Abstract
Background and Objectives
Screening and early diagnosis for heart failure (HF) are critical. However, conventional screening diagnostic methods have limitations, and electrocardiography (ECG)-based HF identification may be helpful. This study aimed to develop and validate a deep-learning algorithm for ECG-based HF identification (DEHF).
Methods
The study involved 2 hospitals and 55,163 ECGs of 22,765 patients who performed echocardiography within 4 weeks were study subjects. ECGs were divided into derivation and validation data. Demographic and ECG features were used as predictive variables. The primary endpoint was detection of HF with reduced ejection fraction (HFrEF; ejection fraction [EF]≤40%), and the secondary endpoint was HF with mid-range to reduced EF (≤50%). We developed the DEHF using derivation data and the algorithm representing the risk of HF between 0 and 1. We confirmed accuracy and compared logistic regression (LR) and random forest (RF) analyses using validation data.
Results
The area under the receiver operating characteristic curves (AUROCs) of DEHF for identification of HFrEF were 0.843 (95% confidence interval, 0.840–0.845) and 0.889 (0.887–0.891) for internal and external validation, respectively, and these results significantly outperformed those of LR (0.800 [0.797–0.803], 0.847 [0.844–0.850]) and RF (0.807 [0.804–0.810], 0.853 [0.850–0.855]) analyses. The AUROCs of deep learning for identification of the secondary endpoint was 0.821 (0.819–0.823) and 0.850 (0.848–0.852) for internal and external validation, respectively, and these results significantly outperformed those of LR and RF.
Conclusions
The deep-learning algorithm accurately identified HF using ECG features and outperformed other machine-learning methods.
Keywords: Deep learning, Heart failure, Electrocardiography, Machine learning, Artificial intelligence
INTRODUCTION
Heart failure (HF) has a prevalence as high as 2% of adults overall (8% of adults aged≥75 years), affecting 26 million patients worldwide and 3.5 million new patients every year.1) It is a critical disease, with 17–45% of patients admitted for HF dying within 1 year and the majority of the remaining patients dying within 5 years.2) Patients with HF have reduced physical activity, and many are hospitalized repeatedly, leading to deterioration of quality of life and great expense. The cost of treatment for patients with HF accounts for 2% of total health care expenses and is expected to double by 2030 due to population aging.3)
Various methods are used for the diagnosis of HF. These methods, however, require a physical examination, echocardiography, and laboratory tests, as well as a high level of expertise for interpretation of results and making a diagnosis.4) Furthermore, existing methods are fixed tools that do not account for the relationships among variables and thus provide limited performance.5),6) For these reasons, existing screening and early diagnosis strategies for HF are limited in value. Electrocardiography (ECG) is non-invasive and simple to perform and is widely used as part of a general check-up. The ability to identify HF using only demographic factors and ECG could be used for early diagnosis and would enable referral for further investigation.
A previous study showed a significant association between HF and ECG features.7) However, statistical limitations associated with logistic regression (LR) analysis prevented researchers from developing a predictive model for HF using ECG. Several attempts have now been made to develop a predictive model for HF using machine-learning.8),9),10) To achieve high accuracy with limited information, we used deep-learning techniques to develop a diagnostic algorithm. Deep-learning technique has achieved state-of-art performance in several medical domains, such as image detection and clinical outcome prediction.11),12),13) An advantage of deep-learning technique is the automatic-learning feature and ability to identify associations using available data.14) This study developed and validated a deep-learning algorithm for ECG-based HF identification (DEHF).
METHODS
Study population
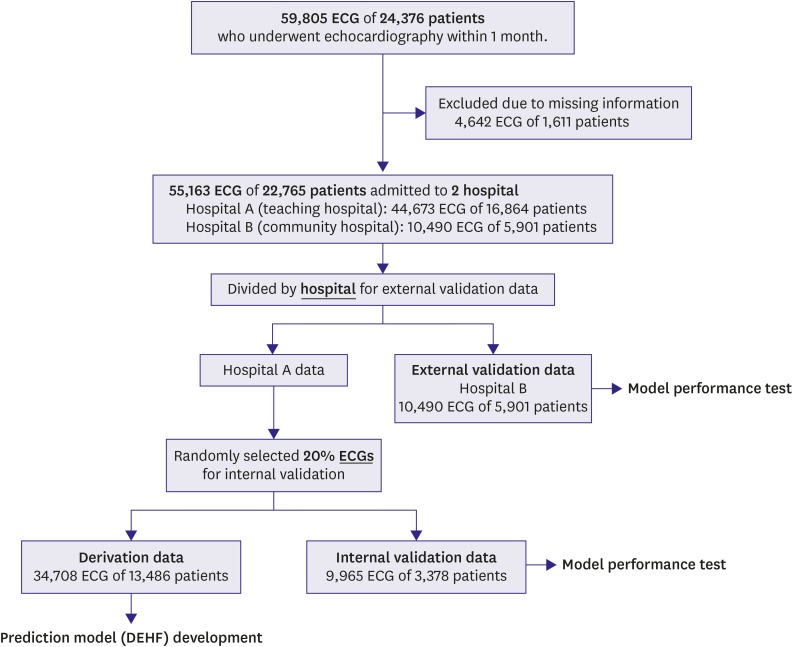
We performed a multicenter retrospective cohort study involving 2 hospitals. The study subjects were ECGs of adult (aged≥18 years) patients who had undergone echocardiography within 4 weeks. We excluded patients with missing values (Figure 1). The Sejong General Hospital Institutional Review Board (IRB) (No. 2018-0384) and Mediplex Sejong Hospital IRB (No. 2018-024) approved this study protocol and waived the need for informed consent due to impracticality and minimal harm. We excluded subjects with missing demographic and echocardiographic information.
Figure 1. Study flow chart.
DEHF = deep-learning algorithm for electrocardiography-based heart failure identification; ECG = electrocardiography.
Data management
The characteristics of both hospitals were different (hospital A: a cardiovascular teaching hospital, hospital B: a community general hospital). Data from hospital A (October 2016–July 2018) were split into algorithm derivation and internal validation data by randomization. Data from hospital B (March 2017–July 2018) were only used for external validation. The derivation data were used to develop the deep-learning algorithm, DEHF. We evaluated the accuracy of the algorithm using internal validation data that were not used for algorithm derivation. Furthermore, we used external validation data from hospital B to verify that the algorithm was applicable across centers.
The primary endpoint was detection of HF with reduced ejection fraction (HFrEF), defined as ≤40% on echocardiography.4) The secondary endpoint was detection of HF with mid-range to reduced ejection fraction (EF), defined as ≤50% on echocardiography.4) We used demographic information and ECG features including age, sex, weight, height, heart rate, presence of atrial fibrillation (AF) or atrial flutter (AFL), QT interval, QRS duration, R wave axis, and T wave axis, as the predictive variables. For use of the algorithm in AF, we did not include the P wave axis or PR interval as predictive variables.
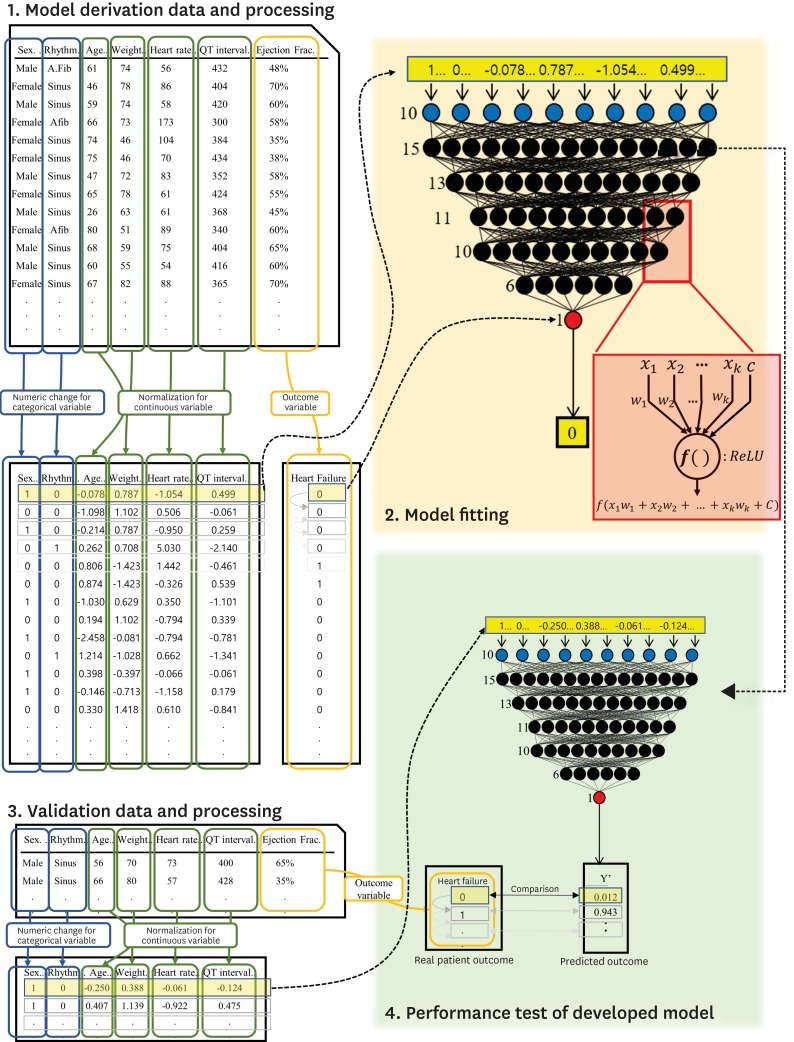
Development of deep-learning algorithm
As shown in Figure 2, we developed the deep-learning algorithm, DEHF, using only derivation data. The algorithm was developed using deep neural network (DNN), a method of deep-learning with 5 hidden layers, 45 nodes, and dropout layers.15) Because there was no gain in accuracy with more than 5 layers, we used 5 to minimize the parameters to be learned. The first to fifth layers consisted of 15, 13, 11, 10, and 6 nodes, and used a rectified linear unit as the activation function.16) The last layer consisted of 1 node, which represented the risk of each outcome and used a sigmoid function.
Figure 2. Development and validation of DEHF.
DEHF = deep-learning algorithm for electrocardiography-based heart failure identification; ECG = electrocardiography; HF = heart failure.
We used TensorFlow (the Google Brain Team) as the backend.17) Furthermore, we used the Adagrad optimizer with default parameters and binary cross-entropy as the loss function. As shown in Figure 2, the value at 1 node of the DNN is added by multiplying the values from the upper layer nodes (xk) by their weights (wk). The added value, (x1+w1+x2+w2+...+xkwk+c), is processed by the activation function, and the value of f(x1+w1+x2+w2+...+xkwk+c) is sent to the next node.
As shown in Figure 2, before using the derivation data for DEHF development, we replaced the values of the categorical variables with binary numeric values and normalized the value of the continuous variables.18) This data preprocessing was separately performed for the derivation, interval validation, and external validation data.18) To train the deep-learning algorithm, we input each value of the derivation data in the input layer and adjusted the weight (wk) using back propagation.18)
Development of machine-learning-based algorithm for comparison
We also developed LR and random forest (RF) machine-learning algorithms, for comparison of performance with the DEHF. In previous studies, LR and RF were the most commonly used machine-learning methods and showed better performance than traditional methods in several medical domains.19) We identified the best LR algorithm among all possible algorithms using the glmulti package in R (R Foundation, Vienna, Austria).20),21) We used original Akaike IC as the information criterion and used pairwise interactions. For LR algorithm selection, we used forward-backward directions.
RF is used to construct a multitude of decision trees. Each decision tree partitions the sample data by splitting the variables at discrete cut-points. Each tree is derived by randomly selecting data from the derivation data, and the RF algorithm concludes with a summary result for each decision tree. In this study, the RF algorithm consisted of 10,000 decision trees using the randomForest package in R (R Foundation).21) The optimal number of variables, which were randomly sampled as candidates at each split, was determined using 10-fold cross-validation.
Validation of algorithm performance and statistical analysis
After we developed the deep-learning and machine-learning algorithms, we compared their performance using the internal and external validation data that were not used for algorithm development. We used the area under the receiver operating characteristic curve (AUROC) as the comparative measure. The AUROC is a frequently used metric and the receiver operating characteristic (ROC) curve shows the sensitivity against 1-specificity. We evaluated the 95% confidence interval (CI) using bootstrapping (10,000 times resampling with replacement).22)
We confirmed characteristics of the HF patient group as shown in Table 1. Continuous variables are presented as mean and standard deviation and compared using the unpaired Student's t-test or Mann-Whitney U-test. Categorical variables are expressed as frequencies and percentages and compared using the χ2 test.
Table 1. Baseline characteristics.
| Characteristics | HFrEF (EF≤40%) | HFmrEF (40%≤EF≤50%) | Normal left ventricular systolic function (50%≤EF) | p value* | |
|---|---|---|---|---|---|
| Total patients | 1,391 | 1,538 | 19,836 | ||
| Age (years) | 64.30±14.20 | 64.82±13.30 | 60.83±15.03 | <0.001 | |
| Female | 504 (36.21) | 558 (36.28) | 9,796 (49.38) | <0.001 | |
| Body surface area (m2) | 1.68±0.21 | 1.69±0.20 | 1.68±0.20 | 0.082 | |
| Echocardiography data | |||||
| EF | 27.97±7.36 | 44.07±2.77 | 59.90±6.50 | <0.001 | |
| Left atrial dimension (mm) | 45.84±12.64 | 43.67±9.47 | 40.34±8.46 | <0.001 | |
| Septal dimension (mm) | 10.08±1.87 | 10.61±1.74 | 10.12±1.90 | <0.001 | |
| Posterior wall thickness (mm) | 9.82±1.66 | 10.14±1.60 | 9.73±1.59 | 0.036 | |
| Aortic dimension (mm) | 32.85±4.96 | 33.14±4.53 | 31.60±4.12 | <0.001 | |
| E | 69.32±25.22 | 63.94±21.35 | 65.03±18.56 | <0.001 | |
| A | 65.71±23.73 | 71.78± 20.78 | 70.75±19.58 | <0.001 | |
| Deceleration time | 167.34±59.73 | 191.50±56.06 | 203.87±52.25 | <0.001 | |
| E′ | 4.81±2.11 | 5.37±1.96 | 6.53±2.51 | <0.001 | |
| A′ | 6.26±2.52 | 7.59±2.28 | 8.47±2.13 | <0.001 | |
| E/E′ | 17.35±9.79 | 14.17±8.12 | 11.45±5.71 | <0.001 | |
| Peak TRPG | 27.76±12.18 | 23.59±10.05 | 21.91±7.92 | <0.001 | |
| Estimated PA pressure | 33.75±14.31 | 27.97±11.08 | 25.63±9.05 | <0.001 | |
| Left ventricular systolic dimension (mm) | 46.62±10.98 | 36.23±6.94 | 29.19±5.11 | <0.001 | |
| Left ventricular diastolic dimension (mm) | 57.94±9.55 | 51.03±6.47 | 47.24±5.29 | <0.001 | |
| Total Electrocardiograms | 7,405 | 5,560 | 42,198 | ||
| AF or AFL | 2,010 (27.14) | 1,369 (24.62) | 5,036 (11.93) | <0.001 | |
| Heart rate | 85.41±22.91 | 79.08±20.00 | 73.76±17.66 | <0.001 | |
| QT interval | 410.43±58.77 | 412.54±55.91 | 405.42±46.52 | <0.001 | |
| QTc | 478.00±40.83 | 463.76±41.19 | 442.17±36.75 | <0.001 | |
| QRS duration | 111.95±27.81 | 102.65±23.04 | 96.21±18.36 | <0.001 | |
| R wave axis | 24.19±68.54 | 30.59±56.06 | 37.32±45.62 | <0.001 | |
| T wave axis | 94.04±87.79 | 69.10±81.08 | 49.94±59.54 | <0.001 | |
Data are shown as mean±standard deviation or number (%).
AF = atrial fibrillation; AFL = atrial flutter; EF = ejection fraction, HFrEF = heart failure with reduced ejection fraction; HFmrEF = heart failure with mid-range ejection fraction; PA = pulmonary artery, TRPG = trans-tricuspid pressure gradient.
*An alternative explanation for this p value is based on differences between the 3 groups.
We confirmed the importance of variables in each developed algorithm. We confirmed the deviance difference of each predictive variable in the LR model and mean decrease in Gini coefficient for each predictive variable in RF to assess the importance of the variable. For variable importance in the deep-learning model, we assessed the decrease in accuracy (AUROC) when each variable was excluded.
RESULTS
We included 59,805 ECG studies of 24,376 patients with value of left ventricular systolic function confirmed on echocardiography within 4 weeks. We excluded 4,642 ECG studies of 1,611 patients with missing values. As shown in Figure 1, the study population comprised 22,765 patients, of whom 1,391 had HFrEF. Baseline characteristics of study subjects are shown in Table 1. A deep-learning predictive model was developed using 34,708 ECG studies with derivation data. The performance test was conducted using 9,965 interval validation data from hospital A and 10,790 external validation data from hospital B. We provided the deep-learning algorithm (DEHF), coding book for input data, example of input data, and python code for validation as a supplemental file to this article.
As shown in Table 1, HF patients had a significantly prolonged QT interval and QRS duration, as well as a significantly greater heart rate, longer T wave duration, and significantly shorter R wave duration. HF patients also had a greater proportion with AF/AFL.
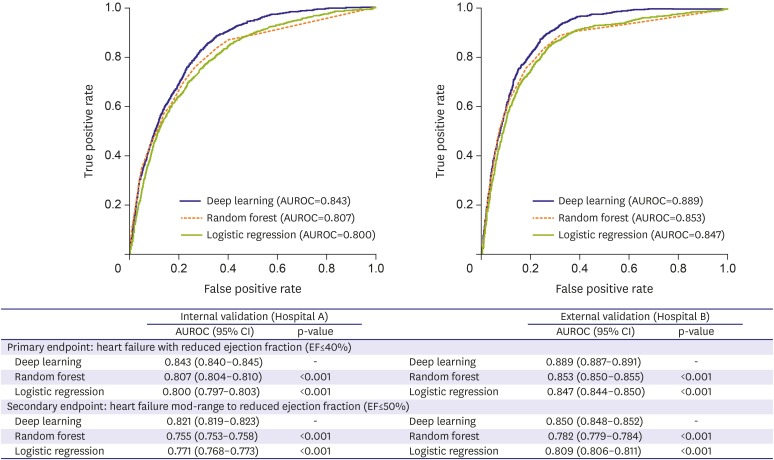
As shown in Figure 3, the ROC curve of the DEHF was above the ROC curve of the other models for the primary and secondary endpoints. This means that the DEHF is more accurate than the other models in all aspects of sensitivity and specificity. During internal validation for identification of the primary endpoint (HFrEF), the AUROC of the deep-learning algorithm, DEHF, was 0.843 (95% CI, 0.840–0.845), and this result significantly outperformed RF (0.807 [0.804–0.810]) and LR (0.800 [0.797–0.803]). In the external validation, the AUROC of the DEHF was 0.889 (0.887–0.891), and this result significantly outperformed the RF (0.853 [0.850–0.855]) and LR (0.847 [0.844–0.850]). The AUROC values of DL were significantly higher than those of RF and LR (p<0.001). At the 90% sensitivity point in external validation, the specificities of DL, RF, and LR were 0.604, 0.587, and 0.487, respectively. As shown in Figure 3, the AUROC values of DL for identification of the secondary endpoint, i.e., mid-range to reduced left ventricular EF (≤50%), were 0.821 (0.819–0.823) and 0.850 (0.848–0.852) for internal and external validation, respectively, and the AUROC value of DL was significantly higher than that of RF or LR (p<0.001).
Figure 3. AUROC of each algorithm for identification of HF.
AUROC = area under the receiver operating characteristic curve; EF = ejection fraction; HF = heart failure; HFrEF = heart failure with reduced ejection fraction; HFmrEF = heart failure with mid-range ejection fraction.
As shown in Table 2, the variable importance was different for each prognostic model. All 3 models used T wave duration as an important predictive variable. While LR and RF used heart rate and QRS duration as important predictive variables, their importance in deep-learning is low. Instead, deep-learning used weight and presence of AF or AFL as important variables.
Table 2. Importance of variables in derivation data for each algorithm.
| Variable importance | LR (deviance difference) | RF (mean decreased Gini) | Deep-learning (difference in AUROC) |
|---|---|---|---|
| 1 | Heart rate (−1,265.7) | T-wave axis (777.0) | T-wave axis (0.103) |
| 2 | T-wave axis (−821.7) | QRS duration (416.0) | Weight (0.087) |
| 3 | QRS duration (−502.6) | Heart rate (299.5) | AF/AFL (0.073) |
| 4 | QT interval (−323.9) | R wave axis (183.4) | Age (0.070) |
| 5 | Sex (−176.8) | Height (76.1) | Heart rate (0.069) |
| 6 | AF/AFL (−106.3) | Age (65.7) | QT interval (0.067) |
| 7 | R-wave axis (−30.1) | QT interval (44.8) | R-wave axis (0.064) |
| 8 | Weight (−29.0) | AF/AFL (44.7) | QRS duration (0.063) |
| 9 | Height (−2.2) | Weight (40.6) | Height (0.061) |
| 10 | Age (−0.4) | Sex (34.4) | Sex (0.055) |
AF = atrial fibrillation; AFL = atrial flutter; AUROC = area under the receiver operating characteristic curve; LR = logistic regression; RF = random forest.
DISCUSSION
This study developed and validated a deep-learning algorithm, DEHF, for identification of HF using ECG. Through validation, this study confirmed that the performance of the deep-learning algorithm was excellent for identification of HF, with greater accuracy than that using RF or LR.
HF has high prevalence, and is associated with increased health care expenses, repeated hospitalization, and significant reduction in quality of life, which may be resolved with rapid diagnosis and effective treatment. Recent guidelines from the American College of Cardiology and American Heart Association4) for the initial diagnosis of HF and referral for echocardiography recommend the use of B-type natriuretic peptide in combination with clinical assessment. These methods, however, require consultations and many tests, as well as a high level of expertise for interpretation of large amounts of complex data and determination of a treatment plan. Furthermore, existing methods are fixed tools that do not account for the relationships among variables and thus provide limited performance for early diagnosis and screening.5),6)
This led to various attempts to use a new method, i.e., machine-learning, for the diagnosis of HF. Deep-learning and machine-learning are branches of artificial intelligence science, a study of algorithms that allows computers to independently collect data and make new predictions. Thus, machine-learning enables computers to establish a new predictive algorithm without direct and explicit input by a human. Son et al.23) and Masetic and Subasi24) developed machine-learning predictive algorithms based on age, sex, blood pressure, and findings of hematology; echocardiography; ECG; radiography; and physical activity in populations ranging from 15 to 4,489 patients, with an AUROC of 0.77 to 0.95 for the accuracy of HF diagnosis. Betanzos et al.25) and Isler26) developed classification algorithms based on the type of HF (HF with preserved EF, mid-range EF, and reduced EF). Melillo et al.27) developed classification algorithms based on the severity of HF. Guidi et al.28) developed a remote care system and a monitoring tool for patients with HF.
Studies to date have shown potential for the diagnosis of HF; however, the fact that they use test results from various modalities limits their use for early diagnosis of HF as a screening tool. Because of this, we developed an identification algorithm using only baseline demographic information and ECG features. We used deep-learning to develop a high-performance algorithm. An important advantage of deep-learning compared with machine-learning is feature learning.14) Machine-learning techniques are limited in their ability to process natural data in their raw form. Machine-learning requires careful engineering to design a feature extractor that transforms the raw data into suitable internal representation. This process requires a lot of manpower, and important information may be missed. On the other hand, deep-learning includes feature learning, which is a set of methods that allows a model to be created using raw data for automatic identification of the features and relationships needed to perform a task.14) It is important to note that feature learning is not designed by humans. As this process is conducted automatically, it is effective at identifying intricate structures in high-dimensional data without information loss and requires very little engineering by humans.14) Therefore, it can be quickly applied to other tasks with ease. Owing to these prospects, deep-learning has been applied in various domains, and shows better performance than all other methods.14)
In general, the predictive accuracy of external validation is lower than that of internal validation. However, in the present study, the accuracy of external validation outperformed internal validation in all predictive models. As shown in the Supplementary Figure 1, hospital A (internal validation) had a greater proportion of HF patients, as well as a greater proportion of patients in bordering areas. This finding may be due to differences in the characteristics of the 2 hospitals (hospital A: a cardiovascular teaching hospital, hospital B: a community general hospital). Therefore, the task of predicting HF using internal validation might be easier than that using external validation.
DEHF, LR, and RF predicted endpoints using different structures. The patients in whom each model correctly predicted the endpoints also differed. Moreover, the variable importance of DEHF is different from that of LR or RF, as shown in Table 2. For this reason, different algorithms can complement each other's weaknesses; thus, many researchers attempt to improve accuracy by combining predictive algorithms. This method, called an ensemble algorithm, is our next area of research.
Several limitations were present in our study. First, deep-learning is considered a black box. Although we can fit the deep-learning algorithm by confirming each weight, we cannot interpret the algorithm in terms of the approach to the decision for a clinical endpoint. For example, if the deep-learning algorithm in this study predicts that a patient has HF, the reason for the prediction cannot be ascertained. Attempts to explain deep-learning are recent, and this will be our next area of study.29) Second, as this study was only conducted in 2 hospitals in Korea, it is necessary to validate this model in HF patients in other countries.30) For this reason, we have provided supplemental files with our deep-learning model (DEHF), data preprocessing method, and code for validation. The deep-learning algorithm can be developed more easily than a machine-learning method. Using our results, other researchers can develop algorithm for their own patients. Third, we did not use raw ECG signals but instead used features of ECG. We aimed for easy application of DEHF in local clinics and general check-ups, but this method could limit the performance of a predictive algorithm. We plan to conduct a study with raw ECG signals for prediction of HF. Despite several limitations, deep-learning has achieved high predictive performance in several medical domains. Medical researchers should investigate the applicability and future development of deep-learning in various domains of medicine.
Competency in medical knowledge: this study developed and validated a DEHF. With this algorithm, we can identify HF using only demographic and ECG features. Many patients can be identified at an early stage and referred for diagnostic investigation. The deep-learning algorithm achieved state-of-the-art performance in identification of HF and outperformed other machine-learning algorithms.
Translational outlook: deep-learning technology has not been widely applied in the medical field. Hence, further investigation and validation are required in various medical fields.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Kwon JM, Jeon KH, Park J.
- Data curation: Kwon JM, Jeon KH, Kim KH, Kim HM, Kim MJ, Lim SM, Song PS, Park J, Oh BH.
- Formal analysis: Kwon JM, Jeon KH, Kim MJ, Lim SM, Choi RK.
- Investigation: Kwon JM.
- Methodology: Kwon JM, Jeon KH, Kim KH, Kim MJ, Choi RK.
- Project administration: Kwon JM.
- Resources: Kwon JM.
- Software: Kwon JM.
- Supervision: Kwon JM, Kim KH.
- Validation: Kwon JM, Jeon KH, Kim KH.
- Visualization: Kwon JM.
- Writing - original draft: Kwon JM, Kim KH.
- Writing - review & editing: Kwon JM, Kim KH, Kim HM, Lim SM, Song PS, Park J, Oh BH.
SUPPLEMENTARY MATERIAL
Distribution of EF in validation groups.
References
- 1.Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol. 2016;13:368–378. doi: 10.1038/nrcardio.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014;1:4–25. doi: 10.1002/ehf2.12005. [DOI] [PubMed] [Google Scholar]
- 3.Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63:1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed] [Google Scholar]
- 4.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776–803. doi: 10.1016/j.jacc.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 5.Bagley SC, White H, Golomb BA. Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol. 2001;54:979–985. doi: 10.1016/s0895-4356(01)00372-9. [DOI] [PubMed] [Google Scholar]
- 6.Breiman L. Statistical modeling: the two cultures. Stat Sci. 2001;16:199–215. [Google Scholar]
- 7.Nainwal A, Kumar Y, Jha B. Morphological changes in congestive heart failure ECG; 2nd International Conference on Advances in Computing, Communication, & Automation (ICACCA); 2016 Sep 30–Oct 1; Fri, India. Bareilly: Institute of Electrical and Electronics Engineers; 2016. [Google Scholar]
- 8.Hendry PB, Krisdinarti L, Erika M. Scoring system based on electrocardiogram features to predict the type of heart failure in patients with chronic heart failure. Cardiol Res. 2016;7:110–116. doi: 10.14740/cr473w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Attia ZI, Kapa S, Lopez-Jimenez F, et al. Screening for cardiac contractile dysfunction using an artificial intelligence-enabled electrocardiogram. Nat Med. 2019;25:70–74. doi: 10.1038/s41591-018-0240-2. [DOI] [PubMed] [Google Scholar]
- 10.Sengupta PP, Kulkarni H, Narula J. Prediction of abnormal myocardial relaxation from signal processed surface ECG. J Am Coll Cardiol. 2018;71:1650–1660. doi: 10.1016/j.jacc.2018.02.024. [DOI] [PubMed] [Google Scholar]
- 11.Johnson KW, Torres Soto J, Glicksberg BS, et al. Artificial intelligence in cardiology. J Am Coll Cardiol. 2018;71:2668–2679. doi: 10.1016/j.jacc.2018.03.521. [DOI] [PubMed] [Google Scholar]
- 12.Ting DS, Cheung CY, Lim G, et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017;318:2211–2223. doi: 10.1001/jama.2017.18152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwon JM, Lee Y, Lee Y, Lee S, Park J. An algorithm based on deep learning for predicting in-hospital cardiac arrest. J Am Heart Assoc. 2018;7:e008678. doi: 10.1161/JAHA.118.008678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–444. doi: 10.1038/nature14539. [DOI] [PubMed] [Google Scholar]
- 15.Pal SK, Mitra S. Multilayer perceptron, fuzzy sets, and classification. IEEE Trans Neural Netw. 1992;3:683–697. doi: 10.1109/72.159058. [DOI] [PubMed] [Google Scholar]
- 16.Nair V, Hinton GE. Rectified linear units improve restricted Boltzmann machines; Proceedings of the 27th International Conference on Machine Learning (ICML-10); 2010 Jun 21–24; Mon, Israel. Haifa: International Machine Learning Society; 2010. [Google Scholar]
- 17.Abadi M, Barham P, Chen J, et al. TensorFlow: a system for large-scale machine learning; Proceedings of the 12th USENIX Symposium on Operating Systems Design and Implementation (OSDI' 16); 2016 Nov 2–4; Wen, USA. Savannah (GA): USENIX Association; 2016. [Google Scholar]
- 18.Jayalakshmi T, Santhakumaran A. Statistical normalization and backpropagation for classification. Int J Comput Theory Eng. 2011;3:89–93. [Google Scholar]
- 19.Shouval R, Hadanny A, Shlomo N, et al. Machine learning for prediction of 30-day mortality after ST elevation myocardial infraction: an acute coronary syndrome Israeli survey data mining study. Int J Cardiol. 2017;246:7–13. doi: 10.1016/j.ijcard.2017.05.067. [DOI] [PubMed] [Google Scholar]
- 20.Calcagno V, de Mazancourt C. Glmulti: an R package for easy automated model selection with (generalized) linear models. J Stat Softw. 2010;34:1–29. [Google Scholar]
- 21.Khalilia M, Chakraborty S, Popescu M. Predicting disease risks from highly imbalanced data using random forest. BMC Med Inform Decis Mak. 2011;11:51. doi: 10.1186/1472-6947-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Stat Med. 2000;19:1141–1164. doi: 10.1002/(sici)1097-0258(20000515)19:9<1141::aid-sim479>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 23.Son CS, Kim YN, Kim HS, Park HS, Kim MS. Decision-making model for early diagnosis of congestive heart failure using rough set and decision tree approaches. J Biomed Inform. 2012;45:999–1008. doi: 10.1016/j.jbi.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Masetic Z, Subasi A. Congestive heart failure detection using random forest classifier. Comput Methods Programs Biomed. 2016;130:54–64. doi: 10.1016/j.cmpb.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Alonso-Betanzos A, Bolón-Canedo V, Heyndrickx GR, Kerkhof PL. Exploring guidelines for classification of major heart failure subtypes by using machine learning. Clin Med Insights Cardiol. 2015;9:57–71. doi: 10.4137/CMC.S18746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Isler Y. Discrimination of systolic and diastolic dysfunctions using multi-layer perceptron in heart rate variability analysis. Comput Biol Med. 2016;76:113–119. doi: 10.1016/j.compbiomed.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 27.Melillo P, De Luca N, Bracale M, Pecchia L. Classification tree for risk assessment in patients suffering from congestive heart failure via long-term heart rate variability. IEEE J Biomed Health Inform. 2013;17:727–733. doi: 10.1109/jbhi.2013.2244902. [DOI] [PubMed] [Google Scholar]
- 28.Guidi G, Pettenati MC, Melillo P, Iadanza E. A machine learning system to improve heart failure patient assistance. IEEE J Biomed Health Inform. 2014;18:1750–1756. doi: 10.1109/JBHI.2014.2337752. [DOI] [PubMed] [Google Scholar]
- 29.Fong RC, Vedaldi A. Interpretable explanations of black boxes by meaningful perturbation. Proc IEEE Int Conf Comput Vis. 2017:3449–3457. [Google Scholar]
- 30.Wolpert DH. The supervised learning no-free-lunch theorems. In: Roy R, Köppen M, Ovaska S, Furuhashi T, Hoffmann F, editors. Soft Computing and Industry. London: Springer; 2002. pp. 25–42. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distribution of EF in validation groups.