Abstract
Objective
To evaluate age-dependent productivity loss caused by menstruation-related symptoms, measured in absenteeism (time away from work or school) and presenteeism (productivity loss while present at work or school).
Methods
Design/setting: internet-based, cross-sectional survey conducted in the Netherlands from July to October 2017.
Participants: 32 748 women aged 15–45 years, recruited through social media.
Outcome measures: self-reported lost productivity in days, divided into absenteeism and presenteeism; impact of menstrual symptoms; reasons women give when calling in sick; and women’s preferences regarding the implications of menstruation-related symptoms for schools and workplaces.
Results
A total of 13.8% (n=4514) of all women reported absenteeism during their menstrual periods with 3.4% (n=1108) reporting absenteeism every or almost every menstrual cycle. The mean absenteeism related to a woman’s period was 1.3 days per year. A total of 80.7% (n=26 438) of the respondents reported presenteeism and decreased productivity a mean of 23.2 days per year. An average productivity loss of 33% resulted in a mean of 8.9 days of total lost productivity per year due to presenteeism. Women under 21 years were more likely to report absenteeism due to menstruation-related symptoms (OR 3.3, 95% CI 3.1 to 3.6). When women called in sick due to their periods, only 20.1% (n=908) told their employer or school that their absence was due to menstrual complaints. Notably, 67.7% (n=22 154) of the participants wished they had greater flexibility in their tasks and working hours at work or school during their periods.
Conclusions
Menstruation-related symptoms cause a great deal of lost productivity, and presenteeism is a bigger contributor to this than absenteeism. There is an urgent need for more focus on the impact of these symptoms, especially in women aged under 21 years, for discussions of treatment options with women of all ages and, ideally, more flexibility for women who work or go to school.
Keywords: menstruation, community gynaecology, menstrual cycle, presenteeism, absenteeism
Strengths and limitations of this study.
This is the largest cohort study to analyse the impact of menstruation-related symptoms on work and school productivity.
The survey was performed among the general female population and is consequently not per se related to one specific gynaecological condition.
Due to the way of recruitment of participants, there may have been some degree of selection bias.
Outcomes are based on self-reported data and consequently lack objectivity regarding productivity loss.
The generalisability of the study may be limited to employment and school systems comparable with the Dutch.
Background
Menstruation-related symptoms (MRSs) are diverse and widespread among women. Symptoms include dysmenorrhoea, heavy menstrual bleeding and premenstrual mood disturbances with reported prevalence of 45%–90%, 14%–25% and 20%–29%, respectively.1–3 Studies show that women with MRSs have lower scores on several domains of quality of life such as general health and physical, mental, social and occupational functioning during their periods.1 4–7 Furthermore, these symptoms may create considerable financial burdens on patients and their families as well as on society.5 6 8–12 Such financial burdens are related to the costs of visits to the doctor, over-the-counter drugs and medical or surgical treatment. However, costs related to productivity loss could be the largest cost driver. Productivity costs are defined as costs associated with paid and unpaid production loss and the replacement of productive people due to illness or disability.13 Productivity costs can be divided into costs related to absenteeism and costs related to presenteeism. Absenteeism represents the total amount of time off work or away from school, and presenteeism represents the loss of productivity while present at a job or school.
Although the literature is scarce and the results are variable, studies on specific patient groups generally show that MRSs can cause absenteeism.14–16 Research on the association between MRSs and presenteeism is even more limited. It has been suggested that research into possible impairments in quality of life caused by menstrual symptoms should not focus on single symptoms but rather on a complex of symptoms that vary widely but that are all related to the menstrual cycle. This complex includes both standard symptoms, like heavy menstrual bleeding and abdominal cramps, and also less common symptoms, like nausea and cold sweats.17 18
Taking all symptoms into account, it seems likely that the real impact of MRSs is underestimated in the general population. Despite being almost two decades into the 21st century, discussions about MRSs may still be rather taboo. This survey-based exploratory study aimed to quantify the burden of MRSs in the general female population, with burden defined as the number of lost days at work or school due to absenteeism and presenteeism. Furthermore, it was aimed to study the impact of specific symptoms on absenteeism and presenteeism.
Methods
This cross-sectional study consisted of an online survey that was distributed from 12 July to 11 October 2017. All data were anonymously collected and stored under the privacy rules of the Radboud University Medical Center. Patients gave informed consent when they initiated the questionnaire.
Patient and public involvement
A group of women, among which were several members of the Dutch Patient Endometriosis Foundation, women with a linguistic education and women with a medical origin, was involved in the conduct of this study at several stages, that is, in the development and dissemination of the questionnaire and in the analysis and interpretation of the results. One of the authors of this manuscript, BDB, is the chair of the Dutch Patient Endometriosis Foundation. Additional contributions are noted in the Acknowledgements section.
Questionnaire development
The questionnaire had several parts, and online supplementary appendix 1 provides details about the questions. Part 1 consisted of questions about each woman’s basic characteristics. Part 2 had questions about menstrual symptoms, and part 3 had questions related to absenteeism and presenteeism. Adaptive questioning was used with a maximum of six questions per page. Participants were asked in a lay manner how long their menstrual cycle was and what the exact meaning of a menstrual cycle was. The duration of the cycle was divided in five categories (25 days or less, 26–30 days, 31–35 days, 36–40 days and 41 days or more). Furthermore, participants could indicate if they had an irregular cycle, meaning more than 10 days difference per cycle, if they were amenorrhoeic due to the use of an intrauterine device (IUD) or the continuous use of oral contraceptives, or the option ‘I do not know’. Additional questions about absenteeism and presenteeism were included that were based on the Productivity Cost Questionnaire from the Institute for Medical Technology Assessment (iMTA-PCQ).19 We modified the iMTA-PCQ-recommended recall period of 4 weeks to 3 months so that it was in line with the relevant time period for this study and so we could include multiple menstrual periods. We assumed the amount of presenteeism to be larger than the amount of absenteeism. Therefore, the recall period for absenteeism was extended to 6 months to maintain accuracy. Visual analogue scales (VAS) were used to quantify the amount of pain, or the intensity of the symptom, and the impairment due to pain or the other symptom. Presenteeism was measured by asking women to what extent they were able to be as productive as possible compared with a day without MRSs. This was scored on a scale from 0 to 10, with 0 being totally unproductive and 10 fully productive. In separate questions, participants were asked to quantify their absenteeism that was related to MRSs and absenteeism for any other reason than MRSs. For the latter, we did not specifically ask the underlying reason.
bmjopen-2018-026186supp001.pdf (332.2KB, pdf)
Target population and recruitment
The study population comprised women between 15 and 45 years old. The upper age limit was chosen to avoid interference from menopausal symptoms; the lower to have a time margin after the average menarche age, since it is known that the first periods are irregular and often accompanied with discomfort and uncertainty. A large number of women were approached with the aim of obtaining a cohort that was representative of the general female population in terms of level of education, medical history and/or gynaecological diagnosis. Women were invited to complete a survey using an online questionnaire tool20 through a campaign on social media platforms Facebook and Twitter. Patient organisations, colleagues and visitors of the Facebook page of one of the authors (TN) were asked to share the link to the questionnaire in order to reach the widest possible audience.
On 12 July 2017, a link to the questionnaire was posted on Facebook and Twitter through the account of one of the authors (TN). In the post, both women with and without MRSs were encouraged to fill in the questionnaire. Within 24 hours of the first posting on social media, over 6000 respondents had filled in the questionnaire, and by July 18, there were 15 000 respondents, which was announced by a repost of the link to the questionnaire. A third post was made on Facebook and Twitter on 16 September 2017, to reach women who may have been on holiday when the first posts were created.
Data analysis
The outcome measures were presented in a descriptive way; we used valid percentages in case of missing values where necessary. We distinguished between women who were mainly working or mainly studying. Therefore, we present these data for two groups, that is, for women who worked more than 5 hours per week (‘working group’) and for women who studied more than 5 hours per week (‘studying group’).
We used binary logistic regression to calculate ORs. Absenteeism and presenteeism were used as dependant variables. As independent variables, we used the following parameters: women younger than 21 versus women aged 21 and older, smoking yes or no, reports of absenteeism not related to MRSs, educational level, the use of oral contraception and the use of an levonorgestrel-releasing IUD. All independent variables were used in an univariate as well as a multivariate analysis. We also studied the association between pain scores and both absenteeism and presenteeism, given that the literature shows that pain scores of 0–4, 5–6 and 7 or higher have a different impact on activity, mood and sleep.21 22 Analyses were performed using IBM SPSS Statistics V.22.00.
Assumptions and transformation of the original data
To present data on level of education in an international format, we had to transform the original data, which was based on the Dutch school system.23 The categorical data of participants’ length of menstrual cycle were transformed into averages.
With regard to the evaluation of absenteeism and presenteeism, ‘the guideline for economic evaluations in healthcare in the Netherlands’ was used.24 A work day accounts for 8 hours. For most sectors in the Netherlands, a full-time work-week is 36 hours. The maximum amount of working hours per year was set at 1558 when they were working full time. We asked women to report their absenteeism due to MRSs per cycle and used a recall period of 6 months.
To calculate the percentages for absenteeism, 1 day of absenteeism accounted for 8 hours of lost productivity. When a woman reported to study or work more than 40 hours per week, we transformed these hours to 40 for reasons of clarity in the calculations and comparability with the data of the Dutch Central Bureau of Statistics (CBS). We made a few other transformations for categorical data. For absenteeism related to MRSs, the category ‘more than three days per cycle’ was considered to be 4 days per cycle. For absenteeism that was not related to MRSs, the category ‘more than ten days in the past six months’ was considered to be 11 days in the past 6 months.
To present yearly data, we multiplied some of these data based on the original recall period. The number of days for absenteeism related to MRSs was based on days per cycle, which were therefore multiplied by 12.7 based on the reported average menstrual cycle of 28.8 days (see table 1). These values were then multiplied by one if the woman reported that she called in sick ‘every period’, 0.75 if she reported ‘almost every period’, 0.5 if she reported ‘half of all periods’ and 0.25 if she reported calling in sick ‘only once in a while’. Values for absenteeism that was not related to MRS were based on a recall period of 6 months and were therefore multiplied by two in order to obtain the number of days per year. The values for presenteeism were based on a recall period of 3 months and were therefore multiplied by four.
Table 1.
Basic characteristics of study participants (n=32 748)
| Number (percentage) | Mean±SD | Median | |
| Age, years | 28.6±8.6 | 28 | |
| 15–19 | 6141 (18.8) | ||
| 20–24 | 6118 (18.7) | ||
| 25–29 | 5825 (17.8) | ||
| 30–34 | 5483 (16.7) | ||
| 35–40 | 4687 (14.3) | ||
| 41–45 | 4494 (13.7) | ||
| Level of education | |||
| Low | 4020 (12.3) | ||
| Medium | 12 335 (37.9) | ||
| High | 16 229 (49.8) | ||
| Hours/week | |||
| Paid work | 21.7±14.7 | 24 | |
| Study | 7.4±13.6 | 0 | |
| Voluntary work | 0.8±3.1 | 0 | |
| Menstrual cycle | |||
| Regular cycle | 25 717 (78.5) | ||
| Duration | 28.8±3.0 | 28 | |
| Amenorrhoea due to LG-IUD/OC | 3675 (11.2) | ||
| Irregular, variation >10 days per cycle | 2495 (7.6) | ||
| Do not know | 861 (2.6) | ||
| Days with blood loss per cycle | 5.4±1.6 | 5 | |
| Visited a doctor for MRSs | |||
| No | 17 873 (54.6) | ||
| Yes, general practitioner | 10 141 (31.0) | ||
| Yes, gynaecologist | 4698 (14.4) | ||
| Diagnosis for MRSs* | |||
| No | 29 731 (90.8) | ||
| Yes | 3017 (9.2) | ||
| Endometriosis | 1120 (3.4) | ||
| PCOS | 588 (1.8) | ||
| Adenomyosis | 103 (0.3) | ||
| Fibroids | 275 (0.8) | ||
| Other | 1901 (5.8) | ||
| Contraception* | |||
| Hormonal contraception | 11 993 (36.6) | ||
| OC | 8650 (26.4) | ||
| LG-IUD | 2752 (8.4) | ||
| Other hormonal: injection, transdermal and so on | 882 (2.7) | ||
| No hormonal contraception | 20 755 (63.4) | ||
| Cu-IUD | 771 (2.4) | ||
| Female sterilisation | 423 (1.3) | ||
| No female contraception | 19 639 (60.0) | ||
| Nulliparous | 21 585 (66.0) | ||
| Paid work >5 hours a week | 26 104 (79.7) | ||
| Age | 29.7±8.3 | 29 | |
| Hours of paid work/week | 27.0±11.4 | 28 | |
| Hours spent on study/week | 7.5±13.4 | 0 | |
| >40 hours of paid work/week | 1047 (3.2) | ||
| Study >5 hours a week | 8764 (26.8) | ||
| Age | 22.0±6.2 | 20 | |
| Hours spent on study/week | 27.4±12.1 | 30 | |
| Hours of paid work/week | 15.5±11.3 | 12 | |
| >40 hours spent on study/week | 322 (1.0) |
Mean duration of cycle based on women with a regular cycle.
*More than one answer possible.
Cu-IUD, copper intrauterine device; LG-IUD, levonorgestrel-releasing intrauterine device; MRSs, menstruation-related symptoms; PCOS, polycystic ovary syndrome; OC, oral contraceptive.
Results
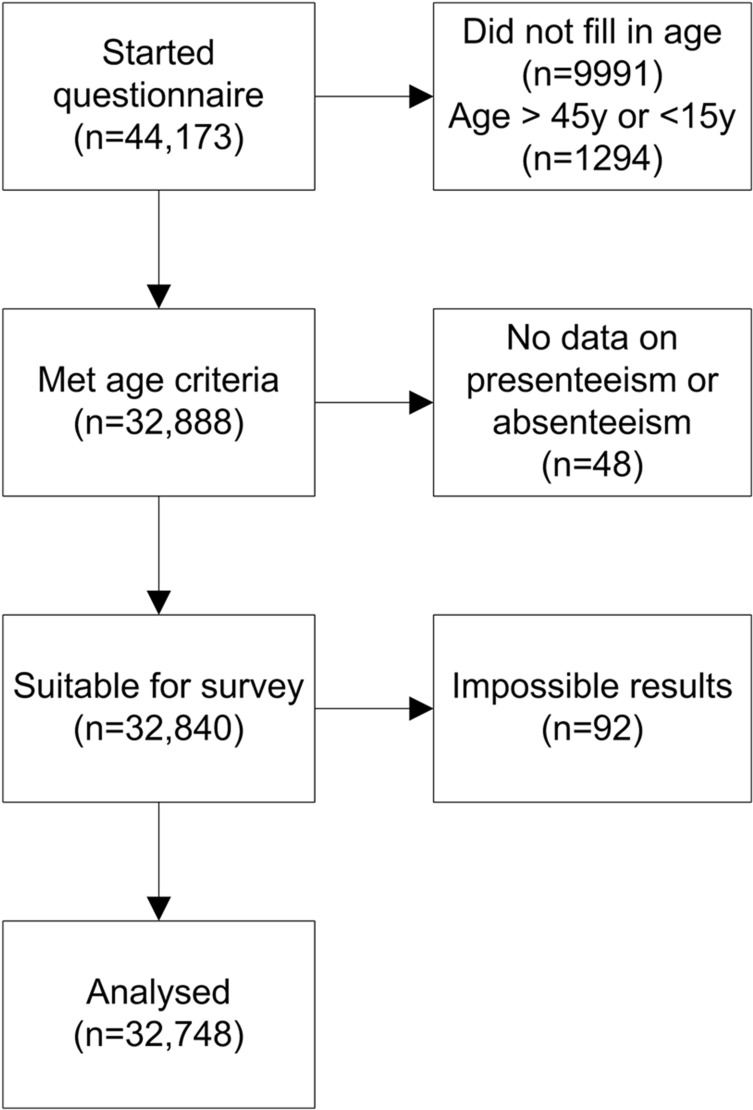
A total of 44 173 women initiated the questionnaire. We excluded participants who did not report a date of birth or whose age did not fulfil the inclusion criteria (figure 1). There were no duplicates of IP addresses. Women who did not answer questions related to absenteeism and presenteeism were excluded. Furthermore, cases with impossible results (eg, 10 000 000 days of presenteeism in 3 months or 140 changes of sanitary pads a day) were excluded. This resulted in a total of 32 748 women in the final analysis.
Figure 1.
Flow chart for the respondents.
Table 1 summarises the basic characteristics of the participants. We found that 45.4% (n=14 839) had visited a doctor for menstrual complaints in the past, with a total of 3017 (9.2%) women reporting a diagnosis of a menstrual disorder, such as endometriosis or fibroids.
The mean age of women in the working group was higher than the mean ager of women in the studying group. The mean number of working hours per week in the working group was 27.0 (SD 11.4), and the mean number of study hours in the studying group was 27.4 (SD 12.1). A total of 7335 women (22.4%) reported both working and studying more than 5 hours per week. In this group, 3001 women were working more than 16 hours a week, and 5284 women in the study group were studying more than 16 hours a week.
Absenteeism
Table 2 shows the results on absenteeism due to MRSs. Although 13.8% of the women (n=4514) reported absenteeism due to MRSs, only 1108 women (3.4%) reported absenteeism every cycle or almost every cycle. The percentage of absenteeism in every cycle or almost every cycle was 2.4% in the working group and 4.5% in the studying group. The mean absenteeism due to MRSs was 0.9 days per year for the working group and 1.6 day per year for the study group.
Table 2.
Reported absenteeism caused by menstruation-related symptoms
| Number (percentage) | Mean±SD | |
| All (n=32 748) | ||
| Absenteeism | 4514 (13.8) | |
| ≤0.5 day | 538 (1.6) | |
| 1 day | 2259 (6.9) | |
| 2 days | 1171 (3.6) | |
| 3 days | 349 (1.1) | |
| >3 days | 184 (0.6) | |
| Total days of absenteeism per year | 1.3±5.9 | |
| Work (n=26 104) | ||
| Absenteeism | 2926 (11.2) | |
| ≤0.5 day | 374 (1.4) | |
| 1 day | 1476 (5.7) | |
| 2 days | 757 (2.9) | |
| 3 days | 211 (0.8) | |
| >3 days | 98 (0.4) | |
| Total days of absenteeism per year | 0.9±3.9 | |
| Study (n=8764) | ||
| Absenteeism | 1715 (19.6) | |
| ≤0.5 day | 234 (2.7) | |
| 1 day | 921 (10.5) | |
| 2 days | 423 (4.8) | |
| 3 days | 92 (1.0) | |
| >3 days | 41 (0.5) | |
| Total days of absenteeism per year | 1.6±5.0 |
Women were asked to report the average amount of days on which they were absent due to menstruation-related symptoms per cycle. The total days of absenteeism per year was calculated. The added numbers of women in the work and study group exceed the total amount of participants, since 2120 women reported to both study and work more than 5 hours/week.
We also calculated the mean total absenteeism that was not related to MRSs. For the entire group, this was 3.3 days per year; for the working group, it was 3.5 days, and for the studying group, it was 4.3 days. The mean percentage of absenteeism that was not related to MRSs was 3.5% in the working group and 3.7% in the studying group. Consequently, absenteeism due to MRSs in our cohort accounted for, on average, 22% of the total absenteeism in the working group and 24% in the studying group.
Presenteeism
Table 3 shows the numbers reported for presenteeism. Over 80 % of all women reported presenteeism during their periods. The differences between the working group and the study group were not large in terms of prevalence and lost productivity. The mean number of lost productive days per year due to presenteeism was more than sevenfold greater than the mean number of lost productive days due to absenteeism.
Table 3.
Reported presenteeism caused by menstruation-related symptoms
| Number (percentage) | Mean±SD | Median | |
| All (n=32 748) | |||
| Presenteeism | 26 438 (80.7) | ||
| Number of days in the past 3 months | 5.8±5.3 | 5.0 | |
| Percentage of productivity loss per day | 33.0±24.8 | 30.0 | |
| Days/year of lost productivity | 8.9±11.0 | 5.6 | |
| Work (n=26 104) | |||
| Presenteeism | 21 252 (81.4) | ||
| Number of days in the past 3 months | 5.7±5.2 | 5.0 | |
| Percentage of productivity loss per day | 31.7±24.7 | 30.0 | |
| Days/year of lost productivity | 8.4±10.6 | 4.8 | |
| Study (n=8764) | |||
| Presenteeism | 7385 (84.3) | ||
| Number of days in the past 3 months | 6.3±5.3 | 5.0 | |
| Percentage of productivity loss per day | 36.8±24.2 | 40.0 | |
| Days/year of lost productivity | 10.5±11.8 | 7.2 |
Women were asked to report the amount of days on which they were less productive and to what extent. The total days of lost productivity per year was calculated. The added numbers of women in the work and study group exceed the total amount of participants, since 2120 women reported to both study and work more than 5 hours/week.
Note that the values presented in days/year of lost productivity do not add up exactly, since these data were calculated on an individual basis and are not the result of merely multiplying the two averages.
Factors associated with absenteeism and presenteeism
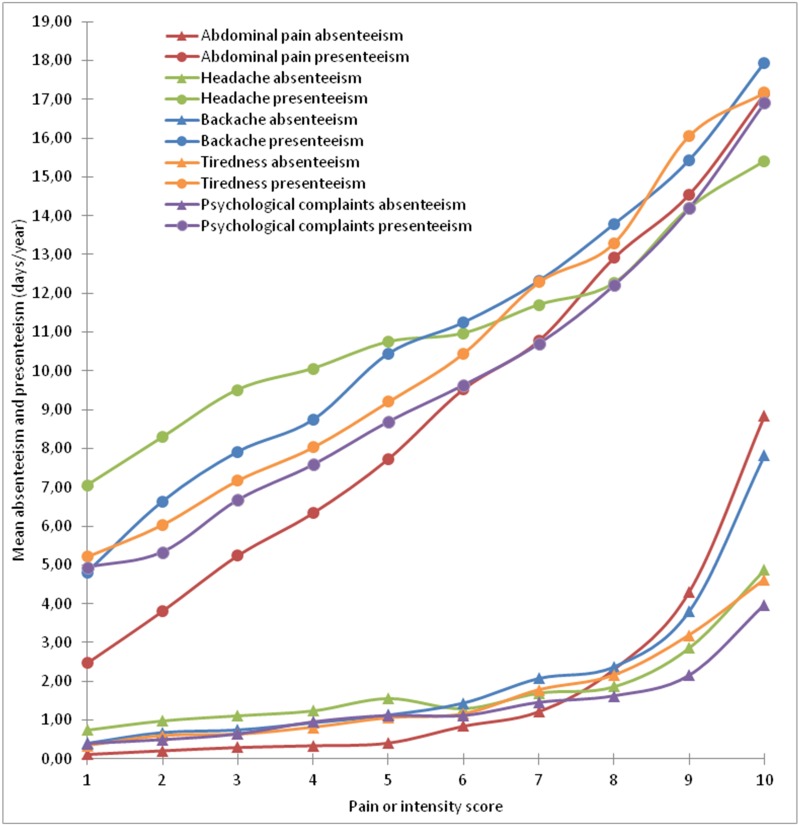
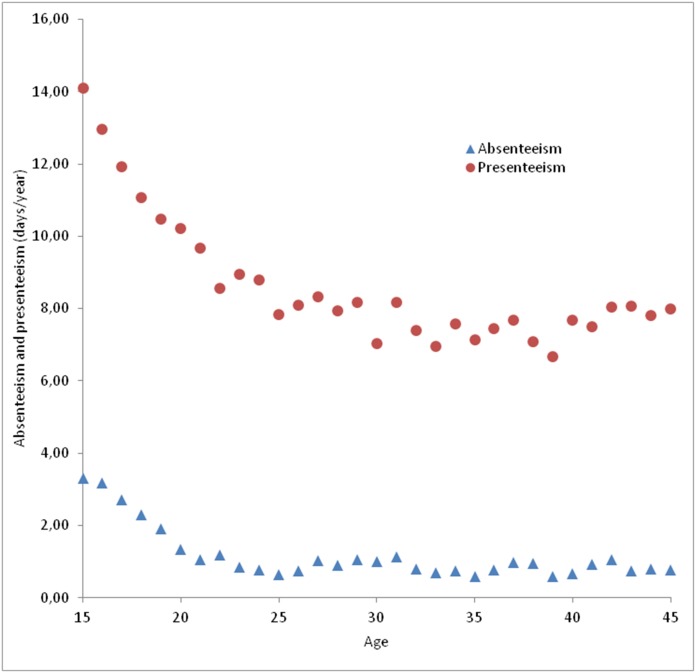
Figure 2 shows the association between reported pain or discomfort scores and both absenteeism and presenteeism. As seen in detail in table 4, high VAS scores were significantly associated with higher levels of absenteeism and presenteeism. The strongest relationship was found for abdominal pain scores that were seven or higher on a scale from 0 to 10. ORs were 5.6 for absenteeism (95% CI 5.0 to 6.2) and 8.8 for presenteeism (95% CI 8.1 to 9.5). Figure 3 shows the association between age and both presenteeism and absenteeism. As shown in both figure 3 and table 4, we found that younger women showed significantly higher rates of absenteeism and presenteeism. A levonorgestrel-releasing IUD is associated with especially less presenteeism.
Figure 2.
The relationship between pain and intensity scores, related to absenteeism and presenteeism, in lost days per year.
Table 4.
ORs and 95% CIs for factors related to absenteeism and presenteeism
| Absenteeism | Presenteeism | |||
| OR (95% CI) | OR after correction (95% CI) | OR (95% CI) | OR after correction (95% CI) | |
| Age <21 years* | 3.7 (3.4 to 3.9) | 3.3 (3.1 to 3.6) | 1.4 (1.3 to 1.5) | 1.3 (1.2 to 1.4) |
| Smoking† | 1.3 (1.2 to 1.5) | 1.3 (1.2 to 1.4) | 1.5 (1.3 to 1.6) | 1.4 (1.3 to 1.6) |
| Absenteeism not related to MRSs in the past 6 months‡ | 2.2 (2.1 to 2.4) | 1.7 (1.6 to 1.9) | 1.4 (1.3 to 1.5) | 1.3 (1.2 to 1.4) |
| Level of education§ | ||||
| Low | 4.5 (4.1 to 4.9) | 2.7 (2.4 to 3.0) | 1.3 (1.2 to 1.4) | 1.1 (1.0 to 1.2)** |
| Medium | 2.2 (2.1 to 2.4) | 1.7 (1.5 to 1.8) | 1.3 (1.2 to 1.4) | 1.2 (1.1 to 1.2) |
| High | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| Oral contraception¶ | ||||
| No | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| Yes | 1.2 (1.1 to 1.3) | 1.0 (0.9 to 1.1)†† | 0.9 (0.9 to 1.0) | 0.9 (0.8 to 0.9) |
| LG-IUD¶ | ||||
| No | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| Yes | 0.7 (0.6 to 0.8) | 0.9 (0.8 to 1.0) | 0.5 (0.5 to 0.6) | 0.5 (0.5 to 0.6) |
| Abdominal pain score¶ | ||||
| 0–4 | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| 5–6 | 2.6 (2.3 to 2.9) | 2.2 (1.9 to 2.4) | 5.2 (4.8 to 5.7) | 5.3 (4.9 to 5.7) |
| >7 | 7.0 (6.4 to 7.8) | 5.6 (5.0 to 6.2) | 8.7 (8.0 to 9.4) | 8.8 (8.1 to 9.5) |
| Headache pain score¶ | ||||
| 0–4 | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| 5–6 | 1.5 (1.3 to 1.6) | 1.5 (1.4 to 1.6) | 3.0 (2.7 to 3.3) | 3.1 (2.8 to 3.4) |
| >7 | 2.0 (1.8 to 2.1) | 2.3 (2.1 to 2.5) | 3.5 (3.2 to 3.9) | 3.7 (3.4 to 4.1) |
| Backache pain score¶ | ||||
| 0–4 | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| 5–6 | 1.6 (1.5 to 1.7) | 1.4 (1.3 to 1.5) | 3.5 (3.2 to 3.9) | 3.5 (3.2 to 3.8) |
| >7 | 2.7 (2.5 to 2.9) | 2.2 (2.1 to 2.4) | 4.7 (4.2 to 5.2) | 4.5 (4.0 to 5.0) |
| Tiredness intensity score¶ | ||||
| 0–4 | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| 5–6 | 1.8 (1.7 to 2.0) | 1.8 (1.6 to 2.0) | 3.3 (3.1 to 3.6) | 3.3 (3.1 to 3.6) |
| >7 | 3.0 (2.8 to 3.2) | 2.8 (2.6 to 3.1) | 5.1 (4.7 to 5.6) | 5.2 (4.7 to 5.7) |
| Psychological complaints intensity score¶ | ||||
| 0–4 | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) | 1.0 (n/a) |
| 5–6 | 1.6 (1.5 to 1.7) | 1.5 (1.4 to 1.7) | 2.7 (2.5 to 2.9) | 2.6 (2,5 to 2.9) |
| >7 | 2.2 (2.0 to 2.4) | 2.1 (2.0 to 2.3) | 4.4 (4.0 to 4.7) | 4.3 (4.0 to 4.7) |
ORs >1 correlate with a higher prevalence of absenteeism or presenteeism. ORs <1 correlate with a lower prevalence of absenteeism or presenteeism.
*Correction for smoking and absenteeism that was not related to menstruation-related symptoms (MRSs).
†Correction for age, absenteeism that was not related to MRSs and level of education.
‡Correction for age, smoking and level of education.
§Correction for age, smoking and absenteeism that was not related to MRSs.
¶Correction for age, smoking, absenteeism that was not related to MRSs and level of education.
**P=0.26, ††p=0.73 for all other ORs, p<0.05.
LG-IUD, levonorgestrel-releasing intrauterine device.
Figure 3.
The relationship between age and average absenteeism and presenteeism.
Menstruation and suggested implications for schools and workplaces
From the respondent who had been calling in sick due to MRSs, 20.1% (n=908) told their employer or school menstrual symptoms were the reason, 46.4% (n=2092) only mentioned the presenting symptom. No reason was given by 27.7% (n=1250), while 5.8% (n=260) made up another reason. Comparing women aged below 21 years with women aged 21 years and above, we found that younger women were less open about their MRSs being the reason for calling in sick (12.0%) versus women older than 21 (27.0%). Women were asked to report suggestions on how work places and conditions could be changed in order for them to function better during their menstrual periods. There were 32 708 responses to this multiple-choice question, to which each woman could give more than one answer. The majority of women (67.7%, n=22 154) preferred more flexibility during their periods, such as the possibility of doing less physical work (32.1%, n=10 499), the ability to work from home (39.5%, n=12 917), more time for personal care (28.3%, n=9241) or the ability to take a day off and make up for it later (11.5%, n=3756). In addition, 32.9% wished they could take a complete day off without any consequences. A percentage of 27.2 (n=8890) did not wish for any changes in policy. Many women (79.7%, n=26 072) were open to discussing MRSs with their company doctor, and 56.7% (n=18 579) thought that doing so would draw more attention to MRS-related matters.
Discussion
This survey-based study showed that menstruation-related absenteeism and, to a greater extent, presenteeism are widespread in the general female population. In our cohort, MRSs accounted for up to 24% of total absenteeism for women who were working and studying. The annual productivity loss due to presenteeism was sevenfold times more than the annual productivity loss due to absenteeism, and women younger than 21 years experience the largest burden. Symptom severity scores showed significant and strong associations with both absenteeism and presenteeism. When women called in sick due to MRSs, only one in five stated openly that menstrual symptoms were the main reason. A majority of women prefers more flexibility during their periods when it comes to work or school.
There have been few studies on absenteeism and presenteeism related to MRSs in the general female population. To our knowledge, Tanaka’s study25 is the only other published study on absenteeism and presenteeism due to MRSs in the general female population. In a cohort of 19 254 Japanese women, a total of 3311 (17.2%) reported work productivity lost in the prior 3 months, mostly in the form of decreased efficiency (62.0%, n=2052). Of these 2052 subjects, the mean number of workdays lost due to decreased efficiency was 5.7 days in 3 months. After recalculation, this accounts for 2.4 days per year for the entire population. This is fewer days than the 8.9 days per year in our cohort. However, the numbers for absenteeism were more similar, with a mean of 1.0 day of absenteeism per year in the entire Japanese cohort compared with 1.3 days in our cohort. Differences in regulations of social services, a difference in attitude towards sick leave and a different method of data collection might explain these differences. It has been suggested in research on musculoskeletal symptoms that rates of absenteeism might be lower in Japan compared with European countries and the USA. Consequently, presenteeism might therefore be a more representative variable.26 27
More data are available regarding the impact of dysmenorrhoea on quality of life and absenteeism. De Sanctis et al reviewed studies on dysmenorrhoea in multiple countries, some of which included menstruation-related absenteeism data.14 They found that the prevalence of school absences in adolescents that was due to dysmenorrhoea varied between 7.7% and 57.8%. Since the review included 41 140 women in 27 countries, and there was a high degree of heterogeneity in the outcome measures, no firm conclusions could be drawn. Hailemeskel et al evaluated 440 female university students in Ethiopia.28 Among students with dysmenorrhoea, 66.8% reported a loss of concentration in class, and 56.3% reported class absences during the last month. In a questionnaire-based study of 706 Hispanic female adolescents, 38% reported missing school due to dysmenorrhoea during the 3 months prior to the survey, and 59% reported a decrease in concentration in class due to dysmenorrhoea.29
Absenteeism and presenteeism due to endometriosis in other studies was greater than in our study, which was not surprising.9 14 30 However, some interesting parallels can be drawn to findings from a recent study by Soliman et al.14 They found that the average number of hours of presenteeism, 5.3 hours per week, was far greater than the number of hours of absenteeism, which was 1.1 hours per week. Furthermore, younger women had significantly higher levels of lost productivity than their older counterparts, and more severe symptoms were associated with more absenteeism and presenteeism. This was in line with our findings, since we also found higher rates of both absenteeism and presenteeism in younger women. A taboo on talking openly about MRS, undertreatment and less flexibility at school might be possible explanations for these differences. Comparing our outcomes with studies on other non-gynaecological conditions is hard due to differences in methods and presentation of findings and the cyclic character of MRSs. However, the incidence of presenteeism seems to be as high as it is in patients with inflammatory bowel disease.31 Moreover, the amount of impairment is comparable with severe gastro-oesophageal reflux (31.9%), moderate irritable bowel syndrome (36.6%) and allergic rhinitis (33.4%–39.8%)%).32
Our finding that only 20.1% of women were open about their menstrual symptoms as a reason for calling in sick may confirm the general idea that women tend not to speak openly about MRSs. Wong et al found that in a cohort of schoolgirls in Malaysia, 76.1% considered dysmenorrhoea a normal part of the menstrual cycle.15 In the context of the findings noted above, our study also suggests there is a taboo for women in terms of discussing menstrual problems with their employers. The latter may therefore conclude that the impact of MRSs on their employees is negligible. Considering the fact that we also found that 68% of women wish that they had greater flexibility during their periods, either at school or at work, more openness about MRSs in the employment setting seems desirable. The reasons underlying this taboo are likely to have a historical basis; indeed, since ancient times, menstruation has been surrounded with mythical stories and has not been well understood. However, in recent years, the lay literature in developed countries has focused more attention on MRSs.33–35 The prevalence and the impact of MRSs on the general population and the number of women who are asking for a different approach all reflect the need to change the view of menstrual symptoms and the way they are addressed in society.
This study consisted of a large cohort, and it reached a large number of women within the age range that was aimed for. The questionnaire was developed in collaboration with patient representatives to make it understandable by and relevant to most women. The cohort appeared to be a representative sample of the general female population based on the number of working hours.33 When we compare our data with the national registries, the total amount of absenteeism is found to be comparable, regardless of whether it was related to MRSs.36 37 It is difficult to compare our numbers on women with a diagnosis explaining their MRSs with numbers found in other studies. We found that only 9% of the participants had such a diagnosis, which seems about as expected or even somewhat low.3 38–40 In contrast, 45% of the women in the study reported consulting a physician for their MRSs. This number was relatively high compared with other studies in which, for example, the percentage of women with dysmenorrhoea who sought medical advice was approximately 15%.15 16 An important factor might be the Dutch health system in which general practitioners are available free of charge. Women with a low level of education were relatively under-represented.41 As our results show, especially absenteeism related to MRSs is associated with a low level of education, and this might have biased our results. We expect women with lower educational levels to do more physical jobs or jobs with less flexibility. Therefore, our findings on work productivity loss might be underestimated. However, our finding could be overestimated due to the possibility that women with more MRSs might be more likely to respond to a questionnaire, as it may seem more relevant to them. Moreover, we were not able to provide data on presenteeism not related to MRSs nor were we able to correct for comorbid health conditions. Thus, these results must be interpreted with caution. Due to the way that the questionnaire was distributed through social media, there may have been some selection bias. However, a recent review stated that Facebook is a useful recruitment tool for healthcare research.42 Although we did not use a validated questionnaire, our most important outcomes were based on questions derived from the PCQ, which itself is based on validated questions and which is recommended by guidelines for cost research.24 Self-reported absenteeism generally shows a good correlation with official records, although accuracy decreases with increasing recall period.43 This might have initiated a recall bias in our cohort. It is unknown to what extend recall bias affects reports on presenteeism.44 In general, although results vary among studies on premenstrual complaints, a prospective collection of data on symptoms is advisable.45 46 Furthermore, an extrapolation of a 3-month and 6-month timeframe to a yearly basis may intrinsically imply some degree of uncertainty, for example, when the influenza season is not included in the original analysis. Finally, these results may not be generalised internationally due to variability in the regulation of social services in different countries, and this is also a limitation of our study. In he Netherlands, wages are paid during sick leave that has duration of less than 1 year, but women in other countries may not have this benefit. Since we know that many factors influence menstrual symptoms, including biological, cultural, and environmental factors, these differences might well influence both absenteeism and presenteeism.6 14 47
In conclusion, we have found that the impact of MRSs on work and school productivity is considerable and that presenteeism contributes significantly more to the matter than absenteeism. Future research should identify how women affected by MRSs could be helped best and how their productivity can be improved in order to reduce the societal impact regarding absenteeism and presenteeism.
Supplementary Material
Acknowledgments
The authors would like to thank Reinoud Oomen, Peter de Vroed, Steven Giesbers, Elsbeth Teeling, Paula Kragten and Annemarie Haverkamp for their valuable contributions in the development and dispersion of the questionnaire.
Footnotes
Contributors: TEN, BDB and JWMA conceived the study. MES wrote the first and successive drafts of the manuscript. MES, TEN and EMMA modelled and analysed the data. TEN, EMMA, JWMM, BDB and JWMA contributed to study conception and design. MES and TEN collected the data. All authors revised the manuscript for important intellectual content. MES and TEN had full access to the data and take responsibility for the integrity of the data and the accuracy of the data analysis. TEN is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: Approval for this study was obtained from the local medical ethics committee ‘Commissie Mensgebonden Onderzoek (CMO)’ under number file number 2017–3387 on 12 July 2017.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data from this study are available from a repository. Data are available on request from the corresponding author.
Patient consent for publication: Not required.
References
- 1. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update 2015;21:762–78. 10.1093/humupd/dmv039 [DOI] [PubMed] [Google Scholar]
- 2. Yonkers KA, Simoni MK. Premenstrual disorders. Am J Obstet Gynecol 2018;218:68–74. 10.1016/j.ajog.2017.05.045 [DOI] [PubMed] [Google Scholar]
- 3. Shapley M, Jordan K, Croft PR. An epidemiological survey of symptoms of menstrual loss in the community. Br J Gen Pract 2004;54:359–63. [PMC free article] [PubMed] [Google Scholar]
- 4. Liu Z, Doan QV, Blumenthal P, et al. . A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health 2007;10:183–94. 10.1111/j.1524-4733.2007.00168.x [DOI] [PubMed] [Google Scholar]
- 5. Rapkin AJ, Winer SA. Premenstrual syndrome and premenstrual dysphoric disorder: quality of life and burden of illness. Expert Rev Pharmacoecon Outcomes Res 2009;9:157–70. 10.1586/erp.09.14 [DOI] [PubMed] [Google Scholar]
- 6. Knox B, Azurah AG, Grover SR. Quality of life and menstruation in adolescents. Curr Opin Obstet Gynecol 2015;27:309–14. 10.1097/GCO.0000000000000199 [DOI] [PubMed] [Google Scholar]
- 7. Peuranpää P, Heliövaara-Peippo S, Fraser I, et al. . Effects of anemia and iron deficiency on quality of life in women with heavy menstrual bleeding. Acta Obstet Gynecol Scand 2014;93:654–60. 10.1111/aogs.12394 [DOI] [PubMed] [Google Scholar]
- 8. Jensen JT, Lefebvre P, Laliberté F, et al. . Cost burden and treatment patterns associated with management of heavy menstrual bleeding. J Womens Health 2012;21:539–47. 10.1089/jwh.2011.3147 [DOI] [PubMed] [Google Scholar]
- 9. Fourquet J, Báez L, Figueroa M, et al. . Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil Steril 2011;96:107–12. 10.1016/j.fertnstert.2011.04.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Klein S, D’Hooghe T, Meuleman C, et al. . What is the societal burden of endometriosis-associated symptoms? a prospective Belgian study. Reprod Biomed Online 2014;28:116–24. 10.1016/j.rbmo.2013.09.020 [DOI] [PubMed] [Google Scholar]
- 11. Heinemann LA, Minh TD, Filonenko A, et al. . Explorative evaluation of the impact of severe premenstrual disorders on work absenteeism and productivity. Womens Health Issues 2010;20:58–65. 10.1016/j.whi.2009.09.005 [DOI] [PubMed] [Google Scholar]
- 12. Frick KD, Clark MA, Steinwachs DM, et al. . Financial and quality-of-life burden of dysfunctional uterine bleeding among women agreeing to obtain surgical treatment. Womens Health Issues 2009;19:70–8. 10.1016/j.whi.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 13. Krol M, Brouwer W, Rutten F. Productivity costs in economic evaluations: past, present, future. Pharmacoeconomics 2013;31:537–49. 10.1007/s40273-013-0056-3 [DOI] [PubMed] [Google Scholar]
- 14. Soliman AM, Coyne KS, Gries KS, et al. . The Effect of Endometriosis Symptoms on Absenteeism and Presenteeism in the Workplace and at Home. J Manag Care Spec Pharm 2017;23:745–54. 10.18553/jmcp.2017.23.7.745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wong LP. Attitudes towards dysmenorrhoea, impact and treatment seeking among adolescent girls: a rural school-based survey. Aust J Rural Health 2011;19:218–23. 10.1111/j.1440-1584.2011.01213.x [DOI] [PubMed] [Google Scholar]
- 16. De Sanctis V, Soliman AT, Elsedfy H, et al. . Dysmenorrhea in adolescents and young adults: a review in different country. Acta Biomed 2017;87:233–46. [PMC free article] [PubMed] [Google Scholar]
- 17. Collins Sharp BA, Taylor DL, Thomas KK, et al. . Cyclic perimenstrual pain and discomfort: the scientific basis for practice. J Obstet Gynecol Neonatal Nurs 2002;31:637–49. 10.1177/0884217502239207 [DOI] [PubMed] [Google Scholar]
- 18. Monagle L, Dan A, Krogh V, et al. . Perimenstrual symptom prevalence rates: an Italian-American comparison. Am J Epidemiol 1993;138:1070–81. 10.1093/oxfordjournals.aje.a116825 [DOI] [PubMed] [Google Scholar]
- 19. Bouwmans C, Krol M, Severens H, et al. . The iMTA Productivity Cost Questionnaire: A Standardized Instrument for Measuring and Valuing Health-Related Productivity Losses. Value Health 2015;18:753–8. 10.1016/j.jval.2015.05.009 [DOI] [PubMed] [Google Scholar]
- 20. Surveymonkey. Surveymonkey, software for online surveys. 2018. http://www.surveymonkey.net
- 21. Bodian CA, Freedman G, Hossain S, et al. . The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology 2001;95:1356–61. [DOI] [PubMed] [Google Scholar]
- 22. Serlin RC, Mendoza TR, Nakamura Y, et al. . When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995;61:277–84. 10.1016/0304-3959(94)00178-H [DOI] [PubMed] [Google Scholar]
- 23. UNESCO Institute for Statistics U. International Standard Classification of Education ISCED 2012;2011. [Google Scholar]
- 24. Institution DH. Zorginstituut Nederland) D. Guideline for the execution of economic evaluations in healthcare. Richtlijn voor het uitvoeren van economische evaluaties in de gezondheidszorg) 2016. https://www.zorginstituutnederland.nl/publicaties/publicatie/2016/02/29/richtlijn-voor-het-uitvoeren-van-economische-evaluaties-in-de-gezondheidszorg [Google Scholar]
- 25. Tanaka E, Momoeda M, Osuga Y, et al. . Burden of menstrual symptoms in Japanese women: results from a survey-based study. J Med Econ 2013;16:1255–66. 10.3111/13696998.2013.830974 [DOI] [PubMed] [Google Scholar]
- 26. Nakata K, Tsuji T, Vietri J, et al. . Work impairment, osteoarthritis, and health-related quality of life among employees in Japan. Health Qual Life Outcomes 2018;16:64 10.1186/s12955-018-0896-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Matsudaira K, Palmer KT, Reading I, et al. . Prevalence and correlates of regional pain and associated disability in Japanese workers. Occup Environ Med 2011;68:191–6. 10.1136/oem.2009.053645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hailemeskel S, Demissie A, Assefa N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: evidence from female university students in Ethiopia. Int J Womens Health 2016;8:489–96. 10.2147/IJWH.S112768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med 2000;154:1226–9. 10.1001/archpedi.154.12.1226 [DOI] [PubMed] [Google Scholar]
- 30. Nnoaham KE, Hummelshoj L, Webster P, et al. . Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 2011;96:366–73. 10.1016/j.fertnstert.2011.05.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Büsch K, da Silva SA, Holton M, et al. . Sick leave and disability pension in inflammatory bowel disease: a systematic review. J Crohns Colitis 2014;8:1362–77. 10.1016/j.crohns.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 32. Cash B, Sullivan S, Barghout V. Total costs of IBS: employer and managed care perspective. Am J Manag Care 2005;11(1 Suppl):S7–16. [PubMed] [Google Scholar]
- 33. George R. Bad blood: the taboo on talking about periods is damaging lives. The Guardian 2016. [Google Scholar]
- 34. Aufrichtig A. Period pain: why do so many women suffer from menstrual cramps in silence? The Guardian 2016. [Google Scholar]
- 35. Betts H. The P Word: A last taboo. The Telegraph 2013. [Google Scholar]
- 36. Central Bureau of Statistics C. Statline - Active workforce; duration of labour. (Werkzame beroepsbevolking; arbeidsduur) 2018. [Google Scholar]
- 37. Central Bureau of Statistics C. Statline - Sick leave according to employees; gender and age. (Ziekteverzuim volgens werknemers; geslacht en leeftijd) 2017. [Google Scholar]
- 38. Robinson LL, Ismail KM. Clinical epidemiology of premenstrual disorder: informing optimized patient outcomes. Int J Womens Health 2015;7:811–8. 10.2147/IJWH.S48426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Giudice LC, Kao LC. Endometriosis. The Lancet 2004;364:1789–99. 10.1016/S0140-6736(04)17403-5 [DOI] [PubMed] [Google Scholar]
- 40. Central Bureau of Statistics C. Statline - People attending the general practitioner; diagnosis, age, gender. (Personen naar bij de huisarts bekende diagnose; leeftijd, geslacht) 2016. [Google Scholar]
- 41. Central Bureau of Statistics C. Statline - Social monitor, properity and weel-being in the Dutch society. (Sociale Monitor, welvaart en welzijn in de Nederlandse samenleving) 2018. [Google Scholar]
- 42. Whitaker C, Stevelink S, Fear N. The Use of Facebook in Recruiting Participants for Health Research Purposes: A Systematic Review. J Med Internet Res 2017;19:e290 10.2196/jmir.7071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Severens JL, Mulder J, Laheij RJ, et al. . Precision and accuracy in measuring absence from work as a basis for calculating productivity costs in The Netherlands. Soc Sci Med 2000;51:243–9. 10.1016/S0277-9536(99)00452-9 [DOI] [PubMed] [Google Scholar]
- 44. Bouwmans C, De Jong K, Timman R, et al. . Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv Res 2013;13:217 10.1186/1472-6963-13-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Janda C, Kues JN, Andersson G, et al. . A symptom diary to assess severe premenstrual syndrome and premenstrual dysphoric disorder. Women Health 2017;57:837–54. 10.1080/03630242.2016.1206055 [DOI] [PubMed] [Google Scholar]
- 46. O’Brien PM, Bäckström T, Brown C, et al. . Towards a consensus on diagnostic criteria, measurement and trial design of the premenstrual disorders: the ISPMD Montreal consensus. Arch Womens Ment Health 2011;14:13–21. 10.1007/s00737-010-0201-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lee AM, So-Kum Tang C, Chong C. A culturally sensitive study of premenstrual and menstrual symptoms among Chinese women. J Psychosom Obstet Gynaecol 2009;30:105–14. 10.1080/01674820902789241 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-026186supp001.pdf (332.2KB, pdf)