Abstract
Objective This study aims to report the clinical features of pediatric patients diagnosed with subscapular osteochondroma submitted to surgical treatment at Hospital Infantil Joana de Gusmão (HIJG), in Florianópolis, Santa Catarina, Brazil, between 2003 and 2017.
Methods Analytical, descriptive and retrospective case series of seven patients with subscapular osteochondroma diagnosis.
Results The average age of the analyzed patients was 9.5 years-old; 71% of the patients were male. The mean time between onset of symptoms and the surgical procedure was 1.2 years. Approximately 71% of the patients presented osteochondroma in the right scapula, and 57.1% of the lesions were classified as sessile. At the clinical examination, winged scapula was observed in 85.7%, crepitus in 71.4%, and 42.9% of the patients complained about pain.
Conclusion The winged scapula can have different etiologies, including subscapular osteochondroma. The knowledge about functional anatomy and orthopedic semiology added to the correct systematization approach to bone tumors is the basis for the correct differential diagnosis and adequate treatment.
Keywords: osteochondroma, scapula, bone neoplasms
Introduction
An osteochondroma is a bone exostosis in which a continuous cortical layer projects from the underlying bone, is filled with cancellous bone and covered by a cartilaginous tissue of 1 to 3 mm in thickness. It is probably originated from a growth modification of the physeal plate, which accompanies the growth rate and results in an appearance of bony prominences. 1
Osteochondromas account for 10 to 15% of all bone tumors. They are the most common benign bone tumors, corresponding to 30 to 50% of the cases. 2 3 Most osteochondromas are single lesions, which can occur in two forms: sessile or pedunculated. They mainly affect the metaphyseal region of long bones, especially the knee (distal femur and proximal tibia) and the proximal humerus, and rarely occur on flat bones. However, it is the most common benign tumor of the scapula, accounting for approximately 5% of such lesions 2 3 ( Fig. 1 ).
Fig. 1.

Axial radiograph of the scapula showing an osteochondroma in the middle third of its anterior aspect.
Osteochondromas are most common in patients younger than 30 years-old, and its prevalence is higher in males, with a 1:5 ratio. 4 5 Malignant osteochondromas are rare to malignant, occurring in approximately 2% of the cases when in solitary form. 6 7
The winged scapula (scapula alata) is a syndrome with several etiologies, and the most common cause related to long thoracic nerve injury. However, subscapular osteochondroma is an important differential diagnosis, and, in this case, the disorder is referred to as pseudo-winging of the scapula and characterized by a mobile or fixed scapular deformity. 8 9 Described by McWilliams in 1914, the pseudo-winging of the scapula secondary to an osteochondroma is difficult to differentiate from the winged scapula resulting from long thoracic nerve lesion; therefore, it must always be included among the diagnostic possibilities for this type of clinical manifestation. 10 11
The literature has few studies relating the winged scapula to subscapular osteochondromas, and most of them are case reports.
Therefore, this study aims to report the clinical features of pediatric patients diagnosed with subscapular osteochondroma and submitted to surgical treatment at Hospital Infantil Joana de Gusmão (HIJG), in Florianópolis, SC, Brazil.
This study was approved by the Ethics and Research Committee of HIJG under the number 2.213.465.
Materials and Methods
This study is an analytical, descriptive, and retrospective case series.
Seven medical reports from children aged 4 to 14 years-old, admitted for subscapular osteochondroma resection at the orthopedics and traumatology department of a children's hospital (Hospital Infantil de Ortopedia e Traumatologia) from February 2003 to March 2017, were analyzed.
The instrument for data collection was constructed by the authors through a protocol developed for this study, which addresses socioeconomic characteristics, age, gender, and location of the lesion, in addition to a descriptive analysis of tumoral and clinical features of the patients studied.
The collected information was stored in an electronic database (Excel). Categorical variables were described as absolute (n) and relative (%) frequency. The statistical analysis was performed with the SPSS Statistics for Windows, Version 22.0 software (IBM Corp., Armonk, NY, USA).
Results
The medical records from 7 patients diagnosed with subscapular osteochondroma and submitted to the surgical treatment at HIJG between 2003 and 2017 were analyzed.
Among these patients, 71% were male. Their average age was 9 years, 5 months-old, ranging from 4 to 14 years-old. The average time from symptoms onset to surgery was 1 year, 2 months.
According to the tumor-related characteristics, 5 patients (71.4%) presented the scapula osteochondroma on the right side and 2 (28.6%), on the left side. Of this total, 57.1% were sessile lesions, and the tumor was in the scapular region (solitary) in approximately 43% of the cases ( Fig. 2 ).
Fig. 2.

Clinical image of a subscapular osteochondroma.
Regarding the clinical picture, most patients, namely 85.6%, presented pseudo-winging of the scapula at the physical examination, whereas crepitation was noted in 71.4% of the children. Less than half of the patients (42.9%) complained of pain. Out of the seven patients, three had bursitis ( Table 1 ).
Table 1. Database.
| Name | Gender | Age | Evolution Time | Side | Solitary/Multiple | Sessile/Pedunculated | Pain | Winged Scapula | Crepitation | Bursitis |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 14 | 1.7 | Right | Solitary | Pedunculated | No | Yes | Yes | Yes |
| 2 | M | 14 | 0.9 | Right | Multiple | Sessile | Yes | Yes | Yes | No |
| 3 | F | 6 | 1.3 | Left | Multiple | Sessile | No | Yes | Yes | No |
| 4 | M | 4 | 1.2 | Right | Multiple | Pedunculated | No | Yes | No | No |
| 5 | M | 12 | 1.8 | Left | Solitary | Sessile | Yes | Yes | Yes | Yes |
| 6 | F | 10 | 1.2 | Right | Multiple | Sessile | No | Yes | Yes | No |
| 7 | M | 7 | 0.7 | Right | Solitary | Pedunculated | Yes | No | No | Yes |
Source: Prepared by the author, 2017.
As for cases distribution, among the observed variables, there was a predominance of the right side, “winged” (snapping), and absence of bursitis (six among seven cases for all these variables). Regarding type, form, pain and crepitation, there was a balance between presence and absence ( Table 2 ).
Table 2. Statistical analysis.
| Variable | Frequency (%) |
|---|---|
| Side | |
| Left | 1 (14.3) |
| Right | 6 (85.7) |
| Type | |
| Solitary | 3 (42.9) |
| Multiple | 4 (57.1) |
| Form | |
| Sessile | 3 (42.9) |
| Pedunculated | 4 (57.1) |
| Pain | |
| Present | 3 (42.9) |
| Absent | 4 (57.1) |
| “Winged Scapula” (Snapping) | |
| Yes | 1 (14.3) |
| No | 6 (85.7) |
| Crepitation | |
| Yes | 4 (57.1) |
| No | 3 (42.9) |
| Bursitis | |
| Yes | 1 (14.3) |
| No | 6 (85.7) |
Source: Prepared by the author, 2017.
Discussion
Osteochondroma accounts for 30 to 50% of benign bone tumors, but only 4% of scapular tumors. McWilliams was the first author to describe an osteochondroma with scapular deformity in a case report published in 1914. 10
Osteochondroma is the most common benign tumor in the metaphyseal region of long bones and rarely affects flat bones; however, it is the most frequent benign tumor in the scapula. 2 3
Its presence, and, therefore, its diagnosis is noted due to the growth and increased volume in the scapular region at ectoscopy. Clinical manifestations, such as local pain, are usually delayed and may be secondary to neurovascular structures compression, bursa thickening (when present), peduncle fracture, or malignant transformation. Other symptoms, such as scapular protuberance, crepitation, edema, and loss of mobility, may be present depending on the size and location of the tumor, both in the sagittal and coronal planes. 12 The “pseudo-winging of the scapula” is observed when the tumor is located in the medial, inferior, and ventral border of the scapula, where the tumor concavity is dislocated over the convex aspect of the rib cage, leading the scapula to the lateral region of the shoulder girdle. It happens when the patient performs the abduction associated with the internal shoulder rotation. 13 This picture is very similar to the long thoracic nerve paralysis, in which the integrity of the serratus anterior muscle is evaluated through a maneuver in which the patient pushes a surface longitudinal to the axis of the upper limbs with both elbows in extension. This test is considered positive when there is an excessive scapular lateral dislocation that is asymmetric to the contralateral side, thus resulting in a “winged scapula” ( Fig. 3 ).
Fig. 3.

Clinical image of a winged scapula.
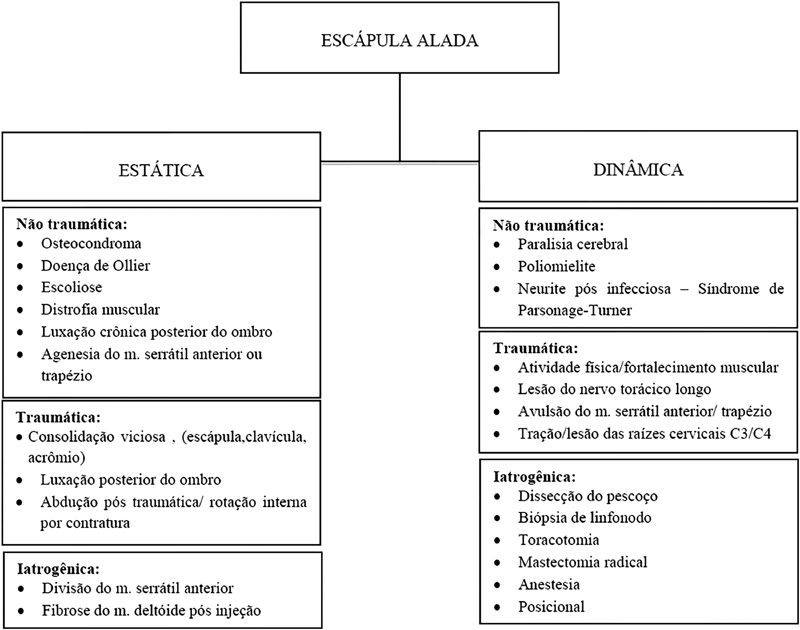
Differential diagnoses for winged scapula also include amyotrophic neuralgia, nerve damage, scapulothoracic dyskinesias, and any other fascioscapular thoracic dystrophy 12 14 ( Fig. 4 ).
Fig. 4.
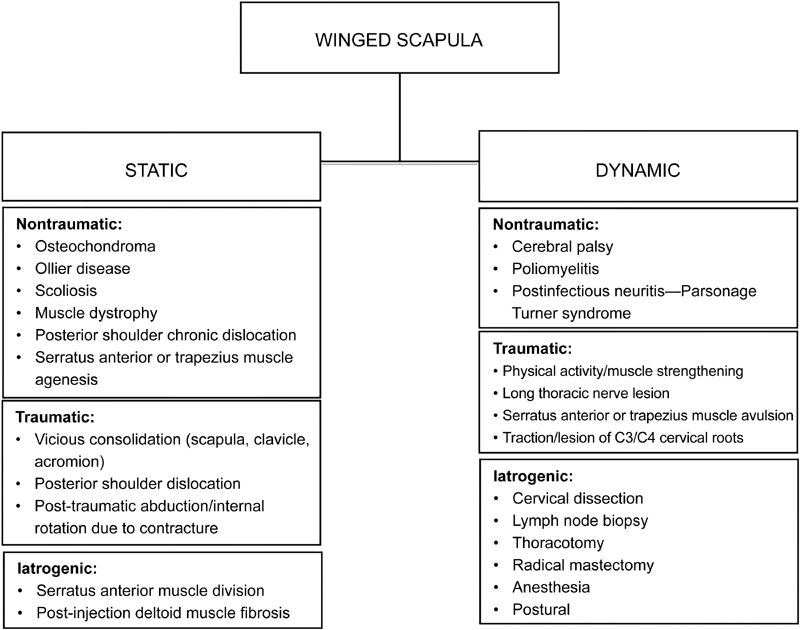
Differential diagnosis of scapular lesions.
Fiddian e Wing 15 classified the winged scapula according to its mobility as static (A) or dynamic (B), and, per its anatomical origin, in four types: type I, resulting from nervous lesion (most common), type II, related to a muscle lesion, type III, per bone etiology, and type IV, per joint damage. All studied patients were classified as dynamic winged scapula with bone origin (B-III)
The malignant transformation of the osteochondroma is uncommon. In solitary forms, it occurs in approximately 2% of the cases and, in multiple forms, around 27%. 16 The literature highlights that the thickness of the cartilaginous layer is a predictive factor for aggressiveness, that is, a thickness higher than 2.0 cm is a strong indicator of malignant transformation, and it is associated with marginal calcification. 12 16 As for clinical manifestations, it is necessary to keep in mind the osteochondroma growth after skeletal maturity, since these tumors tend to stop growing during the second decade of life. In all our operated cases, the resected material was referred to the pathological anatomy service, and the presence of malignant cells was ruled out.
The postresection osteochondroma recurrence rate is around 2%, and it is due to the presence of residual cartilage and its perichondrium after the surgical procedure. 17 There was no tumor recurrence in our study.
Radiographic studies in anteroposterior, lateral scapular and axillary views are enough for lesion identification. In case of difficult interpretation, a computed tomography can be useful to improve the access strategy. Since it is a cartilaginous lesion, a magnetic resonance scan is an excellent adjunct technique, mainly to evaluate the cartilaginous layer thickening and the presence and extension of the bursa.
Several authors describe the presence of a bursa between the osteochondroma and the involved soft tissues (dorsal and serratus anterior muscles) due to the friction between the tumor and the rib cage, resulting in the formation of synovial fluid and causing local pain because of the inflammatory process. 18 Orlow, 19 in 1891, was the first author to describe it, using the term exostosis bursata . In our study, there were 3 cases with bursa formation, including 2 with local pain; this can be a suspicion factor, considering that, among those who did not present it (57%), only 1 child complained of pain.
There was no relationship between the analyzed data to support any conclusion as per type, form, evolution time, pain, crepitation and presence of pseudo-winging of the scapula. Data are isolated and not correlated.
This topic was chosen to highlight an organizational chart for diagnosis. While complaints regarding osteochondromas are relatively usual at orthopedics outpatient facilities, this presentation is not common, and it can go unnoticed, resulting in an untimely diagnosis.
Since this is a rare event, the sample size does not allow the determination of possible relationships between variables. Therefore, further studies are required, increasing the collection time or the experimental field to gather more information.
The main limitation of this study lies in its retrospective and observational design and in the lack of a control group. However, our case series is larger when compared to a literature review on the subject, since most papers are case reports.
Conclusion
The winged scapula can have several etiologies, including the subscapular osteochondroma. The knowledge of the functional anatomy and orthopedics semiology, in addition to the correct systematization for bone tumors approach, is the basis for the correct differential diagnosis and proper treatment.
Conflitos de Interesses Os autores declaram não haver conflito de interesses.
Trabalho feito no Hospital Infantil Joana de Gusmão, Florianópolis, SC, Brasil.
This study was performed at Hospital Infantil Joana de Gusmão (HIJG), Florianópolis, SC, Brazil.
Referências
- 1.Ermiş M N, Aykut U S, Durakbaşa M O, Ozel M S, Bozkuş F S, Karakaş E S. Snapping scapula syndrome caused by subscapular osteochondroma. Eklem Hastalik Cerrahisi. 2012;23(01):40–43. [PubMed] [Google Scholar]
- 2.Unni K K, Inwards C Y, Dahlin D C. Philadelphia: Lippincott Williams & Wilkins; 2010. Dhalin's bone tumors: general aspects and data on 10,165 cases. 6th ed. [Google Scholar]
- 3.Mohsen M S, Moosa N K, Kumar P. Osteochondroma of the scapula associated with winging and large bursa formation. Med Princ Pract. 2006;15(05):387–390. doi: 10.1159/000094275. [DOI] [PubMed] [Google Scholar]
- 4.Galate J F, Blue J M, Gaines R W. Osteochondroma of the scapula. Mo Med. 1995;92(02):95–97. [PubMed] [Google Scholar]
- 5.Bovée J V. Multiple osteochondromas. Orphanet J Rare Dis. 2008;3:3. doi: 10.1186/1750-1172-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dharmadhikari R P. Painful Snapping and Pseudo-winging Scapula due to a large Scapular Osteochondroma. J Orthop Case Rep. 2012;2(02):10–13. [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed A R, Tan T S, Unni K K, Collins M S, Wenger D E, Sim F H. Secondary chondrosarcoma in osteochondroma: report of 107 patients. Clin Orthop Relat Res. 2003;(411):193–206. doi: 10.1097/01.blo.0000069888.31220.2b. [DOI] [PubMed] [Google Scholar]
- 8.Chillemi C, Franceschini V, Ippolito G, Pasquali R, Diotallevi R, Petrozza V et al. Osteochondroma as a cause of scapular winging in an adolescent: a case report and review of the literature. J Med Case Reports. 2013;7:220. doi: 10.1186/1752-1947-7-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flugstad N A, Sanger J R, Hackbarth D A. Pseudo-winging of the scapula caused by scapular osteochondroma: review of literature and case report. Hand (N Y) 2015;10(02):353–356. doi: 10.1007/s11552-014-9659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McWilliams C A. Subscapular exostosis with adventitious bursa. https://jamanetwork.com/journals/jama/article-abstract/437705 JAMA. 1914;LXIII(17):1473–1474. [Google Scholar]
- 11.Martin R M, Fish D E. Scapular winging: anatomical review, diagnosis, and treatments. Curr Rev Musculoskelet Med. 2008;1(01):1–11. doi: 10.1007/s12178-007-9000-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jindal M. Delayed Presentation of Osteochondroma at Superior Angle of Scapula-A Case Report. J Orthop Case Rep. 2016;6(03):32–34. doi: 10.13107/jocr.2250-0685.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walter J, Kiely N, Cool P, Tyrrell P, Quinlivan R M. An unusual case of scapula winging. Neuromuscul Disord. 2013;23(03):277–278. doi: 10.1016/j.nmd.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Orth P, Anagnostakos K, Fritsch E, Kohn D, Madry H. Static winging of the scapula caused by osteochondroma in adults: a case series. J Med Case Reports. 2012;6:363. doi: 10.1186/1752-1947-6-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fiddian N J, King R J. The winged scapula. Clin Orthop Relat Res. 1984;(185):228–236. [PubMed] [Google Scholar]
- 16.Garrison R C, Unni K K, McLeod R A, Pritchard D J, Dahlin D C. Chondrosarcoma arising in osteochondroma. Cancer. 1982;49(09):1890–1897. doi: 10.1002/1097-0142(19820501)49:9<1890::aid-cncr2820490923>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 17.Ceberut K, Korkmaz M, Ergin I, Müslehiddinoglu A. Bursa formation with scapular osteochondroma in hereditary multiple exostosis. J Coll Physicians Surg Pak. 2013;23(07):512–514. [PubMed] [Google Scholar]
- 18.Ali A A, Sharma P, Rege R, Seena C R, Rajesh S. Exostosis Bursata - Multimodality Imaging Approach. J Clin Diagn Res. 2016;10(09):TD03–TD04. doi: 10.7860/JCDR/2016/15688.8431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orlow L W. Die exostosis bursata und ihreentstehung. Dtsch Z Chir. 1891:293–308. [Google Scholar]