Abstract
Purpose
The aims of this study were first, to compare panoramic radiography with cone-beam computed tomography (CBCT) for evaluating topographic relationships, such as the classification of maxillary posterior teeth and their distance to the maxillary sinus floor; and second, to determine the relationship between maxillary sinus pathology and the presence of apical lesions.
Materials and Methods
In total, 285 paired CBCT and panoramic radiography records of patients (570 maxillary sinuses) were retrospectively analyzed. Both imaging modalities were used to determine the topographic relationship of the maxillary posterior teeth to the sinus floor. Mucosal thickening >2 mm was considered a pathological state. Data were analyzed using the chi-square, Wilcoxon, and Mann-Whitney U tests. Odds ratios (ORs) and confidence intervals (CIs) were calculated.
Results
The closest vertical distance measurements made between posterior maxillary teeth roots and the maxillary sinus on panoramic radiography and CBCT scans showed statistically significant differences from each other (P<0.05). Compared to panoramic radiography, CBCT showed higher mean values for the distance between the maxillary sinus floor and maxillary posterior teeth roots. The CBCT images showed that at least 1 apical lesion adjacent to the right maxillary sinus increased the risk of maxillary sinus pathology by 2.37 times (OR, 2.37; 95% CI, 1.58-3.55, P<0.05).
Conclusion
Panoramic radiography might lead to unreliable diagnoses when evaluating the distance between the sinus floor and posterior roots of the maxillary teeth. Periapical lesions anatomically associated with maxillary sinuses were a risk factor for sinus mucosal thickening.
Keywords: Cone-Beam Computed Tomography; Radiography, Panoramic; Paranasal Sinus Disease
Introduction
Inflammation of the maxillary sinuses, also known as maxillary sinusitis, may occur due to viral, bacterial, and fungal agents. Approximately 10%–12% of cases of maxillary sinusitis are reported to be caused by odontogenic infections in the roots of posterior teeth that are adjacent to the maxillary sinus space. As a result of the transport of microorganisms from infected periapical tissues, acute or chronic sinusitis can develop.1 It has been reported that apical periodontitis,2 periodontal diseases,3 implant therapy,4 and tooth extraction5 increase the risk of maxillary sinusitis. Apical and marginal periodontitis account for 83% of all dental causes of maxillary sinusitis.2
A normal sinus is not observed on a radiograph unless there is an increase in mucosal thickness or irritation by an allergic or infectious agent.1 Mild maxillary sinus mucosal thickening is a normal finding in asymptomatic individuals.6 In fact, maxillary sinusitis has been classified as mucosal thickening exceeding 2 mm in most circumstances.7 Based on this, it has been suggested that maxillary sinus mucosal thickening over 2 mm should be considered as indicative of a pathological condition.1,8
Panoramic radiography,9 which is the modality most commonly used to evaluate the relationship of the maxillary posterior teeth roots to the maxillary sinus, allows imaging of anatomical structures at a low cost and a relatively low radiation dose. However, panoramic radiography has disadvantages, such as the superposition of anatomical structures, unwanted magnification, and the lack of cross-sectional analysis.10 For this reason, panoramic radiographs can be inadequate for investigating the relationships between the upper posterior teeth and the maxillary sinus.11 Ever since it was first introduced in 1998,12 cone-beam computed tomography (CBCT) has become popular in diagnosis and treatment planning in dentistry.13 Although computed tomography (CT)14,15 is considered the gold standard for displaying the paranasal sinuses, CBCT is generally preferred for clinical applications because of its lower radiation dose,16 higher resolution, and lower scanning time.1 It allows 3-dimensional cross-sectional imaging, which eliminates distortion and superposition.17
Maxillary posterior teeth roots can cause oroantral communications due to their proximity to the sinus floor.18 For posterior maxillary pre-implant surgical procedures or tooth extractions, most dentists use panoramic radiographs to evaluate the distance between the dental root apex and the maxillary sinus. It is important for clinicians to be able to connect the results of 2-dimensional images to the reality of the situation. The first aim of this study was to compare panoramic radiography with CBCT for evaluating topographic relationships, such as the classification of maxillary posterior teeth and their distance to the maxillary sinus floor, and the second was to determine the relationship between maxillary sinus pathology and the presence of apical lesions.
Materials and Methods
Sample and Study Design
In our study, 285 patients' digital records (paired panoramic radiographs and CBCT scans) were examined retrospectively. Patients who had both CBCT scans and panoramic radiographs taken for various reasons, such as implant surgery, third molar surgery, and orthodontic treatment, were included in the study. The patients were 18–68 years of age (mean, 28.58 years), 38% (n=111) were male, and 61.1% (n=174) were female. The study protocol was approved by the Research Ethics Committee of Necmettin Erbakan University, Faculty of Dentistry (no. 2017/012). All procedures were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Individuals who had second premolar, first molar, and second molar teeth in the right and left maxillary posterior region were included in the study. Individuals younger than 18 years of age with maxillary posterior teeth with open apices, individuals with maxillary implants in the posterior region, and individuals lacking any of the teeth examined in the study were not included. Since periodontal diseases can cause maxillary sinus pathology,3 teeth with alveolar bone loss of more than half of the bone support were also excluded.
Image Acquisition
In this retrospective study, the records were analyzed of patients whose radiographs were taken according to the department's routine protocol, which ensured the elimination of distortions and patient positioning errors by stabilizing patients' heads while keeping their Frankfurt horizontal plane parallel to the floor. Additionally, all panoramic radiographs were taken by the same technician, using the same panoramic device (2D Veraviewpocs, J Morita, MFG Co., Kyoto, Japan). The included scans were taken according to the manufacturer's recommendations, which included specific exposure parameters according to the patients' head size and age. All of the CBCT images used in the study were taken in a sitting position using a Morita 3D Accuitomo 170 device (J Morita MFG Corp., Kyoto, Japan) operated at 90 kVp and 5 mA, with 17.5 seconds of rotation time, 0.25-mm voxels, and a 100-mm field of view, according to the manufacturer's recommended protocol. All observations were made by a single maxillofacial radiologist with 7 years of experience in maxillofacial radiology, using i-Dixel version 2.0 (manufactured by J Morita, MFG Corp.) on a 2.66 GHz Intel Xeon PC with 3.25 GB of RAM, the Windows XP Professional operating system, and a 27-inch flat panel color display with a resolution of 2,560×1,600 pixels (U2711HTM; Dell, Round Rock, TX, USA).
Radiographic Assessment
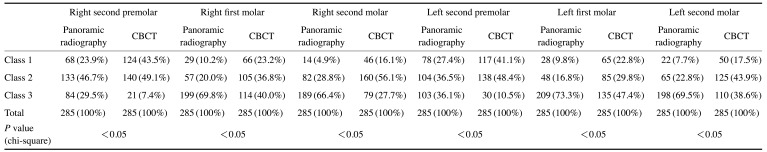
A total of 1,710 teeth (570 premolars and 1,140 molars) were grouped according to endodontic treatment status and the presence of periapical lesions, as shown in Figure 1. The presence or absence of periapical lesions was determined separately on the panoramic radiographs and CBCT images, by the same observer. A periapical lesion was considered to be present when the lamina dura was invisible and there was a periapical radiolucency around the root apex indicating bone destruction.19 The following groups were defined: group 1, non-endodontically treated teeth without an apical lesion; group 2, non-endodontically treated teeth with an apical lesion; group 3, endodontically treated teeth without an apical lesion; and group 4, endodontically treated teeth with an apical lesion (Fig. 1).
Fig. 1. Grouping of teeth on sagittal cone-beam computed tomography slices by apical condition. A, B, C, and D represent groups 1, 2, 3, and 4, respectively.
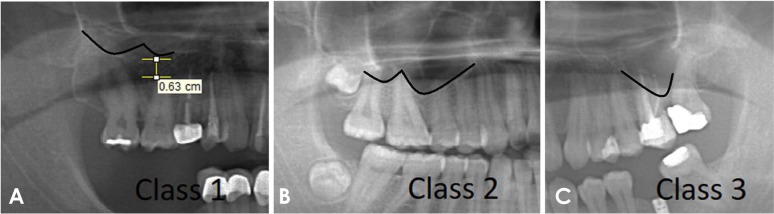
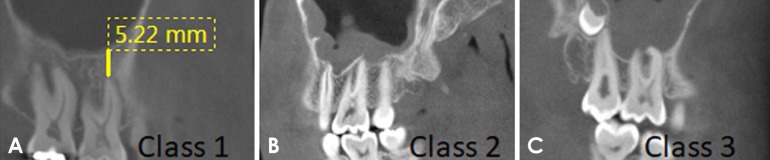
A total of 570 maxillary sinus images of 285 patients were evaluated to identify maxillary sinus pathology (maxillary sinus mucosal thickening >2 mm) in both the right and left sinuses (Fig. 2). The smallest vertical distance of the tooth roots to the maxillary sinuses was measured on panoramic radiography and CBCT scans. To ensure standardization of the measurements on CBCT, the software was oriented parallel to the occlusal surface and sagittal slices were used for distance measurements. Based on the study of Oberli et al.,20 the topographic relationships between roots and the adjacent maxillary sinuses were categorized in both panoramic images (Fig. 3) and sagittal CBCT slices (Fig. 4) as follows: class 1, the presence of distance between the root tip and the sinus floor; class 2, contact between the root tip and the sinus floor without the root entering the sinus; and class 3, presence of the root tip inside the sinus.
Fig. 2. Measurement of maxillary sinus mucosal thickening on a sagittal cone-beam computed tomography slice.

Fig. 3. Classification of the topographic relationships of maxillary first molars with the maxillary sinus on panoramic radiographs. A, B, and C represent classes 1, 2, and 3, respectively.
Fig. 4. Classification of the topographic relationships of maxillary first molars with the maxillary sinus on sagittal cone-beam computed tomography slices. A, B, and C represent classes 1, 2, and 3, respectively. CBCT, cone-beam computed tomography.
Statistical Analysis
All statistical analyses were performed using SPSS version 21 (IBM Corp., Armonk, NY, USA). Mean values and standard deviations were calculated as descriptive statistics. The measurements were repeated in 50 patients twice by 1 observer. The intraobserver correlation coefficient was calculated. The conformity of continuous numerical variables to the normal distribution was analyzed by the Shapiro-Wilk test. A normal distribution was not found, and non-parametric tests were therefore applied. The Mann-Whitney U test was used (1) to compare distance measurements between the sexes and (2) to determine the relationship between distance measurements and pathology of the maxillary sinus (presence/absence). The Wilcoxon signed-rank test was used to compare the smallest vertical distances of the roots of maxillary posterior teeth to the maxillary sinuses on panoramic radiographs and CBCT scans. The Pearson chi-square test was used (1) to determine the relationship between the apical status of the teeth (groups 1–4) in the 2 imaging modalities and (2) to analyze the topographic relationships of the roots of the teeth with the maxillary sinus (classes 1–3) in both imaging methods. Odds ratios (ORs) and confidence intervals (CIs) were calculated. The OR is a measurement of the relationship between an exposure and an outcome. The presence of at least 1 apical lesion adjacent to the maxillary sinus was regarded as the exposure, or risk factor, in this study. P values<0.05 were considered to indicate statistical significance.
Results
The Cronbach alpha values for intraobserver reliability ranged from 0.84 to 0.93 on the CBCT measurements and from 0.81 to 0.91 on the panoramic measurements. According to the review of CBCT scans, pathology was present in 41.8% (n=119) of the right maxillary sinuses and in 43.5% (n=124) of the left maxillary sinuses. In the analysis of panoramic radiography examinations, pathology was seen in 49.8% (n=142) of the right maxillary sinuses and in 38.9% (n=111) of the left maxillary sinuses. There was a statistically significant difference between the 2 methods in the detection of maxillary sinus pathology (P=0.025, P<0.05, respectively. More pathologies were detected on the panoramic images (n=253) than on the CBCT scans (n=243).
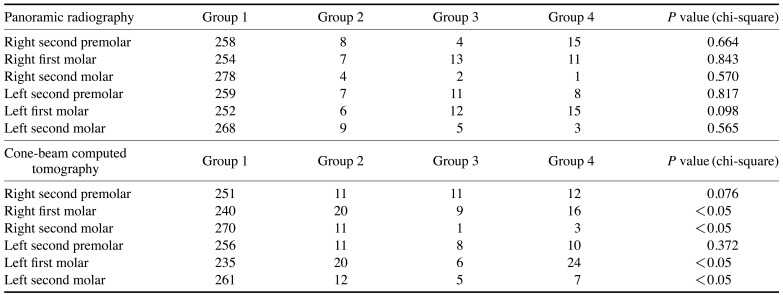
No statistical significance was found for the relationship between the presence of maxillary sinus pathology and the apical status of the maxillary posterior teeth in the analysis of panoramic radiographs (P>0.05). In contrast, a statistically significant relationship was found between the apical status of the right and left first and second molars and the presence of maxillary sinus pathology on the CBCT scans (Table 1). In cases where apical lesions were present in the right and left first and second molar teeth, maxillary sinus pathology was observed more frequently.
Table 1. Maxillary sinus pathology according to root canal treatment status and the presence of an apical lesion.
Group 1: non-endodontically treated teeth without an apical lesion, group 2: non-endodontically treated teeth with an apical lesion, group 3: endodontically treated teeth without an apical lesion, group 4: endodontically treated teeth with an apical lesion
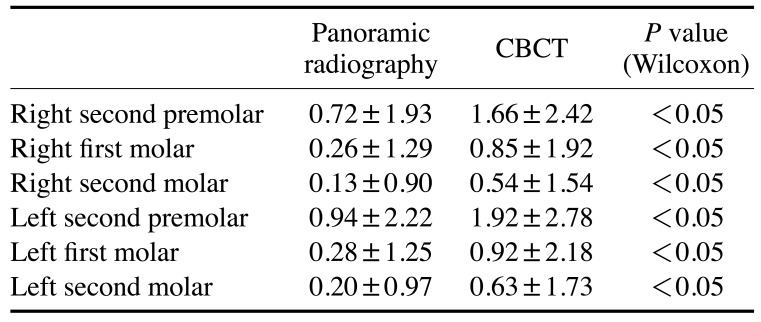
The panoramic radiography and CBCT scans showed statistically significant differences (Wilcoxon test, P<0.05) in all of the measurements of the closest vertical distance between the roots and the maxillary sinus. These distance measurements did not show a statistically significant difference between the 2 groups according to sex (Mann-Whitney U test, P>0.05). The CBCT measurements had larger mean values for all teeth (Table 2). In both imaging methods, the right and left second molar teeth showed the closest distance to the maxillary sinus. In both imaging methods, the distance from the roots of the maxillary teeth and the sinus floor did not show a significant relationship with the pathology of the maxillary sinus (Mann-Whitney U test, P>0.05).
Table 2. The closest vertical distances between maxillary posterior teeth roots to the sinus floor measured using panoramic radiography and cone-beam computed tomography (CBCT) (unit: mm).
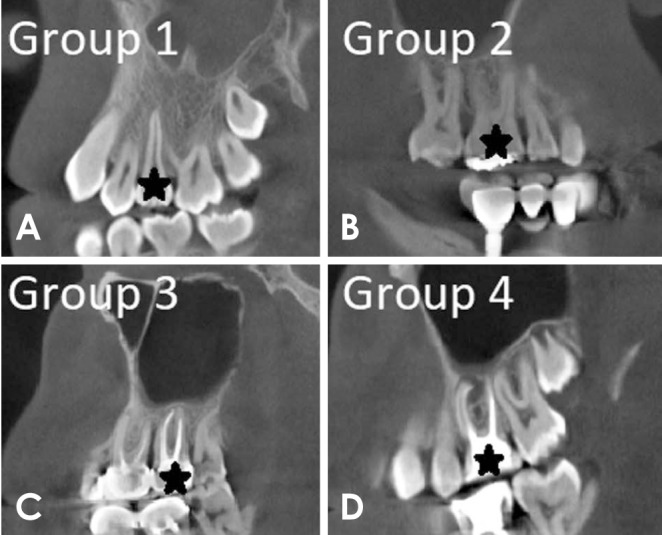
When the topographic relationships between dental roots and the maxillary sinus were examined, a statistically significant difference was found between the results of panoramic radiography and CBCT (P<0.05) (Table 3). In both imaging modalities, the second premolar was farthest from the maxillary sinus (class 1), and the left first molar was the tooth most commonly seen within the maxillary sinus (class 3) (Table 3). Compared to CBCT, the distance between the roots and the maxillary sinus was smaller on the panoramic radiographs. However, the panoramic radiographs showed a higher proportion of class 3 relationships (with the root tips seen in the sinus) than CBCT.
Table 3. Classification of topographic relationships of the right and left maxillary posterior teeth with the maxillary sinuses (number and percentage).
Class 1: distance between the root tip and the sinus floor, class 2: contact between the root tip and the sinus floor without the root entering the sinus, class 3: presence of the root tip inside the sinus, CBCT: cone-beam computed tomography
Binary logistic regression analysis of the CBCT images showed that the presence of at least 1 apical lesion adjacent to the maxillary sinus increased the likelihood of maxillary sinus pathology by 2.37 times (OR, 2.37; 95% CI, 1.58–3.55, P<0.05). In contrast, on the panoramic radiographs, the presence of at least 1 apical lesion was not associated with a significant risk increase for maxillary sinus pathology (OR, 1.02; 95% CI, 0.64–1.65, P>0.05).
Discussion
In this study, the relationship between the maxillary sinus floor and maxillary posterior teeth roots was analyzed using CBCT and panoramic radiography. Furthermore, the relationship between maxillary sinus pathology and apical lesions was investigated. In previous studies on this topic, it has been emphasized that the sinus floor and maxillary molar teeth roots are closely related.11,21,22 In our study, the relationships between the maxillary sinus and the second premolar, first molar, and second molar teeth were investigated. The measurements of the closest vertical distance between the tooth root and the maxillary sinus on panoramic radiographs and CBCT scans showed statistically significant differences between these imaging methods. Specifically, the vertical distance measurements on CBCT scans showed higher values (P<0.001). Panoramic radiography is an easy-to-access, cheap, and low-dose imaging method that is generally the first-line technique for examining teeth and jaws in dentistry. Nonetheless, the horizontal and vertical magnification factors of panoramic radiographs and variations in the positioning of patients decrease the reliability of distance measurements on panoramic radiographs. For this reason, panoramic radiography is not recommended for distance measurements and is less reliable than 3-dimensional imaging techniques.23 In this retrospective study, records were analyzed of patients whose radiographs were taken according to the department's routine protocol, which ensured the elimination of distortions and patient positioning errors by stabilizing patients' heads while keeping their Frankfurt horizontal plane parallel to the floor. This protocol is important because the reliability of the panoramic radiography method is highly dependent on the patients' head position. If this step is neglected, there could be distortions or enlargements depending on the position of the maxillary structures and the head, preventing proper measurements from being made.
In our study, the classification proposed by Oberli et al.20 was applied to classify the topographic relationships between the teeth and the sinus. This classification was used to describe the spatial relationship of posterior teeth roots with the sinus floor on CBCT and panoramic images, and the 2 imaging methods showed significant differences regarding this relationship. Class 1 (presence of distance between the root tip and sinus) was found less often on the panoramic radiographs. Panoramic radiography yielded a higher proportion of class 3 relationships (with the root tips seen in the sinus) than CBCT. The immediate relationship between the position of the tip of the root and the maxillary sinus is a predictive factor for oroantral communication.24 Both overdiagnosis and underdiagnosis of this relationship are possible using panoramic radiography. The true spatial relationships between (1) the sinus and the root tip and (2) the sinus and a lesion can only be determined using CBCT for the above-mentioned reasons (magnification, distortion, and head positioning).
Maxillary posterior roots and the sinus floor are separated by bone and/or sinus mucosa.22 The thinness of this tissue structure may fail to prevent periapical and periodontal infections from infiltrating into the maxillary sinus. Increased proximity of the maxillary posterior root to the base of the sinus has been reported to increase the risk of a tooth-related mucosal reaction.9 However, in our study, the distance between the roots of maxillary teeth and the sinus floor showed no relationship to maxillary sinus pathology on either imaging method. Based on the CBCT images, the presence of at least 1 apical lesion adjacent to the maxillary sinus was found to increase maxillary sinus pathology by 2.37 times. Since periodontal diseases can cause maxillary sinus pathology,3 teeth with alveolar bone loss more than half of the bone support were excluded from the study. Moreover, periodontal diseases cannot be diagnosed using radiological parameters alone; instead, radiological findings should be combined with a clinical examination. However, this study has the limitations of a cross-sectional study design, and no clinical examinations, such as pocket probing depth measurements or bleeding score calculations, were performed to assess periodontal disease activity. In future studies, clinical examinations of the patients and evaluations of periodontal disease activity will eliminate this problem.
The presence of at least 1 apical lesion was not associated with a significant risk increase for maxillary sinus pathology on the panoramic radiographs (OR, 1.02; 95% CI, 0.64–1.65, P>0.05). Previous studies have reported ORs of 3.5,7 16.4,25 and 9.7515 for mucosal thickening in the presence of teeth with periapical lesions. It is believed that bacteria and toxins in apical lesions can infiltrate the maxillary sinuses directly or via the numerous vascular anastomoses, porous alveolar bone marrow, and lymphatics, thereby infecting the sinus mucosa.1 In some instances, mucositis (intrinsic sinus pathology, not related to a periapical lesion) can co-occur with a periapical lesion of the premolars or molars. This study was limited to a cross-sectional evaluation, so it was difficult to arrive at a definitive conclusion related to the causes of mucosal hypertrophy in the maxillary sinus. Further analyses in longitudinal studies are needed.
In addition, although not evaluated in our study, the severity of periapical lesions may affect the prevalence of mucosal thickening. Lu et al.1 reported that the prevalence of maxillary sinus mucosal thickening was 41.5% in patients without apical periodontitis, more than 70% in patients with mild and moderate apical periodontitis, and 100% in those with severe apical periodontitis. The ORs calculated in our study were lower than those previously reported in the literature,7,15,25 which may have been due to differences in the severity of periapical lesions in the teeth included in the study.
In their study, Pommer et al.26 stated that the ideal sinus mucosal thickness was 0.09±0.05 mm on average. In contrast, Aimetti et al.27 reported that the mean sinus mucosal thickness was 0.97±0.36 mm. In another study, it was emphasized that the sinus mucosa could only be seen when its thickness was 2 mm or more. It was also stated that a thickness exceeding 2 mm should be considered pathological.28 For this reason, in our study, cases where the sinus floor mucosa thickness was 2 mm or more were classified as pathological. The reported prevalence of mucosal thickening of the maxillary sinus ranges from 12%7 to 60.5%.15 This variation could be attributed to differences in race or age, as well as to the use of different diagnostic techniques.1 In this study, the rate of mucosal thickening exceeding 2 mm, which was defined as pathological, was found to be 41.8% in the right maxillary sinus and 43.5% in the left maxillary sinus in the CBCT examinations. On the panoramic radiographs, the frequency of pathology was 49.8% in the right maxillary sinus and 38.9% in the left maxillary sinus.
In this study, compared to panoramic radiography, CBCT was more effective for the diagnosis of periapical lesions. Panoramic radiography is useful for the diagnosis of large periapical lesions. However, because of its low spatial resolution, it is inadequate for diagnosing initial periapical lesions and for evaluating relationships between teeth and the sinus.9 The spatial resolution of an imaging method is defined as its capability to resolve fine details.29 Furthermore, the anatomic superpositions common on panoramic radiographs make it difficult to detect periapical lesions.30
In conclusion, compared to CBCT imaging, panoramic radiography showed different vertical distance measurement values when evaluating the spatial relationships between the teeth and the maxillary sinus. Furthermore, the presence of periapical lesions adjacent to the maxillary sinuses was found to be a risk factor for sinus mucosal thickening.
References
- 1.Lu Y, Liu Z, Zhang L, Zhou X, Zheng Q, Duan X, et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod. 2012;38:1069–1074. doi: 10.1016/j.joen.2012.04.027. [DOI] [PubMed] [Google Scholar]
- 2.Melén I, Lindahl L, Andréasson L, Rundcrantz H. Chronic maxillary sinusitis. Definition, diagnosis and relation to dental infections and nasal polyposis. Acta Otolaryngol. 1986;101:320–327. doi: 10.3109/00016488609132845. [DOI] [PubMed] [Google Scholar]
- 3.Abrahams JJ, Glassberg RM. Dental disease: a frequently unrecognized cause of maxillary sinus abnormalities? AJR Am J Roentgenol. 1996;166:1219–1223. doi: 10.2214/ajr.166.5.8615273. [DOI] [PubMed] [Google Scholar]
- 4.Doud Galli SK, Lebowitz RA, Giacchi RJ, Glickman R, Jacobs JB. Chronic sinusitis complicating sinus lift surgery. Am J Rhinol. 2001;15:181–186. doi: 10.2500/105065801779954120. [DOI] [PubMed] [Google Scholar]
- 5.Kretzschmar DP, Kretzschmar JL. Rhinosinusitis: review from a dental perspective. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:128–135. doi: 10.1016/s1079-2104(03)00306-8. [DOI] [PubMed] [Google Scholar]
- 6.Savolainen S, Eskelin M, Jousimies-Somer H, Ylikoski J. Radiological findings in the maxillary sinuses of symptomless young men. Acta Otolaryngol Suppl. 1997;529:153–157. doi: 10.3109/00016489709124109. [DOI] [PubMed] [Google Scholar]
- 7.Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e80–e87. doi: 10.1016/j.tripleo.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 8.Ren S, Zhao H, Liu J, Wang Q, Pan Y. Significance of maxillary sinus mucosal thickening in patients with periodontal disease. Int Dent J. 2015;65:303–310. doi: 10.1111/idj.12186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shahbazian M, Vandewoude C, Wyatt J, Jacobs R. Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin Oral Investig. 2014;18:293–300. doi: 10.1007/s00784-013-0963-x. [DOI] [PubMed] [Google Scholar]
- 10.von Arx T, Fodich I, Bornstein MM. Proximity of premolar roots to maxillary sinus: a radiographic survey using cone-beam computed tomography. J Endod. 2014;40:1541–1548. doi: 10.1016/j.joen.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 11.Sharan A, Madjar D. Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:375–381. doi: 10.1016/j.tripleo.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 12.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8:1558–1564. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 13.Bremke M, Sesterhenn AM, Murthum T, Al Hail A, Bien S, Werner JA. Digital volume tomography (DVT) as a diagnostic modality of the anterior skull base. Acta Otolaryngol. 2009;129:1106–1114. doi: 10.1080/00016480802620621. [DOI] [PubMed] [Google Scholar]
- 14.Maestre-Ferrín L, Galán-Gil S, Carrillo-García C, Peñarrocha-Diago M. Radiographic findings in the maxillary sinus: comparison of panoramic radiography with computed tomography. Int J Oral Maxillofac Implants. 2011;26:341–346. [PubMed] [Google Scholar]
- 15.Shanbhag S, Karnik P, Shirke P, Shanbhag V. Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. J Endod. 2013;39:853–857. doi: 10.1016/j.joen.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:106–114. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 17.Howe RB. First molar radicular bone near the maxillary sinus: a comparison of CBCT analysis and gross anatomic dissection for small bony measurement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:264–269. doi: 10.1016/j.tripleo.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 18.Hauman CH, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002;35:127–141. doi: 10.1046/j.0143-2885.2001.00524.x. [DOI] [PubMed] [Google Scholar]
- 19.Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:114–119. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Oberli K, Bornstein MM, von Arx T. Periapical surgery and the maxillary sinus: radiographic parameters for clinical outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:848–853. doi: 10.1016/j.tripleo.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 21.Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol. 1992;73:345–346. doi: 10.1016/0030-4220(92)90133-b. [DOI] [PubMed] [Google Scholar]
- 22.Kwak HH, Park HD, Yoon HR, Kang MK, Koh KS, Kim HJ. Topographic anatomy of the inferior wall of the maxillary sinus in Koreans. Int J Oral Maxillofac Surg. 2004;33:382–388. doi: 10.1016/j.ijom.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 23.Nishikawa K, Suehiro A, Sekine H, Kousuge Y, Wakoh M, Sano T. Is linear distance measured by panoramic radiography reliable? Oral Radiol. 2010;26:16–19. [Google Scholar]
- 24.Lopes LJ, Gamba TO, Bertinato JV, Freitas DQ. Comparison of panoramic radiography and CBCT to identify maxillary posterior roots invading the maxillary sinus. Dentomaxillofac Radiol. 2016;45:20160043. doi: 10.1259/dmfr.20160043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brüllmann DD, Schmidtmann I, Hornstein S, Schulze RK. Correlation of cone beam computed tomography (CBCT) findings in the maxillary sinus with dental diagnoses: a retrospective cross-sectional study. Clin Oral Investig. 2012;16:1023–1029. doi: 10.1007/s00784-011-0620-1. [DOI] [PubMed] [Google Scholar]
- 26.Pommer B, Unger E, Sütö D, Hack N, Watzek G. Mechanical properties of the Schneiderian membrane in vitro. Clin Oral Implants Res. 2009;20:633–637. doi: 10.1111/j.1600-0501.2008.01686.x. [DOI] [PubMed] [Google Scholar]
- 27.Aimetti M, Massei G, Morra M, Cardesi E, Romano F. Correlation between gingival phenotype and Schneiderian membrane thickness. Int J Oral Maxillofac Implants. 2008;23:1128–1132. [PubMed] [Google Scholar]
- 28.Cagici CA, Yilmazer C, Hurcan C, Ozer C, Ozer F. Appropriate interslice gap for screening coronal paranasal sinus tomography for mucosal thickening. Eur Arch Otorhinolaryngol. 2009;266:519–525. doi: 10.1007/s00405-008-0786-6. [DOI] [PubMed] [Google Scholar]
- 29.Brüllmann D, Schulze RK. Spatial resolution in CBCT machines for dental/maxillofacial applications - what do we know today? Dentomaxillofac Radiol. 2015;44:20140204. doi: 10.1259/dmfr.20140204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Temmerman A, Hertelé S, Teughels W, Dekeyser C, Jacobs R, Quirynen M. Are panoramic images reliable in planning sinus augmentation procedures? Clin Oral Implants Res. 2011;22:189–194. doi: 10.1111/j.1600-0501.2010.02000.x. [DOI] [PubMed] [Google Scholar]