Abstract
While racial discrimination (RD) is associated with increased alcohol-related problems among African Americans (AAs), researchers have not examined how RD contributes to the physical consequences of alcohol consumption over time. Additionally, the protective role of religious coping has been discussed but not formally tested in pathways connecting RD to the physical consequences of alcohol consumption. To address this gap, we estimated latent growth mediation models in a sample of 465 AA emerging adults. We found that RD increased physical consequences of alcohol consumption over time through psychological distress. After identifying two profiles of religious coping (i.e., low and high religious coping), RD indirectly influenced the physical consequences of alcohol consumption through psychological distress among AAs in the low religious coping group. Our results signal the importance of developing alcohol-misuse prevention programs that address the psychological consequences of RD. Integrating culturally-tailored coping strategies (e.g., religious coping) may bolster the efficacy of these prevention programs.
Keywords: Racial discrimination, Health Disparities, Alcohol, Religious Coping
Although epidemiologists posit that African Americans (AAs) use less alcohol than White Americans from youth to adulthood (Substance Abuse and Mental Health Services Administration [SAMHSA], 2011), AAs who consume alcohol report more alcohol-related problems such as drinking-related illnesses and accidents (see Zapolski et al., 2014). To understand why AAs are likely to experience alcohol-related problems, racial discrimination (RD) has been implicated as a risk factor (Hurd, Varner, Caldwell, & Zimmerman, 2014; Lee, Heinze, Neblett, Caldwell, & Zimmerman, 2017). RD, a salient source of stress for AAs, can increase the risk of alcohol-related problems from adolescence to adulthood (Boynton et al., 2014; Gibbons et al., 2014; Lee et al., 2017) and, in the long-run, deteriorate health, contributing to racial health disparities (Williams & Mohammad, 2013). Scholars have also postulated that AAs may be especially vulnerable to RD-related stress during emerging adulthood (Arnett & Brody, 2008; Hurd et al., 2014; Lee et al., 2017), suggesting that RD may more strongly contribute to alcohol-related problems during this life stage. While different types of alcohol-related problems can deteriorate health (e.g., social difficulties), certain alcohol-related problems may be more proximal to physical conditions (e.g., poor sleep, injury, and vomiting). Thus, the health consequences associated with heavy alcohol consumption remains a persistent public health concern. Yet, our understanding of how RD influences the physical consequences of alcohol consumption over time is limited. In light of the suggested associations between RD, psychological distress, and the frequency of alcohol use (Hurd et al., 2014), one might surmise that RD contributes to physical consequences of heavy alcohol consumption by invoking psychological distress.
Religious involvement, discussed as religious participation and commitment to religious beliefs, has been documented as a protective factor against the psychological (Lee, Neblett, & Jackson, 2014) and physiological consequences (Cooper, Thayer, & Waldstein, 2013) of RD for AAs. Contrarily, religious coping, defined as the use of religious beliefs and practices to cope with stressors (Pargament, Magyar-Russellm & Murray-Swank, 2005), has been understudied as a protective factor within the context of RD. Few researchers, however, have examined religious coping as a protective factor against psychological and physiological consequences of RD (Hope, Assari, Cole-Lewis, & Caldwell, 2017). It is, therefore, unclear whether religious coping buffers the association between psychological distress and the physical consequences of alcohol consumption or whether religious coping directly reduces psychological distress linked with RD. One issue has been that researchers have treated religious coping as a summary index which does not account for differences in the religious coping strategy used. It is plausible, for example, that two participants reporting identical level of religious coping may use different religious coping strategies (e.g., prayer, faith-based meaning making). An alternative measurement method is a person-centered approach that groups participants into distinct patterns of religious coping (Pearce, Foster, & Hardie, 2013). Profiles would reflect a subgroup of participants who copes using religion in a similar way.
To address identified gaps in this literature, we examined whether RD increased the physical consequences of heavy alcohol consumption through psychological distress (see Figure 1). We also examined whether profiles higher in religious coping offset the mediational pathway from RD to the physical consequences of alcohol cosnumption through psychological distress.
Figure 1.
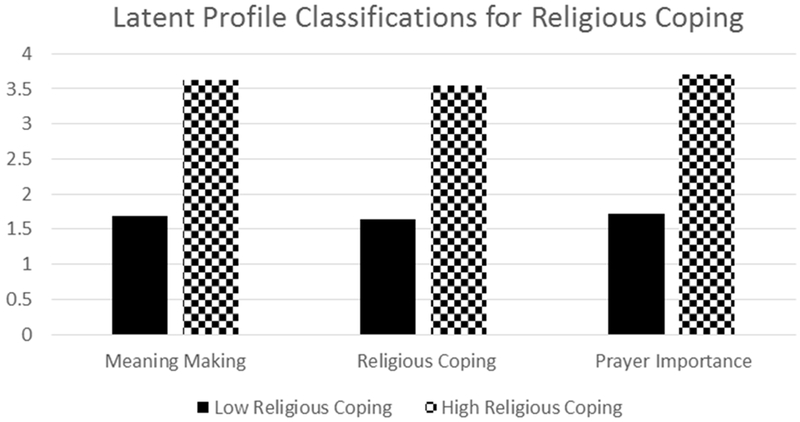
Low and high profiles of religious coping.
Racial Discrimination and Physical Consequences of Alcohol Consumption
RD, defined as “…the unequal treatment of persons or groups on the basis of their race or ethnicity” (Pager & Shepherd, 2008, p. 2), is a prevalent and persistent stressor in the lives of AAs (Williams & Mohammad, 2013). The stressfulness of discrimination cannot be understated, as discrimination has been associated with heightened psychological (Hurd et al., 2014) and physiological (Lee et al., 2017) stress responses among AA emerging adults. Furthermore, physiological stress responses to RD were observed several days after an RD encounter, suggesting the far-reaching mental and physical health implications of RD (Hoggard, Byrd, & Sellers, 2015). To elucidate how RD might influence health, Harrell (2000) noted that routine RD exposure can exhaust an individual’s coping resources, which can contribute to the genesis of psychopathology and negative health behaviors.
In line with Harrell’s conception of racism-related stress, mounting evidence suggests that RD can generate vulnerabilities for alcohol related problems among AA emerging adults (Lee et al., 2017). For instance, those who reported higher levels of RD were more likely to report heavier alcohol use (Hurd et al., 2014; Lee et al., 2017), negative-mood-related drinking (O’Hara, Armeli, Scott, Covault, & Tennen, 2015), and other alcohol-related problems (Boynton et al., 2014). In conjunction with Harrell’s (2000) model, other models such as the tension-reduction model (Conger, 1956) and affect regulation model (Cooper, Frone, Russel, & Mudar, 1995) similarly contend that AAs may consume alcohol in problematic ways to cope (e.g., avoidance coping) with racism-related stress. Heavy, stress-related drinking can consequently generate vulnerabilities for alcohol-related illnesses such as cardiovascular disease (Chamik, Viswanathan, Gedeon, & Bovet, 2018). Thus, it is tenable to earmark RD as a contributor to racial health inequities that can accelerate health deterioration by increasing the risk for physical consequences tied to heavy alcohol consumption for AA emerging adults.
Emerging adulthood, a distinct developmental period between adolescence and adulthood, has been characterized by change and exploration for most people in love, work, identity, and worldviews (Arnett, 2000). For AAs, emerging adulthood is also a key developmental period for examining the role of RD on psychological distress and the physical consequences of alcohol consumption. Researchers have documented racial crossover effects in heavy drinking, indicating that AAs are more likely than White Americans to consume alcohol during emerging adulthood (Watt, 2008). Scholars have acknowledged that AAs may confront more RD as they navigate and complete developmental tasks related to emerging adulthood – such as, pursuing higher education, job training, employment opportunities, and navigating racial identity development - within a social system that espouses interpersonal, institutional, and cultural racism (Arnett & Brody, 2008; Hope, Hoggard, & Thomas, 2015). Consequently, RD may be particularly damaging to the mental health of AA emerging adults and may contribute to racial disparities in alcohol-related problems (Hurd et al., 2014). Further, given the increasing rate of RD during this life stage (Lee et al., 2017), a longitudinal investigation may help us better assess how RD shapes pathways to the physical consequences of alcohol consumption.
Notably, several researchers have found no association between RD and overall alcohol-related problems (Borrell et al., 2007; Broman, 2007; Kwate, Valdimarsdotti, Guevarra, & Bovbjerg, 2003). To explain these counterintuitive findings, some have suggested that the individual’s psychological response to RD (Zapolski et al., 2014) may explain the link between RD and alcohol-related physical health problems.
Psychological Distress as a Mediator
The association between RD and poorer psychological outcomes is well documented among AA emerging adults (Hurd et al., 2014; Lee, Neblett, & Jackson, 2015; Jones, Lee, Gaskin, & Neblett, 2013). Experiencing RD not only heighten stress, but increases symptoms of depression (Banks & Kohn-Wood., 2007), anxiety (Lee et al., 2015), and post-traumatic stress disorder (Polanco-Roman, Danies, & Anglin, 2016). Mental health deterioration induced by RD may, in turn, increase the likelihood of physical alcohol-related problems (Boynton et al., 2014; Gibbons et al., 2014). Coping motives may explain why psychological distress mediates the association between RD and alcohol-related problems (Martin, Tuch, & Roman, 2003). Specifically, RD may exacerbate depressive and anxiety symptoms, which increases alcohol-related problems. Building on this theory, RD-related psychological distress can shape cognitive processes around alcohol consumption such as, increasing alcohol expectancies (Hatzenbuehler, Corbin, & Fromme, 2011) and reducing self-regulatory abilities that play a vital role in responsible drinking (Gibbons et al., 2012). Thus, when taken together, it is plausible for RD to influence the physical consequences of alcohol consumption through psychological distress.
Religious Coping as a Protective Factor
Religious involvement (e.g., service attendance) has been consistently documented as a predictor of less alcohol consumption (Nasim, Belgrave, Jagers, Wilson, & Owens, 2007; Steinman & Zimmerman, 2004) and less alcohol-related problems among AA young adults (Bowie, Ensminger, & Robertson). To a lesser extent, religious coping defined as, “the use of religious beliefs or behaviors to facilitate problem-solving to prevent or alleviate the negative emotional consequences of stressful life circumstances” (Koenig, Pargament, & Nielsen, 1998, p. 513), has been recognized as a predictor of positive health behaviors and outcomes among AA emerging adults (Holt, Clark, Debnam, & Roth, 2014). While studies of religious coping and alcohol consumption are limited among AA emerging adults, AA adults portrayed religion as central to the maintenance of positive health behaviors and metaphorically described their bodies as temples that must be kept clean and pure in a qualitative study (Holt & McClure, 2006). They also discussed faith as crucial to their psychological well-being, mentioning that psychological well-being is vital to maintaining positive health behaviors (Holt & McClure, 2006). Holt et al. (2014) also found that religious coping mediates the association between religious participation and heavy alcohol use among AA adults. Thus, it is plausible that religious coping, for AA emerging adults, may reduce the likelihood of experiencing physical consequences tied to alcohol consumption.
The protective role of religious coping in the context of RD has received limited attention, especially in regards to its role for AA emerging adults. Yet, Hayward and Krause (2015) examined similar links to discrimination among AA adults and suggested that religious coping may mitigate the adverse effects of RD. In addition, religious involvement (e.g., media use, service attendance) was associated with less maladaptive coping behaviors (e.g., self-blame, passive acceptance) for AA and Caribbean Black adults contending with racism-related stress (Hayward & Krause, 2015). Hope et al. (2017) also found that congregational support (i.e., social support from church members) buffered the association between RD and the likelihood of meeting psychiatric diagnostic criteria among Black adolescents. Other researchers investigated optimism (Lee et al., 2014) and religious problem-solving (Lewis-Coles & Constantine, 2006) as methods by which religion might promote adaptive coping methods for racism-related stress. Reflective of this, religious coping may disrupt pathways from racial discrimination to negative psychiatric (Hope et al., 2017) or health behavior outcomes (Holt et al., 2014).
Gleaning from the few studies on the protective characteristics of religious coping on health, two mechanisms may explain how religious coping disrupts the influence of RD on the physical consequences of alcohol consumption. First, religious coping may moderate the influence of RD on the physical consequences of alcohol consumption by reducing psychological distress. Second, religious coping may directly decrease the effect of RD on the physical consequences of alcohol consumption. To understand how religious coping protects AAs at emerging adulthood against RD-related consequences, it is important to test these mechanisms.
Study Aims and Hypotheses
To better understand of how RD shapes the physical consequences of alcohol consumption, the first aim of the study was to test whether psychological distress mediated the longitudinal association between RD and the physical consequences of alcohol consumption. Given the documented mechanism from RD to alcohol consumption through psychological distress (Gibbons et al., 2012; Hurd et al., 2014), we hypothesized that psychological distress would mediate the longitudinal association between RD and the physical consequences of alcohol consumption. The second aim of our study was to test whether high levels of religious coping across three pre-existing indicators (i.e., prayer to cope, religious faith coping, and religious meaning making) could moderate the longitudinal pathway from RD to the physical consequences of alcohol consumption through psychological distress. Consistent with research that delineates the positive influence of religious coping on health behaviors among AAs (Holt et al., 2014), we hypothesized that direct and indirect effects from RD to the physical consequences of alcohol consumption would be mitigated for those in the higher religious coping group.
Method
Participants
Participants included 465 AA emerging adults (49% male) from the Flint Adolescent Study (FAS). The FAS is an ongoing, longitudinal study that examines psychological, social, and biological risk and protective factors associated with school dropout, substance use, and substance-use related problems. In the present study, data were examined at wave 5 (2000-2001; Mage = 20.05), 6 (2001-2002; Mage = 20.98), 7 (2002-2003; Mage = 22.07), and 8 (2003-2004; Mage = 23.06), which reflects emerging adulthood. Data at each measurement period were collected approximately 1 year apart. The original sample consisted of 850 ninth graders (92% response rate) who were identified as at risk for school dropout due to a grade point average of 3.0 or lower at the end of eighth grade. Participants were not eligible to participate in the study if they were diagnosed with an emotional or neurodevelopmental disability. Data were collected annually from 850 adolescents across four main public high schools in Flint, Michigan (979 initial contacts, refusal rate = 13.2%). The original sample was predominantly AA (80.1%) and 16.8% White, 3.1% mixed race, and 50% female. The current study is limited to the AA sample. Of note, 139 of 604 AA participants were missing data on all of the variables from Wave 5 and onwards and were dropped from the current study.
Procedure
After obtaining consent, trained interviewers conducted interviews with the participants in the community setting (e.g., public library). Participants were also asked to complete a paper-and-pencil questionnaire after the interview that consisted of items that evaluated the participant’s sociodemographic background, racial discrimination experiences, psychological distress, alcohol consumption, alcohol-related problems, and other sensitive topics. The university institutional review board approved all study protocols.
Measures
Physical Consequences of Alcohol of Consumption.
The participants’ physical consequences of alcohol consumption was measured at waves 5 to 8 using 7-items from the Physical Consequence subscale of the Drinker Inventory of Consequences (DrInc; Miller, Tonigan, & Longabaugh, 1995). This subscale measures the frequency of the physical consequences of alcohol consumption (e.g., worse sleep quality, vomiting, or getting physically injured while drinking) in the past three months on a 4-point Likert-type scale ranging from “never” to “daily or almost daily.” Items were averaged to approximate the physical consequences of alcohol consumption for each participant at each wave. The physical consequences of alcohol consumption subscale demonstrated satisfactory to good reliability at each wave (i.e., αwave5 = .72, αwave6 = .81, αwave7 = .74, αwave8 = .76).
Racial Discrimination (RD).
Perceived RD was measured using the 18-item Daily Life Experience scale (DLE; Harrell, 1997). The DLE measures the frequency of race-related, interpersonal transactions as experienced in the past year (e.g., “Others reacting to you as if they were afraid or intimidated,” “Not being hired for a job”). Participants responded on 6-point Likert-type scale ranging from 0 (never happened to me) to 5 (once a week or more) and their responses were averaged at each wave. The DLE demonstrated good reliability at each wave (i.e., αwave5 = .94, αwave6 = .94, αwave7 = .95, αwave8 = .95).
Psychological Distress.
On a 12-item scale, participants reported the perceived level of psychological distress (i.e., depressive and anxiety symptoms) on the Brief Symptom Inventory (BSI; Derogatis, 1993). Participants responded on a 5-point Likert-type scale ranging 0 (never) to 4 (very often), and items were averaged at each wave. The BSI demonstrated good reliability (i.e., αwave5 = .88, αwave6 = .89, αwave7 = .89, αwave8 = .88).
Religious Coping.
To measure the use of religious coping methods, we examined three indicators of religious coping: “I use my religious faith to cope,” “I pray when I need help,” and “faith gives meaning to my life.” Participants responded on a Likert-type scale of 0 (not true) to 1 (very true) for each item. Rather than averaging the items, items were used to explore subgroups of individuals that uniquely varied across the indicators of religious coping.
Covariates.
The participant’s sex was assessed at Wave 1 (i.e., 0 = female, 1 = male), while age was assessed at wave 5. Educational attainment was also assessed at Wave 5 and responses ranged from 0 (did not graduate HS) to 7 (attending/completed college or more education). The frequency of alcohol consumption was measured with two items in wave 5. Specifically, we evaluated the participants’ alcohol consumption during the last 12 months and the last 30 days. Both items were measured using a 7-point scale from 0 (none) to 6 (40+ times) and averaged at wave 5. Religious involvement was also measured using two items at Wave 5. The first item measured frequency of attendance at religious services using a 7-point scale ranging from 0 (not at all) to 6 (more than once a week). The second item measured the number of religious activities in which each participant was involved (i.e, ranging from 0 to 3 activities). The two items were averaged to approximate the participant’s level of religious participation. Lastly, the participant’s diet was assessed as a marker for non-substance use related, negative health behavior. In particular, using a single item at wave 5, we evaluated how often the participant consumed foods high on fat (e.g., fried foods) on a weekly basis (i.e., 0 = never, 5 = daily).
Analytic Approach
All statistical analyses were conducted using Mplus, version 8 (Muthén & Muthén, 2017). Descriptive statistics and the correlations between study variables were examined. As an initial step to examining the first study aim, we fit unconditional latent growth models (LGMs) to characterize within- and between-person variation for variables measured longitudinally (i.e., RD, psychological distress, and the physical consequences of alcohol consumption). We compared the model fit between intercept-only (i.e., stable trajectory) and intercept-slope LGMs (i.e., trajectories that change over time). Model fit was considered acceptable if the root mean square error of approximation (RMSEA) was less than .05, comparative fit index (CFI) was greater than 0.90, and if the standardized root mean square residual (SRMR) was less than .05 (Bollen & Curran, 2006). χ2 likelihood ratio tests (LRTs) were conducted to compare model fit between the intercept-slope and the intercept-only models. Due to zero-inflation in the physical consequences of alcohol consumption (>40% of participants at each wave), Tobit analysis and maximum likelihood estimation with robust standard errors were used to generate model parameters. Information criteria (Akaike Information Criterion [AIC] and Bayesian Information Criterion [BIC]) were examined to assess and compare model fit between the intercept-only and the intercept-slope model. A reduction of 10 units in the AIC, BIC, and adjusted BIC for the intercept-slope model indicated an improvement in model fit (Wasserman, 2000).
To evaluate the first aim of the study, we fit a latent growth mediation model (LGMM) as detailed by Cheong and colleagues (2003). Specifically, indirect effects were calculated by multiplying the effects between latent growth terms from RD to psychological distress, and psychological distress to the physical consequences of alcohol consumption (see Cheong et al., 2003 for a detailed review of LGMM). We used Tobit modelling to estimate model parameters as this approach models the probability of reaching floor effects in LGMs that have zero-inflated, continuous outcomes (Wang, Zhang, McArdle, & Salthouse, 2008). We also fit an LGMM not accounting for censoring in the physical consequences of alcohol consumption to derive traditional structural equation model (SEM) model fit indicators (e.g., RMSEA, CFI, SRMR). While MLR accounts for non-normality in the outcome variable, Tobit models, with MLR are preferred as this approach models the probability of reaching floor effects in LGMs that have zero-inflated, continuous outcomes (Wang et al., 2008).
To examine if religious coping moderates paths from RD to the physical consequences of alcohol consumption (aim 2), we first conducted latent profile analyses (LPAs) to identify distinct patterns of religious coping. A finite number of latent profiles were obtained by selecting the number of profiles that demonstrated optimal model fit, as indicated by having a lower AIC, BIC, and adjusted BIC. We also conducted LRTs – that is, Vuong–Lo–Mendell–Rubin likelihood ratio tests (VLMR LRT; Lo, Mendell, & Rubin, 2001), Lo–Mendell–Rubin adjusted likelihood ratio tests (LMR LRT; Lo et al., 2001), and bootstrap likelihood ratio test (B-LRT; Feng & McCulloch, 1996) - to determine significant improvement in model fit between the n versus n − 1 latent profile models. A nonsignificant difference suggested that n − 1 class solution was preferred. Participants’ posterior classification probabilities were used to classify each participant into one of the profile classifications. The participants’ profile classification were used as subgroups to conduct multi-group LGMM.
Results
Descriptive statistics are reported in Table 1. We noted small to modest correlations across covariates, with the largest correlations between repeated measures of RD, psychological distress, and physical consequences of alcohol consumption.
Table 1.
Descriptive Statistics and Intercorrelations Between Study Variables
| Study Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | M (SD) or % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | -- | 50.8% Female | |||||||||||||||||
| 2. Age | −.09* | -- | 20.06 (0.65) | ||||||||||||||||
| 3. Educational Attainment | .05 | −.33** | -- | 4.24 (1.71) | |||||||||||||||
| 4. Average Alcohol Consumption | −.16** | −.07 | .03 | -- | 3.88 (3.35) | ||||||||||||||
| 5. Religious Participation | .01 | −.08T | .24** | −.14** | -- | 2.11 (1.22) | |||||||||||||
| 6. High Fat Diet | .05 | .04 | −.09T | .16** | −.09T | -- | 3.92 (1.11) | ||||||||||||
| 7. RD (W5) | −.09T | −.03 | .01 | .25** | −.06 | −.04 | -- | 0.82 (0.83) | |||||||||||
| 8. RD (W6) | −.18** | .03 | −.07 | .14** | .01 | −.02 | .42** | -- | 0.77 (0.84) | ||||||||||
| 9. RD (W7) | −.22** | −.02 | −.01 | .14** | .04 | .03 | .44** | .45** | -- | 0.76 (0.83) | |||||||||
| 10. RD (W8) | .21** | .04 | −.01 | .19** | .03 | −.01 | .40** | .33** | .52** | -- | 0.81 (0.87) | ||||||||
| 11. Distress (W5) | .13** | .03 | −.18** | .15** | .05 | .10* | .31** | .29** | .16** | .13* | -- | 0.66 (0.61) | |||||||
| 12. Distress (W6) | .11** | .02 | −.10* | .19** | −.07 | .11* | −.24** | .30** | .20** | .23** | .54** | -- | 0.64 (0.62) | ||||||
| 13. Distress (W7) | .17** | .08 | −.14** | .19** | −.11* | .11* | .25** | .23** | .21** | .20** | .48** | .56** | -- | 0.70 (0.62) | |||||
| 14. Distress (W8) | −.08T | −.08 | −.04 | .15** | −.04 | .10* | .21** | .16** | .25** | .25** | .43** | .55** | .56** | -- | 0.66 (0.61) | ||||
| 15. Physical Consequences (W5) | −.21** | .02 | −.14* | 28** | −.03 | .08 | .12T | .14* | .10 | .27** | .15* | .06 | −.01 | .06 | -- | 0.17 (0.24) | |||
| 16. Physical Consequences (W6) | −.22** | −.01 | −.21** | .23** | .04 | .11 | .14* | .22** | .22** | .24** | .21** | .20** | .12 | .18** | .42** | -- | 0.26 (0.40) | ||
| 17. Physical Consequences (W7) | −.18** | .04 | −.14* | .45** | −.04 | .12T | .16* | .13T | .17** | .17* | .17* | .15* | .15* | .20** | .61** | .42** | -- | 0.24 (0.36) | |
| 18. Physical Consequences (W8) | −.15** | −.07 | −.06 | .44** | −.11T | .14* | .16* | .15* | .24** | .26** | .28** | .29** | .14* | .33** | .46** | .65** | .64** | -- | 0.19 (0.32) |
Note.
p < .10.
p < .05.
p < .01.
Unconditional Latent Growth Models
Intercept and slope estimates for unconditional latent growth models for RD, psychological distress, and physical consequences of alcohol consumption across waves 5-8 are reported in Table 2.
Table 2.
Unconditional Latent Growth Models and Likelihood Ratio Tests Between Intercept-Only and Intercept-Slope Models
| χ2 (df) | p-value | RMSEA | 90% C.I. | CFI | SRMR | Intercept | Slope | Var(Intercept) | Var(Slope) | Δχ2 | Δdf | LRT p-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercept-only RD | 22.54 (8) | < .01 | .06 | .02, .08 | .96 | .05 | 0.80** | -- | .31** | -- | -- | -- | -- |
| Intercept and Slope RD | 15.63 (5) | < .01 | .06 | .03, .10 | .97 | .04 | 0.81** | −.01 | .33** | .021* | 6.916 | 3 | .08 |
| Intercept-only Distress | 13.85 (8) | .09 | .04 | .00, .07 | .99 | .04 | .659** | -- | .20** | -- | -- | -- | -- |
| Intercept and Slope Distress | 8.26 (5) | .15 | .03 | .00, .07 | .99 | .03 | .656** | .< .01 | .22** | .010* | 5.968 | 3 | .11 |
| Intercept-only Physical Consequences | -- | -- | -- | -- | -- | -- | .06* | -- | .13** | -- | -- | -- | -- |
| Intercept and Slope Physical Consequences | -- | -- | -- | -- | -- | -- | .13** | −.07** | .04* | .04** | -- | -- | -- |
Note. df = Degrees of Freedom. RMSEA = Root Mean Square Error of Approximation. C.I. = Confidence Interval. CFI = Confirmatory Factor Index. SRMR = Standardized Roomt Mean Residual. Var = Variance. LRT = Likelihood Ratio Test.
Racial Discrimination.
Both the intercept-only and intercept-slope growth models for RD demonstrated acceptable fit, with significant variability in the intercepts for each model. Despite significant variability in the RD slopes across participants, the average slope point estimate did not differ significantly from zero and the LRT. Thus we retained the intercept-only model for future analyses.
Psychological Distress.
The intercept-only and intercept-slope growth models for psychological distress also demonstrated good fit to the data, with significant heterogeneity of intercepts for both models. Like RD, we observed significant variability in distress slopes over time, but the overall average slope was not different from zero. Comparisons to an intercept-only model suggest that allowing slopes to vary did not improve the model fit.
Physical Consequences of Alcohol Consumption.
Results from the physical consequences of alcohol consumption growth model suggests a decrease in consequences from wave 5 to wave 8 (β = −0.07, p < .01). Participants reported significant variability in both intercepts and slopes, suggesting that each could be modeled as outcomes in later analyses.
Aim 1: Psychological Distress as a Mediator using LGMM
We tested our hypothesized conceptual model by regressing the latent intercept and slope of physical consequences of alcohol consumption on the latent intercepts of both psychological distress and RD (see Table 3).
Table 3.
Latent Growth Mediation from RD to the Physical Consequences of Alcohol Use
| b | s.e. | p -value | |
|---|---|---|---|
| Slope of Physical Consequences | |||
| Intercept of Psychological Distress | .10 | .05 | .04 |
| Intercept of Racial Discrimination | −.05 | .04 | .24 |
| Sex | −.02 | .03 | .50 |
| Age | < .01 | .02 | .99 |
| Educational Attainment | .01 | .01 | .15 |
| Average Alcohol Consumption | .02 | < .01 | < .01 |
| Service Attendance | −.01 | .01 | .54 |
| High Fat Diet | < .01 | .01 | .74 |
| Intercept of Physical Consequences | |||
| Intercept of Psychological Distress | .07 | .10 | .45 |
| Intercept of Racial Discrimination | .05 | .09 | .57 |
| Sex | −.13 | .06 | .03 |
| Age | −.02 | .05 | .64 |
| Educational Attainment | −.05 | .02 | < .01 |
| Average Alcohol Consumption | .04 | .01 | < .01 |
| Service Attendance | .02 | .02 | .42 |
| High Fat Diet | .02 | .02 | .39 |
| Intercept of Psychological Distress | |||
| Intercept of Racial Discrimination | .43 | .05 | < .01 |
| Sex | .30 | .04 | < .01 |
| Age | −.01 | .03 | .78 |
| Educational Attainment | −.04 | .01 | .01 |
| Average Alcohol Consumption | .02 | < .01 | < .01 |
| Service Attendance | −.03 | .02 | .07 |
| High Fat Diet | .03 | .02 | .12 |
| Intercept of Racial Discrimination | |||
| Sex | −.27 | .06 | < .01 |
| Age | −.02 | .04 | .70 |
| Educational Attainment | −.01 | .02 | .50 |
| Service Attendance | .02 | .03 | .36 |
| Indirect Effects | |||
| RD → Distress → Intercept for Physical Consequences | .03 | .04 | .45 |
| RD → Distress → Slope for Physical Consequences | .04 | .02 | .04 |
Note. AIC = 7068.31, BIC = 7283.69, aBIC = 7118.66.
Racial Discrimination and Psychological Distress Intercepts.
Sex predicted both RD and psychological distress, with females reporting less RD, but higher levels of psychological distress. Both educational attainment and average alcohol consumption also predicted the intercept of psychological distress, with lower attainment and higher alcohol consumption being associated with more distress. Notably, the intercept of RD was also associated with more psychological distress.
Physical Consequences of Alcohol Consumption.
Participant sex, educational attainment and average alcohol consumption were each associated with baseline levels of the physical consequences of alcohol consumption, such that females, more educated and less alcohol-using participants reporter fewer consequences. The intercept of psychological distress was also associated with the slope of the physical consequences of alcohol consumption such that more distress was associated with more physical consequences over time. The total effects of RD intercepts on physical consequence intercepts and slopes were decomposed into both the direct effects as well as the indirect effects through psychological distress. RD intercepts did not directly predict either intercept or slope of the physical consequences of alcohol consumption. RD did, however, have an indirect influence on physical consequence slopes through psychological distress (βind = 0.04, p < .05), such that higher levels of RD accelerated the positive rate of change in physical consequences through psychological distress.
To approximate model fit using the traditional structural equation modeling fit indicators (e.g., RMSEA, CFI, and TLI) we re-estimated the model using MLR. The model, even after unaccounting for the zero-inflation in the data, fit the data well (i.e., RMSEA = .048, CFI = .90, SRMR = .04).
Aim 2: Protective Patterns of Religious Coping
To examine whether religious coping moderated the mediated association noted above, we first used LPA to determine an appropriate number of patterns of responses that would in turn be used as levels for the multi-group analysis. Results of the LPA are reported in Table 4 and indicate that a two-class solution (high and low religious coping) provided empirically and substantively defensible categories of coping patterns. As shown in Figure 1, participants classified into the high religious coping profile reported higher levels of religious coping across all religious coping indicators than those in the low religious coping group. Although fit indices suggest that a 3-class solution may also fit the data, we opted for a two level coping variable given the non-significant LMR test, the low (n = 18) number of participants classified into the third category, and the relative similarity between the second and third class which may be thought of as two levels of low religious coping.
Table 4.
Latent Profile Analysis Goodness of Fit Indices for Religious Coping
| Class | AIC | BIC | aBIC | Entropy | VLMR LRT | LM Adjusted LRT | B-LRT | Class 1 | Class 2 | Class 3 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Class | 6531.41 | 6572.96 | 6541.22 | -- | -- | -- | -- | 471 | -- | -- |
| 2 Class | 5595.92 | 5662.39 | 5611.61 | 0.93 | .00 | .00 | .00 | 116 | 354 | -- |
| 3 Class | 5107.06 | 5198.47 | 5128.64 | 0.95 | .19 | .20 | .00 | 350 | 102 | 18 |
Note. Missing data handled with Full Information Maximum Likelihood (FIML).
Physical Consequences of Alcohol Consumption by Coping Profile.
Using the newly created religious coping profiles, the multi-group analysis of the LGMM is reported in Table 5. In contrast to the full sample analysis, only average alcohol consumption consistently predicted higher baseline levels and trajectories of the physical consequences of alcohol consumption in the low and high religious coping profiles. Among high religious coping participants, higher education was also associated with lower baseline levels of physical consequences.
Table 5.
Latent Growth Mediation Across Latent Profiles of Religious Coping
| Low Religious Coping | High Religious Coping | |||||
|---|---|---|---|---|---|---|
| b | s.e. | p | b | s.e. | p | |
| Slope of PCs | ||||||
| Intercept of Psychological Distress | .15 | .06 | .02 | .09 | .07 | .17 |
| Intercept of Racial Discrimination | −.09 | .04 | .04 | −.03 | .05 | .56 |
| Sex | −.03 | .05 | .53 | −.01 | .04 | .89 |
| Age | −.07 | .05 | .23 | .02 | .02 | .37 |
| Educational Attainment | −.01 | .02 | .68 | .01 | .01 | .12 |
| Average Alcohol Consumption | .03 | .01 | < .01 | .01 | < .01 | < .01 |
| Religious Service Attendance | −.01 | .03 | .87 | −.02 | .01 | .06 |
| High Fat Diet | −.03 | .02 | .28 | .01 | .01 | .23 |
| Intercept of PCs | ||||||
| Intercept of Psychological Distress | .01 | .14 | .97 | .13 | .14 | .34 |
| Intercept of Racial Discrimination | .18 | .10 | .07 | −.05 | .10 | .61 |
| Sex | −.09 | .12 | .41 | −.14 | .08 | .09 |
| Age | .13 | .12 | .25 | −.04 | .04 | .39 |
| Educational Attainment | −.02 | .03 | .53 | −.04 | .02 | .03 |
| Average Alcohol Consumption | .03 | .01 | .03 | .04 | .01 | < .01 |
| Religious Service Attendance | −.03 | .06 | .61 | .04 | .02 | .08 |
| High Fat Diet | .03 | .05 | .51 | .01 | .02 | .70 |
| Intercept of Psychological Distress | ||||||
| Intercept of Racial Discrimination | .33 | .09 | < .01 | .44 | .06 | < .01 |
| Sex | .30 | .09 | < .01 | .29 | .05 | < .01 |
| Age | −.02 | .08 | .82 | −.01 | .04 | .83 |
| Educational Attainment | −.05 | .03 | .09 | −.04 | .01 | .01 |
| Average Alcohol Consumption | .02 | .01 | .09 | .02 | .01 | < .01 |
| Religious Service Attendance | −.07 | .05 | .20 | −.03 | .02 | .17 |
| Unhealthy Diet | .03 | .05 | .46 | .03 | .02 | .17 |
| Intercept of Racial Discrimination | ||||||
| Sex | −.24 | .16 | .13 | −.26 | .07 | < .01 |
| Age | −.13 | .11 | .23 | .01 | .05 | .91 |
| Educational Attainment | −.05 | .05 | .26 | −.01 | .02 | .83 |
| Religious Service Attendance | .06 | .10 | .51 | .03 | .03 | .27 |
| Indirect Effects | b | s.e. | p | b | s.e. | p |
| RD → Distress → Intercept of PCs | .00 | .04 | .97 | .06 | .06 | .35 |
| RD → Distress → Slope of PCs | .05 | .02 | < .05 | .04 | .03 | .18 |
Note. When we unaccounted for zero-inflation, the model fit the data well: RMSEA = .06, CFI = .90, and TFI = .91. PCs = physical consequences.
The multi-group analyses revealed notable differences in both the direct and indirect effects of RD on physical consequences of alcohol consumption. For those reporting low levels of religious coping, we found direct effects of both psychological distress and RD on baseline levels of the physical consequences of alcohol consumption (i.e., intercepts). These direct effects were not significant for members of the high religious coping profile. Moreover, the indirect effect of RD on the physical consequences of alcohol consumption trajectories through psychological distress held for members of the low religious coping profile (βind.LowCoping = 0.05, p < .05), but not for the high religious coping profile. That is, participants with higher levels of religious coping did not experience the same increase in the trajectory of the physical consequences of alcohol consumption as a result of higher psychological distress. The results suggest that members of the low religious coping profile were at higher direct and indirect risk of the physical consequences of alcohol consumption as a result of RD than those in the high religious profile.
Like Aim 1, we estimated our LGMM using MLR to obtain the traditional model fit indicators used in SEM. Even after unaccounting for zero-inflation in the physical consequences of alcohol consumption, the multi-group LGMM model fit the data well (i.e., RMSEA = .05, CFI = .90, SRMR = .05).
Discussion
Consistent with Clark and colleagues (1999), our results reinforce the conception of psychological well-being as intermediate to the connection between RD and negative health behaviors. In particular, we found that RD invoked higher levels of psychological distress, which increased the rate of change in the physical consequences of alcohol consumption throughout emerging adulthood. Our results build on prior studies of RD, psychological distress, and alcohol-related problems in two important ways. First, psychological distress fully mediated the longitudinal association between RD and the physical consequences of alcohol consumption, suggesting that the psychological consequences of RD may contribute strongly to negative health behaviors among AA emerging adults (see Gibbons, 2016). Specifically, using alcohol in health compromising ways may accelerate the deterioration of health and, consequently, contribute to the racial disparities in the patterning of health (Williams & Mohammed, 2013). Second, instead of broadly assessing alcohol-related problems (e.g., social difficulties, socio-economic consequences of alcohol consumption), we examined an indicator of alcohol-related problems that was proximal to health (i.e., the physical consequences of alcohol consumption). By doing so, our study is one of the first to suggest that RD can accelerate a pattern of drinking that directly implicates physiological functioning (e.g., poor sleep, injury, and illness). Together, as elucidated by Clark and colleagues’ (1999) racism and health model, the adverse psychological influences of RD may increase risk for health deteriorating behaviors, which, in turn, to contribute to racial health disparities.
Consistent with studies that have documented religious coping as a health promotive factor for AAs (e.g., Holt et al., 2014), our findings frame religious coping as protective against the physical consequences of alcohol consumption in the context of RD. Specifically, RD predicted higher levels of psychological distress in the low and high religious coping profiles, while psychological distress accelerated the increase of the physical consequences of alcohol consumption in only the low religious coping profile. Our results suggest that religious coping can, within the context of racism-related psychological distress, reduce the likelihood of drinking in a health deteriorating manner. Scholars, such as Holt and colleagues (2014), have argued that religiously involved AAs burdened by stress (e.g., illness, financial stress) may use religious coping, rather than stress-related drinking, to reduce distress. Thus, religious coping may be an important health promotive activity for religiously involved AAs contending with RD.
The high religious coping profile endorsed a higher level of psychological distress than individuals in the low religious coping profile. Although religious involvement can buffer the link between RD and mental health outcomes (e.g., Hope et al., 2017), higher levels of religious coping may signal higher levels of psychological distress. That is, while it is plausible that religious coping promotes psychological adjustment in the context of stress (e.g., Ano & Vasconcelles, 2005), it is also plausible that individuals who routinely use religious coping do so because of heightened psychological distress. Furthermore, the type of religious coping used (i.e., positive versus negative religious coping) may explain why the association between RD and psychological distress was stronger among those in the high religious coping profile. Not all forms of religious coping are positive or yield positive effects for individuals experiencing stress related to racial discrimination. Holt and colleagues (2014) posited that, among AAs, positive religious coping (e.g., collaborating with the divine to cope with stress) promoted positive health behaviors, whereas negative religious coping (e.g., viewing stressors as divine punishment) promoted negative health behaviors. Embracing this line of thinking, RD may have been more strongly linked with psychological distress in the high religious coping profile if a proportion of members in this profile employed negative religious coping methods.
Despite the interesting findings, several limitations restrict the generalization of our study findings. First, our measurement of religious coping was limited to three single-item indicators, limiting the number of profiles we can extract. Although we detected effects with three indicators of religious coping, religious coping offers diverse methods of coping across various situations (see Pargament, Koenig, & Perez, 2000). Second, the Flint Adolescent Study did not contain information about the religious affiliation of each participant. Given that patterns of religious coping vary across religious affiliations (e.g., Aflakseir & Coleman, 2011), it is necessary to examine how AAs from different religious affiliations (with varying degrees of religious commitment) rely on religion cope to offset and counteract the pernicious effects of racism. Third, our sample included AA emerging adults residing in a predominantly AA city in the Midwest. As neighborhood-level characteristics (e.g., racial composition) shape RD experience (English, Lambert, Evans, & Zonderman, 2014) and the physical availability of alcohol (LaVeist & Wallace, 2000), it is important to test whether our results are generalizable across multiple contexts.
Fourth, not all African Americans report religious involvement or use religious coping. For example, non-religiously involved AAs use non-religious forms of adaptive coping methods (e.g., general social support) to regulate RD-related stress (Brondolo, Brady, Pencille, Beaty, & Contrada, 2009). Although our study uniquely contributes to the understanding of religious coping as a protective factor against the adverse effects of RD, future studies that investigate religious and non-religious coping responses to racism-related stress among AA emerging adults is necessary regardless of religious affiliation and involvement. Moreover, in light of the documented link between religious social support and health (Hope et al., 2017), it is possible that this type of social support is a confounding factor in our results. To this end, future investigations should control for religious social support when investigating the protective role of religious coping. Lastly, RD is also a multidimensional construct that occurs in various contexts (e.g., interpersonal transactions, institutional; Williams & Mohammed, 2013). To build upon our findings, future work should examine how patterns of RD experience across different contexts uniquely shape pathways into negative health behaviors.
Conclusion
Our study contributes to the research on RD and health behaviors in two important ways. First, although researchers have examined longitudinal mechanisms bridging RD to alcohol consumption (Hurd et al., 2014), our study is one of the first to examine a longitudinal pathway from RD to the physical consequences of alcohol consumption. Guided by Harrell’s conception of racism-related stress, our findings mark psychological distress and the physical consequences of alcohol consumption as potentially important pathogenic processes that link racism to health. Second, our results suggest that religious coping can protect the health of AAs by mitigating the association between distress and the physical consequences of alcohol consumption in the context of RD. That is, religious coping offers another way of coping with RD-related distress to disrupt the psychological pathway from RD to the physical consequences of alcohol consumption. Findings from our study highlight the need for future investigations to examine if religious coping can disrupt other novel psychological (e.g., optimism) and social (e.g., feeling isolated) pathways connecting racism to alcohol misuse.
The successful transition from high school to emerging of adulthood is jeopardized with persistent exposure to RD experiences linked to psychological distress for AA emerging adults. These experiences exacerbate the negative physical consequences of alcohol consumption at a time when they should be achieving the developmental tasks of young adulthood. Our results suggest this negative chain of experiences related to RD is mitigated for emerging adults who engage in religious coping. Finding ways to break this chain of negative influence requires intervention at multiple levels of influence that include changes at the societal and interpersonal levels. For example, at the individual-level, the development and implementation of alcohol misuse prevention programs for AAs may include components that directly addresses the psychological toll of RD (Unger, 2017). Further, alcohol misuse prevention programs that incorporate religious coping strategies may be particularly beneficial when working with religiously involved AAs who are contending with racism-related stress.
Acknowledgments
This research was supported by a grant from the NIH (T32 HD 79350-2) for the first author (D.B.L.).
References
- Aflakseir A, & Coleman PG (2011). Initial development of the Iranian religious coping scale. Journal of Muslim Mental Health,6(1), 44–61. doi: 10.3998/jmmh.10381607.0006.104 [DOI] [Google Scholar]
- Agrawal A, Grant JD, Haber JR, Madden PA, Heath AC, Bucholz KK, & Sartor CE (2017). Differences between White and Black young women in the relationship between religious service attendance and alcohol involvement. The American journal on addictions, 26(5), 437–445. doi: 10.1111/ajad.12462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ano GG, & Vasconcelles EB (2005). Religious coping and psychological adjustment to stress: A meta-analysis. Journal of clinical psychology, 61(4), 461–480. doi: 10.1002/jclp.20049 [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American psychologist, 55(5), 469–480. doi: 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Arnett JJ, & Brody GH (2008). A fraught passage: The identity challenges of African American emerging adults. Human Development 51(5-6), 291–293. doi: 10.1159/000170891 [DOI] [Google Scholar]
- Banks KH, & Kohn-Wood LP (2007). The influence of racial identity profiles on the relationship between racial discrimination and depressive symptoms. Journal of Black Psychology, 33(3), 331–354. doi: 10.1177/0095798407302540 [DOI] [Google Scholar]
- Bollen KA, & Curran PJ (2006). Latent curve models: A structural equation perspective. John Wiley & Sons. [Google Scholar]
- Borrell LN, Jacobs DR Jr, Williams DR, Pletcher MJ, Houston TK, & Kiefe CI (2007). Self-reported racial discrimination and substance use in the Coronary Artery Risk Development in Adults Study. American Journal of Epidemiology, 166(9), 1068–1079. doi: 10.1093/aje/kwm180 [DOI] [PubMed] [Google Scholar]
- Bowie JV, Ensminger ME, & Robertson JA (2006). Alcohol-use problems in young black adults: effects of religiosity, social resources, and mental health. Journal of Studies on Alcohol, 67(1), 44–53. doi: 10.15288/jsa.2006.67.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boynton MH, O’Hara RE, Covault J, Scott D, & Tennen H (2014). A mediational model of racial discrimination and alcohol-related problems among African American college students. Journal of studies on alcohol and drugs, 75(2), 228–234. doi: 10.15288/jsad.2014.75.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broman C (2007). Perceived discrimination and alcohol use among Black and White college students. Journal of Alcohol and Drug Education, 51(1), 8–16. Retrieved from https://search-proquest-com.proxy.lib.umich.edu/docview/217437427?pq-origsite=360link [Google Scholar]
- Brondolo E, Ver Halen NB, Pencille M, Beatty D, & Contrada RJ (2009). Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of behavioral medicine, 32(1), 64–88. doi: 10.1007/s10865-008-9193-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TL, Parks GS, Zimmerman RS, & Phillips CM (2001). The role of religion in predicting adolescent alcohol use and problem drinking. Journal of Studies on Alcohol, 62(5), 696–705. doi: 10.15288/jsa.2001.62.696 [DOI] [PubMed] [Google Scholar]
- Chamik T, Viswanathan B, Gedeon J, & Bovet P (2018). Associations between psychological stress and smoking, drinking, obesity, and high blood pressure in an upper middle-income country in the African region. Stress and Health, 34(1), 93–101. doi: 10.1002/smi.2766 [DOI] [PubMed] [Google Scholar]
- Cheong J, MacKinnon DP, & Khoo ST (2003). Investigation of mediational processes using parallel process latent growth curve modeling. Structural Equation Modeling, 10(2), 238–262. doi: 10.1207/S15328007SEM1002_5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, & Williams DR (1999). Racism as a stressor for African Americans: A biopsychosocial model. American psychologist, 54(10), 805–816. doi: 10.1037/0003-066X.54.10.805 [DOI] [PubMed] [Google Scholar]
- Conger JJ (1956). Reinforcement theory and the dynamics of alcoholism. Quarterly journal of studies on alcohol, 296–305. Retrieved from https://www-ncbi-nlm-nih-gov.proxy.lib.umich.edu/pubmed/13336262 [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, & Mudar P (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of personality and social psychology, 69(5), 990–1005. Retrieved from https://www-ncbi-nlm-nih-gov.proxy.lib.umich.edu/pubmed/7473043 [DOI] [PubMed] [Google Scholar]
- Cooper DC, Thayer JF, & Waldstein SR (2013). Coping with racism: the impact of prayer on cardiovascular reactivity and post-stress recovery in African American women. Annals of Behavioral Medicine, 47(2), 218–230. doi: 10.1007/s12160-013-9540-4 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Spencer PM (1982). Administration and procedures: BSI manual I. Baltimore: Clinical Psychometric Research. [Google Scholar]
- Feng ZD, & McCulloch CE (1996). Using bootstrap likelihood ratios in finite mixture models. Journal of the Royal Statistical Society. Series B (Methodological), 609–617. Retrieved from http://www.jstor.org.proxy.lib.umich.edu/stable/2345897 [Google Scholar]
- Galvan FH, & Ceatano R (2003). Alcohol use and related problems among ethnic minorities in the United States. Alcohol Research, 27(1), 87–94. Retrieved from https://search-proquest-com.proxy.lib.umich.edu/docview/222391730?pq-origsite=360link&accountid=14667 [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Kingsbury JH, Weng CY, Gerrard M, Cutrona C, Wills TA, & Stock M (2014). Effects of perceived racial discrimination on health status and health behavior: A differential mediation hypothesis. Health Psychology, 33(1), 11–19. doi: 10.1037/a0033857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, O’hara RE, Stock ML, Gerrard M, Weng CY, & Wills TA (2012). The erosive effects of racism: Reduced self-control mediates the relation between perceived racial discrimination and substance use in African American adolescents. Journal of personality and social psychology, 102(5), 1089–1104. doi: 10.1037/a0027404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP (1997). The Racism and Life Experience Scales (RaLES): Self-administration version. Unpublished manuscript.
- Harrell SP (2000). A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American journal of Orthopsychiatry, 70(1), 42–57. Retrieved from https://www-ncbi-nlm-nih-gov.proxy.lib.umich.edu/pubmed/10702849 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, & Fromme K (2011). Discrimination and alcohol-related problems among college students: A prospective examination of mediating effects. Drug & Alcohol Dependence, 115(3), 213–220. doi: 10.1016/j.drugalcdep.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward RD, & Krause N (2015). Religion and strategies for coping with racial discrimination among African Americans and Caribbean Blacks. International Journal of Stress Management, 22(1), 70–91. doi: 10.1037/a0038637 [DOI] [Google Scholar]
- Hoggard LS, Byrd CM, & Sellers RM (2015). The lagged effects of racial discrimination on depressive symptomology and interactions with racial identity. Journal of counseling psychology, 62(2), 216–225. doi: 10.1037/cou0000069 [DOI] [PubMed] [Google Scholar]
- Holt CL, Clark EM, Debnam KJ, & Roth DL (2014). Religion and health in African Americans: The role of religious coping. American journal of health behavior, 38(2), 190–199. doi: 10.5993/AJHB.38.2.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, & McClure SM (2006). Perceptions of the religion-health connection among African American church members. Qualitative health research, 16(2), 268–281. doi: 10.1177/1049732305275634 [DOI] [PubMed] [Google Scholar]
- Hope EC, Hoggard LS, & Thomas A (2015). Emerging into adulthood in the face of racial discrimination: Physiological, psychological, and sociopolitical consequences for african american youth. Translational Issues in Psychological Science, 1(4), 342–351. doi: 10.1037/tps0000041 [DOI] [Google Scholar]
- Hope MO, Assari S, Cole-Lewis YC, & Caldwell CH (2017). Religious social support, discrimination, and psychiatric disorders among Black adolescents. Race and Social Problems, 9(2), 102–114. doi: 10.1007/s12552-016-9192-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurd NM, Varner FA, Caldwell CH, & Zimmerman MA (2014). Does perceived racial discrimination predict changes in psychological distress and substance use over time? An examination among Black emerging adults. Developmental psychology, 50(7), 1910–1918. doi: 10.1037/a0036438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, Pargament KI, & Nielsen J (1998). Religious coping and health status in medically ill hospitalized older adults. The Journal of nervous and mental disease, 186(9), 513–521. Retrieved from https://www-ncbi-nlm-nih-gov.proxy.lib.umich.edu/pubmed/9741556 [DOI] [PubMed] [Google Scholar]
- Kwate NOA, Valdimarsdottir HB, Guevarra JS, & Bovbjerg DH (2003). Experiences of racist events are associated with negative health consequences for African American women. Journal of the National Medical Association, 95(6), 450–460. Retrieved from https://www-ncbi-nlm-nih-gov.proxy.lib.umich.edu/pmc/articles/PMC2594553/ [PMC free article] [PubMed] [Google Scholar]
- Lee C, Mun EY, White HR, & Simon P (2010). Substance use trajectories of black and white young men from adolescence to emerging adulthood: A two-part growth curve analysis. Journal of ethnicity in substance abuse, 9(4), 301–319. doi: 10.1080/15332640.2010.522898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DB, Heinze JE, Neblett EW, Caldwell CH, & Zimmerman MA (2017). Trajectories of Racial Discrimination That Predict Problematic Alcohol Use Among African American Emerging Adults. Emerging Adulthood, 1–11. doi: 10.1177/2167696817739022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DB, Neblett EW Jr, & Jackson V (2015). The role of optimism and religious involvement in the association between race-related stress and anxiety symptomatology. Journal of Black Psychology, 41(3), 221–246. doi: 10.1177/0095798414522297 [DOI] [Google Scholar]
- Lee DB, Peckins MK, Heinze JE, Miller AL, Assari S, & Zimmerman MA (2017). Psychological pathways from racial discrimination to cortisol in African American males and females. Journal of behavioral medicine, 41(2), 1–13. doi: 10.1007/s10865-017-9887-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Coles MAEL, & Constantine MG (2006). Racism-related stress, Africultural coping, and religious problem-solving among African Americans. Cultural Diversity and Ethnic Minority Psychology, 12(3), 433–443. doi: 10.1037/1099-9809.12.3.433 [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. Retrieved from http://www.jstor.org.proxy.lib.umich.edu/stable/2673445 [Google Scholar]
- Martin JK, Tuch SA, & Roman PM (2003). Problem drinking patterns among African Americans: the impacts of reports of discrimination, perceptions of prejudice, and” risky” coping strategies. Journal of health and social behavior, 408–425. doi: 10.2307/1519787 [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, & Longabaugh R (1995). The drinker inventory of consequences (DrInC). Project MATCH monograph series, 4 [Google Scholar]
- Mulia N, & Zemore SE (2012). Social adversity, stress, and alcohol problems: are racial/ethnic minorities and the poor more vulnerable?. Journal of Studies on Alcohol and Drugs, 73(4), 570–580. doi: 10.15288/jsad.2012.73.570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998-2017). Mplus User’s Guide. Eighth Edition Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Meyers JL, Brown Q, Grant BF, & Hasin D (2017). Religiosity, race/ethnicity, and alcohol use behaviors in the United States. Psychological medicine, 47(1), 103–114. doi: 10.1017/S0033291716001975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’hara RE, Boynton MH, Scott DM, Armeli S, Tennen H, Williams C, & Covault J (2014). Drinking to cope among African American college students: An assessment of episode-specific motives. Psychology of addictive behaviors, 28(3), 671–681. doi: 10.1037/a0036303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pager D, & Shepherd H (2008). The sociology of discrimination: Racial discrimination in employment, housing, credit, and consumer markets. Annu. Rev. Sociol, 34, 181–209. doi: 10.1146/annurev.soc.33.040406.131740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pargament KI, Koenig HG, & Perez LM (2000). The many methods of religious coping: Development and initial validation of the RCOPE. Journal of clinical psychology, 56(4), 519–543. doi: [DOI] [PubMed] [Google Scholar]
- Pearce LD, Foster EM, & Hardie JH (2013). A person-centered examination of adolescent religiosity using latent class analysis. Journal for the scientific study of religion, 52(1), 57–79. doi: 10.1111/jssr.12001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanco-Roman L, Danies A, & Anglin DM (2016). Racial discrimination as race-based trauma, coping strategies, and dissociative symptoms among emerging adults. Psychological Trauma: Theory, Research, Practice, and Policy, 8(5), 609–617. doi: 10.1037/tra0000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-44, HHS Publication No. (SMA) 12-4713 Rockville, MD: Substance Abuse and Mental Health Services Administration, 2012. [Google Scholar]
- Unger JB (2015). Preventing substance use and misuse among racial and ethnic minority adolescents: Why are we not addressing discrimination in prevention programs? Substance use & misuse, 50(8-9), 952–955. doi: 10.3109/10826084.2015.1010903 [DOI] [PubMed] [Google Scholar]
- Wang L, Zhang Z, McArdle JJ, & Salthouse TA (2008). Investigating ceiling effects in longitudinal data analysis. Multivariate behavioral research, 43(3), 476–496. doi: 10.1080/00273170802285941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman L (2000). Bayesian model selection and model averaging. Journal of mathematical psychology, 44(1), 92–107. doi: 10.1006/jmps.1999.1278 [DOI] [PubMed] [Google Scholar]
- Watt TT (2008). The race/ethnic age crossover effect in drug use and heavy drinking. Journal of Ethnicity in Substance Abuse, 7(1), 93–114. doi: 10.1080/15332640802083303 [DOI] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and health I: Pathways and scientific evidence. American Behavioral Scientist, 57(8), 1152–1173. doi: 10.1177/0002764213487340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski TC, Pedersen SL, McCarthy DM, & Smith GT (2014). Less drinking, yet more problems: understanding African American drinking and related problems. Psychological bulletin, 140(1), 188–223. doi: 10.1037/a0032113 [DOI] [PMC free article] [PubMed] [Google Scholar]


