Abstract
Early institutional rearing is associated with increased risk for subsequent peer relationship difficulties, but the underlying mechanisms have not been identified. Friendship characteristics, social behaviors with peers, normed assessments of social problems, and social cue use were assessed in 142 children (mean age=10.06, SD=2.02; range 7–13 years), of whom 67 were previously institutionalized (PI) and 75 were raised by their biological families. Anxiety and attention-deficit/hyperactivity disorder (ADHD) symptoms, often elevated among PI children, were examined as potential mediators of PI status and baseline social functioning and longitudinal follow-ups (two, four years later). Twenty-seven percent of PI children fell above the CBCL Social Problems cutoff. Examination of specific social behaviors with peers indicated that PI and comparison children did not differ in empathic concern or peer social approach, though parents were more likely to endorse aggression/overarousal as a reason PI children might struggle with friendships. Comparison children outperformed PI children in computerized testing of social cue use learning. Finally, across these measures, social difficulties exhibited in the PI group were mediated by ADHD symptoms with predicted social problems assessed four years later. These findings show that when PI children struggle with friendships, mechanisms involving attention and behavior regulation are likely contributors.
Keywords: institutional rearing, institutional care, social problems, ADHD
The development of social skills and the formation of meaningful relationships with peers depend, in part, on socialization behaviors learned with primary caregivers (Laible & Thompson, 2007). A child’s primary caregiver comprises the first and the most influential social context in early life, and the quality of early child-caregiver interactions has been linked to children’s social behavior (Feldman & Klein, 2003). Sensitive responding by a caregiver is postulated to imbue children with self-efficacy as a social partner (Bornstein, Hendricks, Haynes, & Painter, 2007), and quality of caregiving is linked to children’s behavior with peers, including antisocial and aggressive behavior (Shaw, Bell, & Gilliom, 2000). Institutional care (i.e., orphanage rearing) is an extreme form of psychosocial deprivation, in which caregiving experiences are species atypical (McLaughlin, Sheridan, & Nelson, 2017; Tottenham, 2012). Rotating staff, high child-to-caregiver ratios, and regimented care, do not permit children’s individual needs to be met beyond instrumental care (Smyke et al., 2007). Though the quality of institutions vary (Zeanah, Smyke, & Settles, 2006), exposure to institutional care is associated with negative cognitive, emotional, and social outcomes (van IJzendoorn et al., 2011). Approximately 8 million children reside in institutional care (Csâky, 2009), and current evidence promotes family-based placements early in life to mitigate the long-term impact of psychosocial deprivation (Zeanah, Humphreys, Fox, & Nelson, 2017). Following placements into families, although behavior in many domains exhibit rebound, risk in the socio-emotional domain can remain elevated (Tottenham, 2012).
Early institutional care exposure has been linked to poorer social functioning, including behavioral inhibition in social contexts, reduced social support, more “quarrelsome” and bullying behavior, and reduced prosocial behavior (Almas et al., 2012, 2015; Hodges & Tizard, 1989; Humphreys et al., 2018; Sonuga-Barke, Schlotz, & Kreppner, 2010), though may vary by age and sex (Julian & McCall, 2016). In addition to specific social difficulties, several studies have linked institutional care history to higher total problems on standardized measures of social functioning (i.e., the CBCL Social Problems narrow-band subscale [Groza, Ryan, & Cash, 2003; Hawk & McCall, 2010; Kim, Shin, & Carey, 1999; Merz & McCall, 2010]).
Other forms of psychopathology that are known to be associated with the absence of adequate caregiving, specifically reactive attachment disorder (RAD) and disinhibited social engagement disorder (DSED) (American Psychiatric Association, 2013), have been examined as potential correlates or predictors of social functioning in children with institutional care exposure (Guyon-Harris, Humphreys, Fox, Nelson, & Zeanah, 2018b; Sonuga-Barke et al., 2010). However, symptoms of these disorders are relatively rare in later childhood and early adolescence (Gleason et al., 2011; Guyon-Harris et al., in press; Guyon-Harris, Humphreys, Fox, Nelson, & Zeanah, 2018a). Other forms of psychopathology (e.g., anxiety and attention-deficit/hyperactivity disorder [ADHD]) found at higher rates among previously institutionalized (PI) children (Ellis, Fisher, & Zaharie, 2004; Humphreys, Gleason, et al., 2015; Kreppner, O’Connor, & Rutter, 2001; Tottenham et al., 2010; Wiik et al., 2011), may also be important in considering potential pathways from early institutional care exposure and social functioning difficulties.
Drawing from the larger clinical and developmental literatures, social difficulties have been associated with both anxiety (e.g., Erath, Flanagan, & Bierman, 2007; Strauss, Lease, Kazdin, Dulcan, & Last, 1989) and ADHD symptoms (e.g., Bagwell, Molina, Pelham, & Hoza, 2001; de Boo & Prins, 2007; Humphreys, Galán, Tottenham, & Lee, 2016). However, the types of social functioning deficits differ based on domain of psychopathology; anxious children are more shy and withdrawn (Strauss et al., 1989), whereas children with ADHD are more likely to engage in inappropriate social behavior, such as excessive intrusiveness and aggression (Merrell & Boelter, 2001) and exhibit difficulty learning from social cues (Humphreys et al., 2016). As noted above, both anxiety and ADHD are common phenotypes in PI children (Ellis et al., 2004; Humphreys, Gleason, et al., 2015; Kreppner et al., 2001; Tottenham et al., 2010; Wiik et al., 2011). Thus, both anxiety and ADHD symptoms are potential candidates for linking early experiences of early institutional rearing and later social functioning. Furthermore, given that the types of social behavior problems may differ based on each form of psychopathology, potential mechanistic models are warranted that include both candidate domains as predictors in a framework facilitating the distillation of peer-directed behavior into its varied forms.
The goal of the present study was to examine social behaviors with peers among children with and without a history of institutional rearing. In order to do this, we created a measure of friendship behaviors, as well as administered a well-validated standardized measure of broad-based social problems (Child Behavior Checklist [CBCL] Social Problems narrow-band scale; Achenbach & Rescorla, 2001) and a computerized laboratory assessment of social cue use. In order to explore the variation in PI children, and to determine whether specific forms of psychopathology (i.e., anxiety and ADHD symptoms) may explain risk for social difficulties in this population, we included both forms of psychopathology in multiple mediation analyses of the association between PI status and social functioning. Longitudinal data from this sample allowed us to examine these associations cross-sectionally and longitudinally at follow-up assessments occurring approximately two and four years after the baseline assessment.
Methods
Participants
At Wave 1, a total of 142 individuals (67 PI and 75 healthy comparison, never-institutionalized), aged 7–13 years old (M=10.06, SD=2.02; 80 girls and 62 boys) residing in the United States were included in the present study. The parent study (NIMH R01MH091864) included a wider age range, and for the present study only 7–13 year olds were included in order to reduce the heterogeneity in friendship behaviors. While social behaviors with peers are likely to change across the school-age period, we excluded high school age participants given that the specific social behaviors in this period may not be comparable to social behaviors in elementary and middle school age children. For both the PI and comparison children, families were recruited via formal interest organizations, adoption agencies, flyer advertisements within the surrounding community, friend referral, or from state birth records. PI children were adopted into families in the United States, while comparison children were selected to not differ from the PI group in terms of age. This volunteer, community sample of children were required to reside with their biological families, and were included if they were psychiatrically healthy (i.e., non-clinical), which was confirmed via parent report. However, no formal diagnostic assessment or definition of what did or did not constitute this label was provided. See Table 1 for more information about the sample. A subset of the sample provided CBCL data at Wave 2 (n=66; M age=12.31, SD=2.17) and Wave 3 (n=48; Mage=13.71, SD=2.26). All data were from Wave 1 unless otherwise specified. The protocol was approved by the university Institutional Review Board. Participants parents provided informed consent and children provided assent.
Table 1.
Participant demographics
| PIa (n=67) | Comparison (n=75) | |
|---|---|---|
| Age (in years) | 10.17 (1.98) | 9.97 (2.06) |
| Range: 7.27–13.98 | Range: 7.02–13.85 | |
| Sex (% girls) | 66% | 47% |
| Country of Origin | Azerbaijan (2) Belarus (1) China (20) Guatemala (3) Indian (1) Kazakhstan (10) Romania (1) Russia (18) Slovak Republic (1) South Korea (2) Ukraine (4) Vietnam (1) Missing (3) |
|
| Age placed in institution (months) | 7.45 (14.20) Median: 1.00 Range: 0.00–72.00 |
— |
| Age adopted (months) | 28.49 (27.07) Median: 15.50 Range: 0.13–120.00 |
— |
| Months in institutional care | 21.23 (18.19) Median: 13.64 Range: 0.13–90.00 |
— |
Note. Means (SD). PI=previously institutionalized.
Adoption details available for subsample (N=63).
Procedure
Children attended a 2- to 3-hour laboratory session with their parent in the Psychology Department, in which the parent completed questionnaires and the child completed a number of activities, including computerized assessments of the social cue use task (described below). Participants were invited to return to the laboratory for Wave 2 (mean years following baseline=2.15, SD=0.55) and Wave 3 (mean years following baseline=3.51, SD=0.87).
Measures
Institutional Care History.
Parents of PI children were asked to provide their best estimates (if not known) regarding their child’s institutional care history, including at age placement into institutional care and age at adoption (typically believed to be more accurate than age of placement information; Merz & McCall, 2010). Ninety six percent (n=64) of PI children’s parents provided this information.
Friendship Questionnaire (FQ).
The FQ was developed by NT and was designed to capture parent report of child friendships and social behavior. This measure obtains details on friendships and social behaviors with peers not assessed on the CBCL Social Problems subscale, including specific types of behaviors that occur in the context of peer interactions, as well as information about the child’s best friend and peer group. In order to obtain scales representing child behavior in social situations, we conducted a principal components analysis (PCA) on items assessing behavior (items 5–9; see the Appendix). These items were selected because they assess the child’s overt peer-directed behavior. All items with sufficient variability (i.e., at least 5 individuals provided a nondominant response) were standardized (i.e., Z-scored) and entered into a PCA in SPSS specifying orthogonal (varimax with Kaiser Normalization) rotation within the full sample. Factors with an eigenvalue over 1 were extracted and factor scales from the analysis were saved, per similar approaches in related research (e.g., Delis, Freeland, Kramer, & Kaplan, 1988). Cross-loading of variations to different factors was allowed. Three scales were obtained, and the authors named each factor based on a review of items with factor loadings with an absolute value of .4: social approach, aggression/overarousal, and empathic concern.
Child Behavior Checklist 6–18 (CBCL; Achenbach & Rescorla, 2001).
The 113-item rating scale was completed by the parent and provided measures of child psychopathology. Responses were scored on a 3-point scale, from 0 for “not true” to 2 for “very true or often true.” The CBCL was normed on a large sample of children ages 6–18 years and possesses excellent test-retest and interrater reliability, as well as adequate to excellent internal consistency (Achenbach & Rescorla, 2001). The total score from the attention problems narrow-band subscale at Wave 1 was used as our measure of ADHD symptoms. Items assessing inattention, hyperactivity, and impulsivity are included in this scale, though these items do not map on perfectly to the symptoms of ADHD in DSM-5 (American Psychiatric Association, 2013). The CBCL Social Problems narrow-band scale was used at Waves 1, 2, and 3 to assess social problems, and includes items assessing behavior (e.g., dependence on parents) but also mood states (e.g., loneliness; jealousy) and how others treat the child (e.g., whether the child is teased). In addition, in order to identify social problems that meet the threshold for clinical concern, a cutoff based on a T score of 65 or greater was used to create a binary split (i.e., those below vs. at/above the clinical cutoff).
Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al., 1997).
This 41-item rating scale was completed by the parent in order to assess child anxiety symptoms. Items are rated on a 3-point scale, with higher scores signifying more anxiety. This measure has been shown to have good internal consistency (α=.74 to .93) (Birmaher et al., 1997). For the purpose of the present study we used the total score from the SCARED as a global measure of child anxiety.
Computerized Social Cue Use Task.
A social cue use task (previously referred to as a social decision-making task) was developed (Humphreys et al., 2016) using faces from the NimStim set of facial expressions (Tottenham et al., 2009), and was added to the study protocol after the start of initial data collection and thus was only available in a subset of participants (n=105; 65 comparison and 40 PI). The images were taken from a morphing face task in which separate images of one of three individuals’ faces morphed from ‘happy’ to ‘angry’ (Kirsh & Mounts, 2007; Li & Tottenham, 2013). There were a total of 27 trials composed of a series of facial images that became increasingly angry. See Figure 1A for visual representation of the task. The task was embedded in a Halloween “trick or treat” candy acquisition game. Participants were told to press a button to “knock” on doors and earn “candy” (represented as points) for every knock they executed (i.e., more knocks earned more candy). At the beginning of each trial a face appeared on the screen and with each press the face changed toward a fixed angry expression point (Li & Tottenham, 2013), such that facial expressions grew increasingly angry with each successive knock. At a given angry expression point, an additional knock would result in the door slamming and the loss of the candy earned from that trial.
Figure 1.
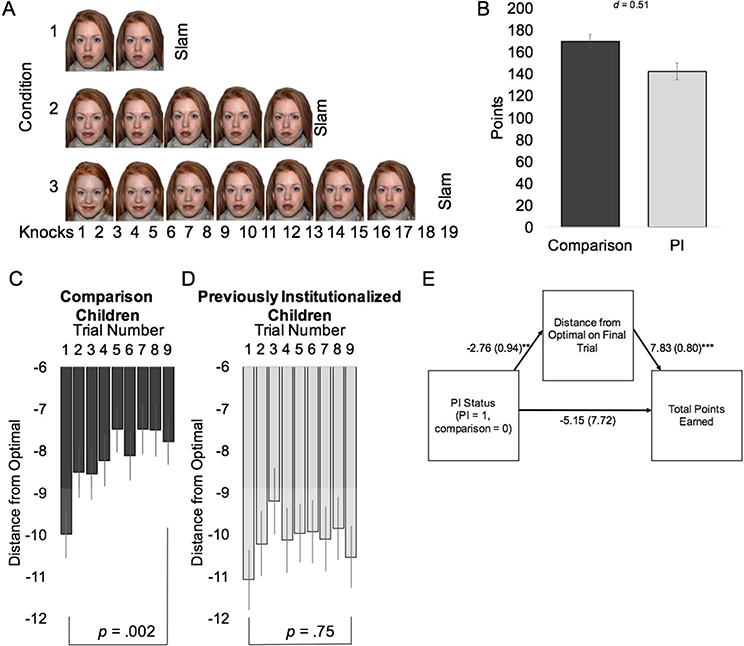
(A) Illustration of the social cue use task. Condition 1=quick condition (trial ends at 7 knocks). Condition 2=intermediate condition (trial ends at 13 knocks). Condition 3=slow condition (trial ends at 19 knocks). (B) Mean points earned on the task by institutional care history. (C) Distance from optimal behavior on the social cue use task on the slow-to-anger condition among comparison children and (D) previously institutionalized children, (E) mediation model with distance from optimal performance on the final trial for the slow-to-anger condition mediating the association between caregiving group and total points earned, coefficient (standard error). Note. PI=previously institutionalized. Error bars=1 standard error. **p<.001. ***p<001.
Trials were presented in three conditions: (1) “slow-to-anger condition” allowed for 19 knocks before door slamming, (2) “intermediate condition” allowed for 13 knocks, and (3) “quick-to-anger condition” allowed for 7 knocks. Trial progression and face identity were randomized within task third (i.e., all presentations occurred within each third of the task in a random order). Each knock results in one point, with the exception of knocks on trials that end with a door slam, in which no points are awarded. The primary outcome of the social cue use task was points, which could be examined as a total score across the task and by examining scores within each of the three task conditions (i.e., quick-to-anger, intermediate, and slow-to-anger), with higher points earned indicating greater ability to use social cues to guide behavior. Lower scores may indicate either stopping knocking prior to the optimal end point or knocking past the final angry face. Previous work using this task indicated a negative association between points earned on this task and CBCL Social Problems (Humphreys et al., 2016). A related but secondary outcome of the social cue use task was the distance of knocks from the optimal stopping point (“distance from optimal”, in which values closer to zero represent more optimal performance). Similar to other tasks (e.g., Lejuez et al., 2003), trials in which the participant surpasses the optimal level were excluded as it is unclear how to weight trials that end after the optimal stopping point as participants may have stopped knocking on the trial that resulted in the door slam or continued to an unknown point.
Data Analytic Procedures
Analysis of covariance (ANCOVA) was used to examine the association between PI status and each measure of social functioning (i.e., FQ factors, CBCL Social Problems scores, and social cue use on the computerized task), with sex and age at testing as covariates. With the exception of descriptive purposes, which examined the CBCL Social Problems clinical cutoff, the dimensional measure of CBCL Social Problems was used throughout. We also tested mediation, in which anxiety and ADHD symptoms were entered simultaneously as putative mediators of the association between PI status and the social functioning metrics listed above, with sex and age at testing as covariates. These multiple mediation models were tested using a single step mediation method with 1,000 samples with replacement using SPSS PROCESS (Hayes, 2013), which provides 95% bias corrected and accelerated confidence intervals (CI) of the indirect effect. If the 95% CI does not include zero, the indirect effect is considered statistically significant, supporting mediation. For the longitudinal analysis of CBCL Social Problems, the later assessment scores were used in place of the cross-sectional score. Lastly, we used partial regression and ANCOVA to examine the association between institutional care history (i.e., age at adoption and months in institutional care) in relation to putative mediators and social functioning variables.
Results
Descriptive statistics are presented along with bivariate correlations to examine the association between PI status, sex, age at testing, anxiety, ADHD symptoms, and CBCL Social Problems (Table 2). As anticipated (based on recruitment of a psychiatrically healthy comparison group), PI status was significantly associated with anxiety and ADHD symptoms at all three Waves (these findings are similar when partialling out the effect of sex). Across the full sample, girls had higher levels of anxiety, however, because girls were overrepresented in the PI group, we examined whether the association between sex and anxiety remained when covarying for PI status and age at testing. There was a statistical trend for girls to have higher anxiety scores than boys (F(1,133)=3.41, p=.067, Cohen’s d=0.31 [95% CI −0.03, 0.65]), even after accounting for PI status. Importantly, proposed mediators (i.e., anxiety and ADHD symptoms) of the association between early institutional rearing and social functioning were positively correlated and both demonstrated bivariate associations with exposure to institutional rearing and higher levels of CBCL Social Problems.
Table 2.
Descriptive statistics and bivariate correlations on standardized measures
| PI status | Sex | Age | ADHD symptoms | Anxiety | Social Problems | Social Problems (Wave 2) | Social Problems (Wave 3) | |
|---|---|---|---|---|---|---|---|---|
| PI status (PI=1) | 1 | .19* | .05 | 45*** | .32*** | .34*** | 48*** | .31* |
| Sex (female=1) | 1 | .05 | −.03 | .21* | .07 | .10 | .16 | |
| Age | 1 | −.003 | −.01 | .11 | .08 | −.08 | ||
| ADHD symptoms | 1 | .61*** | .75*** | .59*** | .58*** | |||
| Anxiety symptoms | 1 | .56*** | .61*** | .56*** | ||||
| Social Problems | 1 | .56*** | 54*** | |||||
| Social Problems (Wave 2) | 1 | 72*** | ||||||
| Social Problems (Wave 3) | 1 | |||||||
| Mean (SD) or % | 47% | 56% | 10.06 (2.02) | 4.92 (4.36) | 17.47 (13.15) | 2.50 (2.63) | 1.98 (2.27) | 2.31 (2.59) |
| Range | 0 – 1 | 0 – 1 | 7 – 13 | 0 – 20 | 0 – 69 | 0 – 13 | 0 – 10 | 0 – 9 |
| N available | 142 | 142 | 142 | 131 | 137 | 131 | 119 | 88 |
Note. PI=previously institutionalized. ADHD=attention-deficit/hyperactivity disorder.
p<.05.
p<.01.
p<.001.
PI Status and Friendship Behavior
The FQ assessed a number of friendship-related behaviors, and those that met criteria for inclusion in the factor analysis can be found in the Appendix. Additionally, we obtained the following descriptive data regarding each child’s closest friendships (see Table 3). The majority of PI and comparison youth were reported to have a best friend as well as a small group of friends. Parents reported on their child’s closest friend’s age and sex. Using ordinal generalized linear regression (with 2=younger friend, 1=same age friend, 0=older friend) a significant effect of PI status was found (Wald χ2(1)=5.29, p=.021). Though the majority of children in both groups had a best friend that was their same age, the effect was driven by comparison children being more likely than PI children to have an older best friend. Comparison and PI youth both overwhelmingly identified their closest friend as belonging to the same sex.
Table 3.
Description of Friendships
| PI (n=67) | Comparison (n=75) | Χ2 | |
|---|---|---|---|
| Has a best friend | 65% | 76% | 1.99 |
| Has a small group of friends | 79% | 84% | 0.76 |
| Age of closest friend | 5.29* | ||
| 1+ years younger | 17% | 8% | |
| Same age | 66% | 60% | |
| 1–2 years older | 17% | 32% | |
| Closest friend is of the same sex | 91% | 92% | 0.05 |
Note. PI=previously institutionalized.
p<.05.
As noted above, the PCA of the FQ resulted in the identification of three factors, which were termed social approach, aggression/overarousal, and empathic concern. After controlling for sex and age at testing, the CBCL Social Problems subscale was correlated with difficulties in social approach (r(122)=.35, p<.001) and aggression/overarousal (r(122)=.34, p<.001). This measure was not significantly correlated with empathic concern (r(122)=−.048, p=.60). We conducted three separate ANCOVAs, with each factor included as the outcome, with PI status as a predictor and sex and age at testing as covariates. As can be seen in Figure 2, PI children did not significantly differ from comparison children on social approach (F(1,130)=0.29, p=.59, d=0.09 [95% CI −0.24, 0.43]) or empathic concern (F(1,130)=1.06,p=.30, d=0.18 [95% CI - 0.16, 0.52]). In contrast, PI children had significantly higher scores on aggression/overarousal (F(1,130)=5.17, p=025, d=−0.39 [95% CI −0.73, −0.05]).
Figure 2. Group differences based on previous institutional care on factors from the Friendship Questionnaire.
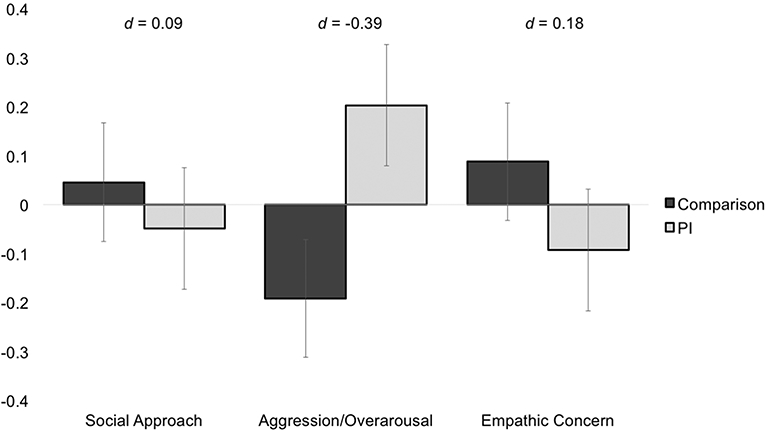
Note. PI=previously institutionalized. Error bars=1 standard error.
PI Status and CBCL Social Problems
An identical approach to examining the association of PI status and social functioning used above was repeated with the outcome of CBCL Social Problems (i.e., an ANCOVA with PI status as a predictor controlling for sex and age at testing). This analysis revealed that PI children had significantly higher CBCL Social Problems scores than comparison children (F(1,127)=15.45, p<.001, d=−0.70 [95% CI −1.05, −0.34]). Sex and age at testing were not significantly associated with CBCL Social Problems (ps>.33). Using a binary split to identify those at clinical concern based on T scores, which allows comparison to age and sex matched norms, 27% of the PI individuals vs. 8% of the comparison children had scores in this range (compared to the 5% that would be expected based on age and sex norms).
Computerized Social Cue Use Task
A laboratory measure of social cue use was collected in a subset of participants. Total number of points earned on this task ranged from 38–256 (M=159.10, SD=54.53). We used a repeated measures ANCOVA to examine the effect of PI status on points, with condition repeated by task condition (i.e., quick-to-anger, intermediate, and slow-to-anger), controlling for sex and age at testing. The between subjects analysis revealed that, overall, PI children earned fewer points than comparison children (F(1,101)=7.35,p=.01, d=0.51 [95% CI 0.11, 0.91]; Figure 1B). These analyses were repeated with distance from the optimal stopping point as the outcome, and PI children (M=−6.36 [SE=0.11]) were further from the optimal stopping point, on average, than comparison children (M=−4.96 [SE=0.09]) (F(1,2502)=97.38,p<.001, d=0.51 [95% CI 0.11, 0.91]).
Performance over the course of the task differed by group and condition, which was confirmed by a significant three-way interaction (F(2,100)=4.34, p=.016) from a repeated measures ANCOVA with distance from the optimal stopping point as the outcome of interest, first vs. last trial, condition, and PI status as predictors, and sex and age at testing as covariates. Changes in performance on the slow-to-anger condition were the most pronounced based on PI status. As can be seen in Figure 1C, comparison children improved their performance with greater trials, whereas PI children were relatively stable in their distance from optimal performance (Figure 1D). PI children had smaller gains from the first to last trial than comparison children (F(1,97)=8.64, p=.004, d=0.59 [95% CI 0.18, 1.00]). Using two paired t-tests to compare the distance from optimal on the first and last trial, we found that PI children did not differ on the final and first trial (M difference=−0.22 [SE=0.70], t(35)=−0.32, p=.75), whereas the comparison children scores were significantly more optimal on the final trial compared to the first (M difference=−2.42 [SE=0.74], t(58)=−3.28, p=.002). Distance from optimal scores on this final trial ranged from 0 to −17 (M=−8.82, SD=4.91), with higher (i.e., less negative) scores indicating greater ability to use facial emotion cues to guide social behavior. Consistent with expectations, this distance from optimal performance was negatively associated with CBCL Social Problems, after controlling for sex and age at testing (r(87)=−.23, p=.029). Further, the distance from optimal performance significantly mediated the association between PI status and overall points earned on the task using a single step mediation analysis (indirect effect=−21.65, 95% CI [−36.98, −7.79]), suggesting that the lower points earned in the PI group were associated with group differences in this marker of learning from social cues (Figure 1E).
Tests of Multiple Mediation
We examined whether psychopathology in children (i.e., anxiety and ADHD symptoms) had unique mediating effects on discrete aspects of social functioning as measured via three Waves of CBCL Social Problems, factors from the FQ, and social cue use. Multiple mediation allowed for simultaneous testing of both putative mediators as well as the statistical control of specified covariates (i.e., sex and age at testing). The summary of mediation results can be found in Table 4. The direct effect of PI status on CBCL Social Problems and the FQ factors were not statistically significant when anxiety and ADHD symptoms were included in the model, with the exception of the social approach factor, such that PI status was associated with reduced difficulties in social approach in the full model. ADHD symptoms, but not anxiety, significantly mediated the association between PI status and CBCL Social Problems and aggression/overarousal. Anxiety symptoms, but not ADHD, mediated the association between PI status and increased difficulties in social approach. PI status was directly associated with suboptimal social cue use behavior, and there was a significant indirect effect of ADHD symptoms, but not anxiety.
Table 4.
Summary of single step multiple mediation analyses.
| Outcome | Direct Effect of PI Status | Anxiety Specific Indirect Effect | ADHD Symptoms Specific Indirect Effect | Total Indirect Effect of PI Status |
|---|---|---|---|---|
| CBCL Social Problems | −0.17 (−0.85, 0.50) | 0.21 (−0.10, 0.71) | 1.71 (0.98, 3.64) | 1.92 (1.05, 2.93) |
| CBCL Social Problems (Wave 2) | 0.79 (−0.18, 0.08) | 0.37 (−0.18, 1.36) | 0.68 (0.09, 1.62) | 1.05 (0.42, 2.23) |
| CBCL Social Problems (Wave 3) | 0.06 (−1.33, 1.44) | 0.45 (−0.28, 1.66) | 1.10 (0.47, 1.18) | 1.55 (0.70, 2.56) |
| Social Approach | −0.45 (−0.83, −0.07) | 0.22 (0.04, 0.43) | 0.17 (−0.04, 0.45) | 0.38 (0.16, 0.64) |
| Aggression/Overarousal | −0.02 (−0.39, 0.37) | −0.05 (−0.25, 0.09) | 0.46 (0.17, 0.80) | 0.41 (0.18, 0.68) |
| Empathic Concern | −0.05 (−0.47, 0.37) | 0.01 (−0.16, 0.18) | −0.06 (−0.32, 0.18) | −0.05 (−0.26, 0.15) |
| Social Cue Usea | −2.20 (−4.26, −0.14) | 0.14 (−0.11, 0.99) | −0.80 (−1.93, −0.07) | −0.66 (−1.65, 0.02) |
Note. Estimate (95% bias corrected bootstrap confidence intervals). Bolded values indicate that the 95% confidence intervals do not include zero. PI=previously institutionalized. CBCL=child behavior checklist.
Distance from optimal on the final trial of the social cue use task.
The longitudinal analyses of social problems from the CBCL were consistent with the cross-sectional data, indicating that ADHD symptoms significantly mediated the association between PI status and higher CBCL Social Problems scores at all three time points. Taken together, these mediation results show that higher ADHD symptoms prospectively mediated the association between PI status and social functioning difficulties.
Institutional Care History
The PI sample represents a heterogeneous group, as children varied in age at adoption and duration of time spent in institutional care. Given severity of deprivation experiences is associated with longer term functioning (Julian, 2013), as a secondary analysis we examined age at adoption and months spent in institutional care (transformed using a square root transformation to correct for positive skew) in relation to CBCL Social Problems, FQ factors, as well as anxiety and ADHD symptoms among PI children with available data. Unfortunately, the small cell sizes found using a group-based approach (necessary for examining the possibility of stepwise approaches to age at adoption; see Merz & McCall, 2010) precluded us from examining outcomes using this approach. Using partial correlation, controlling for sex and age at testing, the age at adoption was not significantly associated with any social functioning outcome or with anxiety (ps>.10). However, there was a positive association between age at adoption and ADHD symptoms (r(59)=.30, p=.020), indicating that those children adopted at later ages had higher levels of ADHD symptoms. For months spent in institutional care, there was a trend level finding for greater duration of institutional care and social problems (r(59)=.23, p=.072), the longer duration of institutional care exposure was associated with ADHD symptoms (r(59)=.30, p=.019).
Discussion
We examined social functioning using a multimodal longitudinal assessment approach in a sample of children with and without a history of early institutional rearing. Our findings build upon prior literature on PI children’s social functioning in two important ways. First, we identified domains of social behavior with peers that are (and are not) associated with early institutional rearing. Specifically, using a validated measure of social problems, we found that PI children are more likely than age and sex norms to meet the clinical concern threshold. We found that, at the group level, parents of PI children were more likely than parents of healthy comparison children without a history of institutional care to endorse aggression/overarousal behaviors as reasons for friendship challenges. PI children were reported to be similar to comparison children in their mean levels of social approach and empathic concern. PI children were just as likely as comparison youth to establish close friendships, though comparison children were more likely to have an older best friend. In addition, using a laboratory-based assessment of social cue use, we observed that PI children, on average, had more difficulties in learning from social cues and adjusting behavior accordingly when compared to the never institutionalized comparison children. Second, we explored potential mechanisms for impaired social functioning in this heterogeneous group of children who experienced early institutional rearing. Based on the clinical and developmental literatures, anxiety and ADHD symptoms were identified as potential correlates of social difficulties, and ADHD symptoms mediated the association between PI status and behavior characterized by aggression/overarousal as well as CBCL Social Problems both cross-sectionally and longitudinally. Anxiety symptoms only mediated the association between PI status and decreased social approach behavior.
On average, PI children have more social difficulties than children without a history of institutional rearing, a finding that is supported by previous research (Groza et al., 2003; Hawk & McCall, 2010; Hodges & Tizard, 1989; Julian & McCall, 2016; Kim et al., 1999; Merz & McCall, 2010; Sonuga-Barke et al., 2010). Observational data from social interactions from the Bucharest Early Intervention Project, which followed a group of children who experienced severe psychosocial deprivation in Romanian institutions, identified deficits in social competence following institutional rearing (Almas et al., 2015). In the current study we find evidence that early exposure to institutional care is associated with greater likelihood of social problems. Early social experiences play a critical role in the development of neural pathways that control for appropriate social interactions (Callaghan & Tottenham, 2015; Gabard-Durnam et al., 2014; Tottenham, 2012, 2015). Accordingly, poor caregiving in early development can impede the ability to build appropriate social behaviors later in life (Landry, Smith, Miller-Loncar, & Swank, 1997; Tottenham et al., 2010).
Difficulties establishing and maintaining friendships in school-age children are thought to involve multiple domains of competence. Friendship training programs for children with social difficulties include teaching how to initiate social contact (e.g., making eye contact and introducing oneself), seek permission before joining games or play activities, and responding to insults appropriately (Frankel, 2005; Frankel & Feinberg, 2002; Frankel, Myatt, Cantwell, & Feinberg, 1997). While we did not examine these specific behaviors, our findings along with previous work find that children with institutional rearing histories are at risk for poorer friendship quality (Hawk & McCall, 2010) lower levels of popularity (Hodges & Tizard, 1989), and increased aggression/overarousal in social interactions with peers. The endorsement of aggressive and dysregulated behavior as reasons for any friendship difficulty in PI children is consistent with the finding that early institutional rearing enhances the risk of developing externalizing problems later in life (Humphreys, Gleason, et al., 2015), and their association may be due, in part, to similar behaviors from the FQ aggression/overarousal factor and externalizing psychopathology, including hyperactivity and impulsivity.
Furthermore, PI children, on average, had greater difficulties learning from social cues. Despite the findings that emotional face processing may be a case of relative sparing following institutional rearing (Young, Luyster, Fox, Zeanah, & Nelson, 2017), and early institutional care is unrelated to emotional identification of angry faces (Bick, Luyster, Fox, Zeanah, & Nelson, 2017; Fries & Pollak, 2004), here, when angry faces were used as social cues for decisionmaking, we found differences in behavioral responses to incrementally increasing angry emotional facial cues. The ability to understand and use facial expressions of emotion to guide and adjust behavior is an important task for navigating social interactions. In a separate line of work using the same social cue use task in clinically diagnosed children with and without ADHD, we found that that poorer learning on the task helped to explain the association between ADHD symptoms and social problems from the CBCL (Humphreys et al., 2016).
ADHD symptoms were a significant mediator for every social behavior outcome in which PI and the comparison children differed. ADHD symptoms are a long-lasting phenotype associated with early institutional rearing (Humphreys & Zeanah, 2015; Stevens et al., 2008), and there is mixed evidence regarding whether caregiving quality can alter the trajectory of higher ADHD symptoms over time among children with a history of institutional care (Humphreys, Gleason, et al., 2015; Tibu, Humphreys, Fox, Nelson, & Zeanah, 2014). However, additional time in institutional care appeared to be associated with ADHD symptoms in the present study, consistent with some prior work (Stevens et al., 2008). In fact, the association between age at adoption and months spent in institution care was specifically associated with greater ADHD symptoms, and did not reach statistical significance in the prediction of social problems (in contrast with prior work linking older age at placement to social problems [Groza et al., 2003; Julian & McCall, 2016; Sonuga-Barke et al., 2010]). Given the persistent indirect effects found for ADHD symptoms in mediating the association between PI status and social functioning outcomes when measured concurrently and at two subsequent follow-up assessments, further exploration into whether attentional deficits may be responsible for impairments in other domains associated with early institutional rearing is warranted. This link suggest that treatment of ADHD symptoms may have benefits for social functioning following institutional care, though this remains to be formally tested.
Anxiety symptoms were also elevated in these children with a history of early institutional rearing relative to the comparison group in this sample. Other samples of adolescents and young adults with a history of institutional care are mixed, though most find increased anxiety in this population (Ellis et al., 2004; Erol, Simsek, & Münir, 2010; Humphreys, Gleason, et al., 2015; Sonuga-Barke et al., 2017), and it is possible that the subgroup of PI children with elevated anxiety symptoms may be different in important ways than those children with elevated DSED signs, though both may be associated with social difficulties. DSED has been linked to poorer inhibitory control (Bruce, Tarullo, & Gunnar, 2009), which could manifest in the type of behavior characterized here as aggression or overarousal. In contrast, social reticence has also been linked to institutional care history (Almas et al., 2015), and may be a behavioral feature of the anxiety exhibited in some PI children. It follows that anxious children, despite a desire to engage with others socially, may miss out on social opportunities due to anxiety. This in turn may result in fewer opportunities to take part in social interactions required for acquisition of social skills, creating a cascade of additional anxiety and lack of social opportunities. Though there was no bivariate association between PI status and social approach, anxiety was found to significantly mediate the association between PI status and reduced social approach.
The findings from this study should be considered in the context of several important limitations. First, we selected anxiety and ADHD symptoms as a priori psychopathology domains of interest due to their increased prevalence in children with a history of institutional rearing. Other forms of psychopathology are relevant to social functioning and found in elevated rates among children with early institutional care exposure, including autism-like behaviors, disinhibited social behavior, depression, oppositional behavior, and callous-unemotional traits (Goff & Tottenham, 2015; Humphreys, McGoron, et al., 2015; Humphreys, Nelson, Fox, & Zeanah, 2017; Kumsta et al., 2010; Levin, Fox, Zeanah, & Nelson, 2015; Rutter, Colvert, et al., 2007; VanTieghem et al., 2016) also merit study in the context of early caregiving quality. Previous work has linked deprivation-specific patterns from children who were cared for in Romanian orphanages, including cognitive impairment, disinhibited social behavior, “quasiautism”, as well as inattention/overactivity behaviors with peer difficulties in PI children (Rutter, Colvert, et al., 2007; Rutter, Kreppner, et al., 2007; Sonuga-Barke et al., 2010). Second, our measurement of social functioning included the use of the FQ, which is the first ever use of this assessment and no test-retest information was available. Though there was convergence between the aggression/overarousal factor and CBCL Social Problems total score, the other factors were unrelated to this measure. As a related point, it is unclear whether empathic concern measured the same construct as is assessed in studies of callous-unemotional traits, as past research indicates that children with histories of institutional care, on average, are more likely to be callous-unemotional (Humphreys, McGoron, et al., 2015; Kumsta, Sonuga-Barke, & Rutter, 2012). Third, some of our measures were only available cross-sectionally (i.e., the social cue use task). Fourth, there are limitations in our approach to compare groups in our sample (e.g., more females in PI sample, healthy comparison sample selection).
There is no ideal control group for children that have experienced institutional care abroad followed by international adoption. Nonetheless, the inclusion of a never-institutionalized comparison group is helpful for providing a benchmark in which to compare PI children on measures and tasks that are not normed in a population representative sample, thereby allowing us to probe potential mechanisms underlying any social difficulties following this type of early caregiving neglect. In addition, the PI sample was heterogeneous in terms of months in institutional care, age at placement, country of origin, and experiences of institutional care quality. While duration of exposure to institutional care/age adopted appeared to be associated with some aspects of current functioning, the lack of accurate assessments of age at placement and adoption, as well as the lack of prenatal and preadoption histories for these children makes it difficult to disentangle various forms of risk that could be affecting observed behaviors. The English and Romanian Adoptees Study (Rutter, Sonuga-Barke, & Castle, 2010) and Bucharest Early Intervention Project (Zeanah et al., 2003) both indicate that age at adoption are important predictors of later functioning. However, the current sample is more diverse than those exemplars given the breadth of countries of origin in our sample, which may be associated with more variation in pre-adoption quality of care. Such non-assessed differences in children who experienced institutional care (e.g., quality of attachment relationships in early life) may be relevant to both ADHD symptoms and social functioning. While this study has limitations regarding knowledge about the role of the preadoption environment and perfect accuracy about age at adoption in some cases, this design allows for the assessment of the duration of exposure to neglect, which is not usually possible in most human studies that assess correlates and consequences of early adversity (i.e., because the majority of children in adverse environments remain in the same environment throughout childhood).
Conclusion
In conclusion, our study provides new insight into the mechanisms underlying the previously well-documented risk for social functioning difficulties among children with early institutional rearing. It is worth noting that the majority of PI children did not meet the threshold for clinical concern in social problems, and when factors of social functioning were identified, PI and comparison children did not significantly differ in their social approach behaviors or in empathic concern. We found instead that parents were more likely to endorse increased aggression/overarousal as a reason for potential friendship difficulties in children with histories of institutional care, compared to never institutionalized participants. For those PI children, behaviors when with peers were more likely to be characterized by aggression/overarousal, difficulties in attention, hyperactivity, and impulsivity, as well as poorer social cue use (i.e., emotional expressions) to guide behavior. This provides insight into how social functioning may be impaired following early institutional care exposure. These findings show that when PI children struggle with friendships, mechanisms involving attention and behavior regulation are likely contributors. Therefore, interventions targeting attention and behavior regulation may be beneficial for social difficulties as well.
Supplementary Material
Acknowledgements:
The authors thank the participants. This research was supported by National Institute of Mental Health Grants F32-MH107129 (KLH) and R01-MH091864 (NT), the Dana Foundation (NT), the Brain and Behavior Research Foundation (formerly NARSAD) Young Investigator Award 23819 (KLH), a Klingenstein Third Generation Foundation Fellowship (KLH), and a Jacobs Foundation Early Career Research Fellowship (KLH).
References
- Achenbach TM, & Rescorla LA (2001). ASEBA School Age Forms and Profiles. Burlington, VT: University of Vermont. Burlington, VT: ASEBA. [Google Scholar]
- Almas AN, Degnan KA, Radulescu A, Nelson CA, Zeanah CH, & Fox NA (2012). Effects of early intervention and the moderating effects of brain activity on institutionalized children’s social skills at age 8. PNAS, 109 Suppl, 17228–31. doi: 10.1073/pnas.1121256109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almas AN, Degnan KA, Walker OL, Radulescu A, Nelson CA, Zeanah CH, & Fox NA (2015). The effects of early institutionalization and foster care intervention on children’s social behaviors at the age of eight. Social Development, 24(2), 225–239. doi: 10.1111/sode.12089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) (5th ed.). Arlington, VA, DC: American Psychiatric Publishing. [Google Scholar]
- Bagwell CL, Molina BSG, Pelham WE, & Hoza B (2001). Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1285–1292. doi: 10.1097/00004583-200111000-00008 [DOI] [PubMed] [Google Scholar]
- Bick J, Luyster R, Fox NA, Zeanah CH, & Nelson CA (2017). Effects of early institutionalization on emotion processing in 12-year-old youth. Development and Psychopathology, 29(05), 1749–1761. doi: 10.1017/S0954579417001377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 545–53. doi: 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Bornstein MH, Hendricks C, Haynes OM, & Painter KM (2007). Maternal sensitivity and child responsiveness: Associations with social context, maternal characteristics, and child characteristics in a multivariate analysis. Infancy, 12(2), 189–223. [DOI] [PubMed] [Google Scholar]
- Bruce J, Tarullo AR, & Gunnar MR (2009). Disinhibited social behavior among internationally adopted children. Development and Psychopathology, 21(1), 157–171. doi: 10.1017/S0954579409000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan BL, & Tottenham N (2015). The neuro-environmental loop of plasticity: A cross-species analysis of parental effects on emotion circuitry development following typical and adverse caregiving. Neuropsychopharmacology, 41(1), 1–14. doi: 10.1038/npp.2015.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csáky C (2009). Keeping children out of harmful institutions: Why we should be investing in family-based care. Save the Children, 1–34. [Google Scholar]
- de Boo GM, & Prins PJM (2007). Social incompetence in children with ADHD: Possible moderators and mediators in social-skills training. Clinical Psychology Review, 27, 78–97. doi: 10.1016/j.cpr.2006.03.006 [DOI] [PubMed] [Google Scholar]
- Delis DC, Freeland J, Kramer JH, & Kaplan E (1988). Integrating clinical assessment with cognitive neuroscience: Construct validation of the California Verbal Learning Test. Journal of Consulting and Clinical Psychology, 56(1), 123–130. doi: 10.1037/0022-006X.56.1.123 [DOI] [PubMed] [Google Scholar]
- Ellis BH, Fisher PA, & Zaharie S (2004). Predictors of disruptive behavior, developmental delays, anxiety, and affective symptomatology among institutionally reared Romanian children. Journal of the American Academy of Child and Adolescent Psychiatry, 43(10), 1283–92. doi: 10.1097/01.chi.0000136562.24085.160 [DOI] [PubMed] [Google Scholar]
- Erath SA, Flanagan KS, & Bierman KL (2007). Social anxiety and peer relations in early adolescence: Behavioral and cognitive factors. Journal of Abnormal Child Psychology, 35, 405–416. doi: 10.1007/s10802-007-9099-2 [DOI] [PubMed] [Google Scholar]
- Erol N, Simsek Z, & Münir K (2010). Mental health of adolescents reared in institutional care in Turkey: Challenges and hope in the twenty-first century. European Child and Adolescent Psychiatry, 19(2), 113–124. doi: 10.1007/s00787-009-0047-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman R, & Klein PS (2003). Toddlers’ self-regulated compliance to mothers, caregivers, and fathers: Implications for theories of socialization. Developmental Psychology, 39(4), 680–692. doi: 10.1037/0012-1649.39.4.680 [DOI] [PubMed] [Google Scholar]
- Frankel FD (2005). Parent-Assisted Children’s Friendship Training In Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice, 2nd ed. (pp. 693–715). Retrieved from http://search.ebscohost.com.proxy-ub.rug.nl/login.aspx?direct=true&db=psyh&AN=2005-00278-026&site=ehost-live&scope=site [Google Scholar]
- Frankel FD, & Feinberg D (2002). Social problems associated with ADHD vs. ODD in children referred for friendship problems. Child Psychiatry and Human Development, 33(2), 125–146. doi: 10.1023/A:1020730224907 [DOI] [PubMed] [Google Scholar]
- Frankel FD, Myatt R, Cantwell DP, & Feinberg DT (1997). Parent-assisted transfer of children’s social skills training: Effects on children with and without attention-deficit hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 36(8), 1056–1064. doi: 10.1097/00004583-199708000-00013 [DOI] [PubMed] [Google Scholar]
- Fries ABW, & Pollak SD (2004). Emotion understanding in postinstitutionalized Eastern European children. Development and Psychopathology, 16, 355–369. doi: 10.1017/S0954579404044554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabard-Durnam LJ, Flannery J, Goff B, Gee DG, Humphreys KL, Telzer E, ... Tottenham N (2014). The development of human amygdala functional connectivity at rest from 4 to 23 years: A cross-sectional study. Neuroimage, 95, 193–207. doi: 10.1016/j.neuroimage.2014.03.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason MM, Fox NA, Drury S, Smyke AT, Egger HL, Nelson CA, ... Zeanah CH (2011). Validity of evidence-derived criteria for reactive attachment disorder: Indiscriminately social/disinhibited and emotionally withdrawn/inhibited types. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 216–231. doi: 10.1016/j.jaac.2010.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff B, & Tottenham N (2015). Early-life adversity and adolescent depression: mechanisms involving the ventral striatum. CNS Spectrums, 20(4), 337–345. doi: 10.1017/S1092852914000674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groza V, Ryan SD, & Cash SJ (2003). Institutionalization, behavior and international adoption: Predictors of behavior problems. Journal of Immigrant Health, 5(1), 5–17. doi: 10.1023/A:1021096028003 [DOI] [PubMed] [Google Scholar]
- Guyon-Harris KL, Humphreys KL, Degnan KA, Fox NA, Nelson CA, & Zeanah CH (in press). A prospective longitudinal study of reactive attachment disorder following early institutional care: Considering variable- and person-centered approaches. Attachment & Human Development. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon-Harris KL, Humphreys KL, Fox NA, Nelson CA, & Zeanah CH (2018a). Course of disinhibited social engagement disorder from early childhood to early adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 57(5), 329–335.e2. doi: 10.1016/J.JAAC.2018.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon-Harris KL, Humphreys KL, Fox NA, Nelson CA, & Zeanah CH (2018b). Signs of attachment disorders and social functioning among early adolescents with a history of institutional care. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk B, & McCall RB (2010). CBCL behavior problems of post-institutionalized international adoptees. Clinical Child and Family Psychology Review, 13(2), 199–211. doi: 10.1007/s10567-010-0068-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis. New York, NY: Guilford; New York: Guilford Press; doi: 978-1-60918-230-4 [Google Scholar]
- Hodges J, & Tizard B (1989). Social and family relationships of ex-institutional adolescents. Journal of Child Psychology and Psychiatry, 30, 77–97. doi: 10.1111/j.1469-7610.1989.tb00770.x [DOI] [PubMed] [Google Scholar]
- Humphreys KL, Galán CA, Tottenham N, & Lee SSS (2016). Impaired social decision-making mediates the association between ADHD and social problems. Journal of Abnormal Child Psychology, 44(5), 1023–1032. doi: 10.1007/s10802-015-0095-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Gleason MM, Drury SS, Miron D, Nelson CA, Fox NA, & Zeanah CH (2015). Effects of institutional rearing and foster care on psychopathology at age 12 years in Romania: Follow-up of an open, randomised controlled trial. The Lancet Psychiatry, 2(7), 625–634. doi: 10.1016/S2215-0366(15)00095-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, McGoron L, Sheridan MA, McLaughlin KA, Fox NA, Nelson CA, & Zeanah CH (2015). High-quality foster care mitigates callous-unemotional traits following early deprivation in boys: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 54(12), 977–983. doi: 10.1016/j.jaac.2015.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Miron D, McLaughlin KA, Sheridan MA, Nelson CA, Fox NA, & Zeanah CH (2018). Foster care promotes adaptive functioning in early adolescence among children who experienced severe, early deprivation. Journal of Child Psychology and Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Nelson CA, Fox NA, & Zeanah CH (2017). Signs of reactive attachment disorder and disinhibited social engagement disorder at age 12 years: Effects of institutional care history and high-quality foster care. Development and Psychopathology, 29(2), 675–684. doi: 10.1017/S0954579417000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, & Zeanah CH (2015). Deviations from the expectable environment in early childhood and emerging psychopathology. Neuropsychopharmacology, 40(1), 154–170. doi: 10.1038/npp.2014.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julian MM (2013). Age at adoption from institutional care as a window into the lasting effects of early experiences. Clinical Child and Family Psychology Review, 16(2), 101–145. doi: 10.1007/s10567-013-0130-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julian MM, & McCall RB (2016). Social skills in children adopted from socially-emotionally depriving institutions. Adoption Quarterly, 19(1), 44–62. doi: 10.1080/10926755.2015.1088106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim WJ, Shin YJ, & Carey MP (1999). Comparison of Korean-American adoptees and biological children of their adoptive parents: A pilot study. Child Psychiatry and Human Development, 29(3), 221–228. doi: 10.1023/A:1022665024514 [DOI] [PubMed] [Google Scholar]
- Kirsh SJ, & Mounts JRW (2007). Violent video game play impacts facial emotion recognition. Aggressive Behavior, 33(4), 353–358. doi: 10.1002/ab.20191 [DOI] [PubMed] [Google Scholar]
- Kreppner JM, O’Connor TG, & Rutter M (2001). Can inattention/overactivity be an institutional deprivation syndrome? Journal of Abnormal Child Psychology, 29(6), 513–28. [DOI] [PubMed] [Google Scholar]
- Kumsta R, Kreppner J, Rutter M, Beckett C, Castle J, Stevens S, & Sonuga-Barke EJ (2010). III. Deprivation-specific psychological patterns. Monographs of the Society for Research in Child Development, 75(1), 48–78. doi: 10.1111/j.1540-5834.2010.00550.x [DOI] [PubMed] [Google Scholar]
- Kumsta R, Sonuga-Barke E, & Rutter M (2012). Adolescent callous-unemotional traits and conduct disorder in adoptees exposed to severe early deprivation. British Journal of Psychiatry, 200, 197–201. doi: 10.1192/bjp.bp.110.089441 [DOI] [PubMed] [Google Scholar]
- Laible D, & Thompson RA (2007). Early socialization: A relationship perspective In Grusec JE & Hastings PD (Eds.), Handbook of Socialization: Theory and Research (pp. 181–207). New York: Guilford Press. [Google Scholar]
- Landry SH, Smith KE, Miller-Loncar CL, & Swank PR (1997). Predicting cognitive-language and social growth curves from early maternal behaviors in children at varying degrees of biological risk. Developmental Psychology, 33(6), 1040–1053. doi: 10.1037/0012-1649.33.6.1040 [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin WM, Jones HA, Richards JB, Strong DR, Kahler CW, & Read JP (2003). The Balloon Analogue Risk Task (BART) differentiates smokers and nonsmokers. Experimental and Clinical Psychopharmacology, 11, 26–33. doi: 10.1037/1064-1297.11.1.26 [DOI] [PubMed] [Google Scholar]
- Levin AR, Fox NA, Zeanah CH, & Nelson CA (2015). Social communication difficulties and autism in previously institutionalized children. Journal of the American Academy of Child and Adolescent Psychiatry, 54(2), 108—115.e1. doi: 10.1016/j.jaac.2014.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YH, & Tottenham N (2013). Exposure to the self-face facilitates identification of dynamic facial expressions: Influences on individual differences. Emotion, 13(2), 196–202. doi: 10.1037/a0030755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, & Nelson CA (2017). Neglect as a violation of species-expectant experience: Neurodevelopmental consequences. Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrell KW, & Boelter E (2001). An investigation of relationships between social behavior and ADHD in children and youth: Construct validity of the Home and Community Social Behavior Scales. Journal of Emotional and Behavioral Disorders, 9(4), 260–269. doi: 10.1177/106342660100900406 [DOI] [Google Scholar]
- Merz EC, & McCall RB (2010). Behavior problems in children adopted from psychosocially depriving institutions. Journal of Abnormal Child Psychology, 38(4), 459–470. doi: 10.1007/s10802-009-9383-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Colvert E, Kreppner J, Beckett C, Castle J, Groothues C, ... Sonuga-Barke EJSS (2007). Early adolescent outcomes for institutionally-deprived and non-deprived adoptees. I: disinhibited attachment. Journal of Child Psychology and Psychiatry, 48(1), 17–30. doi: 10.1111/j.1469-7610.2006.01688.x [DOI] [PubMed] [Google Scholar]
- Rutter M, Kreppner J, Croft C, Murin M, Colvert E, Beckett C, ... Sonuga-Barke E (2007). Early adolescent outcomes of institutionally deprived and non-deprived adoptees. III. Quasi-autism. Journal of Child Psychology and Psychiatry, 48(12), 1200–1207. doi: 10.1111/j.1469-7610.2007.01792.x [DOI] [PubMed] [Google Scholar]
- Rutter M, Sonuga-Barke EJ, & Castle J (2010). I. Investigating the impact of early institutional deprivation on development: Background and research strategy of the English and Romanian Adoptees (ERA) study. Monographs of the Society for Research in Child Development, 75(1), 1–20. doi: 10.1111/j.1540-5834.2010.00548.x [DOI] [PubMed] [Google Scholar]
- Shaw DS, Bell RQ, & Gilliom M (2000). A truly early starter model of antisocial behavior revisited. Clinical Child and Family Psychology Review, 3(3), 155–172. doi: 10.1023/A:1009599208790 [DOI] [PubMed] [Google Scholar]
- Smyke AT, Koga SF, Johnson DE, Fox NA, Marshall PJ, Nelson CA, & Zeanah CH (2007). The caregiving context in institution-reared and family-reared infants and toddlers in Romania. Journal of Child Psychology and Psychiatry, 48, 210–218. doi: 10.1111/j.1469-7610.2006.01694.x [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Kennedy M, Kumsta R, Knights N, Golm D, Rutter M, ... Kreppner J (2017). Child-to-adult neurodevelopmental and mental health trajectories after early life deprivation: the young adult follow-up of the longitudinal English and Romanian Adoptees study. The Lancet, 389(10078), 1539–1548. doi: 10.1016/S0140-6736(17)30045-4 [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Schlotz W, & Kreppner J (2010). V. Differentiating developmental trajectories for conduct, emotion, and peer problems following early deprivation. Monographs of the Society for Research in Child Development, 75(1), 102–124. [DOI] [PubMed] [Google Scholar]
- Stevens SE, Sonuga-Barke EJS, Kreppner JM, Beckett C, Castle J, Colvert E, ... Rutter M (2008). Inattention/overactivity following early severe institutional deprivation: presentation and associations in early adolescence. Journal of Abnormal Child Psychology, 56(3), 385–98. doi: 10.1007/s10802-007-9185-5 [DOI] [PubMed] [Google Scholar]
- Strauss CC, Lease CA, Kazdin AE, Dulcan MK, & Last CG (1989). Multimethod assessment of the social competence of children with anxiety disorders. Journal of Clinical Child Psychology, 18, 184–189. doi: 10.1207/s15374424jccp1802_10 [DOI] [Google Scholar]
- Tibu F, Humphreys KL, Fox NA, Nelson CA, & Zeanah CH (2014). Psychopathology in young children in two types of foster care following institutional rearing. Infant Mental Health Journal, 35(2), 123–131. doi: 10.1002/imhj.21428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N (2012). Risk and developmental heterogeneity in previously institutionalized children. The Journal of Adolescent Health, 51(2 Suppl), S29–33. doi: 10.1016/j.jadohealth.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N (2015). Social scaffolding of human amygdala-mPFCcircuit development. Social Neuroscience, 10(5), 1–11. doi: 10.1080/17470919.2015.1087424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Hare TA, Quinn BT, McCarry TW, Nurse M, Gilhooly T, ... Casey BJ (2010). Prolonged institutional rearing is associated with atypically large amygdala volume and difficulties in emotion regulation. Developmental Science, 13, 46–61. doi: 10.1111/j.1467-7687.2009.00852.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, ... Nelson C (2009). The NimStim set of facial expressions: Judgments from untrained research participants. Psychiatry Research, 168(3), 242–249. doi: 10.1016/j.psychres.2008.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van IJzendoorn MH, Palacios J, Sonuga-Barke EJS, Gunnar MR, Vorria P, McCall RB, ... Juffer F (2011). I. Children in institutional care: Delayed development and resilience. Monographs of the Society for Research in Child Development, 76(4), 8–30. doi: 10.1111/j.1540-5834.2011.00626.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanTieghem M, Bolger N, Gabard-Durnam LJ, Goff B, Flannery J, Humphreys KL, ... Tottenham N (2016). Adaptation and attachment: Effects of valence bias and parent-child relationship security on internalizing problems following early institutional rearing. [DOI] [PMC free article] [PubMed]
- Wiik KL, Loman MM, Van Ryzin MJ, Armstrong JM, Essex MJ, Pollak SD, & Gunnar MR (2011). Behavioral and emotional symptoms of post-institutionalized children in middle childhood. Journal of Child Psychology and Psychiatry, 52, 56–63. doi: 10.1111/j.1469-7610.2010.02294.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A, Luyster RJ, Fox NA, Zeanah CH, & Nelson CA (2017). The effects of early institutionalization on emotional face processing: evidence for sparing via an experience-dependent mechanism. British Journal of Developmental Psychology, 35(3), 439–453. doi: 10.1111/bjdp.12185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH, Humphreys KL, Fox NA, & Nelson CA (2017). Alternatives for abandoned children: insights from the Bucharest Early Intervention Project. Current Opinion in Psychology, 15. doi: 10.1016/j.copsyc.2017.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH, Nelson CA, Fox NA, Smyke AT, Marshall P, Parker SW, & Koga S (2003). Designing research to study the effects of institutionalization on brain and behavioral development: The Bucharest Early Intervention Project. Development and Psychopathology, 15, 885–907. doi: 10.1017/S0954579403000452 [DOI] [PubMed] [Google Scholar]
- Zeanah CH, Smyke AT, & Settles L (2006). Children in orphanages In McCartney K & Phillips D (Eds.), Blackwell Handbook of Early Childhood Development (pp. 224–254). Malden, MA: Blackwell Publishing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


