Abstract
Background
Alcohol use disorders affect 10% of the European population. Alcohol-related liver disease (ALD) is the most common indication for liver transplantation in Slovakia. The aim of this study was to determine the proportion of patients with ALD who received a liver transplant who had alcohol relapsed, and the risk factors for alcohol relapse, as well as to compare clinical outcomes according to relapse.
Material/Methods
A retrospective study of consecutive patients with ALD, who underwent liver transplantation in a single transplant center between May 2008 and December 2017. We included adult patients who received a liver transplant due to ALD and excluded those who died <1 month after liver transplantation. We recorded demographic and clinical characteristics, graft injury, and overall mortality and compared them between relapsers and abstainers.
Results
During the study period, we reviewed 196 cases of liver transplantation in 191 patients. We excluded 87 patients for non-ALD etiology and 15 patients by predefined criteria. The final analysis was carried out in 89 patients, mean aged 55 years; 24.7% were female. We diagnosed relapse in 23 patients (26%) with harmful drinking in 52% and occasional drinking in 48% of relapsers. The independent risk factors associated with relapse were: smoking (OR=5.92, P=0.006), loss of social status (OR=7.61, P=0.002), and time after liver transplantation (OR=1.0008, P=0.015). Graft injury was more frequent in relapsers with 2 independent risk factors: occasional drinking (OR=12.7, P=0.0005), and harmful drinking (OR=36.6, P<0.0001); overall survival was unaffected.
Conclusions
We found relapse to alcohol drinking in 26% of patients who received a liver transplant for ALD. Risk factors associated with alcohol drinking relapse were time, cigarette smoking, and loss of social status. Graft injury was more frequent in relapsers, but mortality was similar between relapsers and non-relapsers.
MeSH Keywords: Liver Cirrhosis, Alcoholic; Liver Diseases, Alcoholic; Liver Transplantation; Alcohol-Induced Disorders
Background
Behavioral and mental disorders related to alcohol addiction, called alcohol use disorders, affect 10% of European population; one of the consequences of alcohol use disorders is alcoholic liver disease (ALD) that may lead to cirrhosis and is the most common indication for liver transplantation (LTx) in Slovakia [1–3]. Slovakia ranks fourth in Europe for mortality rate from liver cirrhosis, with ALD being the most prevalent cause [4]. According to the 2018 Global Report on Alcohol and Health, consumption of pure alcohol per capita per year in Slovakia exceeds 11 L (almost double the average of 6.4 L). There are no officially accepted governmental policies to combat alcohol use disorders. Despite conflicting evidence behind the “6-months rule”, Slovak patients with a chronic form of ALD would only be eligible for LTx after at least 6 months of abstinence from alcohol consumption documented by the addictologist [5–7].
The management of patients referred with decompensated chronic liver disease for consideration of LTx to our center followed standard protocol. We attempt to confirm the etiology and stability of the decompensated state of the liver by the usual spectrum of evaluations: from history taking to hepatic venous pressure gradient and (transjugular) liver biopsy. We attempt to determine if the patient is critical with the diagnosis of ALD. Then we review the data related to the patient’s existing abstinence interval and refer the patient to a dedicated addictologist. This expert directly cooperates with our transplant center, and his or her task is to confirm etiology, sobriety, duration of abstinence interval of at least 6 months, and outlook concerning the long-term adherence to abstinence. The only exception is severe acute alcoholic hepatitis not responding to standard treatment in patients fulfilling the criteria of the Lille protocol.
The precise proportion of patients with alcohol use relapse after LTx (a form of alcohol use disorders) is not known; however, according to the literature, the prevalence ranges from 7% to 95% [5,8–10]. One of the reasons for this wide variation lies in differing definitions of the term “recurrence” and “relapse.” Post-LTx alcohol use relapse may lead to numerous consequences, such as liver graft injury (prevalence up to 17%) [11], liver graft loss (up to 32%) [12], and reduced 10-year survival (45% versus 85% in non-relapsers) [11]. The most common alcohol consumption patterns following LTx are occasional drinking (alcohol slip-ups), i.e., consumption of a limited amount of alcohol, followed by re-established abstinence, and harmful drinking, i.e., consumption of 4 or more drinks per day, or drinking for 4 or more successive days (Table 1) [13].
Table 1.
Patterns of relapse to alcohol drinking after liver transplantation [13].
| Definition | |
|---|---|
| Harmful (addictive) drinking | Consumption of four or more drinks in a day or for 4 or more days in succession |
| Occasional drinking (slip-up) | Consumption of a limited amount of alcohol, followed by re-established abstinence |
Risk factors for alcohol use relapse are not well established. The most commonly cited risk factors in the literature are (younger) age, cigarette smoking, mental disorders, non-compliance with regular follow-up, loss of social status (e.g., divorce, bereavement), and unemployment [14]. Our patients are routinely followed according to their clinical status and usually, if stable, on a 3-month follow-up schedule.
In this study, we aimed to determine the proportion of ALD patients who received a transplant who relapsed to alcohol drinking after LTx, and the risk factors for alcohol use relapse. We also compared clinical outcomes according to the presence or absence of alcohol use relapse.
Material and Methods
In this retrospective, single-center study we analyzed the data in consecutive patients who received a liver transplant for the chronic form of ALD during the interval from May 2008 to December 2017. We excluded patients who died during the first month after LTx and patients younger than 18 years of age.
We analyzed the following demographic and clinical variables: age, sex, model for end-stage liver disease (MELD), Child-Pugh score, ascites (grade 1, mild: detected by imaging; grade 2, moderate: physician’s objective assessment, 3, large or gross: marked by abdominal distention), hepatic encephalopathy, and survival/mortality. We diagnosed alcohol use relapse based on the clinical suspicion accompanied by the presence of at least 2 of the following criteria. 1) The patient admitted that he or she drinks alcohol on history taking by the physician. 2) The source of this information was the patient’s family member or other surrogate living with the patient in the household. 3) Laboratory abnormalities raised the suspicion of alcohol use relapse. We considered suspicious the presence of at least 2 of the following: if the ratio of aspartate aminotransferase (AST) to alanine aminotransferase (ALT) levels was higher than 1; the gamma-glutamyltransferase (GMT) level was above the upper limit of normal (ULN); mean corpuscular volume of erythrocytes (MCV) was above the ULN. A positive blood alcohol test alone sufficed for diagnosing alcohol relapse [15]. We divided the pattern of alcohol use relapse to occasional and harmful drinking according to the literature [13] (Table 1). We chose from the literature risk factors of alcohol use relapse which we would also be able to extract from the files of our patients: age, cigarette smoking, mental disorders, non-compliance with regular follow-up, loss of social status (e.g., divorce, bereavement), and unemployment.
We defined liver graft injury as a new onset of elevations above ULN of AST, ALT, GMT, or bilirubin which was then found on at least 1 more measurement 3 months apart. We also recorded liver graft failure and overall mortality.
For statistical analysis, we used legally obtained software MedCalc v.17 (Ostende, Belgium). We present the results of continuous variables as medians and the interquartile ranges results for proportions as numbers of cases and percentages. Comparison of continuous variables was carried out using the Mann-Whitney test, and the chi-square test was used to compare proportions. To identify factors independently associated with graft injury, all parameters statistically appearing to be associated (i.e., P<0.12) were entered into a backward multivariate logistic regression. We compared overall survival between the patients with and without alcohol use relapse with Kaplan-Meier survival curves. We defined statistical significance by the probability of null-hypothesis inferior to 0.05.
All participants signed the informed consent before liver LTx and agreed with a data publication.
Ethical approval
All procedures involving human participants were approved according to the ethical standards of the institutional research committee, including the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The reported clinical and research activities were consistent with the Principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.
Results
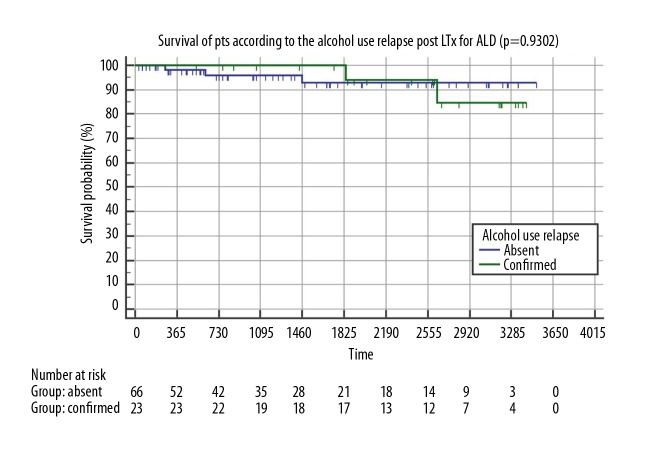
From the 196 LTx in 191 patients performed during the observation period of 115 months, 87 patients (45.5%) underwent LTx due to non-alcohol use disorders etiology and we excluded 15 patients by the predefined criteria of death during the first month post LTx. Our final cohort included 89 out of 191 patients (46.6%) for the final analysis (Figure 1). Patients transplanted due to ALD had a mean age of 55.35 years (IQR 48.79 to 59.87), and 24.7% were female. The mean MELD score was 16.0 points (IQR 13.79 to 19.00 points), and the mean Child-Pugh score was 10.0 points (IQR 9 to 11 points). Summary statistics and study group characteristics are displayed in Table 2.
Figure 1.
Flowchart: Alcohol use relapse rates after LTx.
Table 2.
Summary statistics and characteristics of 89 patients who underwent liver transplantation for ALD.
| n=89 Median/% |
25–75 percentile | |
|---|---|---|
| Age at liver transplantation | 55.35 | 48.79 to 59.87 |
| Sex (% females) | 24.70 | |
| Blood group A (%) | 51.70 | |
| Blood group B (%) | 18.00 | |
| Blood group AB (%) | 13.50 | |
| Blood group 0 (%) | 16.90 | |
| Child_Pugh_score | 10.00 | 9.00 to 11.00 |
| MELD_score | 16.00 | 13.79 to 19.00 |
| INR | 1.55 | 1.37 to 1.66 |
| Serum creatinine | 77.00 | 62.50 to 95.50 |
| Serum albumin | 30.00 | 26.25 to 34.75 |
| Serum bilirubin | 53.50 | 38.50 to 86.50 |
| Ascites_stage (Gr. 1–3) | 2.00 | 2.00 to 3.00 |
| Hepatic encephalopathy stage (Gr. 1–3) | 1.00 | 1.00 to 2.00 |
| BMI before liver transplantation | 27.00 | 24.00 to 30.00 |
| Duration_hospital_stay | 26.00 | 20.00 to 37.00 |
| Days_survived (from LTx to end of study period) | 1586.00 | 591.25 to 2621.25 |
| Alcohol relapse (%) | 25.80 | |
| Relapse_harmul drinking (%) | 13.50 | |
| Relapse_occasional_drinking (%) | 12.40 | |
| Relapse_admitted_by_patient (%) | 60.90 | |
| Relapse_reported_by relative (%) | 17.40 | |
| Relapse_dg_by_labs (%) | 17.40 | |
| Relapse_dg._blood_alcohol (%) | 4.35 | |
| Mental disorders (%) | 1.12 | |
| 6_months_rule followed (%) | 100.00 | |
| Cigarette smoking (%) | 24.70 | |
| Graft_injury (%) | 28.10 | |
| Loss of social status (divorce. loss_of_partner. single) (%) | 22.50 | |
| Compliance_with_controls (%) | 87.60 | |
| Employed_post_Tx (%) | 22.50 | |
| Unemployed_post_Tx (%) | 2.25 | |
| Invalidity_post_Tx (%) | 48.30 | |
| Retirement_post_Tx (%) | 27.00 |
We observed alcohol use relapse in 23 out of 89 patients (26%) transplanted for ALD. We did not find any post-transplantation alcohol use in the 153 patients transplanted for non-ALD liver disease (P=0.0001). In 12 patients (52%) the pattern of alcohol use relapse was harmful drinking, and in 11 patients (48%) it was occasional drinking (P=non significance), (Figure 1).
In order to determine possible risk factors in our cohort, we compared the risk factor prevalence between relapsers and non-relapsers (Table 3). Patients who relapsed to alcohol use were non-significantly younger (52.57 [AR 37.6] versus 56.15 [AR 47.57], P=0.11), more often smoked cigarettes (13 [56.52%] versus 9 [13.64%], P=0.0001), have lost their social status by divorce or bereavement (13 [56.5%] versus 7 [10.6%], P<0.0001), and were non-compliant with regular appointments (9 [39.1%] versus 2 [3%], P<0.0001). In contrast, we did not observe differences between relapsers and non-relapsers concerning sex, unemployment, premature retirement due to invalidity (IP), or the age-related retirement (OAP). Included study patients had no documented mental disorders.
Table 3.
Characteristics and risk factors for alcohol use relapse among 89 patients who underwent liver transplantation for ALD.
| Variable | No alcohol use relapse n=66 Median/% AR |
Alcohol use relapse n=23 Median/% AR |
P* |
|---|---|---|---|
| Age at liver transplantation | 56.15/47.57 | 52.57/37.60 | 0.1111 |
| Sex (% Females) | 25.76 | 21.74 | 0.7072 |
| Hospital stay (days) | 25.00/44.77 | 26.00/45.65 | 0.8882 |
| Days survived (from LTx to end of study period) | 1228.0/39.46 | 2595.0/60.86 | 0.0006 |
| Death post-Ltx (%) | 4.55 | 8.70 | 0.4969 |
| Mental disorders (%) | 0.00 | 4.35 | 0.2284 |
| 6 months rule before LTx (%) | 100.00 | 100.00 | 1.0000 |
| Smoking (%) | 13.64 | 56.52 | 0.0001 |
| Graft injury (%) | 12.12 | 73.91 | <0.0001 |
| Loss of social status (divorce loss of part single) (%) | 10.61 | 56.52 | <0.0001 |
| Compliance with controls (%) | 96.97 | 60.87 | <0.0001 |
| Employed post Tx (%) | 22.73 | 21.74 | 0.9241 |
| Unemployed post Tx%) | 1.52 | 4.35 | 0.5193 |
| Invalidity post Tx(%) | 45.45 | 56.52 | 0.3683 |
Mann-Whitney test, AR – average rank.
We observed graft injury in 17 patients (73.9%) with alcohol use relapse as compared to 8 patients (12.1%) without relapse (P<0.0001).
In the search for possible risk factors associated with liver graft injury in patients with alcohol use relapse we used univariate analysis and identified the following risk factors: younger age, harmful pattern of drinking, cigarette smoking, loss of social status, and non-compliance with regular appointments (Table 4).
Table 4.
Characteristics and risk factors for liver graft injury among 89 patients who underwent liver transplantation for ALD.
| Variable | No graft_injury n=64 Median/% AR |
Graft_injury n=25 Median/% AR |
P* |
|---|---|---|---|
| Age at liver transplantation | 56.15/48.42 | 51.95/36.24 | 0.0456 |
| Sex (% Females) | 26.56 | 20.00 | 0.5288 |
| Hospital stay (days) | 25.00/43.53 | 27.00/48.76 | 0.3906 |
| Days survived (from LTx to end of study period) | 1270.0/41.34 | 1910.0/54.36 | 0.0327 |
| Death post Ltx (%) | 3.13 | 12.00 | 0.1358 |
| Alcohol use relapse (%) | 9.38 | 68.00 | <0.0001 |
| Harmful drinking (%) | 3.13 | 40.00 | <0.0001 |
| Occasional drinking(%) | 6.25 | 28.00 | 0.0073 |
| Mental disorders (%) | 0.00 | 4.00 | 0.2552 |
| 6 months rule prior to LTx (%) | 100.00 | 100.00 | 1.0000 |
| Cigarette smoking (%) | 15.63 | 48.00 | 0.0019 |
| Loss of socialstatus (divorce loss of part single) (%) | 14.06 | 44.00 | 0.003 |
| Compliance with controls (%) | 95.31 | 68.00 | 0.0008 |
| Employed post Tx (%) | 21.88 | 24.00 | 0.8334 |
| Unemployed post Tx (%) | 1.56 | 4.00 | 0.5691 |
| Invalidity post Tx (%) | 45.31 | 56.00 | 0.3724 |
Mann-Whitney test, AR – average rank.
In the multivariate logistic model displayed in Table 5A, we revealed 3 independent risk factors for alcohol relapse: days post liver transplantation (OR=1.0008; 95%CI 1.0001–1.0014, P=0.015), cigarette smoking (OR=5.92, 95%CI 1.6665–21.0308; P=0.006) and loss of social status (OR=7.61; 95%CI 2.0859–27.7745, P=0.0021).
Table 5.
Multivariate logistic regression model for independent predictors of alcohol relapse (A) and liver graft injury (B) among 89 patients after liver transplantation for ALD.
| A. Alcohol use relapse | Odds ratio | 95% CI | P |
|---|---|---|---|
| Days post liver transplantation | 1.0008 | 1.0001–1.0014 | 0.015 |
| Cigarette smoking | 5.9201 | 1.6665–21.0308 | 0.006 |
| Loss of social status (divorce, loss of partner, single) | 7.6115 | 2.0859–27.7745 | 0.0021 |
Cox & Snell R2=0.3195, significance liver: P<0.0001, AUROC=0.857 (0.767–0.922), 82.02% correctly classfied. Variables entered: days survived, cigarette smoking, loss of social status, compliance with controls and age. Variables excluded: compliance with controls, age.
| B. Liver graft injury | Odds ratio | 95% CI | P |
|---|---|---|---|
| Relapse of occasional drinking | 12.69 | 3.025–53.22 | 0.0005 |
| Relapse of harmful drinking | 36.25 | 6.69–196.18 | <0.0001 |
Cox & Snell R2=0.299, significance liver: P<0.0001, AUROC=0.801 (0.703–0.878), 84.27% correctly classfied. Variables entered: days survived, cigarette smoking, loss of social status, compliance with controls, relapse of occasional drinking, relapse of harmful drinking. Variables excluded: days survived, smoking, loss of social status, compliance with controls.
In the multivariate logistic model displayed in Table 5B, we revealed 2 independent risk factors of liver graft injury: occasional drinking (OR=12.69, 95%CI 3.025–53.22, P=0.0005), and harmful drinking (OR=36.25, 95%CI 6.69–196.18, P<0.0001).
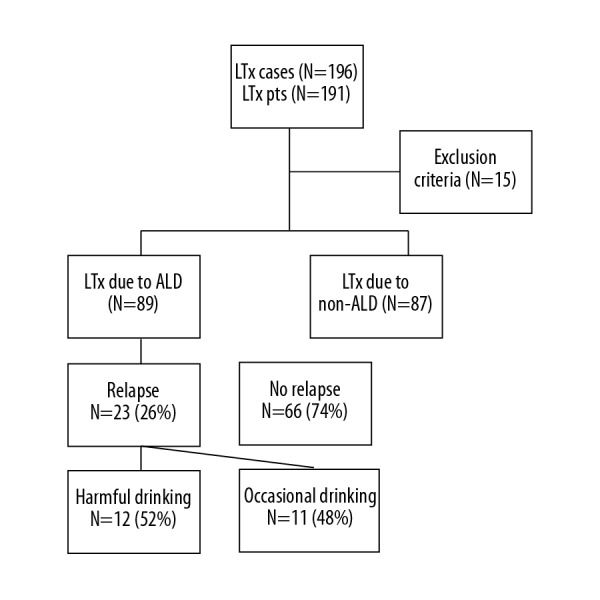
We did not find a significant difference in mortality during follow-up between patients with or without alcohol use relapse: 2 patients (9%) versus 3 patients (5%), P=0.83.
Comparison of overall survival between patients with and without alcohol use relapse is displayed in Figure 2. Kaplan-Meier survival curves revealed no difference in overall survival according to alcohol use relapse after LTx for ALD patients (P=0.93), (Figure 2).
Figure 2.
Overall survival of patients according to the alcohol use relapse following the liver transplantation for ALD.
Discussion
The most important finding of this single-center retrospective study covering 10 years of our LTx program was the alcohol use relapse rate of 26% seen in patients transplanted for ALD. This rate compares well with other studies [5,8–10,16]. However, some studies found alcohol use also in patients transplanted for other indications than ALD. This finding might be explained by the different inclinations of the ALD and non-ALD cohorts to drink, as was shown in the study by Abosh et al. that only 2% of patients who received a liver transplant for non-ALD drank alcohol after LTx [17]. However, we cannot exclude the possibility that our methodology caused the differences found, as we focused primarily on patients transplanted for ALD. The relatively high prevalence of alcohol use relapse in our cohort among other things adds to the arguments against the clinical usefulness of the 6-month rule [5,6,18,19]. We have adopted this rule for 2 historical reasons: as a part of the protocol from our mentoring institution and because it harmonized with the atmosphere in the professional and lay community at that time. In light of our results, however, we will have to reconsider. The most probable next step will be to scrutinize the feasibility in this context of the Lille model approach which we already adopted for the patients with acute alcoholic hepatitis [20].
The impact of alcohol use relapse on liver graft injury over time (73.9% versus 12.1%, P<0.0001) concurs with the available data [21], but the non-significant impact on mortality does not. According to available literature, the 1-year survival rate in patients after LTx due to ALD is at least as good as in other etiologies and reaches 93% [1,22–24]. However, with the alcohol use relapse, especially to harmful drinking, the mortality rate increases [25,26]. This discrepancy might be explained by a rather small number of patients and relatively short median follow-up time [11,12] as was the case in our study The median time (in days from LTx) at which we determined the alcohol use relapse was longer in patients with relapse as compared to patients without relapse (1228.0 days versus 2595.0 days, P=0,0006); in fact, the time from LTx was an independent predictor of alcohol relapse. The design of our study allowed us to evaluate only the cumulative rate of alcohol relapse, but not the temporal trends in more detail. However, patients that relapsed had a median time post LTx of over 7 years, which might suggest that the follow-up program of psychological and social support should be long-term, possibly indefinite. The evolution of liver graft injury over time has been addressed in several studies [15,27,28].
Of potential risk factors for alcohol relapse listed in the literature [5,23,25], several associations also appeared in our study: cigarette smoking, loss of social status, and non-adherence with regular follow-up All of these risk factors will be used at our center immediately as warning signals and we will implement them into the daily clinical practice. Also, we will address them in a prospective study. These risk factors could serve as a risk-stratification measure helping us to provide patients at risk with more intensive management by the addictology experts and social support team [18,25,29–34]. Several studies have suggested that younger age and female sex is related to increased alcohol relapse rates [18,21,32,35]. Our patients with alcohol use relapse were almost 3.5 years younger, but the difference was not statistically significant. Although other studies have found the opposite results [5,6,25], we consider younger age, especially in connection with other risk factors, as a reason for increased attention and focused care. Although unemployment could be a significant risk factor for alcohol use relapse [6,7,10,18], we were not able to analyze it as such.
Limitations of our study were the retrospective design, the single-center setting, and the relatively low number of patients. However, a single-center report provides results with unified selection criteria for LTx and unified diagnostic and management protocols. The obvious limitations of our study were the lack of liver biopsies in all patients with alcohol use relapse and the inability to determine the exact time of first relapse.
To the best of our knowledge, this is the first study of its kind in Slovakia, and the second in the published literature from the Central European region [35].
Conclusions
We documented alcohol use relapse in 26% of patients transplanted for ALD; this relatively high rate was comparable with data from the literature. We identified several risk factors associated with alcohol use relapse: cigarette smoking, loss of social status, and non-compliance with regular follow-ups. We will use these risk factors as a trigger for intervention in our center. In our study, alcohol use relapse was associated with liver graft injury but not with mortality, probably due to the limited follow-up time and sample size of our study. These study findings allow us to move forward in methods for data collection, risk stratification of waitlisted patients with ALD, as well as with a more intensive and directed post-transplantation psychological and social support.
Footnotes
Source of support: Departmental sources
The authors declare no conflicts of interest
References
- 1.Burra P, Senzolo M, Adam R, et al. Liver transplantation for alcoholic liver disease in Europe: A study from the ELTR (European Liver Transplant Registry) Am J Transplant. 2010;10:138–48. doi: 10.1111/j.1600-6143.2009.02869.x. [DOI] [PubMed] [Google Scholar]
- 2.Skladaný Ľ, Adamcová Selčanová S, Dropčová A, et al. Transplantácia pečene. Interná Med. 2015;15(3):93–101. [in Slovakian] [Google Scholar]
- 3.Trunecka P, Gerlei Z, Lisik W, et al. Liver transplantation in Central Europe. Clin Exp Hepatol. 2016;2:21–26. doi: 10.5114/ceh.2016.58853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. World Health Statistics 2016 data visualizations dashboard: harmful use of alcohol. Last updated 18-04-12. [Google Scholar]
- 5.De Gottardi A, Spahr L, Gelez P, et al. A simple score for predicting alcohol relapse after liver transplantation: Results from 387 patients over 15 years. Arch Intern Med. 2007;167:1183–88. doi: 10.1001/archinte.167.11.1183. [DOI] [PubMed] [Google Scholar]
- 6.Jauhar S, Talwalkar JA, Schneekloth T, et al. Analysis of factors that predict alcohol relapse following liver transplantation. Liver Transpl. 2004;10:408–11. doi: 10.1002/lt.20086. [DOI] [PubMed] [Google Scholar]
- 7.Kelly M, Chick J, Gribble R, et al. Predictors of relapse to harmful alcohol after orthotopic liver transplantation. Alcohol Alcohol. 2006;41:278–83. doi: 10.1093/alcalc/agh257. [DOI] [PubMed] [Google Scholar]
- 8.Lim JK, Keeffe EB. Liver transplantation for alcoholic liver disease: Current concepts and length of sobriety. Liver Transpl. 2004;10:31–38. doi: 10.1002/lt.20267. [DOI] [PubMed] [Google Scholar]
- 9.Pageaux GP, Michel J, Coste V, et al. Alcoholic cirrhosis is a good indication for liver transplantation, even for cases of recidivism. Gut. 1999;45:421–26. doi: 10.1136/gut.45.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Björnsson E, Olsson J, Rydell A, et al. Long-term follow-up of patients with alcoholic liver disease after liver transplantation in Sweden: Impact of structured management on recidivism. Scand J Gastroenterol. 2005;40:206–16. doi: 10.1080/00365520410009591. [DOI] [PubMed] [Google Scholar]
- 11.Cuadrado A, Fábrega E, Casafont F, Pons-Romero F. Alcohol recidivism impairs long-term patient survival after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl. 2005;11:420–26. doi: 10.1002/lt.20386. [DOI] [PubMed] [Google Scholar]
- 12.Erard-Poinsot D, Guillaud O, Hervieu V, et al. Severe alcoholic relapse after liver transplantation: What consequences on the graft? A study based on liver biopsies analysis. Liver Transpl. 2016;22:773–84. doi: 10.1002/lt.24425. [DOI] [PubMed] [Google Scholar]
- 13.Lucey MR. Liver transplantation for alcoholic liver disease. Clin Liver Dis. 2007;11:283–89. doi: 10.1016/j.cld.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Lim J, Curry MP, Sundaram V. Risk factors and outcomes associated with alcohol relapse after liver transplantation. World J Hepatol. 2017;9(17):771–80. doi: 10.4254/wjh.v9.i17.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pageaux GP, Bismuth M, Perney P, et al. Alcohol relapse after liver transplantation for alcoholic liver disease: Does it matter? J Hepatol. 2003;38:629–34. doi: 10.1016/s0168-8278(03)00088-6. [DOI] [PubMed] [Google Scholar]
- 16.Tawa EA, Hall SD, Lohoff FW. Overview of the genetics of alcohol use disorder. Alcohol Alcohol. 2016;51(5):507–14. doi: 10.1093/alcalc/agw046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abosh D, Rosser B, Kaita K, et al. Outcomes following liver transplantation for patients with alcohol-versus nonalcohol-induced liver disease. Can J Gastroenterol. 2000;14:851–55. doi: 10.1155/2000/867514. [DOI] [PubMed] [Google Scholar]
- 18.Perney P, Bismuth M, Sigaud H, et al. Are preoperative patterns of alcohol consumption predictive of relapse after liver transplantation for alcoholic liver disease? Transpl Int. 2005;18:1292–97. doi: 10.1111/j.1432-2277.2005.00208.x. [DOI] [PubMed] [Google Scholar]
- 19.Tandon P, Goodman KJ, Ma MM, et al. A shorter duration of pre-transplant abstinence predicts problem drinking after liver transplantation. Am J Gastroenterol. 2009;104:1700–6. doi: 10.1038/ajg.2009.226. [DOI] [PubMed] [Google Scholar]
- 20.Mathurin P, Moreno C, Samuel D, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365:1790–800. doi: 10.1056/NEJMoa1105703. [DOI] [PubMed] [Google Scholar]
- 21.Rice JP, Eickhoff J, Agni R, et al. Abusive drinking after liver transplantation is associated with allograft loss and advanced allograft fibrosis. Liver Transpl. 2013;19:1377–86. doi: 10.1002/lt.23762. [DOI] [PubMed] [Google Scholar]
- 22.Dumortier J, Guillaud O, Adham M, et al. Negative impact of de novo malignancies rather than alcohol relapse on survival after liver transplantation for alcoholic cirrhosis: A retrospective analysis of 305 patients in a single center. Am J Gastroenterol. 2007;102:1032–41. doi: 10.1111/j.1572-0241.2007.01079.x. [DOI] [PubMed] [Google Scholar]
- 23.Faure S, Herrero A, Jung B, et al. Excessive alcohol consumption after liver transplantation impacts on long-term survival, whatever the primary indication. J Hepatol. 2012;57:306–12. doi: 10.1016/j.jhep.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 24.Lucey MR, Schaubel DE, Guidinger MK, et al. Effect of alcoholic liver disease and hepatitis C infection on waiting list and posttransplant mortality and transplant survival benefit. Hepatology. 2009;50:400–6. doi: 10.1002/hep.23007. [DOI] [PubMed] [Google Scholar]
- 25.Pfitzmann R, Schwenzer J, Rayes N, et al. Long-term survival and predictors of relapse after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl. 2007;13:197–205. doi: 10.1002/lt.20934. [DOI] [PubMed] [Google Scholar]
- 26.Dumortier J, Dharancy S, Cannesson A, et al. Recurrent alcoholic cirrhosis in severe alcoholic relapse after liver transplantation: A frequent and serious complication. Am J Gastroenterol. 2015;110:1160–66. doi: 10.1038/ajg.2015.204. [DOI] [PubMed] [Google Scholar]
- 27.Burra P, Mioni D, Cecchetto A, et al. Histological features after liver transplantation in alcoholic cirrhotics. J Hepatol. 2001;34:716–22. doi: 10.1016/s0168-8278(01)00002-2. [DOI] [PubMed] [Google Scholar]
- 28.Tang H, Boulton R, Gunson B, et al. Patterns of alcohol consumption after liver transplantation. Gut. 1998;43:140–45. doi: 10.1136/gut.43.1.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelly M, Chick J, Gribble R, et al. Predictors of relapse to harmful alcohol after orthotopic liver transplantation. Alcohol Alcohol. 2006;41:278–83. doi: 10.1093/alcalc/agh257. [DOI] [PubMed] [Google Scholar]
- 30.Egawa H, Nishimura K, Teramukai S, et al. Risk factors for alcohol relapse after liver transplantation for alcoholic cirrhosis in Japan. Liver Transpl. 2014;20:298–310. doi: 10.1002/lt.23797. [DOI] [PubMed] [Google Scholar]
- 31.Satapathy SK, Eason JD, Nair S, et al. Recidivism in liver transplant recipients with alcoholic liver disease: Analysis of demographic, psychosocial, and histology features. Exp Clin Transplant. 2015;13:430–40. [PubMed] [Google Scholar]
- 32.Grąt M, Lewandowski Z, Grąt K, et al. Negative outcomes after liver transplantation in patients with alcoholic liver disease beyond the fifth post-transplant year. Clin Transplant. 2014;28:1112–20. doi: 10.1111/ctr.12427. [DOI] [PubMed] [Google Scholar]
- 33.DiMartini A, Day N, Dew MA, et al. Alcohol consumption patterns and predictors of use following liver transplantation for alcoholic liver disease. Liver Transpl. 2006;12:813–20. doi: 10.1002/lt.20688. [DOI] [PubMed] [Google Scholar]
- 34.Rodrigue JR, Hanto DW, Curry MP. The alcohol relapse risk assessment: A scoring system to predict the risk of relapse to any alcohol use after liver transplant. Prog Transplant. 2013;23:310–18. doi: 10.7182/pit2013604. [DOI] [PubMed] [Google Scholar]
- 35.Zeair S, Cyprys S, Wiśniewska H, et al. Alcohol relapse after liver transplantation: Younger women are at greatest risk. Ann Transplant. 2017;22:725–29. doi: 10.12659/AOT.905335. [DOI] [PMC free article] [PubMed] [Google Scholar]