Abstract
Mindfulness meditation is increasingly incorporated into mental health interventions, and theoretical concepts associated with it have influenced basic research on psychopathology. Here, we review the current understanding of mindfulness meditation through the lens of clinical neuroscience, outlining the core capacities targeted by mindfulness meditation and mapping them onto cognitive and affective constructs of the Research Domain Criteria matrix proposed by the National Institute of Mental Health. We review efficacious applications of mindfulness meditation to specific domains of psychopathology including depression, anxiety, chronic pain, and substance abuse, as well as emerging efforts related to attention disorders, traumatic stress, dysregulated eating, and serious mental illness. Priorities for future research include pinpointing mechanisms, refining methodology, and improving implementation. Mindfulness meditation is a promising basis for interventions, with particular potential relevance to psychiatric comorbidity. The successes and challenges of mindfulness meditation research are instructive for broader interactions between contemplative traditions and clinical psychological science.
Keywords: mindfulness, meditation, psychopathology, neuroscience, RDoC
INTRODUCTION
The family of practices known as mindfulness meditation (MM) has attracted increasing cultural and scientific interest during the past three decades. A remarkable range of MM-related resources are available to the general public (Cavanagh et al. 2014, Spijkerman et al. 2016). Meanwhile, the incorporation of MM into clinical interventions has inspired a wave of scientific and scholarly activity.
Why have these practices attracted such strong interest for mental health treatment? One reason may be versatility. The capacities trained by MM appear applicable to a broad range of conditions and contexts, offering approaches for addressing transdiagnostic factors and comorbidities. A second reason may be diversity: novel, well-validated treatment approaches may reach patients who do not respond to established treatments. A third reason may be interest among patients, which enhances their likelihood of engagement and adherence. Finally, MM practice may extend beyond treating clinical psychopathology to supporting resilience and well-being in the population at large (for a comprehensive review of mindfulness interventions see Creswell 2017; see also Dahl et al. 2015, Davidson & McEwen 2012).
While clinical research on MM began in the 1980s, a tremendous expansion in its scope and pace paralleled the rise of cognitive neuroscience. Accordingly, a neurobehavioral perspective has been integral to research on MM (Davidson 2003, Lutz et al. 2007, 2015). Throughout the past two decades, early exploratory studies on MM have given way to programmatic lines of experimental research and large-scale randomized controlled trials (RCTs). Recently, sufficient evidence has accumulated to allow for systematic reviews and meta-analyses in an expanding range of areas (e.g., Goldberg et al. 2017, 2018b). Meanwhile, echoing broader concerns across the fields of psychology and medicine, growing attention has focused on methodological rigor and critical evaluation of the accumulated evidence for MM (Davidson & Kaszniak 2015, Van Dam et al. 2018).
In this review, we summarize the current status of research on MM and psychopathology in terms of theory, experimental evidence, and clinical outcomes, and we identify important gaps in understanding and priorities for the field in the coming years. We approach the challenge of synthesizing a now-extensive literature by emphasizing convergent and well-replicated neurobehavioral findings and conceptually rigorous theoretical models. To contextualize this work within the broader fields of clinical psychology and cognitive neuroscience, our overview is guided by the Research Domain Criteria (RDoC) matrix developed by the National Institute of Mental Health (Insel et al. 2010).
What is Mindfulness Meditation?
In a clinical setting, most mindfulness meditation–based interventions (MMBIs) rely upon an approach first articulated in the Mindfulness-Based Stress Reduction (MBSR) course developed by Jon Kabat-Zinn and colleagues beginning in 1979 at the University of Massachusetts Medical School in Worcester, Massachusetts (Kabat-Zinn 2011). MBSR emerged as a means of addressing debilitating stress in ambulatory patients, often those with chronic pain. Since that time, MBSR and its many derivatives, such as mindfulness-based cognitive therapy (MBCT; Segal et al. 2002), have been used in numerous therapeutic contexts.
Intervention structure.
The basic structure of an MBSR course, which is generally retained in its derivative forms, consists of an 8-week program of one 2.5 to 3.5 hour session per week in a class typically consisting of 10 to 20 participants, although larger and smaller classes are possible (Santorelli 2014, Santorelli et al. 2017). A single, daylong (8 hour) silent retreat focused on MM practice is held, usually after the sixth week. During class sessions, participants learn the techniques for MM practice through instruction and meditation sessions. MBSR and its derivatives also include considerable didactic instruction in relevant topics, such as the physiology of stress. Participants are expected to engage in approximately 45 minutes of daily homework, which always includes MM practice (Parsons et al. 2017). In addition to formal MM, participants are also encouraged to cultivate mindfulness through informal practices, during which they are engaged in tasks of daily living, but in a manner that draws on the capacities trained by MM (Kabat-Zinn 1990, Santorelli et al. 2017).
Sources in contemplative traditions.
The techniques and instructions for MM found in MBSR are drawn primarily from Buddhist contemplative traditions that seek to cultivate mindfulness, an English term chosen in the nineteenth century as a translation for the Pali term sati. In its most technical sense, sati refers to a form of mental stability that prevents attention from being captured by distractors. The cultivation of that stability runs across the diverse styles of Buddhist mindfulness practices, and despite significant differences, these Buddhist traditions target similar capacities, including those discussed in the section on Targeting Core Capacities (Dunne 2015, Gethin 2015). In creating the style of MM found in MBSR, Kabat-Zinn and colleagues were influenced by the long-standing engagement between Buddhism and psychotherapy (Harrington & Dunne 2015), and in keeping with the syncretic nature of that engagement, their secularized style of MM drew from multiple Buddhist traditions (Kabat-Zinn 2011). Thus, the style of secularized MM found in MBSR is a unique blend of contemplative techniques that, while rooted in Buddhist traditions, is clearly a new formulation of mindfulness practice.
Technique and instruction.
In MBSR and its derivates, the instructions and techniques for MM practice follow a typical protocol. In terms of posture, MM practice is most commonly conducted in a seated, upright position that can ideally be maintained stably for the meditation session without excessive tension. However, in some types of MM such as the body scan, practitioners lie on their backs; likewise, MM can be practiced while walking slowly or while engaging in yoga postures. In MBSR, practitioners work up to a session of seated meditation that is 20 to 30 minutes in length, sometimes supplemented with practices such as the body scan (Kabat-Zinn 1990, Santorelli et al. 2017).
Sessions of seated MM generally begin with a focal object of meditation, usually the sensations of breathing. Practitioners are reminded to adopt a nonaversive stance toward experience, with instructions encouraging a “curious,” “friendly,” or “open” quality of attention. Within this stance, practitioners are instructed to attend moment-by-moment to the object in a “nonjudgmental” way—that is, without becoming caught in conceptual elaborations about the object—while also maintaining a relaxed vigilance for distractions, which inevitably arise. Practitioners are taught that when attention is captured by a distractor, they should recognize that the distraction has occurred and without judgment or reactivity (including reactivity about their performance in meditation), they should return their attention to the object. When the distractor consists of a chain of thoughts, practitioners are encouraged to recognize that the thoughts are merely thoughts. The goal is not to suppress thoughts, but rather to observe them as mental events (Kabat-Zinn 1990, Santorelli et al. 2017).
Targeting Core Capacities
As noted above, these typical instructions for secularized MM emerge from a complex interaction with multiple contemplative traditions, and this complexity may be one reason for the lack of a clear scientific consensus on the precise mechanisms or ingredients of MM. Nevertheless, nearly all formulations involve a core set of therapeutically relevant and interrelated capacities that are enhanced through MM training (Lutz et al. 2015).
Meta-awareness refers to the capacity of an individual to monitor the current contents and processes of the mind in a way that permits a report thereupon (Schooler et al. 2011). A paradigmatic instance of meta-awareness occurs when one notices that one has been thinking about some task-irrelevant content, as when one becomes aware that one has been daydreaming about a vacation while trying to read an article. Meta-awareness of distraction makes it possible to correct for the deviation and redirect attention back to the task at hand. Additionally, meta-awareness provides a means to monitor the quality of attention and notice its context, such as the affective states occurring with attention.
Present-centered awareness refers to sustaining the focus of attention in the present moment. This stands in contrast to becoming caught up in a chain of thoughts about the past or the future, especially in ways that involve mental time travel, or prospective and retrospective episodic memories (Suddendorf & Corballis 2007), for example, thinking about tonight’s dinner or reminiscing about a pleasant vacation. In MM, present-centered awareness is often facilitated by attending to sensory perceptions and body sensations, such as those of the breath (Farb et al. 2015), with practitioners encouraged to recognize that physical sensations occur only in the present.
Nonreactivity to experience refers to the suspension of habitual affective valuation of the current contents of experience, and in MM it is generally facilitated by adopting a stance toward experience that is nonaversive (Lutz et al. 2015), characterized in MBSR as “curious,” “accepting,” and “nonjudging” (Kabat-Zinn 1990). Within MM, a crucial role of this stance is to reduce avoidance of internal stimuli and thereby facilitate more accurate perception of mental contents (Dunne 2015; Lutz et al. 2008b, 2015).
Dereification refers to a shift in the practitioner’s relationship with thoughts, such that thoughts are no longer experienced as reified—that is, they are not experienced as real objects in the world. This shift is often described in terms of decentering, or psychological distancing, by which practitioners position themselves apart from the phenomena being observed (Bernstein et al. 2015, Kross et al. 2012), but a more precise description may be the reduction of experiential fusion (Dahl et al. 2015, Lutz et al. 2015). Much as a moviegoer might become immersed in the contents of a film and lose awareness of the distinction between film images and reality, an individual may experience thoughts as identical, or fused, with the objects that they represent (Dahl et al. 2015). When fused in this way, the thoughts about an impending final examination, for example, are experienced as real depictions of what will happen during the exam. Dereification refers to the opposite stance, such that thoughts and perceptions are no longer perceived as inherent representations of reality, but rather as mental objects that are subject to examination in their own right.
MM is also often understood to facilitate a shift in self-related processing away from a conventional and potentially maladaptive perception of the self as a discrete and unchanging entity (Lin et al. 2018). Relatedly, changes in self-related processing may reduce narrative or autobiographical thought while enhancing an awareness of the current-moment state of the self (Farb et al. 2007). Importantly, some styles of MM, especially in traditional Buddhist contexts, explicitly target such shifts as a primary goal of practice (Dunne 2015), but the form of secular MM provided in widely used MMBIs typically does not; thus, in the latter context, such shifts are understood to occur implicitly via cultivation of the other capacities described above (e.g., Hölzel et al. 2011, Vago & Silbersweig 2012).
Finally, some accounts also include compassion, a motivation to relieve suffering, as a capacity trained by MM. Compassion towards self and others may be an explicit object of focus for meditation practice (Kirby 2017, Lutz et al. 2008a). Some therapeutic interventions also introduce a notion of self-compassion—that is, a compassionate stance toward one’s own experience and suffering. While the cultivation of compassion holds significance for psychopathology (for a review, see Hofmann et al. 2011), it is not consistently integrated into widely adopted MMBIs for mental health. Accordingly, in this review, we consider it as part of the broader contemplative context for MM.
Development Through Structured Training
Over the course of MM training, practitioners are meant to develop the capacities summarized above. In principle, these capacities also become increasingly available over time for use outside of formal meditation contexts. Some changes observed following MMBIs undoubtedly emerge from factors not specific to MM, such as the socially supportive effects of a group intervention. Nevertheless, a series of hypotheses about the development of the core capacities gained through MM training can be stated as follows: (a) The capacity to sustain present-centered awareness is facilitated by the moment-by-moment focus on the meditation object; (b) meta-awareness is cultivated primarily through monitoring for distractions; (c) when, as is frequently the case, a distracting chain of thoughts captures attention and pulls it away from the object, dereification is trained by recognizing that the thoughts are just thoughts and not reality; (d) nonreactivity to experience is cultivated by rehearsing the nonaverse—or “curious” and “nonjudging”—stance toward experience; and (e) changes in self-related processing occur through dereification of self-concept and a decrease in autobiographical, narrative thinking.
The formulation of MM presented above is compatible with a range of practice styles. Neuroscientific research has often used a heuristic distinction between Focused Attention (FA) and Open Monitoring (OM) styles of MM (Lutz et al. 2008b, 2015). In an FA style, the practitioner seeks to sustain focus on a chosen object of meditation, and the emphasis is on sustaining that focus. OM styles, in contrast, emphasize sustaining present-centered awareness and monitoring experience without restricting attention to a single object of focus. MBSR training begins with focus on an object, but an OM style—usually called “choiceless awareness” (Kabat-Zinn 1990)—is introduced as training progresses.
Mindfulness as a Psychological Construct
Some research has investigated mindfulness as a psychological construct, conceptualized in both state and dispositional trait forms. The proposed mindfulness construct has been operationalized via self-report instruments such as the Mindful Attention Awareness Scale (Brown & Ryan 2003), Toronto Mindfulness Scale (Lau et al. 2006), and Five Facet Mindfulness Questionnaire (Baer et al. 2006). These instruments have shown responsiveness to mindfulness interventions, associations with positive psychological outcomes, and incremental validity relative to measures of related constructs such as attentional control (Quaglia et al. 2015). However, the aforementioned lack of definitional consensus complicates the straightforward use of a singular mindfulness construct (Grossman & Van Dam 2011). External validity has been an additional challenge, with mindfulness measures showing signs of demand characteristics (Grossman & Van Dam 2011) and not responding selectively to mindfulness training (Goldberg et al. 2015). The interpretation of items and the constructs tapped also appears to vary across populations; for example, cross-study comparisons of one scale revealed higher ratings in binge drinkers than experienced meditators, driven partially by items related to somatic sensations (Grossman 2008). Thus, while work continues to address these issues, we opt here to emphasize the investigation of MM via neurocognitive constructs and measures.
Clinical and Research Paradigms
The majority of evidence presented in this review derives from one of three research paradigms, each offering distinct contributions. The first is the study of structured, secular MMBIs that incorporate formal meditation practice into a format similar to MBSR, as described above. The effects of such interventions are important because they are the most widely disseminated and influential in mental health treatment, and they form the primary basis for investigating the impact of MM on clinical outcomes (Goldberg et al. 2018b, Goyal et al. 2014). A second paradigm includes brief MM trainings and laboratory-based tasks. This approach allows for more flexiblility in the format and setting of delivery and more detailed experimental study of cognitive and affective processes in MM (e.g., Tang et al. 2015). A third paradigm is case–control research on long-term MM training undertaken in both secular and nonsecular practice communities. Evidence from such training offers insights into the effects of sustained practice (e.g., Gotink et al. 2016) and may also reveal changes that are undetectable or absent during earlier stages of MM practice (Davidson & Kaszniak 2015, Zeidan & Vago 2016).
Another family of mindfulness-informed psychotherapeutic interventions incorporates primarily informal training and conceptual material from mindfulness traditions without a substantial component of formal meditation. Acceptance and commitment therapy incorporates the principles of mindfulness practice into a broader model based on behavior theory that emphasizes the role of context and linguistic framing in psychological problems and aims to increase psychological flexibility (Hayes et al. 2006). In dialectical behavior therapy (DBT), principles of mindfulness form a common thread supporting the development of capacities for emotion regulation, distress tolerance, and interpersonal effectiveness (Linehan 1993). Notably, DBT has shown efficacy in the treatment of borderline personality disorder, a condition for which effective treatments were previously lacking (Lynch et al. 2007). We do not identify borderline personality disorder as a target for MMBIs: The informal approach in DBT is taken specifically because of Linehan’s (1993) observation that such patients typically find formal meditation difficult to tolerate. However, the success of DBT in treating patients with borderline personality disorder and as a treatment for other refactory populations (Lynch et al. 2007) demonstrates the broader potential for integrating principles and concepts from contemplative traditions to contribute to advances in psychological treatment. Although we do not attempt an in-depth review of acceptance and commitment therapy, DBT, and other mindfulness-informed psychotherapies, their rich relationship with formal MM training and Buddhist contemplative traditions has inspired substantial discussion elsewhere (e.g., see Dimidjian et al. 2016).
COGNITIVE AND AFFECTIVE MECHANISMS
Psychopathology is now widely understood to originate in the dysregulation of underlying cognitive and affective systems whose functions cut across standard categories of psychiatric diagnosis (Insel et al. 2010). Therefore, understanding how MM influences these core neurobehavioral systems is critical to modeling its effects on mental health. Accordingly, we next discuss how the effects of MM training may map onto the RDoC domains of cognitive systems, positive valence systems, and negative valence systems at multiple levels of analysis, including neural circuits, behavior, self-report, and standard laboratory paradigms.
The range of mechanisms of action proposed in theoretical accounts of MM is substantial enough that cataloguing them fully would be infeasible (see, e.g., Baer 2003; Chambers et al. 2009; Creswell & Lindsay 2014; Garland et al. 2014a, 2017; Hölzel et al. 2011; Lutz et al. 2015; Teasdale & Chaskalson 2011a,b; Vago & Silbersweig 2012). However, robust evidence bearing on these proposals, particularly in the context of MMBIs for mental health, remains comparatively more limited (see, e.g., Alsubaie et al. 2017, Gu et al. 2015, van der Velden et al. 2015). Accordingly, we focus on a subset of potential mechanisms that have particular relevance to psychological disorders and for which relevant neurobehavioral findings are available.
Cognitive Systems
The core capacities targeted by MM are intimately linked with cognitive function. For any meditative practice, working memory is needed to maintain a task set throughout the session, and styles involving a specific object of focus further require the maintenance of sustained attention toward that object. A central aspect of MM in particular is responding to attentional capture by distracting thought processes. Attentional control is needed to maintain sufficient awareness of mental processes that distraction is detectable; cognitive control circuits must be involved to detect the discrepancy between mental contents and the meditative task set; and inhibitory systems must be enlisted to disengage and return mental focus to the intended task (Lutz et al. 2008b, 2015).
Considerable research has been conducted to examine the effects of MM practice on cognitive systems at the neural level. Tang et al. (2015) note that MM practice relies on multiple high-level mental functions, and, thus, changes in neural function are likely to manifest across large-scale networks in the brain. Lutz et al. (2015) identify three networks with particular relevance for the cognitive aspects of MM training. The first of these is a central executive network (CEN) that is involved in the top-down regulation of attention and includes nodes in the prefrontal cortex (PFC) and parietal cortex. Second, a salience network, involved in bottom-up attentional orienting, incorporates the anterior insula, dorsal anterior cingulate cortex (ACC), amygdala, and dopaminergic midbrain regions. Third, the default mode network (DMN) is concentrated in midline cortical regions, with the posterior cingulate cortex (PCC) and medial PFC as two hub regions. Initially identified by increased activation during rest relative to task-oriented states, the DMN is also linked with spontaneous thought (e.g., mind wandering; Schooler et al. 2011) as well as self-referential thought (Lin et al. 2018).
Altered function has been observed within all of these networks, both during MM practice itself and during the performance of cognitive tasks subsequent to MM training. A recent meta-analysis of functional activations across multiple styles of meditation (Fox et al. 2016) found multiple clusters of consistent activation and deactivation associated with MM-style practices: Among meditation techniques, both FA and OM styles of practice were associated with increased activation in the anterior insula and uniquely activated regions of the dorsal ACC and midcingulate cortex; FA was further distinguished by deactivations in the PCC; and OM was distinguished by activations in the mid–anterior insula and lateral regions of the PFC. The DMN has been a particular focus of investigation (Brewer & Garrison 2014). Functional connectivity within subnetworks of the DMN appears to increase with MM practice, while connectivity between major DMN hubs appears to decrease (Mrazek et al. 2014). Finally, experienced MM practitioners have shown reduced DMN activation during OM-style practice as well as increased resting-state functional connectivity between regions of the DMN and CEN during rest, consistent with greater capacity to regulate self-referential discursive thinking (Brewer et al. 2011, Mrazek et al. 2014).
Executive functioning.
Given the neural changes observed, is it possible that MM training could address psychopathology by modulating or enhancing core cognitive functions? The answer to this question has strong implications for MM-based clinical intervention since virtually all forms of psychopathology are characterized by deficits or dysfunctions in cognitive processing.
With regard to MM-related changes in performance on standard neurocognitive tasks, findings have been modest. Chiesa et al. (2011) reviewed 23 studies of MM effects on cognitive abilities and found effects primarily on attentional performance: MMBIs, mostly in health samples, were associated with some improvements in the selective and executive components of attention, while in case–control studies of longer-term practitioners, MM training was associated with improvements in sustained attention. Gallant (2016) examined MM training and executive functioning across the subdomains of response inhibition, working memory updating, and mental set shifting. Among 12 studies (10 intervention, 2 case–control) that included measures of executive function, Gallant (2016) noted positive effects in 5 of 6 studies on inhibition; and working memory updating was improved in all 3 studies that tested it, albeit using measures that depend on sustained attention. However, only 1 of 5 studies examining set shifting showed performance improvement. Using more restrictive criteria, Lao et al. (2016) reviewed neuropsychological outcomes associated specifically with standardized 8-week MMBIs. Among 18 qualifying studies, Lao et al. (2016) found minimal support for improvements in attentional performance or executive functioning, noting that positive findings on inhibition were potentially confounded with changes in motivation and task strategy.
In light of these findings, expectations should be tempered for MMBI-related enhancement in classical measures of cognitive function, although studies of experienced meditators, while correlational in nature, suggest that improvements may emerge with longer-term training (e.g., Lutz et al. 2008b). The possibility that MM protects against degradation in cognitive abilities due to stress, as observed in predeployment military personnel by Jha et al. (2010, 2015), also deserves further investigation. Critically, evidence in clinical populations remains sparse and was not examined separately in the above reviews. Thus, it remains important to include carefully selected neurocognitive measures in clinical MMBI research designs.
Targeted capacities.
In contrast to conventional executive functioning measures, training effects have been more apparent on tasks and measures more directly linked to the capacities trained in MM. For example, Lao et al.’s (2016) review of cognitive performance measures did observe MMBI-related improvements on behavioral tasks designed to assess meta-awareness, cognitive flexibility, and memory specificity. Findings on meta-awareness, in particular, accord with a separate line of experimental studies on mind wandering in the form of task-unrelated thought (Schooler et al. 2011). In paradigms that combine spontaneous and timed probes of participants’ mental focus on task-relevant versus task-unrelated thought, validated by their successful prediction of behavioral indicators of distraction, MM training has been associated with both reduced mind wandering and increased meta-awareness of distraction (Mrazek et al. 2014).
Attentional capture.
Developing the capacity to detect and disengage from attentional capture by future- or past-orienting thinking (mental time travel; Suddendorf & Corballis 2007) holds a special theoretical relevance for psychopathology. Task-unrelated thought, neurally subserved by the DMN, is known to be biased toward negative affect and self-relevant content, both hallmarks of maladaptive thinking patterns (Watkins 2008). The inability to disengage from such patterns leads to repetitive negative thinking, which is believed to contribute substantially to depression, anxiety, addictive craving, and pain-related distress among other pathologies (e.g., Miloyan et al. 2014, Tapper 2018, Zeidan & Vago 2016). As we discuss applications of MM to specific clinical targets, we detail the empirical findings that provide relatively robust support for reductions in attentional capture as an important transdiagnostic mechanism by which MM practice can ameliorate psychiatric symptoms.
Affective Systems
The RDoC matrix (Insel et al. 2010) distinguishes between negative valence systems that drive responses to aversive stimuli and positive valence systems underlying responses to motivational stimuli. Negative valence processes potentially impacted by MM include loss, acute threat, and sustained threat (Garland et al. 2017, Hölzel et al. 2011, Tang et al. 2015). MM also may impact positive valence–related processes including approach, responsiveness to reward, reward anticipation, and habit (Garland & Howard 2018, Hölzel et al. 2011, Lutz et al. 2015, Tang et al. 2015). Four key ways in which MM may modulate these systems are enhanced emotion awareness, altered emotional reactivity, promotion of cognitive reappraisal, and altered reward processing. Notably, in recent meta-analyses (Fox et al. 2014, 2016), MM practice was consistently associated with changes in the structure and function of regions integral to emotion appraisal, reactivity, and regulation, including the amygdala, ACC, ventromedial PFC, and hippocampus.
Enhanced emotion awareness.
Through cultivating meta-awareness of mental processes and contents and maintaining present-focused attention, MM may improve the ability to detect and recognize emotional states, thus allowing for their regulation via conscious executive control and entrainment of automatic regulatory circuits (Lutz et al. 2015). One way this may occur is through improved interoception, or the perception of internal bodily states (Farb et al. 2012, 2015), although evidence for MM-related improvements in interoception has been mixed (Farb et al. 2015, Haase et al. 2016, Khalsa et al. 2008).
Altered emotional reactivity.
Cultivation of nonreactivity and dereification may alter the coupling between perception and the appraisal of environmental stimuli (Lutz et al. 2015). Clinicians familiar with exposure therapy for panic disorder know that on its own, heightened perceptual awareness of stimuli such as bodily sensations can, in fact, heighten emotional reactivity and exacerbate anxiety symptoms (McNally 2007). However, it is proposed that the incorporation of dereification and nonreactivity in MM training reverses this effect (Creswell & Lindsay 2014). In particular, the repeated experience of affective states without avoidance or distraction by elaborative thoughts may constitute a form of exposure, leading to habituation or extinction of conditioned emotional reactions (Baer 2003, Phelps et al. 2004, Tang et al. 2015). Notably, reduced amygdala activation during an affect-eliciting task has been observed in experienced MM practitioners relative to nonmeditating controls (Kral et al. 2018). Similar effects were seen for participants in MBSR relative to an active control intervention, who furthermore, exhibited increased connectivity between the amygdala and ventromedial PFC (Kral et al. 2018), a key circuit in extinction learning (Phelps et al. 2004).
Cognitive reappraisal.
Cognitive reappraisal involves adopting an altered mental interpretation of a situation or stimulus to promote a more adaptive emotional response. MM training does not explicitly target cognitive reappraisal (Lutz et al. 2015), but it has been proposed to facilitate it indirectly in several ways (e.g., Garland et al. 2014a). Specifically, practicing nonreactivity by decoupling a stimulus from its habitual appraisal value may promote cognitive flexibility and, thus, facilitate more adaptive appraisals (Lutz et al. 2015). Present-centered awareness may also promote reappraisal of inaccurate valuations via the gathering of novel information from the environment (Garland et al. 2014a). While behavioral evidence associating MM training with increased cognitive reappraisal is lacking, reductions in self-reported stress have been shown to be mediated by self-reported reappraisal use among MMBI participants (Garland et al. 2011).
Altered reward processing.
Evidence regarding the effects of MM on reward processing has emerged from the study of reward-related disorders. For example, a brief, lab-based instruction to mindfully attend to smoking images reduced craving, activation of the subgenual ACC, and ACC connectivity to the insula and ventral striatum compared with passively viewing the images (Westbrook et al. 2013). MM training was also associated with lower activation of the amygdala and insula during exposure to a personally relevant stressful stimulus compared with a standard cognitive behavioral treatment for smokers, and lowered stress-related activation in these regions was associated with reduced smoking among participants (Kober et al. 2017). Finally, experienced MM practitioners have shown altered neural activity relative to nonmeditators during reward anticipation, with reduced caudate activation and connectivity with bilateral insula during the anticipation of monetary reward and reduced activation of the ventromedial PFC at reward receipt (Kirk et al. 2015).
Research on the cognitive and affective mechanisms of MM is still at a preliminary stage, and generating a robust evidence base will require overcoming methodological limitations in the literature. One obstacle is the reliance on self-reported measures for key mechanistic constructs, which allows for potentially confounding demand characteristics. Such measures also frequently rely on participants’ capacities for accurate introspection, which may be confounded with MM practice expertise (Davidson & Kaszniak 2015). Interpretations of the neural evidence of the mechanisms of MM also strongly depends on reverse inference, from brain activity to behavior, a practice that can easily mislead (Van Dam et al. 2018). Both of these obstacles can be addressed by developing and using robust behavioral tasks to assess components of MM training, such as those developed for the study of meta-awareness and distraction (Mrazek et al. 2014). Nevertheless, enough evidence has accumulated to suggest that MM does have significant effects on at least some mechanisms of action that are directly relevant to psychopathological processes.
APPLICATIONS TO PSYCHOPATHOLOGY
MM has been studied extensively for the treatment of depression, pain, anxiety, and substance use. For these areas, we briefly review the conceptual relevance of MM, the clinical and translational evidence for the applicability of MMBIs, neurobehavioral evidence regarding the potential mechanisms of action from an RDoC perspective, and priorities for future research. In discussing outcomes, we feature findings from a recent meta-analysis by Goldberg et al. (2018b), which addresses the transdiagnostic nature of MM by examining effect sizes on disorder-specific symptoms across diagnostic conditions and differentiates effects by control condition [wait-list, specific or nonspecific active control, or evidence-based treatment (EBT); see Figure 1]. While Goldberg et al. (2018b) confirmed that the MMBI literature appears to be affected by the common issue of publication bias (Coronado-Montoya et al. 2016), the application of bias correction through trim-and-fill analyses did not alter the direction or statistical significance of the observed effects.
Figure 1.
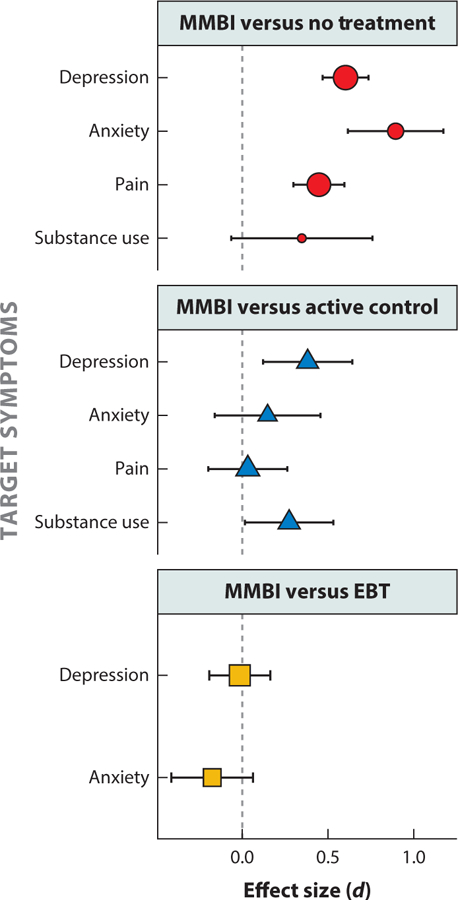
Efficacy of mindfulness meditation–based interventions (MMBIs) for well-established psychiatric targets, by comparison condition. Across disorders, MMBIs show efficacy relative to no treatment; they match or exceed active control interventions; and they perform on par with established evidence-based treatment (EBT). Points in the plot are sized proportionally to their weight in the meta-analysis by Goldberg et al. (2018b). Summary results are presented when at least four studies were available for a given comparison. Figure adapted with the authors’ permission from Goldberg et al. (2018b).
Depression
Research on the application of MMBI to the treatment of depression, most notably the prevention of relapse in major depressive disorder, is arguably the most robust research corpus focused on a specific psychiatric condition. The early development and codification of MBCT (Segal et al. 2002) has facilitated a series of RCTs coupled with basic research on the mechanisms of MBCT.
Clinical applications.
MBCT has been shown to reduce the risk of depressive relapse for patients with recurrent depression at 60-week follow-up when compared with patients not receiving MBCT (hazard ratio = 0.69; Kuyken et al. 2016). It also appears that MBCT may be effective for treating current depression relative to wait-list conditions at posttreatment (d = 0.71 across ten studies) and similar to other active therapies (d = 0.002 across six studies; Goldberg et al., in press), although less is known about its effects at long-term follow-up. Evidence examining the efficacy of MMBIs in general for depression suggests superiority to no treatment (d = 0.59) and other active therapies (d = 0.38) and equivalence to gold-standard EBTs, such as cognitive behavioral therapy (CBT) or antidepressant medications (d = −0.01; Goldberg et al. 2018b), with similar results at long-term follow-up. An exemplar of rigorous RCTs in this area is a trial conducted by Kuyken et al. (2015) that compared MBCT to antidepressant medications (n = 424), finding no differences between the treatments in regard to depressive relapse or cost-effectiveness. A significant strength of research on MMBIs for depression is the frequency of comparison with frontline EBTs (e.g., k = 10 comparisons in 1,064 participants treated with EBTs in Goldberg et al. 2018b).
Implicated mechanisms.
Mechanistic research supports the efficacy of MBCT in targeting depressogenic cognitive processes. MM training is designed to help practitioners exit depressive rumination by returning attention to the present moment, with dereification also reducing the emotional salience of ruminative thought processes. Indeed, in reviews of mechanistic and mediational evidence, both self-reported and laboratory measures of rumination have been predictive of treatment response (Alsubaie et al. 2017, van der Velden et al. 2015). MBCT has also been found to reduce overly generalized autobiographical memory (Williams et al. 2000) and increase the ability to suppress irrelevant mental sets (Greenberg et al. 2017). Neurally, this account is supported by findings of MM-related decreases in DMN activation and increases in DMN connectivity with the dorsolateral PFC, with associations of the former with self-referential and discursive thought and of the latter with top-down attentional control (Brewer et al. 2011).
Research priorities.
With a substantial body of clinical trial research supporting MM for preventing depressive relapse, dissemination and implementation studies may be particularly relevant at this stage. Work on technology-augmented or technology-based forms of MBCT has begun (e.g., Dimidjian et al. 2014) and may help increase access. The mood components of medical conditions (e.g., cancer, diabetes; Tovote et al. 2014) may also be a fruitful avenue for further MMBI development. Research linking MM with the neural circuitry underlying physical health and illness may also be particularly valuable, as MM has been found to modulate inflammatory and endocrine processes that are implicated in many chronic physical illnesses (e.g., Rosenkranz et al. 2013).
Anxiety
Despite early interest in the application of MM to anxiety disorders (Kabat-Zinn et al. 1992), significantly less research has evaluated MM for anxiety relative to depression. No single MMBI has emerged as a dominant MM-based treatment approach for anxiety, although trials have evaluated both MBCT (e.g., Kocovski et al. 2013) and MBSR (e.g., Goldin et al. 2016) for this purpose.
Clinical applications.
MMBIs appear to reduce anxiety symptoms in patients when compared with no-treatment controls (e.g., d = 0.89; Goldberg et al. 2018b). However, their efficacy relative to other active interventions is less clear. MMBIs appear similar to other therapies (d = 0.15) and frontline EBTs, which include exposure-based therapies (d = −0.18; Goldberg et al. 2018b). Here, while MMBIs show efficacy, further work is needed to clarify the specific benefits of this approach to treatment. An exemplar in this regard is a study by Hoge et al. (2013) that randomly assigned 89 participants to either MBSR or a stress management psychoeducation group. Both groups showed comparable reductions in clinician-rated anxiety. However, relatively larger reductions were found in the MBSR condition on measures of clinician-rated global severity, self-reported anxiety, and stress reactivity in response to a laboratory-based social stress task (the Trier Social Stress Test).
Implicated mechanisms.
As with depression, a primary candidate mechanism for the effects of MM on anxiety is a reduction in repetitive negative thinking (Gu et al. 2015). For example, one RCT of MBSR for social anxiety also found indications of changes in self-related processing: Among MBSR participants, the reduction in negative self-related beliefs and associated activity in the dorsomedial PFC (a structure associated with self-relevant cognition) were both predictive of treatment response (Goldin et al. 2012). Another obvious candidate mechanism is exposure leading to reduced reactivity in individuals exposed to both cognitive and physiological symptoms of anxiety during MM practice (Baer 2003, McNally 2007). Decreased self-reported anxiety in anxiety patients following brief MM training was associated with increased activation in regions of the brain that are important in affective appraisal and responding (the ventromedial PFC, ACC, and insula) during meditation compared with rest (Zeidan et al. 2014). Facilitation by MM training of top-down regulation of reactivity to ambiguous stimuli is consistent with an observed correlation between increased PFC–amygdala connectivity and reduced symptoms in patients withgeneralized anxiety following an MBSR course (Hölzel et al. 2013). Dereification of anxiety-related cognitions may contribute to both of these processes, with self-reported dereification having been shown to mediate the effects of MBSR on symptoms of generalized anxiety (Hoge et al. 2015).
Research priorities.
Paralleling MBCT for depression, it may be valuable to develop and test MMBIs specifically designed for anxiety. Efforts to customize MMBIs to anxiety symptoms would be consistent with meta-analytic evidence that symptom-focused psychotherapies for anxiety are most effective (Yulish et al. 2017). Other important questions for future research include determining the degree to which MMBIs are acceptable vis-à-vis frontline exposure-based treatments with known risks for drop out (Imel et al. 2013), although the evidence does not suggest that attrition differs between MM and comparison conditions (Hedman-Lagerlöf et al. 2018).
Pain
Because the first MBSR curriculum was designed to address the challenges of coping with pain in clinical settings (Kabat-Zinn et al. 1985), pain syndromes have been important targets for MMBIs. This emphasis can be traced further back to traditional MM instructions on the use of mindfulness training to decouple pain sensations from emotional distress (Thanissaro Bhikkhu 1997).
Clinical applications.
Reduced pain symptoms and improved quality of life in response to MM training were first reported in empirical trials of MBSR (Kabat-Zinn et al. 1985). A recent quantitative review of pain-related outcome measures across 24 studies with a cumulative total of 1,534 participants found MMBIs superior to no intervention (d = 0.45) and on par with active controls (d = 0.03) (Goldberg et al. 2018b). These conclusions were consistent with a previous comprehensive meta-analysis of meditation-based interventions (Goyal et al. 2014). MMBIs have shown significant benefits for quality of life and more limited evidence for reductions in pain across multiple pain-related syndromes including fibromyalgia, migraine, and chronic pelvic pain (Hilton et al. 2017). Prominent among recent studies is a large (n = 342) RCT of MBSR for low back pain, which found improvements in functioning and pain-related distress relative to treatment as usual (TAU) that were equivalent to those observed in a CBT comparison condition and were sustained at 2-year follow-up (Cherkin et al. 2017).
Implicated mechanisms.
MM practice appears to have neural and behavioral effects on pain processing distinct from opioids, placebo expectancy, or sham interventions (Zeidan et al. 2015, 2016). After brief MM training, reductions in perceived pain intensity and unpleasantness have been associated with activation in appraisal circuitry including the orbitofrontal cortex, ACC, and anterior insula (Zeidan & Vago 2016). Among experienced MM practitioners, the selective reduction in pain unpleasantness relative to intensity (Lutz et al. 2013, Perlman et al. 2010) also suggests decreased affective reactivity. The deactivation of sensory gating circuitry in the thalamus during pain suggests that the present-centered awareness cultivated in MM may also modulate pain signaling at a perceptual stage (Zeidan et al. 2015). Present-moment awareness may also contribute to the inhibition of aversive anticipatory cognition: Experienced MM practitioners exhibit reduced activity in the amygdala and salience network regions (the ACC and anterior insula) between cue and onset of painful stimuli (Lutz et al. 2013). Together, these findings indicate that MM-related changes in sensory processing reactivity, appraisal, and pain-related cognition all may contribute to the amelioration of pain-related distress.
Research priorities.
While RCTs have established the efficacy of MMBIs for pain, and experimental studies of brief training suggest that MM provides pain relief via distinctive mechanisms, mechanistic studies of fully developed MMBIs are still needed to combine these two lines of evidence. In particular, because pain-related syndromes are characterized by a variety of pathogenic alterations in neural pain processing (Bushnell et al. 2013), it will be important to carry out mechanistic studies of MMBIs in specific clinical populations. Finally, for public health reasons, transdiagnostic applications of MMBIs to chronic pain in the context of long-term opioid use should be a high priority (see Garland et al. 2014c for one such initiative).
Substance Use
During the past decade, there has been increasing interest in applying MMBIs to substance use disorders, including the development of several novel MMBIs targeted at treating these disorders [e.g., mindfulness-based relapse prevention (MBRP) for alcohol and drug use disorders (Bowen et al. 2014); mindfulness-oriented recovery enhancement (MORE) for opiate use disorder (Garland et al. 2014b)].
Clinical applications.
MMBIs for substance use disorders have typically joined content and structure similar to MBSR with CBT-derived addiction treatment components (e.g., risk assessment for relapse prevention; Bowen et al. 2014). Evidence for MMBIs for substance use disorders is generally promising. Li et al. (2017) evaluated 34 RCTs, finding that MM treatments were superior to control conditions (e.g., TAU, CBT) in reducing substance use frequency, use-related problems, and craving. Goldberg et al. (2018b) reported that MMBIs were superior to other active therapies (d = 0.27), with MM outperforming EBTs for smoking cessation (d = 0.42). These findings contrast with Goyal et al.’s (2014) report of insufficient trials to assess these outcomes. This discrepancy may be due, in part, to additional studies having been published in recent years. One exemplar study in this area is a trial conducted by Bowen et al. (2014) comparing MBRP to relapse prevention (based on CBT) and TAU (12-step-based treatment) in 286 participants with substance use disorders, with MBRP showing fewer days of substance use compared with both relapse prevention and TAU at 12-month follow-up.
Implicated mechanisms.
Proposed mechanisms underlying the efficacy of MMBIs for substance use disorders include response inhibition and extinction (Tapper 2018), as well as changes in reward processing (Garland & Howard 2018). MM-related reductions in smoking have been associated with lower amygdala and insula activation in response to stress cues, and MM training reduced stress-related activation in these brain regions compared with CBT (Kober et al. 2017). It has also been proposed that MM may increase top-down regulation, reducing automaticity (or autopilot) associated with substance use and decreasing drug-use attentional bias (Brewer et al. 2013). Moreover, the reduction in smoking behavior following brief MM training has been associated with increased resting activation within the ACC and medial PFC, thus linking the activation of these emotion-regulatory brain regions to relevant behavioral outcomes (Tang et al. 2016).
Research priorities.
MMBIs may be promising candidates for incorporation into recently developed adaptive interventions that harness mobile technology to deliver contextually tailored treatment (e.g., in response to situations with high relapse risk; Gustafson et al. 2014, Nahum-Shani et al. 2018). Given strong neuroscientific models of substance use (Koob & Volkow 2016), the use of mechanistic clinical trial designs combining neural and behavioral measures will be especially valuable in this area.
EMERGING TARGETS
Attention Disorders
Interest in the application of MMBIs to attention-deficit/hyperactivity disorder (ADHD) has increased in recent years (Cairncross & Miller 2016). Given that MM involves the cultivation of specific attentional capacities (Lutz et al. 2008b), the pairing of MM with ADHD is a logical clinical application. However, much of the research on MMBIs for ADHD has been limited to non-RCTs. Cairncross & Miller (2016) reviewed 10 studies (4 with wait-list control, 6 with pre-and posttest design) with adult, child, and adolescent samples, and they reported moderate effects on inattention (d = −0.66) and hyperactivity (d = −0.53). Both of the RCTs in adults included in this meta-analysis (Hepark et al. 2015, Mitchell et al. 2017) reported improvements in self-rated and clinician-rated ADHD symptoms in the MM group relative to wait-list controls, with moderate effect size. Mitchell et al. (2017) found no group differences on neurocognitive tests of attention and executive function, albeit within a small sample (n = 20). Therefore, one potential mechanism of action of MMBIs for ADHD may be improved meta-awareness leading to a reduction in attentional capture by task-unrelated thoughts, given findings of MM-related improvement in these capacities in both laboratory tasks and samples of experienced meditators (Lao et al. 2016, Mrazek et al. 2014). Currently, there is a dearth of RCTs assessing the impact of MMBIs on ADHD. Mechanistic RCTs that examine how performance on meta-awareness tasks relates to behavioral symptoms of ADHD may be particularly valuable.
Posttraumatic Stress
Posttraumatic stress disorder (PTSD) and related syndromes are characterized by hyperactivation and context-insensitivity of negative affective systems, accompanied by avoidance of trauma-relevant stimuli. The cultivation of present-centered awareness in formal MM has the potential to improve the regulation of negative affective systems by modulating immediate emotional reactivity and facilitating exposure to unpleasant stimuli. Meanwhile, reduced cognitive elaboration and increased flexibility in appraisal due to dereification may facilitate the restructuring of maladaptive trauma-related cognitions.
Because tolerability, adherence, and retention are challenges in trauma-focused treatment (Imel et al. 2013), adapting MMBIs to PTSD requires paying particular attention to these areas. Suitability must be considered as well: For individuals presenting with extreme emotion dysregulation, attempting to engage nonreactively with internal stimuli for sustained periods in formal MM practice may prove excessively challenging, and using an intervention focused on informal (i.e., not meditation-based) mindfulness practices accompanied by self-regulation skills has been recommended as an effective alternative (Linehan 1993).
The RCT evidence base for trauma-focused MMBIs remains limited. However, an initial meta-analytic review of 18 clinical trials supports their effectiveness relative to a wait-list control in a broad range of conditions (Hedges’ g = −0.44; Hopwood & Schutte 2017), with symptom reduction further associated with the extent of MM training. Neuroimaging of military veterans participating in a mindfulness-based exposure therapy (MBET) protocol developed by King et al. (2016b) found that MM practice was associated with increased activation of the medial PFC and reduced activation of the amygdala during the viewing of angry faces, consistent with the inhibition of socioemotional threat signaling. Participants in the MBET intervention, but not those in a group psychotherapy control intervention, showed increased connectivity between regions of the DMN (PCC) and CEN (dorsolateral PFC), once again suggesting improved regulation of negative repetive thought (King et al. 2016a). A critical issue for ongoing research on trauma-focused MMBIs is to explore their role in multicomponent treatments; for example, MMBIs may have particular value for enhancing emotion regulation skills prior to exposure therapy, for addressing comorbid and residual symptoms, and for relapse prevention (King & Favorite 2016).
Disordered Eating and Obesity
The majority of the research on MMBIs for disordered eating has focused on applications to unrestrained eating (i.e., binge eating and obesity) rather than restrictive eating (i.e., anorexia nervosa). The most widely studied MMBI in this area is mindfulness-based eating awareness training (MB-EAT; Kristeller et al. 2014). Within MB-EAT, MM is included to bring increased awareness to eating experiences (e.g., awareness of satiety cues); increase hedonic pleasure from smaller amounts of food; disrupt the link between harsh self-judgment, eating behavior, and negative affect; and increase self-acceptance (Kristeller & Wolever 2010). Three recent meta-analyses have examined the effects of MMBIs on weight and eating outcomes, two of which failed to find evidence for MMBIs on weight loss or body mass index (BMI), although positive effects of MMBIs were noted on measures of eating attitudes and behaviors (Rogers et al. 2017, Ruffault et al. 2017). Of note, analyses may have been underpowered to detect small effects on BMI (e.g., g = 0.30 to 0.34; Rogers et al. 2017). Goldberg et al. (2018b), who combined eating- and weight-related outcomes, reported a large effect when MMBIs were compared with no treatment (d = 0.79) and no difference when compared with other active therapies (d = 0.08). While several potential mechanisms of action have been proposed (e.g., enhanced emotion regulation and self-regulatory abilities, increased awareness of interoceptive cues; Alberts et al. 2012, Kristeller et al. 2014), few studies have examined these mechanisms of change directly. One recent study found that changes in reward-driven eating (i.e., eating due to loss of control, lack of satiety, and preoccupation with food) mediated the effects of MM-based treatment on weight loss at 12-month follow-up (Mason et al. 2016). Given the often-lengthy course of metabolic changes and evidence that treatment effects are moderated by the length of follow-up (Ruffault et al. 2017), studies including long-term follow-up are crucial.
Serious Mental Illness
The possibility that MM may be safe and efficacious for treating serious mental illness, including psychotic and bipolar disorders, has only recently been proposed. Given the public health costs associated with serious mental illness, along with the side effect profiles of many antipsychotic and mood stabilizer medications, there is a recognized need for effective behavioral therapies (Murray et al. 2017). As with other disorders, interventions have been developed combining MM training with elements from standard CBT-based treatments (e.g., identifying negative schemata; Chadwick et al. 2016). Goldberg et al. (2018b) included seven studies (n = 456) in a meta-analysis examining the effects of MMBIs relative to no treatment on symptoms of psychosis, finding moderate effects at posttreatment (d = 0.50) and large effects at follow-up (d = 1.18). Chu et al. (2018) reported no effects of MMBIs on depression or anxiety symptoms in patients with bipolar disorder across three RCTs in another meta-analysis, although effect sizes were in the moderate range (g = 0.46 and 0.58 for depression and anxiety, respectively). MMBIs for psychosis have emphasized the application of mindful awareness to psychotic experiences (Chadwick et al. 2016, Wang et al. 2016), with the intention of reducing distress and disturbance associated with these experiences rather than reducing their frequency. While evidence does suggest that distress and disturbance associated with psychosis reduces following MMBIs (Chadwick et al. 2016), it has not been established that these changes predict reductions in psychotic symptoms. There are few studies that specify unique mechanisms of action in MMBIs for bipolar disorder, although mechanisms proposed for treating depression and anxiety (i.e., improved emotion regulation, reduced repetitive negative thinking) may be relevant. It will be important to assess the potential iatrogenic effects of MM on psychotic symptoms, given evidence that some forms of intensive meditation practice have been associated with psychotic experiences (Lindahl et al. 2017).
PRACTICAL CONCERNS
Demonstrating the efficacy of MMBIs in research settings does not ensure their effectiveness in real-world clinical practice. Important considerations and potential stumbling blocks associated with bringing MMBIs to health-care consumers include issues of implementation and dissemination; training and treatment fidelity; questions regarding format, duration, and setting; and issues of access and cultural fit.
Implementation and Dissemination
As noted by Dimidjian & Segal (2015), the vast majority of research on MMBIs has been focused on intervention generation and refinement (i.e., National Institutes of Health Stage I research). For several disorders reviewed here, numerous efficacy studies (i.e., testing interventions in research settings; Stage II) have been conducted, many including desirable design features, such as active comparison conditions, lengthy follow-up periods, and large sample sizes (Goldberg et al. 2017). In contrast, few studies have examined the process or impact of implementing MMBIs in actual clinical practice, either through efficacy trials in community clinics (i.e., testing in community settings while maintaining a high level of control and oversight; Stage III), effectiveness studies (i.e., implementation by community providers in routine conditions; Stage IV), or explicit implementation and dissemination research (i.e., studying methods for deployment in community settings; Stage V). Indeed, MBCT appears to be the only MMBI for which there is implementation and dissemination research.
Due to the rigorous research that has been done evaluating MBCT, it may serve as a valuable test case for the implementation and dissemination of other MMBIs. MBCT has been recommended for preventing depressive relapse by the United Kingdom’s (UK) National Institute for Health and Care Excellence (NICE 2018). Yet despite this approval and even within a single-payer health-care system, implementation and dissemination has not been straightforward. Crane & Kuyken (2013) discuss a host of barriers identified by stakeholders (e.g., clinicians and MBCT teachers working in the UK’s National Health Service) associated with the implementation of MBCT. The majority (59%) of respondents reported that MBCT services either do not exist within their organization or do not play a major part and operate with limited organizational support. Respondents also identified structural, cultural, educational, physical, and technological challenges. It is likely that similar barriers will be relevant for other MMBIs that garner empirical support warranting their implementation and dissemination within health-care systems.
Training and Treatment Fidelity
One implementation challenge highlighted by Crane & Kuyken (2013) is the training of MM teachers. While many of the clinical competencies required for the effective delivery of MMBIs likely overlap with general clinical skills (e.g., the ability to form a strong therapeutic alliance with clients; Wampold & Imel 2015), it has been repeatedly asserted that a depth of MM experience is vital for MM teachers (Kabat-Zinn 2011). While routes to certification exist for MBCT and MBSR (Crane et al. 2013), the associated time and financial costs will likely be infeasible for many clinicians delivering MMBIs. Thus, carefully investigating the impact of teacher variables on clinical outcomes will be critical in setting pragmatic standards for MM teachers’ background and training.
One advancement in the area of training has been the development and validation of measures of MMBI adherence and competency. In psychotherapy research, adherence has been defined as “the degree to which therapists are delivering the theory-specified techniques or methods of the intervention” and competence as “the skill with which these techniques or methods are implemented” (Webb et al. 2010, p. 201). Three measures of this kind have been developed that are specific to MMBIs, and they have varying degrees of supporting reliability and validity evidence (Chawla et al. 2010, Crane et al. 2013, Segal et al. 2002). However, the adoption of fidelity assessment remains limited (32.4% of RCTs for psychiatric disorders; Goldberg et al. 2017).
It may also be worthwhile exploring MM teachers’ behaviors and characteristics that go beyond adherence and competence, particularly given the inconsistent (or null) link between adherence and competence with treatment outcome in psychotherapy (Webb et al. 2010). MM researchers may consider exploring other psychotherapy process variables related to the MM teacher, such as the therapeutic alliance, that have been linked to outcome in MMBIs (Bowen & Kurz 2012, Goldberg et al. 2013) and in psychotherapy generally (Flückiger et al. 2018). Such explorations would be in keeping with broader efforts within the field of psychotherapy research that are aimed at leveraging therapists’ contributions to outcome (i.e., therapist effects; Baldwin & Imel 2013, Goldberg et al. 2018a).
Duration, Format, and Practice Setting
Treatment dosage, the format of training, and the practice setting are key practical considerations for implementing MMBIs. While MMBIs are derived from Buddhist contemplative traditions that have historically been practiced intensively for decades (e.g., in monastic communities), MMBIs have typically matched the MBSR course in duration and structure (i.e., 8 weeks in length; Kabat-Zinn 1990). Many consumers of MMBIs find this structure acceptable. Yet for others, this intensity of intervention is not feasible or desirable. Indeed, a recent meta-analysis of 43 studies assessing the relationship between practice time and outcome indicated that, on average, MBSR and MBCT participants complete only 64% of the recommended amount of home MM practice (i.e., 29 minutes per day; Parsons et al. 2017). The continued engagement with home MM practice postintervention is less clear (a maximum of 18.7 minutes per day for studies reviewed by Vettese et al. 2009). Additionally, no systematic study has yet been conducted to determine the optimal duration and density of practice. For example, if an individual were to practice for 20 minutes per day, is it best to complete the practice in one 20-minute period, two 10-minute periods, or five 4-minute periods? The answer to this question is likely to vary for different types of individuals. How to determine the optimal regimen for a particular individual is a critical question that requires dedicated study.
Currently, the amount of course instruction necessary to confer benefits is not clear. Clarifying this area is vital, as effective, brief MMBIs could significantly increase penetration. The potential for more intensive intervention modalities (e.g., meditation retreats) should also be explored. Preliminary meta-analytic evidence suggests that meditation retreats are associated with moderate to large effects on measures of anxiety, depression, stress, and quality of life (Khoury et al. 2017).
There are additional underexplored settings in which (or through which) MMBIs may be implemented. In particular, the increasing ubiquity and sophistication of mobile technologies offer the possibility for vastly increased reach. Several models for the mobile delivery of MMBIs have appeared in the literature, including the development of treatment-specific mobile applications and web-based delivery platforms (Davis et al. 2014, Dimidjian et al. 2014) and delivery in real time through telehealth technology (Niles et al. 2012). Initial research in this area suggests that MMBIs delivered online show small but significant effects on depression, anxiety, and well-being (Spijkerman et al. 2016). It is imperative that technologies that purport to promote mindfulness include meaningful MM training (i.e., they are not mindfulness in name only). Ideally, technology development will be paired with efficacy research (as has been done for Headspace; https://www.headspace.com/), which appears far from the current norm (Mani et al. 2015).
Access and Cultural Fit
The availability of high-quality MMBIs delivered in-person or through mobile technologies represents a central aspect of treatment access. But for access to translate into treatment engagement, health-care consumers must also find treatments culturally accessible and treatment providers culturally competent (Betancourt et al. 2003). It is difficult to determine the cultural accessibility of standard MMBIs within underrepresented populations (e.g., racial and ethnic minorities, individuals from lower socioeconomic status backgrounds) due to the limited research on this topic (Waldron et al. 2018). Nonetheless, there is reason to believe that MMBIs may be effective for underrepresented populations, with a meta-analysis combining mindfulness- and acceptance-based interventions for underrepresented groups reporting treatment effects in the moderate-to-large range (overall g = 0.69; Fuchs et al. 2013). Future research could explore cultural adaptations of traditional MMBIs, given that culture-specific modifications have been shown to improve outcomes in psychotherapy (Benish et al. 2011). While promising theoretical work has begun at this juncture (e.g., Woods-Giscombé & Black 2010), intervention development and testing are sorely needed.
CHALLENGES AND CAUTIONS
Mindfulness Hype
As popular awareness of MM has grown, articles and books in the popular press have made increasingly ambitious claims about its clinical benefits, frequently while citing support from research literature (Van Dam et al. 2018). The phenomenon of inflated expectations associated with a trendy field of research is not unique to MM, but nevertheless is cause for concern. When enthusiasm outstrips empirical support, MM interventions may be deployed prematurely in contexts in which they are untested, ineffective, or even contraindicated, as discussed in the next section. For MMBIs to be considered credible evidence-based interventions, their adoption must be paced and tied to clear standards, such as those developed by Crane et al. (2013), while claims regarding safety and efficacy must accurately reflect the extent and quality of the evidence base.
Risks, Adverse Events, and Contraindications
As the practice of MM becomes more widespread, so does the potential impact of any adverse responses. MM is widely perceived as benign, but adverse events that may have been induced by MM have been documented. Most concerning are case reports gathered by Van Dam et al. (2018) and Lindahl et al. (2017) involving the onset of psychosis, mania, or suicidal ideation. Multiple factors could contribute to such incidents—especially prior psychiatric morbidity—and the incidence of such events relative to the population rate remains unclear. The practice environment may also have a role, especially in the context of intensive retreats, during which conditions such as restricted sleep time and reduced social contact may have a destabilizing effect for some individuals. As with any clinical intervention, the possibility that MM could exacerbate psychiatric symptoms in some circumstances must be taken seriously and addressed appropriately. First, the delivery of MMBIs targeting psychiatric symptoms should be supervised by clinically trained personnel. Second, guidelines could be developed regarding MM interventions and populations that may be at increased risk or for whom the interventions may be contraindicated. Finally, formal reporting systems for adverse events are needed to improve systematic data gathering.
Responses to MM involving anxiety, panic, and trauma-related symptoms may deserve distinct consideration. Enhanced exposure to internal stimuli, both pleasant and aversive, is an intended component of MM practice (Lutz et al. 2015) and, moreover, has been proposed as a mechanism for improved affect regulation in MM (Tang et al. 2015). Even in a therapeutic context, exposure to aversive stimuli remains distressing, by definition. However, when planned and controlled, exposure is also a well-established, effective psychotherapeutic technique (McNally 2007). Thus, this aspect of MM practice may be best addressed by ensuring the quality of instructional guidance and appropriateness of dosage and setting.
Methodological and Theoretical Concerns
The increasingly high profile of MM practices has brought increased scrutiny to the rigor of research in this area. Some of the challenges facing MM are common to all psychological research. For example, concerns about replicability and publication bias (Coronado-Montoya et al. 2016) are relevant across psychological (DeCoster et al. 2015) and medical research (Begley & Ellis 2012). Nevertheless, a recent systematic review of RCTs of MM for psychiatric conditions found discouraging evidence regarding changes in methodological rigor over time (Goldberg et al. 2017). Across 142 studies, none of the six features examined (sample size, length of follow-up, use of active control comparison conditions, assessment of instructor training, assessment of treatment fidelity, use of intention-to-treat analyses) were increasing in frequency. It is vital that future studies include relevant and well-implemented active control interventions, ideally EBTs. In addition to establishing when to recommend MMBIs as frontline interventions, this practice can also address potential sources of bias, such as researcher allegiance (Munder et al. 2013) and participant expectancies.
MM research also continues to grapple with long-standing conceptual issues (Davidson & Kaszniak 2015, Van Dam et al. 2018). Diversity in the definitions and theoretical formulations of mindfulness has been widely accepted as inevitable (Van Dam et al. 2018), but it can generate confusion in empirical findings (Goldberg et al. 2015) and intervention design (Crane et al. 2017). Robust behavioral measures remain limited for key elements of MM, such as nonreactivity and dereification (Grossman & Van Dam 2011, Lutz et al. 2015). It is important to consider that the kinds of definitional and measurement challenges encountered in MM research are not unprecedented and have proven tractable in other areas of psychology, for example, in the development of rigorous research on anxiety (Davidson & Dahl 2017). In the case of MM, optimal responses include mapping components of MM training onto well-established constructs and measures; emphasizing convergent evidence from neural, physiological, behavioral, and subjective levels of analysis; and prioritizing as intervention outcomes changes in observable behavior, stable personality traits, cognitive capacities, and clinical symptomatology (Davidson & Kaszniak 2015, Van Dam et al. 2018).
CONCLUSIONS
MM can be understood as a coherent yet adaptable family of practices that targets multiple neurobehavioral systems implicated in psychopathology. The evidence base for MMBIs, while having significant limitations, shows consistent patterns. Properly designed and delivered, MMBIs perform comparably to established treatments for multiple clinical targets including depression, anxiety, pain, and substance use. Preliminary evidence also suggests effectiveness in disordered eating and PTSD, with mixed results for attention disorders, and possible applicability to serious mental illness. Importantly, MMBIs have not thus far been found to outperform established disorder-specific treatments for short-term symptom reduction. Therefore, the clinical relevance of MM practice does not appear likely to be achieved via competition with such treatments. Rather, the distinctive aspects of formal MM practice relative to other treatment approaches may prove valuable in a clinical setting. Because the development of core capacities in MM targets the transdiagnostic cognitive and affective processes underlying multiple disorders, MM may provide a means for efficiently addressing the widespread occurrence of psychiatric comorbidity. Additionally, MM can be engaged as a self-guided health-related lifestyle behavior, similar to physical exercise, for cumulative benefit and preventive effects.
The field of MM research has reached a threshold of maturation from its early exploratory stage. To meet established standards for EBTs, future research will need to address methodological shortcomings and meet the standards typical for any area of clinical development, for example, by consistently using randomized trial designs with rigorous control conditions, replicating findings, and ensuring there is follow-up with studies of effectiveness and implementation. Consideration must also be given to the potential contribution of common factors across psychotherapies, such as a supportive group and instructor contact, in cases in which MM does not evince distinct mechanisms relative to active control interventions. Finally, ongoing efforts are needed to improve the coherence, clarity, and testability of constructs and theories that relate MM to clinical constructs, such as those found in the RDoC matrix.
Assessing if, where, when, and how MM-based treatments offer comparative advantages will be a priority for implementation research. This will require increased attention to the dose and setting of practice, as well as to the medium of delivery. MM training requires tailoring for specific targets, as with MBCT for depression relapse, MBRP and MORE for substance abuse, and MBET for PTSD. Ultimately, a modular intervention design might be optimal, with core training in MM accompanied by symptom-specific components matched to an individual patient’s presentation. Meanwhile, mobile technology holds great potential for scaling-up the availability of MMBIs; developing an evidence base for smartphone-based intervention should be a high priority for maximizing impact.
Theoretical models for psychopathology and practical approaches to mental health treatment have evolved rapidly and continuously since the establishment of a scientific approach to the field. Basic questions remain open regarding the mechanisms underlying psychopathology and effective clinical practice, especially how to address the scale, range, and complexity of mental health treatment needs. At its best, research on the interventions and theory associated with MM contributes generatively to this process, enriching the tool set available to clinicians and the conceptual landscape for researchers. More broadly, the contemplative traditions from which MM is drawn, as with many others around the world, are intellectually rich and highly developed, with large reserves of material unexplored in their potential for translation into secular contexts. Thus, the scientific study of MM and psychopathology may also serve as a valuable model for adapting elements from our global inheritance of contemplative traditions into secular, empirically validated treatments for psychopathology.
SUMMARY POINTS.
Mindfulness meditation (MM) does not describe a singular technique but rather a family of practices, adapted from contemplative traditions to a secular context, which share a focus on reducing distraction and enhancing awareness of mental experience.
Diverse formulations of secular MM practice share a common emphasis on developing the core capacities of meta-awareness, present-centered awareness, nonreactivity to experience, and dereification, along with changes to self-related processing.
Converging neurobehavioral evidence suggests that the enhancement of a practitioner’s ability to exit unwanted attentional capture by past- and future-orienting thinking is an important transdiagnostic mechanism by which training in MM alleviates psychopathology.
Preliminary evidence supports multiple additional mechanisms by which MM may improve functioning in positive and negative affective systems, including increased emotion awareness, altered emotional reactivity, exposure and extinction, and facilitation of cognitive reappraisal.
Substantial evidence from randomized controlled trials indicates that properly designed and delivered mindfulness meditation–based interventions (MMBIs) can perform comparably to established treatments for symptoms of depression, anxiety, pain, and substance use.
Preliminary evidence supports potential applications to disordered eating, posttraumatic stress, and serious mental illness, while results have been mixed for attention disorders.
Because MMBIs address core processes relevant to multiple disorders, they hold particular potential for use in addressing psychiatric comorbidities.
The effective implementation of MMBIs requires addressing significant practical challenges and questions related to intervention format, training and fidelity, adverse event reporting, and cross-cultural fit.
Significant methodological issues in MM research have been identified, and while most are not unique to the field, research quality is an ongoing concern that must be addressed.
Research on MM demonstrates the wider potential for drawing on contemplative traditions to enrich the field of clinical psychology.
FUTURE ISSUES.
How can definitional controversies be settled so that studies of MM can rely on a shared set of well-defined constructs?
How can core capacities targeted by MM be more robustly operationalized through behavioral tasks?
In clinical populations, can MM enhance broad cognitive functions, such as sustained attention, or more training-specific capacities, such as meta-awareness and cognitive flexibility?
Which of the many mechanistic models best accounts for the beneficial effects of mindfulness on emotion dysregulation?
How do factors such as intensity, duration, and practice context influence the effects of MM on psychopathology?
How can MMBIs best be tailored to address comorbidity and complement existing first-line care?
What formats and settings are the most safe, effective, and efficient for delivering MMBIs?
What are the true rates and severity of adverse effects, and how can they be best addressed through screening, instruction, and intervention design?
ACKNOWLEDGMENTS
We gratefully acknowledge Melissa Rosenkranz, Daniel Grupe, David Perlman, Aaron Heller, and Cecilia Westbrook for their input and feedback on this manuscript. Support for the preparation of this article and some of the key empirical findings from the Davidson lab upon which this is based, along with stipend support for several of the authors, was provided by a grant from the National Center for Complementary and Integrative Health (P01AT004952 to RJD). S.B.G. was supported by a Francisco J. Varela Award from the Mind & Life Institute.
Glossary
- Mindfulness meditation (MM)
a family of meditation practices that shares emphasis on reducing distraction and enhancing awareness of mental experience
- RCT
randomized controlled trial
- Research Domain Criteria (RDoC)
a framework for neuroscience-driven psychopathology research based on studying transdiagnostic constructs across levels of analysis, from molecules to behavior
- Mindfulness meditation–based intervention (MMBI)
a secular clinical intervention involving a significant component of formal mindfulness meditation practice
- Mindfulness-Based Stress Reduction (MBSR)
an 8-week program involving mindfulness meditation, discussions, and home practice;MBSR underlies most contemporary clinical interventions that use formal MM
- Meta-awareness
the capacity of individuals to monitor and report on the current contents and processes of their mind
- Present-centered awareness
sustained attention to current mental content, as contrasted with retrospective or prospective thinking (i.e., mental time travel)
- Nonreactivity to experience
suspension of habitual affective reactions to the current contents of experience
- Dereification
reduction in the habitual attribution of objective reality (reification) to the contents of thought and perception
- Focused Attention (FA)
a style of meditation emphasizing sustained focus on a chosen object of meditation
- Open Monitoring (OM)
a style of meditation emphasizing present-centered awareness and the monitoring of experience, without restricting attention to a fixed focus
- Central executive network (CEN)
a network of brain regions distinguished by task-related activation and associated with goal-driven (top-down) regulation of attention
- PFC
prefrontal cortex
- Salience network
a network of brain regions associated with stimulus-driven (bottom-up) attentional orienting
- ACC
anterior cingulate cortex
- Default mode network (DMN)
a network of brain regions distinguished by task-related deactivation and linked with both spontaneous and self-referential thought
- EBT
evidence-based treatment
Footnotes
DISCLOSURES
R.J.D. is the founder and president, and serves on the board of directors, of the nonprofit organization Healthy Minds Innovations, Inc. The other authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Alberts HJ, Thewissen R, Raes L. 2012. Dealing with problematic eating behaviour: the effects of a mindfulness-based intervention on eating behaviour, food cravings, dichotomous thinking and body image concern. Appetite 58(3):847–51 [DOI] [PubMed] [Google Scholar]
- Alsubaie M, Abbott R, Dunn B, Dickens C, Keil TF, et al. 2017. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin. Psychol. Rev 55:74–91Evaluates the evidence base for mechanisms of action in mindfulness meditation–based interventions using rigorous methodological criteria.
- Baer RA. 2003. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin. Psychol. Sci. Pract 10(2):125–43 [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. 2006. Using self-report assessment methods to explore facets of mindfulness. Assessment 13(1):27–45 [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Imel ZE. 2013. Therapist effects: findings and methods. In Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change, ed. Lambert MJ, Bergin AE, pp. 258–97. New York: Wiley [Google Scholar]
- Begley CG, Ellis LM. 2012. Drug development: raise standards for preclinical cancer research. Nature 483(7391):531–33 [DOI] [PubMed] [Google Scholar]
- Benish SG, Quintana S, Wampold BE. 2011. Culturally adapted psychotherapy and the legitimacy of myth: a direct-comparison meta-analysis. J. Couns. Psychol 58(3):279–89 [DOI] [PubMed] [Google Scholar]
- Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco DM. 2015. Decentering and related constructs: a critical review and metacognitive processes model. Perspect. Psychol. Sci 10(5):599–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. 2003. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep 118(4):293–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Kurz AS. 2012. Between-session practice and therapeutic alliance as predictors of mindfulness after mindfulness-based relapse prevention. J. Clin. Psychol 68(3):236–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, et al. 2014. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry 71(5):547–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Elwafi HM, Davis JH. 2013. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol. Addict. Behav 27(2):366–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Garrison KA. 2014. The posterior cingulate cortex as a plausible mechanistic target of meditation: findings from neuroimaging. Ann. N. Y. Acad. Sci 1307(1):19–27 [DOI] [PubMed] [Google Scholar]
- Brewer JA, Worhunsky PD, Gray JR, Tang Y-Y, Weber J, Kober H. 2011. Meditation experience is associated with differences in default mode network activity and connectivity. PNAS 108(50):20254–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. 2003. The benefits of being present: mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol 84(4):822–48 [DOI] [PubMed] [Google Scholar]
- Bushnell MC, Čeko M, Low LA. 2013. Cognitive and emotional control of pain and its disruption in chronic pain. Nat. Rev. Neurosci 14(7):502–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairncross M, Miller CJ. 2016. The effectiveness of mindfulness-based therapies for ADHD: a meta-analytic review. J. Atten. Disord https://doi.org/10.1177%2F1087054715625301 [DOI] [PubMed]
- Cavanagh K, Strauss C, Forder L, Jones F. 2014. Can mindfulness and acceptance be learnt by self-help? A systematic review and meta-analysis of mindfulness and acceptance-based self-help interventions. Clin. Psychol. Rev 34(2):118–29 [DOI] [PubMed] [Google Scholar]
- Chadwick P, Strauss C, Jones A-M, Kingdon D, Ellett L, et al. 2016. Group mindfulness-based intervention for distressing voices: a pragmatic randomised controlled trial. Schizophr. Res 175(1):168–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers R, Gullone E, Allen NB. 2009. Mindful emotion regulation: an integrative review. Clin. Psychol. Rev 29(6):560–72 [DOI] [PubMed] [Google Scholar]
- Chawla N, Collins S, Bowen S, Hsu S, Grow J, et al. 2010. The Mindfulness-Based Relapse Prevention Adherence and Competence Scale: development, interrater reliability, and validity. Psychother. Res 20(4):388–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkin DC, Anderson ML, Sherman KJ, Balderson BH, Cook AJ, et al. 2017. Two-year follow-up of a randomized clinical trial of mindfulness-based stress reduction versus cognitive behavioral therapy or usual care for chronic low back pain. JAMA 317(6):642–44 [DOI] [PubMed] [Google Scholar]
- Chiesa A, Calati R, Serretti A. 2011. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clin. Psychol. Rev 31(3):449–64 [DOI] [PubMed] [Google Scholar]
- Chu C-S, Stubbs B, Chen T-Y, Tang C-H, Li D-J, et al. 2018. The effectiveness of adjunct mindfulness-based intervention in treatment of bipolar disorder: a systematic review and meta-analysis. J. Affect. Disord 225(2018):234–45 [DOI] [PubMed] [Google Scholar]
- Coronado-Montoya S, Levis AW, Kwakkenbos L, Steele RJ, Turner EH, Thombs BD. 2016. Reporting of positive results in randomized controlled trials of mindfulness-based mental health interventions. PLOS ONE 11(4):e0153220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, et al. 2017. What defines mindfulness-based programs? The warp and the weft. Psychol. Med 47(6):990–99Establishes concrete guidelines for consistency in the design and implementation of, and training for MMBIs.
- Crane RS, Eames C, Kuyken W, Hastings RP, Williams JMG, et al. 2013. Development and validation of the mindfulness-based interventions—Teaching Assessment Criteria (MBI:TAC). Assessment 20(6):681–88 [DOI] [PubMed] [Google Scholar]
- Crane RS, Kuyken W. 2013. The implementation of mindfulness-based cognitive therapy: learning from the UK health service experience. Mindfulness 4(3):246–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD. 2017. Mindfulness interventions. Annu. Rev. Psychol 68(1):491–516 [DOI] [PubMed] [Google Scholar]
- Creswell JD, Lindsay EK. 2014. How does mindfulness training affect health? A mindfulness stress buffering account. Curr. Dir. Psychol. Sci 23(6):401–7 [Google Scholar]
- Dahl CJ, Lutz A, Davidson RJ. 2015. Reconstructing and deconstructing the self: cognitive mechanisms in meditation practice. Trends Cogn. Sci 19(9):515–23Surveys broader context of contemplative practice surrounding MM and relevance to cognitive psychology.
- Davidson RJ. 2003. Alterations in brain and immune function produced by mindfulness meditation. Psychosom. Med 65(4):564–570 [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Dahl CJ. 2017. Outstanding challenges in scientific research on mindfulness and meditation. Perspect. Psychol. Sci 13(1):62–65 [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kaszniak AW. 2015. Conceptual and methodological issues in research on mindfulness and meditation. Am. Psychol 70(7):581–92In-depth discussion of theoretical challenges facing the field of MM research.
- Davidson RJ, McEwen BS. 2012. Social influences on neuroplasticity: stress and interventions to promote well-being. Nat. Neurosci 15(5):689–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Manley AR, Goldberg SB, Smith SS, Jorenby DE. 2014. Randomized trial comparing mindfulness training for smokers to a matched control. J. Subst. Abuse Treat 47(3):213–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeCoster J, Sparks EA, Sparks JC, Sparks GG, Sparks CW. 2015. Opportunistic biases: their origins, effects, and an integrated solution. Am. Psychol 70(6):499–514 [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Arch JJ, Schneider RL, Desormeau P, Felder JN, Segal ZV. 2016. Considering meta-analysis, meaning, and metaphor: a systematic review and critical examination of “third wave” cognitive and behavioral therapies. Behav. Ther 47(6):886–905 [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Beck A, Felder JN, Boggs JM, Gallop R, Segal ZV. 2014. Web-based mindfulness-based cognitive therapy for reducing residual depressive symptoms: an open trial and quasi-experimental comparison to propensity score matched controls. Behav. Res. Ther 63:83–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Segal ZV. 2015. Prospects for a clinical science of mindfulness-based intervention. Am. Psychol 70(7):593–620Outlines steps needed to fully establish MMBIs in mental health care, especially via implementation research.
- Dunne JD. 2015. Buddhist styles of mindfulness: a heuristic approach. In Handbook of Mindfulness and Self-Regulation, ed. Ostafin BD, Robinson MD, Meier BP, pp. 251–70. New York: Springer [Google Scholar]
- Farb NAS, Anderson AK, Segal ZV. 2012. The mindful brain and emotion regulation in mood disorders. Can. J. Psychiatry 57(2):70–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Daubenmier J, Price CJ, Gard T, Kerr C, et al. 2015. Interoception, contemplative practice, and health. Front. Psychol 6:763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Mayberg H, Bean J, McKeon D, et al. 2007. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc. Cogn. Affect. Neurosci 2(4):313–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flückiger C, Del Re AC, Wampold BE, Horvath AO. 2018. The alliance in adult psychotherapy: a meta-analytic synthesis. Psychotherapy In press. 10.1037/pst0000172 [DOI] [PubMed]
- Fox KCR, Dixon ML, Nijeboer S, Girn M, Floman JL, et al. 2016. Functional neuroanatomy of meditation: a review and meta-analysis of 78 functional neuroimaging investigations. Neurosci. Biobehav. Rev 65:208–28 [DOI] [PubMed] [Google Scholar]
- Fox KCR, Nijeboer S, Dixon ML, Floman JL, Ellamil M, et al. 2014. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci. Biobehav. Rev 43:48–73 [DOI] [PubMed] [Google Scholar]
- Fuchs C, Lee JK, Roemer L, Orsillo SM. 2013. Using mindfulness- and acceptance-based treatments with clients from nondominant cultural and/or marginalized backgrounds: clinical considerations, meta-analysis findings, and introduction to the special series. Cogn. Behav. Pract 20(1):1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallant SN. 2016. Mindfulness meditation practice and executive functioning: breaking down the benefit. Conscious. Cogn 40:116–30 [DOI] [PubMed] [Google Scholar]
- Garland EL, Froeliger B, Howard MO. 2014a. Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Front. Psychiatry 4:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Froeliger B, Howard MO. 2014b. Effects of mindfulness-oriented recovery enhancement on reward responsiveness and opioid cue-reactivity. Psychopharmacology 231(16):3229–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Fredrickson BL. 2011. Positive reappraisal mediates the stress-reductive effects of mindfulness: an upward spiral process. Mindfulness 2(1):59–67 [Google Scholar]
- Garland EL, Hanley AW, Baker AK, Howard MO. 2017. Biobehavioral mechanisms of mindfulness as a treatment for chronic stress: an RDoC perspective. Chronic Stress 1:2470547017711912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Howard MO. 2018. Mindfulness-based treatment of addiction: current state of the field and envisioning the next wave of research. Addict. Sci. Clin. Pract 13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Thomas E, Howard MO. 2014c. Mindfulness-oriented recovery enhancement ameliorates the impact of pain on self-reported psychological and physical function among opioid-using chronic pain patients. J. Pain Symptom Manag 48(6):1091–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gethin R 2015. Buddhist conceptualizations of mindfulness. In Handbook of Mindfulness: Theory, Research, and Practice, ed. Brown KW, Creswell JD, Ryan RM, pp. 9–41. New York: Guilford Press [Google Scholar]
- Goldberg SB, Davis JM, Hoyt WT. 2013. The role of therapeutic alliance in mindfulness interventions: therapeutic alliance in mindfulness training for smokers. J. Clin. Psychol 69(9):936–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Hoyt WT, Nissen-Lie HA, Nielsen SL, Wampold BE. 2018a. Unpacking the therapist effect: impact of treatment length differs for high- and low-performing therapists. Psychother. Res 28(4):532–44 [DOI] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Kearney DJ, Simpson TL. 2019. Mindfulness-based cognitive therapy for patients with current depression: A meta-analysis. Cognitive Behaviour Therapy, in press 10.1080/16506073.2018.1556330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, et al. 2018b. Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clin. Psychol. Rev 59:52–60Quantifies effectiveness of mindfulness meditation–based interventions on disorder-specific symptoms across psychiatric conditions.
- Goldberg SB, Tucker RP, Greene PA, Simpson TL, Kearney DJ, Davidson RJ. 2017. Is mindfulness research methodology improving over time? A systematic review. PLOS ONE 12(10):e0187298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Wielgosz J, Dahl C, Schuyler B, MacCoon DS, et al. 2015. Does the Five Facet Mindfulness Questionnaire measure what we think it does? Construct validity evidence from an active controlled randomized clinical trial. Psychol. Assess 28(8):1009–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. 2016. Group CBT versus MBSR for social anxiety disorder: a randomized controlled trial. J. Consult. Clin. Psychol 84(5):427–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ziv M, Jazaieri H, Gross JJ. 2012. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Front. Hum. Neurosci 6:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotink RA, Meijboom R, Vernooij MW, Smits M, Hunink MGM. 2016. 8-week mindfulness based stress reduction induces brain changes similar to traditional long-term meditation practice—a systematic review. Brain Cogn 108:32–41 [DOI] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, et al. 2014. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern. Med 174(3):357–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg J, Shapero BG, Mischoulon D, Lazar SW. 2017. Mindfulness-based cognitive therapy for depressed individuals improves suppression of irrelevant mental-sets. Eur. Arch. Psychiatry Clin. Neurosci 267(3):277–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P 2008. On measuring mindfulness in psychosomatic and psychological research. J. Psychosom. Res 64(4):405–8 [DOI] [PubMed] [Google Scholar]
- Grossman P, Van Dam NT. 2011. Mindfulness, by any other name…: trials and tribulations of sati in western psychology and science. Contemp. Buddhism 12(1):219–39 [Google Scholar]
- Gu J, Strauss C, Bond R, Cavanagh K. 2015. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev 37:1–12 [DOI] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih M-Y, Atwood AK, Johnson RA, et al. 2014. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry 71(5):566–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haase L, Thom NJ, Shukla A, Davenport PW, Simmons AN, et al. 2016. Mindfulness-based training attenuates insula response to an aversive interoceptive challenge. Soc. Cogn. Affect. Neurosci 11(1):182–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington A, Dunne JD. 2015. When mindfulness is therapy: ethical qualms, historical perspectives. Am. Psychol 70(7):621–31Reviews historical developments that led to the integration of mindfulness practices into mental health treatment.
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. 2006. Acceptance and Commitment Therapy: model, processes and outcomes. Behav. Res. Ther 44(1):1–25 [DOI] [PubMed] [Google Scholar]
- Hedman-Lagerlöf M, Hedman-Lagerlöf E, Öst L-G. 2018. The empirical support for mindfulness-based interventions for common psychiatric disorders: a systematic review and meta-analysis. Psychol. Med 48(13):2116–29 [DOI] [PubMed] [Google Scholar]
- Hepark S, Janssen L, de Vries A, Schoenberg PLA, Donders R, et al. 2015. The efficacy of adapted MBCT on core symptoms and executive functioning in adults with ADHD: a preliminary randomized controlled trial. J. Atten. Disord 10.1177/1087054715613587 [DOI] [PubMed]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, et al. 2017. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann. Behav. Med 51(2):199–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Grossman P, Hinton DE. 2011. Loving-kindness and compassion meditation: potential for psychological interventions. Clin. Psychol. Rev 31(7):1126–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Goetter E, Robinaugh DJ, Ojserkis RA, et al. 2015. Change in decentering mediates improvement in anxiety in Mindfulness-Based Stress Reduction for generalized anxiety disorder. Cogn. Ther. Res 39(2):228–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, et al. 2013. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J. Clin. Psychiatry 74(8):786–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Hoge EA, Greve DN, Gard T, Creswell JD, et al. 2013. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. NeuroImage Clin 2:448–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. 2011. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect. Psychol. Sci 6(6):537–59 [DOI] [PubMed] [Google Scholar]
- Hopwood TL, Schutte NS. 2017. A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clin. Psychol. Rev 57:12–20 [DOI] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, Simpson TL. 2013. Meta-analysis of dropout in treatments for posttraumatic stress disorder. J. Consult. Clin. Psychol 81(3):394–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel TR, Cuthbert B, Garvey M, Heinssen R, Pine DS, et al. 2010. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. Am. J. Psychiatry 167(7):748–51 [DOI] [PubMed] [Google Scholar]
- Jha AP, Morrison AB, Dainer-Best J, Parker S, Rostrup N, Stanley EA. 2015. Minds “at attention”: mindfulness training curbs attentional lapses in military cohorts. PLOS ONE 10(2):e0116889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AP, Stanley EA, Kiyonaga A, Wong L, Gelfand L. 2010. Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion 10(1):54–64 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J 1990. Full Catastrophe Living New York: Delacorte Press [Google Scholar]
- Kabat-Zinn J 2011. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemp. Buddhism 12(1):281–306 [Google Scholar]
- Kabat-Zinn J, Lipworth L, Burney R. 1985. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J. Behav. Med 8(2):163–90 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, et al. 1992. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am. J. Psychiatry 149(7):936–43 [DOI] [PubMed] [Google Scholar]
- Khalsa SS, Rudrauf D, Damasio AR, Davidson RJ, Lutz A, Tranel D. 2008. Interoceptive awareness in experienced meditators. Psychophysiology 45(4):671–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B, Knäuper B, Schlosser M, Carrière K, Chiesa A. 2017. Effectiveness of traditional meditation retreats: a systematic review and meta-analysis. J. Psychosom. Res 92:16–25 [DOI] [PubMed] [Google Scholar]
- King AP, Block SR, Sripada RK, Rauch SAM, Giardino N, et al. 2016a. Altered default mode network (DMN) resting state functional connectivity following a mindfulness-based exposure therapy for posttraumatic stress disorder (PTSD) in combat veterans of Afghanistan and Iraq. Depress. Anxiety 33(4):289–99 [DOI] [PubMed] [Google Scholar]
- King AP, Block SR, Sripada RK, Rauch SAM, Porter KE, et al. 2016b. A pilot study of mindfulness-based exposure therapy in OEF/OIF combat veterans with PTSD: altered medial frontal cortex and amygdala responses in social–emotional processing. Front. Psychiatry 7:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AP, Favorite TK. 2016. Mindfulness-Based Cognitive Therapy for combat-related posttraumatic stress disorder. In Mindfulness-Based Cognitive Therapy: Innovative Applications, ed. Eisendrath SJ, pp. 163–91. Cham, Switz: Springer [Google Scholar]
- Kirby JN. 2017. Compassion interventions: the programmes, the evidence, and implications for research and practice. Psychol. Psychother 90(3):432–55 [DOI] [PubMed] [Google Scholar]
- Kirk U, Brown KW, Downar J. 2015. Adaptive neural reward processing during anticipation and receipt of monetary rewards in mindfulness meditators. Soc. Cogn. Affect. Neurosci 10(5):752–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kober H, Brewer JA, Height KL, Sinha R. 2017. Neural stress reactivity relates to smoking outcomes and differentiates between mindfulness and cognitive–behavioral treatments. NeuroImage 151:4–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocovski NL, Fleming JE, Hawley LL, Huta V, Antony MM. 2013. Mindfulness and acceptance-based group therapy versus traditional cognitive behavioral group therapy for social anxiety disorder: a randomized controlled trial. Behav. Res. Ther 51(12):889–98 [DOI] [PubMed] [Google Scholar]
- Koob GF, Volkow ND. 2016. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry 3(8):760–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral TRA, Schuyler BS, Mumford JA, Rosenkranz MA, Lutz A, Davidson RJ. 2018. Impact of short- and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. NeuroImage 181:301–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristeller JL, Wolever RQ. 2010. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eat. Disord 19(1):49–61 [DOI] [PubMed] [Google Scholar]
- Kristeller JL, Wolever RQ, Sheets V. 2014. Mindfulness-based eating awareness training (MB-EAT) for binge eating: a randomized clinical trial. Mindfulness 5(3):282–97 [Google Scholar]
- Kross E, Gard D, Deldin P, Clifton J, Ayduk O. 2012. “Asking why” from a distance: its cognitive and emotional consequences for people with major depressive disorder. J. Abnorm. Psychol 121(3):559–69 [DOI] [PubMed] [Google Scholar]
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, et al. 2015. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet 386(9988):63–73 [DOI] [PubMed] [Google Scholar]
- Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, et al. 2016. Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry 73(6):565–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lao S-A, Kissane D, Meadows G. 2016. Cognitive effects of MBSR/MBCT: a systematic review of neuropsychological outcomes. Conscious. Cogn 45:109–23Reviews effects of mindfulness meditation training on core cognitive functions.
- Lau MA, Bishop SR, Segal ZV, Buis T, Anderson ND, et al. 2006. The Toronto Mindfulness Scale: development and validation. J. Clin. Psychol 62(12):1445–67 [DOI] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, Lazar M. 2017. Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J. Subst. Abuse Treat 75:62–96 [DOI] [PubMed] [Google Scholar]
- Lin Y, Callahan CP, Moser JS. 2018. A mind full of self: self-referential processing as a mechanism underlying the therapeutic effects of mindfulness training on internalizing disorders. Neurosci. Biobehav. Rev 92:172–86 [DOI] [PubMed] [Google Scholar]
- Lindahl JR, Fisher NE, Cooper DJ, Rosen RK, Britton WB. 2017. The varieties of contemplative experience: a mixed-methods study of meditation-related challenges in Western Buddhists. PLOS ONE 12(5):e0176239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. 1993. Cognitive–Behavioral Treatment of Borderline Personality Disorder New York: Guilford Press [Google Scholar]
- Lutz A, Brefczynski-Lewis J, Johnstone T, Davidson RJ. 2008a. Regulation of the neural circuitry of emotion by compassion meditation: effects of meditative expertise. PLOS ONE 3(3):e1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Dunne JD, Davidson RJ. 2007. Meditation and the neuroscience of consciousness: an introduction. In The Cambridge Handbook of Consciousness, ed. Zelazo PD, Moscovitch M, Thompson E, pp. 499–551. New York: Cambridge Univ. Press [Google Scholar]
- Lutz A, Jha AP, Dunne JD, Saron CD. 2015. Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. Am. Psychol 70(7):632–58Characterizes capacities targeted by MM, their neurobiological basis, and their relation to contemplative sources.
- Lutz A, McFarlin DR, Perlman DM, Salomons TV, Davidson RJ. 2013. Altered anterior insula activation during anticipation and experience of painful stimuli in expert meditators. NeuroImage 64:538–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. 2008b. Attention regulation and monitoring in meditation. Trends Cogn. Sci 12(4):163–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR, Trost WT, Salsman N, Linehan MM. 2007. Dialectical behavior therapy for borderline personality disorder. Annu. Rev. Clin. Psychol 3:181–205 [DOI] [PubMed] [Google Scholar]
- Mani M, Kavanagh DJ, Hides L, Stoyanov SR. 2015. Review and evaluation of mindfulness-based iPhone apps. JMIR MHealth UHealth 3(3):e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason AE, Epel ES, Aschbacher K, Lustig RH, Acree M, et al. 2016. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: data from the SHINE randomized controlled trial. Appetite 100:86–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. 2007. Mechanisms of exposure therapy: how neuroscience can improve psychological treatments for anxiety disorders. Clin. Psychol. Rev 27(6):750–59 [DOI] [PubMed] [Google Scholar]
- Miloyan B, Pachana NA, Suddendorf T. 2014. The future is here: a review of foresight systems in anxiety and depression. Cogn. Emot 28(5):795–810 [DOI] [PubMed] [Google Scholar]
- Mitchell JT, McIntyre EM, English JS, Dennis MF, Beckham JC, Kollins SH. 2017. A pilot trial of mindfulness meditation training for ADHD in adulthood: impact on core symptoms, executive functioning, and emotion dysregulation. J. Atten. Disord 21(13):1105–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrazek MD, Mooneyham BW, Schooler JW. 2014. Insights from quiet minds: the converging fields of mindfulness and mind-wandering. In Meditation—Neuroscientific Approaches and Philosophical Implications, Vol. 2, ed. Schmidt S, Walach H, pp. 227–41. Cham, Switz.: Springer [Google Scholar]
- Munder T, Brütsch O, Leonhart R, Gerger H, Barth J. 2013. Researcher allegiance in psychotherapy outcome research: an overview of reviews. Clin. Psychol. Rev 33(4):501–11 [DOI] [PubMed] [Google Scholar]
- Murray G, Leitan ND, Thomas N, Michalak EE, Johnson SL, et al. 2017. Towards recovery-oriented psychosocial interventions for bipolar disorder: quality of life outcomes, stage-sensitive treatments, and mindfulness mechanisms. Clin. Psychol. Rev 52:148–63 [DOI] [PubMed] [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, et al. 2018. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann. Behav. Med 52(6):446–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE (Natl. Institute Health Care Excell.). 2018. Depression in adults: recognition and management NICE; https://www.nice.org.uk/guidance/cg90 [PubMed] [Google Scholar]
- Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. 2012. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol. Trauma 4:538–47 [Google Scholar]
- Parsons CE, Crane C, Parsons LJ, Fjorback LO, Kuyken W. 2017. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav. Res. Ther 95:29–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman DM, Salomons TV, Davidson RJ, Lutz A. 2010. Differential effects on pain intensity and unpleasantness of two meditation practices. Emotion 10(1):65–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelps EA, Delgado MR, Nearing KI, LeDoux JE. 2004. Extinction learning in humans: role of the amygdala and vmPFC. Neuron 43(6):897–905 [DOI] [PubMed] [Google Scholar]
- Quaglia JT, Brown KW, Lindsay EK, Creswell JD, Goodman RJ. 2015. From conceptualization to operationalization of mindfulness. Handbook of Mindfulness: Theory, Research, and Practice, ed. Brown KW, Creswell JD, Ryan RM, pp. 151–170. New York: Guilford Press [Google Scholar]
- Rogers JM, Ferrari M, Mosely K, Lang CP, Brennan L. 2017. Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes. Obes. Rev 18(1):51–67 [DOI] [PubMed] [Google Scholar]
- Rosenkranz MA, Davidson RJ, MacCoon DG, Sheridan JF, Kalin NH, Lutz A. 2013. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain. Behav. Immun 27:174–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, et al. 2017. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: a systematic review and meta-analysis. Obes. Res. Clin. Pract 11(5):90–111 [DOI] [PubMed] [Google Scholar]
- Santorelli SF, ed. 2014. Mindfulness-Based Stress Reduction (MBSR): Standards of Practice Worcester, MA: Ctr. Mindfulness Med. Health Care Soc. [Google Scholar]
- Santorelli SF, Meleo-Meyer F, Koerbel L, Kabat-Zinn J. 2017. Mindfulness-Based Stress Reduction (MBSR) Authorized Curriculum Guide Worcester, MA: Ctr. Mindfulness Med. Health Care Soc. [Google Scholar]
- Schooler JW, Smallwood J, Christoff K, Handy TC, Reichle ED, Sayette MA. 2011. Meta-awareness, perceptual decoupling and the wandering mind. Trends Cogn. Sci 15(7):319–26 [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. 2002. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse New York: Guilford Press [Google Scholar]
- Spijkerman MPJ, Pots WTM, Bohlmeijer ET. 2016. Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin. Psychol. Rev 45:102–14 [DOI] [PubMed] [Google Scholar]
- Suddendorf T, Corballis MC. 2007. The evolution of foresight: What is mental time travel, and is it unique to humans? Behav. Brain Sci 30(3):299–313 [DOI] [PubMed] [Google Scholar]
- Tang Y-Y, Hölzel BK, Posner MI. 2015. The neuroscience of mindfulness meditation. Nat. Rev. Neurosci 16(4):213–25Detailed review of neuroimaging and other neurobiological findings associated with mindfulness meditation.
- Tang Y-Y, Tang R, Posner MI. 2016. Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug Alcohol Depend 163(Suppl. 1):S13–18 [DOI] [PubMed] [Google Scholar]
- Tapper K 2018. Mindfulness and craving: effects and mechanisms. Clin. Psychol. Rev 59:101–17 [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Chaskalson M. 2011a. How does mindfulness transform suffering? I: The nature and origins of dukkha. Contemp. Buddhism 12(1):89–102 [Google Scholar]
- Teasdale JD, Chaskalson M. 2011b. How does mindfulness transform suffering? II: The transformation of dukkha. Contemp. Buddhism 12(1):103–24 [Google Scholar]
- Bhikkhu Thanissaro. 1997. Sallatha sutta: the arrow. Access to Insight https://www.accesstoinsight.org/tipitaka/sn/sn36/sn36.006.than.html
- Tovote KA, Fleer J, Snippe E, Peeters AC, Emmelkamp PM, et al. 2014. Individual Mindfulness-Based Cognitive Therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: results of a randomized controlled trial. Diabetes Care 37(9):2427–34 [DOI] [PubMed] [Google Scholar]
- Vago DR, Silbersweig DA. 2012. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci 6:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, et al. 2018. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect. Psychol. Sci 13:36–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, et al. 2015. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin. Psychol. Rev 37:26–39 [DOI] [PubMed] [Google Scholar]
- Vettese LC, Toneatto T, Stea JN, Nguyen L, Wang JJ. 2009. Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. J. Cogn. Psychother 23(3):198–225 [Google Scholar]
- Waldron EM, Hong S, Moskowitz JT, Burnett-Zeigler I. 2018. A systematic review of the demographic characteristics of participants in US-based randomized controlled trials of mindfulness-based interventions. Mindfulness 2018:1–22 [Google Scholar]
- Wampold BE, Imel ZE. 2015. The Great Psychotherapy Debate: The Evidence for What Makes Psychotherapy Work New York: Routledge [Google Scholar]
- Wang L-Q, Chien WT, Yip LK, Karatzias T. 2016. A randomized controlled trial of a mindfulness-based intervention program for people with schizophrenia: 6-month follow-up. Neuropsychiatr. Dis. Treat 12:3097–3110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins ER. 2008. Constructive and unconstructive repetitive thought. Psychol. Bull 134(2):163–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Barber JP. 2010. Therapist adherence/competence and treatment outcome: a meta-analytic review. J. Consult. Clin. Psychol 78(2):200–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, Tindle HA. 2013. Mindful attention reduces neural and self-reported cue-induced craving in smokers. Soc. Cogn. Affect. Neurosci 8(1):73–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Teasdale JD, Segal ZV, Soulsby J. 2000. Mindfulness-based cognitive therapy reduces overgeneral autobiographical memory in formerly depressed patients. J. Abnorm. Psychol 109(1):150–55 [DOI] [PubMed] [Google Scholar]
- Woods-Giscombé CL, Black AR. 2010. Mind–body interventions to reduce risk for health disparities related to stress and strength among African American women: the potential of mindfulness-based stress reduction, loving-kindness, and the NTU therapeutic framework. Complement. Health Pract. Rev 15(3):115–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yulish NE, Goldberg SB, Frost ND, Abbas M, Oleen-Junk NA, et al. 2017. The importance of problem-focused treatments: a meta-analysis of anxiety treatments. Psychotherapy 54(4):321–38 [DOI] [PubMed] [Google Scholar]
- Zeidan F, Adler-Neal AL, Wells RE, Stagnaro E, May LM, et al. 2016. Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. J. Neurosci 36(11):3391–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, et al. 2015. Mindfulness meditation–based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation–induced analgesia. J. Neurosci 35(46):15307–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Martucci KT, Kraft RA, McHaffie JG, Coghill RC. 2014. Neural correlates of mindfulness meditation–related anxiety relief. Soc. Cogn. Affect. Neurosci 9(6):751–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F, Vago DR. 2016. Mindfulness meditation–based pain relief: a mechanistic account. Ann. N. Y. Acad. Sci 1373(1):114–27 [DOI] [PMC free article] [PubMed] [Google Scholar]


