 | 4171 | 38.6 | 4842 | 38.2 | ||
| 3–4 | 1151 | 17.6 | 628 | 16.7 | 1703 | 15.8 | 1617 | 12.8 | ||
| 5+ | 516 | 7.9 | 286 | 7.6 | 0.13 | 725 | 6.7 | 654 | 5.2 | <0.001 |
| Stage | ||||||||||
| IA-IIB | 1827 | 27.9 | 1125 | 29.8 | 2470 | 22.9 | 3387 | 26.7 | ||
| IIIA | 892 | 13.6 | 519 | 13.8 | 762 | 7.1 | 987 | 7.8 | ||
| IIIB-IV | 3703 | 56.5 | 2069 | 54.9 | 7398 | 68.5 | 8143 | 64.3 | ||
| missing | 134 | 2.0 | 56 | 1.5 | 0.04 | 165 | 1.5 | 153 | 1.2 | <0.001 |
| EGFR mutation* | ||||||||||
| Positive | - | - | - | - | 221 | 5.5 | 472 | 10.3 | ||
| Negative | - | - | - | - | 1880 | 46.5 | 2159 | 47.1 | ||
| Inconclusive | . | - | - | - | 157 | 3.9 | 210 | 4.6 | ||
| Pending | - | - | - | - | 23 | 0.6 | 34 | 0.7 | ||
| not tested | - | - | - | - | 1765 | 43.6 | 1713 | 37.3 | <0.001 | |
*Stage IIIB-IV, year of diagnosis 2010–2016
When comparing diagnostic intensity as well as if primary treatment was decided and/or commenced within three weeks from referral to a specialist unit, in men and women (S2 Table), absolute differences were minor and statistically significant only for a few procedures.
Sex differences in treatment are presented in Table 2. Investigated treatment modalities included surgery and hypofractionated radiotherapy (2007–2016) in early stage; surgery, chemo-radiotherapy (2007–2016), and radiotherapy in locally advanced stage; and systemic therapy, radiotherapy, and chemo-radiotherapy (2007–2016) in late stage disease. We found no evidence of unequal treatment of Swedish men and women with NSCLC, with the exception of chemo-radiotherapy being marginally more common in men with late stage adenocarcinoma (20.2 vs 17.9%, aOR 1.14, 95% CI 1.01–1.29).
Table 2. Treatment intensity.
| Squamous cell carcinoma | |||||||
| Men | Women | ||||||
| n | % | OR (95% CI) | n | % | OR (95% CI)1 | aOR (95% CI)2 | |
| Stage IA-IIB | |||||||
| Surgery | 1063 | 58.2 | 1.00 (ref.) | 683 | 60.7 | 1.04 [0.88,1.22] | 0.92 [0.74,1.15] |
| Hypofractioned radiotherapy* | 137 | 11.2 | 1.00 (ref.) | 108 | 13.4 | 1.25 [0.95,1.65] | 1.16 [0.82,1.63] |
| Stage IIIA | |||||||
| Surgery | 94 | 10.5 | 1.00 (ref.) | 58 | 11.2 | 1.05 [0.74,1.50] | 1.05 [0.70,1.58] |
| Chemo-radiotherapy* | 287 | 45.5 | 1.00 (ref.) | 177 | 44.1 | 0.94 [0.72,1.22] | 1.02 [0.73,1.43] |
| Radiotherapy | 242 | 27.1 | 1.00 (ref.) | 117 | 22.5 | 0.88 [0.68,1.15] | 0.89 [0.65,1.23] |
| Stage IIIB-IV | |||||||
| Chemotherapy | 2149 | 58.0 | 1.00 (ref.) | 1240 | 59.9 | 1.06 [0.94,1.19] | 1.08 [0.92,1.25] |
| Radiotherapy primary tumor | 572 | 15.4 | 1.00 (ref.) | 328 | 15.9 | 1.11 [0.95,1.30] | 1.11 [0.94,1.31] |
| Chemo-radiotherapy* | 488 | 20.2 | 1.00 (ref.) | 254 | 17.9 | 0.85 [0.73,1.01] | 0.89 [0.73,1.08] |
| Adenocarcinoma | |||||||
| Men | Women | ||||||
| n | % | OR (95% CI) | n | % | OR (95% CI)1 | aOR (95% CI)2 | |
| Stage IA-IIB | |||||||
| Surgery | 1816 | 73.5 | 1.00 (ref.) | 2626 | 77.5 | 1.11 [0.97,1.27] | 0.96 [0.81,1.14] |
| Hypofractioned radiotherapy* | 242 | 12.7 | 1.00 (ref.) | 299 | 11.1 | 0.97 [0.80,1.17] | 0.96 [0.76,1.20] |
| Stage IIIA | |||||||
| Surgery | 151 | 19.8 | 1.00 (ref.) | 226 | 22.9 | 1.15 [0.91,1.46] | 1.19 [0.90,1.58] |
| Chemo-radiotherapy* | 311 | 50.3 | 1.00 (ref.) | 385 | 47.4 | 0.84 [0.68,1.05] | 0.86 [0.67,1.10] |
| Radiotherapy | 130 | 17.1 | 1.00 (ref.) | 137 | 13.9 | 0.78 [0.58,1.03] | 0.80 [0.57,1.11] |
| Stage IIIB-IV | |||||||
| Chemotherapy | 4820 | 65.2 | 1.00 (ref.) | 5475 | 67.2 | 1.05 [0.98,1.13] | 0.97 [0.88,1.06] |
| Radiotherapy primary tumor | 509 | 6.9 | 1.00 (ref.) | 493 | 6.1 | 0.90 [0.79,1.02] | 0.89 [0.77,1.02] |
| Chemo-radiotherapy* | 551 | 10.1 | 1.00 (ref.) | 716 | 11.6 | 1.14 [1.02,1.27] | 1.14 [1.01,1.29] |
Numbers (n), percentages (%) of male and female NSCLC patients, and female-to-male odds ratios (ORs) with 95% confidence intervals (CI), undergoing treatment by histological type and stage.
1Adjusted for age and calendar year of diagnosis.
2Additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location.
*Year 2007–2016.
Table 3 shows numbers and percentages of lung cancer deaths in men and women as well as lung cancer-specific female-to-male HR by histology and stage. Overall, there were very small differences between the basic HR and the fully adjusted aHR. Women had a consistently better prognosis with the exception of squamous cell carcinoma stage IIIA. Sex differences in lung cancer mortality were most pronounced in early and locally advanced adenocarcinoma, aHR 0.74 (95% CI 0.66–0.82) and 0.77 (95% CI 0.67–0.88), respectively. In the subgroup analysis of lung adenocarcinomas tested for EGFR, the female-to-male hazard ratio remained unaltered in the models adjusted for sex differences in EGFR mutational status (S3 Table).
Table 3. Lung cancer-specific mortality.
| Squamous cell carcinoma | ||||
| n | % | HR1 (95% CI) | aHR2 (95% CI) | |
| Stage IA-IIB | ||||
| Men | 844 | 46.2 | 1.00 | 1.00 |
| Women | 448 | 39.8 | 0.81 [0.72,0.92] | 0.80 [0.70,0.92] |
| Stage IIIA | ||||
| Men | 599 | 67.2 | 1.00 | 1.00 |
| Women | 364 | 70.1 | 1.06 [0.93,1.21] | 1.04 [0.90,1.21] |
| Stage IIIB-IV | ||||
| Men | 3120 | 84.3 | 1.00 | 1.00 |
| Women | 1713 | 82.8 | 0.94 [0.88,0.99] | 0.87 [0.81,0.92] |
| Adenocarcinoma | ||||
| n | % | HR1 (95% CI) | aHR2 (95% CI) | |
| Stage IA-IIB | ||||
| Men | 875 | 35.4 | 1.00 | 1.00 |
| Women | 943 | 27.8 | 0.69 [0.63,0.76] | 0.74 [0.66,0.82] |
| Stage IIIA | ||||
| Men | 475 | 62.3 | 1.00 | 1.00 |
| Women | 602 | 61.1 | 0.81 [0.71,0.91] | 0.77 [0.67,0.88] |
| Stage IIIB-IV | ||||
| Men | 6167 | 83.4 | 1.00 | 1.00 |
| Women | 6672 | 81.9 | 0.94 [0.88,0.99] | 0.84 [0.81,0.87] |
Numbers (n), percentages (%) of lung cancer deaths in male and female NSCLC patients, and female-to-male hazard ratios (HRs) with 95% confidence intervals (CI) by histological type and stage.
1Adjusted for age and calendar year of diagnosis.
2Additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location.
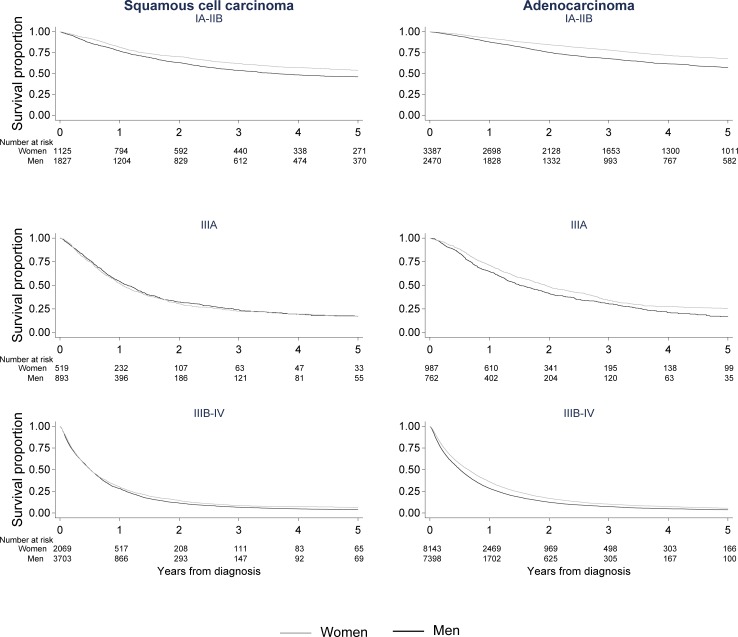
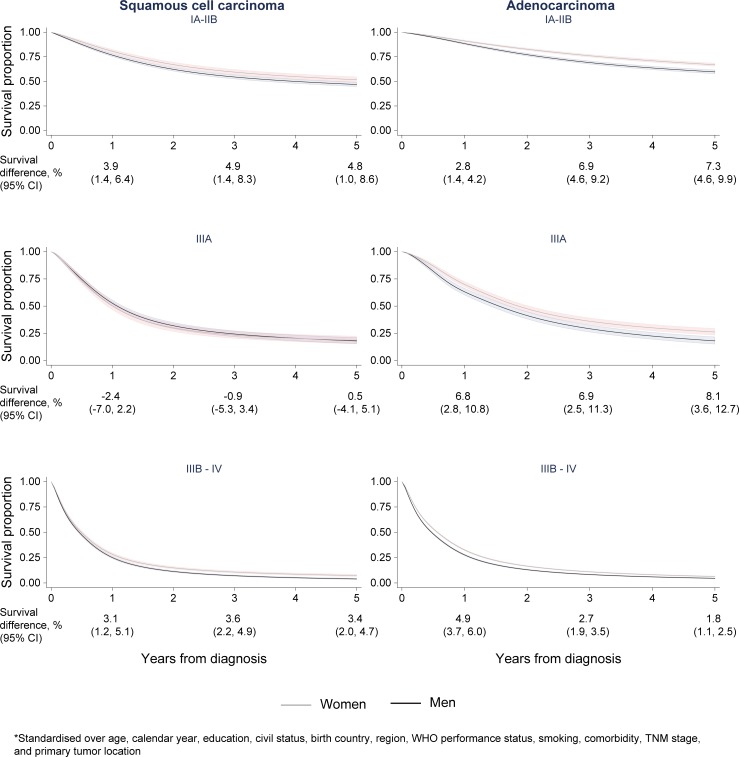
The results in Table 3 are reflected in the Kaplan-Meier curves (Fig 1). Across stage, men with pulmonary adenocarcinoma experienced poorer lung cancer-specific survival. The pattern was similar for squamous cell carcinoma, with the exception of stage IIIA disease where no sex difference in survival was observed. Similarly, the survival curves generated from multivariable, flexible parametric models (Fig 2) showed a significantly, poorer prognosis in men compared to women consistent over histology, stage, and follow-up, with the exception of squamous cell carcinoma stage IIIA. Absolute differences in survival proportions (women-men) were most pronounced 5 years after diagnosis and in early (IA-IIB) 7.3% (95% CI 4.6–9.9) and advanced (IIIA) stage 8.1% (95% CI 3.6–12.7) adenocarcinoma.
Fig 1. Lung cancer-specific survival (Kaplan-Meier).
Lung cancer-specific survival proportion for men and women diagnosed with lung squamous cell and adenocarcinoma by follow-up time (years), stratified on stage group; IA-IIB, IIIA, IIIB-IV.
Fig 2. Standardized lung cancer-specific survival.
Lung cancer-specific survival proportion including 95% confidence intervals for men and women diagnosed with lung squamous cell and adenocarcinoma by follow-up time (years), stratified on stage group; IA-IIB, IIIA, IIIB-IV, and standardized over age, calendar year, level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location.
Results from the sensitivity analysis where each prognostic factor was added sequentially (S2 Fig) revealed that HR estimates remained largely unchanged following statistical adjustments for various clinicopathological factors including the Charlson Comorbidity Index. Additional sensitivity analysis exploring interaction between sex and selected covariates (S4 Table) showed that the female survival advantage in lung adenocarcinoma was remarkably stable with the exception of a possible interaction between sex and smoking history. In squamous cell carcinoma no consistent pattern in combination with superior model fit was seen when allowing for interaction in the model. Results from flexible parametric and Cox regression models were nearly identical (S5 Table).
Discussion
Using data from a large, nationwide population-based lung cancer cohort, we demonstrate that male sex represents an independent, negative prognostic factor in NSCLC. Men with lung adenocarcinoma had a poorer prognosis than women regardless of stage. In lung squamous cell carcinoma the male survival disadvantage was demonstrated in all stage groups, except IIIA. Overall, the effect of careful adjustments for a wide range of prognostic factors was very small if any, supporting the notion that the poorer survival of men with NSCLC reflects yet to be identified sex differences in tumor biology. We found no evidence of unequal clinical management between men and women with NSCLC.
To our knowledge, this is the largest study to date addressing sex differences in NSCLC management and outcome covering individual-level data on a comparable quantity and range of ascertained covariates. The Swedish national registration number enabled record-linkages between the NLCR and other population-based registers and allowed for a complete, unbiased and long-term follow-up. Taken together, the population-based setting, the completeness, and the high data quality ensured the robustness of our approach. We believe that the use of flexible parametric models incorporating relevant confounders to quantify and illustrate mortality and survival in relative as well as absolute measures is preferential in observational studies of cancer survival.
Several limitations deserve mentioning. Despite the inclusion of a wide range of relevant covariates, we did not have access to individual-level data on every established prognostic factor, and data on EGFR and ALK mutations was limited to year 2010–2016 and 2016, respectively. All register-based studies may suffer from misclassification, under-reporting and under-diagnosis, it is however unlikely that these biases would differ substantially between men and women. That said, stage migration, due to revision of the TNM classification and introduction of new diagnostic measures in routine work-up, over time is a potential concern [28]. ECOG performance status is based on a subjective assessment of functional activity at diagnosis and possibly affected by gender-related preconceptions. Smoking history was self-reported, vulnerable to response bias, and did not consider number of pack-years. The comorbidity burden was likely underestimated since the Elixhauser groups were based on discharge records from hospitalizations and did not capture comorbidity in patients not admitted to in-hospital care. The inconsistent findings in locally advanced squamous cell carcinoma are difficult to fully explain. It should be noted that this is a heterogeneous group regarding prognosis as well as treatment, and also the smallest subgroup, adding to the difficulty interpreting results.
Our findings corroborate results from prior studies examining sex differences in NSCLC including a higher proportion of adenocarcinoma in women and squamous cell carcinoma in men. As in earlier studies, we found that women with NSCLC were more often never-smokers, diagnosed at an earlier stage and at younger age than men [2, 3, 8, 9, 17, 18]. Our findings of a female survival advantage being particularly pronounced in early stage NSCLC in general and lung adenocarcinoma in particular, have also been reported previously [7, 9, 29–31]. Previous studies further suggested that female sex is an independent favorable prognostic factor in NSCLC [2–7, 11, 13, 16, 32, 33]. The largest study to date included approximately 200,000 lung cancer patients from the SEER database, reported similar findings, but did not include prognostic factors like comorbidity, performance status, smoking history, educational level, and marital status [3]. The few studies reporting comparable or poorer survival in women have been based on small numbers with results likely to have been influenced by substandard treatment in women [34, 35].
In conclusion, we found a higher lung cancer-specific mortality in men with NSCLC that remained largely unchanged following adjustments for a wide range of prognostic factors. Our results provide no evidence of sex differences in the clinical management of NSCLC in Sweden. Taken together, this indicates that the drivers of differences in NSCLC survival between men and women reflect yet to be identified biological sex differences that most probably differ between histological types of NSCLC. With the reservation of limited follow-up time and lacking data on EGFR targeted therapy, adjusting for EGFR mutational status, a prognostic/predictive factor, in a subgroup analysis did not alter our results. Other known genetic alterations that might differ between men and women, that deserves to be explored further involve DNA repair capacity, TP53, GRPR, CYP1A1, GSTM1, KRAS, and ALK. [17, 36–38]. Estrogen related receptor beta is present in 45–70% pf NSCLC tumors in both sexes, making hormonal influences on tumor biology an appealing hypothesis. [17] The beneficial effect of female sex on prognosis was more or less constant across age group in our data, opposing a female sex hormone influence on survival. While sex differences in treatment toxicity and tumor response provide alternative explanations, earlier studies have not been able to confirm this [4, 32, 39].
Lung cancer is the most commonly diagnosed malignancy as well as cause of cancer death worldwide [40]. Identification and an improved understanding of potentially modifiable factors behind the sex differences in NSCLC survival could potentially prevent or delay a substantial number of cancer deaths. More advanced stage at diagnosis in men could reflect lower health awareness and higher thresholds for seeking health care. Alternatively, observed differences may reflect more aggressive tumor behavior in men, such as faster growth and higher metastatic potential. Irrespective, sex differences in NSCLC biology warrant additional research. In light of the sizable impact of sex on non-small cell lung cancer outcomes, sex should always be reported and results stratified on sex in clinical research.
Supporting information
(PDF)
(PDF)
*Year of diagnosis 2006–2016. **Year of diagnosis 2003–2016. ***Year of diagnosis 2010–2016.
(PDF)
Numbers (n), percentages (%) of male and female NSCLC patients, and female-to male odds ratios (ORs) with 95% confidence intervals (CI) undergoing diagnostic procedures, by histological type.
1Adjusted for age and calendar year of diagnosis. 2Additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location. *Year 2007–2016. **Defined as treatment within 28 days from referral. ***Stage IIIB-IV, year 2010–2016.
(PDF)
Subgroup analysis of numbers (n), percentages (%) of lung cancer deaths and female-to-male hazard ratios (HRs) with 95% confidence intervals (CI) in men and women diagnosed with pulmonary adenocarcinoma in 2010–2016 and tested for EGFR status, by stage group.
HR1: adjusted for age and calendar year of diagnosis. HR2: additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location. HR3: additionally adjusted for EGFR status.
(PDF)
Adjusted female-to-male hazard ratios (HR*) by histological cell type and stage. Exploring the interaction between (i.e. the effect of) female sex and (i.e. on) selected covariates as well as the model fit (p-value) compared to the original model (Table 3).
*Adjusted for age, calendar year, education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity groups, TNM stage, and primary tumor location.
(PDF)
Lung cancer specific mortality, 5-year female-to-male hazard ratios by histological cell type and stage, comparing Cox regression (cox) and flexible parametric models (flex).
Model 0: Unadjusted. Model 1: Adjusted for age and calendar year of diagnosis. Model 2: Additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location.
(PDF)
Acknowledgments
We acknowledge Dr. Paul Lambert for the invaluable support and input on the statistical analyses in general, and in applying flexible parametric models in particular.
The project was made possible by the continuous reporting by Swedish clinicians to the NLCR and the work by the NLCR steering group: Gunnar Wagenius (chairman), Stefan Bergström, Bengt Bergman, Annelie Behndig, Mikael Johansson, Per Fransson, Kristina Lamberg Lundström, Anna Öjdahl-Bodén, Hanna Carstens, Karl-Gustaf Kölbeck, Andreas Hallqvist, Mona Gilleryd, Anders Vikström, Magnus Kentsson, Maria Planck, Eva Brandén, Simon Ekman, and Johan Botling.
Data Availability
The Lung Cancer DataBase Sweden (LcBaSE) is a research database containing detailed clinical and socioeconomic individual-level data from several nationwide registers. Even though LcBaSE is anonymized, single individuals could potentially be identified and their privacy violated. Furthermore, this type of information is labelled sensitive personal data that is confidential and fall under rigorous, legal secrecy restrictions in Sweden. Data cannot be shared publicly without violating the Swedish law. Anyone wishing to access data is prompted to apply for ethical permission through the Swedish Ethical Review Authority (contact details at https://etikprovningsmyndigheten.se), which includes motivating the use of sensitive personal data, specifying the underlying research objective as well as safety aspects concerning data storage and management. Results can only be presented at an aggregated level. Researchers who meet the criteria to access confidential data can in an initial step contact the primary owner of the Lung Cancer Register, the Chief Legal Officer in Region Uppsala in Central Sweden Johan Ahlgren (e-mail: johan.ahlgren@rccuppsalaorebro.se).
Funding Statement
This work was supported by grants from FORTE - The Swedish Research Council for Health, Working Life and Welfare (2012-03047 to ML); the Swedish research council (2017-01954 to GE); and Stockholm County Council (clinical research appointment to GE). The funding bodies had no role in the data collection and analysis and was not involved in the interpretation of results, writing, revision, or approval of the manuscript.
References
- 1.Werner-Wasik M, Scott C, Cox JD, Sause WT, Byhardt RW, Asbell S, et al. Recursive partitioning analysis of 1999 Radiation Therapy Oncology Group (RTOG) patients with locally-advanced non-small-cell lung cancer (LA-NSCLC): identification of five groups with different survival. International journal of radiation oncology, biology, physics. 2000;48(5):1475–82. Epub 2000/12/21. . [DOI] [PubMed] [Google Scholar]
- 2.Radzikowska E, Glaz P, Roszkowski K. Lung cancer in women: age, smoking, histology, performance status, stage, initial treatment and survival. Population-based study of 20 561 cases. Annals of oncology: official journal of the European Society for Medical Oncology. 2002;13(7):1087–93. Epub 2002/08/15. 10.1093/annonc/mdf187 . [DOI] [PubMed] [Google Scholar]
- 3.Fu JB, Kau TY, Severson RK, Kalemkerian GP. Lung cancer in women: analysis of the national Surveillance, Epidemiology, and End Results database. Chest. 2005;127(3):768–77. Epub 2005/03/15. 10.1378/chest.127.3.768 . [DOI] [PubMed] [Google Scholar]
- 4.Cerfolio RJ, Bryant AS, Scott E, Sharma M, Robert F, Spencer SA, et al. Women with pathologic stage I, II, and III non-small cell lung cancer have better survival than men. Chest. 2006;130(6):1796–802. Epub 2006/12/15. 10.1378/chest.130.6.1796 . [DOI] [PubMed] [Google Scholar]
- 5.Chansky K, Sculier JP, Crowley JJ, Giroux D, Van Meerbeeck J, Goldstraw P. The International Association for the Study of Lung Cancer Staging Project: prognostic factors and pathologic TNM stage in surgically managed non-small cell lung cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2009;4(7):792–801. Epub 2009/05/22. 10.1097/JTO.0b013e3181a7716e . [DOI] [PubMed] [Google Scholar]
- 6.Nakamura H, Ando K, Shinmyo T, Morita K, Mochizuki A, Kurimoto N, et al. Female gender is an independent prognostic factor in non-small-cell lung cancer: a meta-analysis. Annals of thoracic and cardiovascular surgery: official journal of the Association of Thoracic and Cardiovascular Surgeons of Asia. 2011;17(5):469–80. Epub 2011/09/02. 10.5761/atcs.oa.10.01637 . [DOI] [PubMed] [Google Scholar]
- 7.Pitz MW, Musto G, Navaratnam S. Sex as an independent prognostic factor in a population-based non-small cell lung cancer cohort. Canadian respiratory journal. 2013;20(1):30–4. Epub 2013/03/05. 10.1155/2013/618691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rena O, Massera F, Boldorini R, Papalia E, Turello D, Davoli F, et al. Non-small cell lung cancer in surgically treated women. Tumori. 2013;99(6):661–6. Epub 2014/02/08. 10.1700/1390.15453 . [DOI] [PubMed] [Google Scholar]
- 9.Sagerup CM, Smastuen M, Johannesen TB, Helland A, Brustugun OT. Sex-specific trends in lung cancer incidence and survival: a population study of 40,118 cases. Thorax. 2011;66(4):301–7. Epub 2011/01/05. 10.1136/thx.2010.151621 . [DOI] [PubMed] [Google Scholar]
- 10.Wainer Z, Wright GM, Gough K, Daniels MG, Russell PA, Choong P, et al. Sex-Dependent Staging in Non-Small-Cell Lung Cancer; Analysis of the Effect of Sex Differences in the Eighth Edition of the Tumor, Node, Metastases Staging System. Clinical lung cancer. 2018;19(6):e933–e44. Epub 2018/09/13. 10.1016/j.cllc.2018.08.004 . [DOI] [PubMed] [Google Scholar]
- 11.Siddiqui F, Bae K, Langer CJ, Coyne JC, Gamerman V, Komaki R, et al. The influence of gender, race, and marital status on survival in lung cancer patients: analysis of Radiation Therapy Oncology Group trials. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2010;5(5):631–9. Epub 2010/05/01. . [DOI] [PubMed] [Google Scholar]
- 12.Gazdar AF. Should we continue to use the term non-small-cell lung cancer? Annals of oncology: official journal of the European Society for Medical Oncology. 2010;21 Suppl 7:vii225–9. Epub 2010/10/15. 10.1093/annonc/mdq372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ou SH, Zell JA, Ziogas A, Anton-Culver H. Prognostic factors for survival of stage I nonsmall cell lung cancer patients: a population-based analysis of 19,702 stage I patients in the California Cancer Registry from 1989 to 2003. Cancer. 2007;110(7):1532–41. Epub 2007/08/19. 10.1002/cncr.22938 . [DOI] [PubMed] [Google Scholar]
- 14.Paesmans M, Sculier JP, Libert P, Bureau G, Dabouis G, Thiriaux J, et al. Prognostic factors for survival in advanced non-small-cell lung cancer: univariate and multivariate analyses including recursive partitioning and amalgamation algorithms in 1,052 patients. The European Lung Cancer Working Party. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 1995;13(5):1221–30. Epub 1995/05/01. 10.1200/jco.1995.13.5.1221 . [DOI] [PubMed] [Google Scholar]
- 15.Kawaguchi T, Matsumura A, Fukai S, Tamura A, Saito R, Zell JA, et al. Japanese ethnicity compared with Caucasian ethnicity and never-smoking status are independent favorable prognostic factors for overall survival in non-small cell lung cancer: a collaborative epidemiologic study of the National Hospital Organization Study Group for Lung Cancer (NHSGLC) in Japan and a Southern California Regional Cancer Registry databases. 10.1097/JTO.0b013e3181e2f607 2010;5(7):1001–10. Epub 2010/06/08. [DOI] [PubMed] [Google Scholar]
- 16.Kawaguchi T, Takada M, Kubo A, Matsumura A, Fukai S, Tamura A, et al. Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: a comprehensive analysis of 26,957 patients with NSCLC. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2010;5(5):620–30. Epub 2010/04/01. 10.1097/JTO.0b013e3181d2dcd9 . [DOI] [PubMed] [Google Scholar]
- 17.Donington JS, Colson YL. Sex and gender differences in non-small cell lung cancer. Seminars in thoracic and cardiovascular surgery. 2011;23(2):137–45. Epub 2011/11/02. 10.1053/j.semtcvs.2011.07.001 . [DOI] [PubMed] [Google Scholar]
- 18.Harichand-Herdt S, Ramalingam SS. Gender-associated differences in lung cancer: clinical characteristics and treatment outcomes in women. Seminars in oncology. 2009;36(6):572–80. Epub 2009/12/10. 10.1053/j.seminoncol.2009.10.007 . [DOI] [PubMed] [Google Scholar]
- 19.Årsrapport från Nationella Lungcancerregistret 2015. Uppsala, Sweden: Regionalt cancercentrum, Uppsala Örebro, 2016 October 2016. Report No.
- 20.Barlow L, Westergren K, Holmberg L, Talback M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta oncologica. 2009;48(1):27–33. 10.1080/02841860802247664 . [DOI] [PubMed] [Google Scholar]
- 21.Ludvigsson JF, Almqvist C, Bonamy AK, Ljung R, Michaelsson K, Neovius M, et al. Registers of the Swedish total population and their use in medical research. European journal of epidemiology. 2016;31(2):125–36. Epub 2016/01/16. 10.1007/s10654-016-0117-y . [DOI] [PubMed] [Google Scholar]
- 22.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36(1):8–27. Epub 1998/02/07. . [DOI] [PubMed] [Google Scholar]
- 23.Sarfati D. Review of methods used to measure comorbidity in cancer populations: no gold standard exists. Journal of clinical epidemiology. 2012;65(9):924–33. Epub 2012/06/29. 10.1016/j.jclinepi.2012.02.017 . [DOI] [PubMed] [Google Scholar]
- 24.Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2007;2(8):706–14. Epub 2007/09/01. 10.1097/JTO.0b013e31812f3c1a . [DOI] [PubMed] [Google Scholar]
- 25.Postmus PE, Kerr KM, Oudkerk M, Senan S, Waller DA, Vansteenkiste J, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology. 2017;28(suppl_4):iv1–iv21. Epub 2017/09/09. 10.1093/annonc/mdx222 . [DOI] [PubMed] [Google Scholar]
- 26.Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. The Stata Journal. 2009;9(2):265–90. [Google Scholar]
- 27.Sjolander A. Regression standardization with the R package stdReg. European journal of epidemiology. 2016;31(6):563–74. Epub 2016/05/18. 10.1007/s10654-016-0157-3 . [DOI] [PubMed] [Google Scholar]
- 28.Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2015;10(9):1243–60. Epub 2015/08/21. 10.1097/jto.0000000000000630 . [DOI] [PubMed] [Google Scholar]
- 29.Alexiou C, Onyeaka CV, Beggs D, Akar R, Beggs L, Salama FD, et al. Do women live longer following lung resection for carcinoma? European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery. 2002;21(2):319–25. Epub 2002/02/05. 10.1016/s1010-7940(01)01114-9 . [DOI] [PubMed] [Google Scholar]
- 30.Debieuvre D, Oster JP, Riou R, Berruchon J, Levy A, Mathieu JP, et al. The new face of non-small-cell lung cancer in men: Results of two French prospective epidemiological studies conducted 10 years apart. Lung cancer. 2016;91:1–6. Epub 2015/12/30. 10.1016/j.lungcan.2015.11.001 . [DOI] [PubMed] [Google Scholar]
- 31.Sakurai H, Asamura H, Goya T, Eguchi K, Nakanishi Y, Sawabata N, et al. Survival differences by gender for resected non-small cell lung cancer: a retrospective analysis of 12,509 cases in a Japanese Lung Cancer Registry study. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2010;5(10):1594–601. Epub 2010/08/26. 10.1097/JTO.0b013e3181f1923b . [DOI] [PubMed] [Google Scholar]
- 32.Albain KS, Crowley JJ, LeBlanc M, Livingston RB. Survival determinants in extensive-stage non-small-cell lung cancer: the Southwest Oncology Group experience. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 1991;9(9):1618–26. Epub 1991/09/01. 10.1200/jco.1991.9.9.1618 . [DOI] [PubMed] [Google Scholar]
- 33.Batevik R, Grong K, Segadal L, Stangeland L. The female gender has a positive effect on survival independent of background life expectancy following surgical resection of primary non-small cell lung cancer: a study of absolute and relative survival over 15 years. Lung cancer. 2005;47(2):173–81. Epub 2005/01/11. 10.1016/j.lungcan.2004.08.014 . [DOI] [PubMed] [Google Scholar]
- 34.Caldarella A, Crocetti E, Comin CE, Janni A, Pegna AL, Paci E. Gender differences in non-small cell lung cancer: a population-based study. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2007;33(6):763–8. Epub 2007/02/20. 10.1016/j.ejso.2007.01.001 . [DOI] [PubMed] [Google Scholar]
- 35.Foegle J, Hedelin G, Lebitasy MP, Purohit A, Velten M, Quoix E. Specific features of non-small cell lung cancer in women: a retrospective study of 1738 cases diagnosed in Bas-Rhin between 1982 and 1997. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2007;2(6):466–74. Epub 2007/06/05. 10.1097/01.jto.0000275340.39960.25 . [DOI] [PubMed] [Google Scholar]
- 36.Planchard D, Loriot Y, Goubar A, Commo F, Soria JC. Differential expression of biomarkers in men and women. Seminars in oncology. 2009;36(6):553–65. 10.1053/j.seminoncol.2009.09.004 . [DOI] [PubMed] [Google Scholar]
- 37.Schwartz AG, Prysak GM, Murphy V, Lonardo F, Pass H, Schwartz J, et al. Nuclear estrogen receptor beta in lung cancer: expression and survival differences by sex. Clinical cancer research: an official journal of the American Association for Cancer Research. 2005;11(20):7280–7. Epub 2005/10/26. 10.1158/1078-0432.ccr-05-0498 . [DOI] [PubMed] [Google Scholar]
- 38.Xiao D, Pan H, Li F, Wu K, Zhang X, He J. Analysis of ultra-deep targeted sequencing reveals mutation burden is associated with gender and clinical outcome in lung adenocarcinoma. Oncotarget. 2016;7(16):22857–64. Epub 2016/03/25. 10.18632/oncotarget.8213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wheatley-Price P, Le Maitre A, Ding K, Leighl N, Hirsh V, Seymour L, et al. The influence of sex on efficacy, adverse events, quality of life, and delivery of treatment in National Cancer Institute of Canada Clinical Trials Group non-small cell lung cancer chemotherapy trials. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer. 2010;5(5):640–8. Epub 2010/04/01. 10.1097/JTO.0b013e3181d40a1b . [DOI] [PubMed] [Google Scholar]
- 40.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International journal of cancer Journal international du cancer. 2015;136(5):E359–86. Epub 2014/09/16. 10.1002/ijc.29210 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
*Year of diagnosis 2006–2016. **Year of diagnosis 2003–2016. ***Year of diagnosis 2010–2016.
(PDF)
Numbers (n), percentages (%) of male and female NSCLC patients, and female-to male odds ratios (ORs) with 95% confidence intervals (CI) undergoing diagnostic procedures, by histological type.
1Adjusted for age and calendar year of diagnosis. 2Additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location. *Year 2007–2016. **Defined as treatment within 28 days from referral. ***Stage IIIB-IV, year 2010–2016.
(PDF)
Subgroup analysis of numbers (n), percentages (%) of lung cancer deaths and female-to-male hazard ratios (HRs) with 95% confidence intervals (CI) in men and women diagnosed with pulmonary adenocarcinoma in 2010–2016 and tested for EGFR status, by stage group.
HR1: adjusted for age and calendar year of diagnosis. HR2: additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location. HR3: additionally adjusted for EGFR status.
(PDF)
Adjusted female-to-male hazard ratios (HR*) by histological cell type and stage. Exploring the interaction between (i.e. the effect of) female sex and (i.e. on) selected covariates as well as the model fit (p-value) compared to the original model (Table 3).
*Adjusted for age, calendar year, education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity groups, TNM stage, and primary tumor location.
(PDF)
Lung cancer specific mortality, 5-year female-to-male hazard ratios by histological cell type and stage, comparing Cox regression (cox) and flexible parametric models (flex).
Model 0: Unadjusted. Model 1: Adjusted for age and calendar year of diagnosis. Model 2: Additionally adjusted for level of education, marital status, birth country, health care region, ECOG performance status, smoking history, Elixhauser comorbidity categories, TNM stage, and primary tumor location.
(PDF)
Data Availability Statement
The Lung Cancer DataBase Sweden (LcBaSE) is a research database containing detailed clinical and socioeconomic individual-level data from several nationwide registers. Even though LcBaSE is anonymized, single individuals could potentially be identified and their privacy violated. Furthermore, this type of information is labelled sensitive personal data that is confidential and fall under rigorous, legal secrecy restrictions in Sweden. Data cannot be shared publicly without violating the Swedish law. Anyone wishing to access data is prompted to apply for ethical permission through the Swedish Ethical Review Authority (contact details at https://etikprovningsmyndigheten.se), which includes motivating the use of sensitive personal data, specifying the underlying research objective as well as safety aspects concerning data storage and management. Results can only be presented at an aggregated level. Researchers who meet the criteria to access confidential data can in an initial step contact the primary owner of the Lung Cancer Register, the Chief Legal Officer in Region Uppsala in Central Sweden Johan Ahlgren (e-mail: johan.ahlgren@rccuppsalaorebro.se).