Abstract
This systematic review and meta-analysis examined the literature on early care and education center (ECEC)-based physical activity interventions to identify ecologic environmental factors that improve cardiovascular fitness (CVF) in preschool-aged children. Data sources included PubMed, Web of Science, Cochrane Library Trials, CINHAL, Science Direct, PsychINFO and SPORTDiscus. Peer-reviewed publications of studies that met the following criteria were eligible for inclusion: (1) mean age of participants between two and a half and five and a half years old enrolled in a pre-primary school; (2) randomized controlled trials or quasi-experimental interventions with a control group; (3) interventions occurring before, during, or immediately after school; (4) use of an objective measure or field-based estimate of CVF; (5) enrolled apparently healthy children. In June of 2018, titles (n = 1197) were reviewed for inclusion into the study and 74 abstracts/full texts were assessed for eligibility. Ten articles met all eligibility criteria and were included in the final review. A random effects meta-analysis suggested a moderate-to-large effect size for ECEC-based interventions to increase CVF (g = 0.75; 95%CI [0.40–1.11]). Interventions that included three or more ecologic environments (g = 0.79 [0.34–1.25]) were more effective than interventions occurring at the individual level (g = 0.67 [0.12–1.22]). Study quality was moderate, and (mean ± SD) 17.9 ± 4.3 (63.9%) of 28 checklist items were reported. Preliminary evidence suggests that ECEC-based interventions to increase CVF are highly effective at improving preschool children's exercise test scores. Although ECEC-based interventions show promise, the small number of studies included in this review limits confidence in these findings. Review registered at PROSPERO CRD42018099115.
Keywords: Child, Preschool, Cardiorespiratory fitness, Systematic review, Physical activity, Social ecology
Highlights
-
•
ECEC-based interventions have a moderate-to-large effect on cardiovascular fitness.
-
•
A majority (5/8) of ECEC-based PA interventions targeted multiple environments.
-
•
Reporting on PA dosage and intervention implementation are lacking.
1. Introduction
Cardiovascular fitness (CVF) is defined as the ability to perform large-muscle, whole-body exercise at moderate to high intensities for extended periods of time (2018 Physical Activity Guidelines Advisory Committee, 2018) and is related to multiple health outcomes in both adults (Myers et al., 2015a) and children (Ortega et al., 2015; Ortega et al., 2008). CVF begins to develop at a young age and tracks into adulthood to predict future CVF, physical activity (PA) and healthy weight profiles (Malina, 2001). Although CVF early in life is primarily determined by biological factors (Malina, 2014), physical activity and developmental (e.g., motor competence) factors also contribute to differences in CVF in young children (Robinson et al., 2015; Stodden et al., 2008) and thus offer a means for improvement.
According to The Institute of Medicine (IOM), Early Care and Education Centers (ECECs) are primary targets for behavioral interventions because of the large number of young children they enroll (McGuire, 2012). Children spend an average of 24.8 h per week at ECECs (SHAPE America, 2015; Iruka and Carver, 2006), which makes ECEC-based intervention an important place to leverage to influence CVF. Children at ECECs spend approximately 80% of their day in sedentary activities and only 2–3% in moderate to vigorous PA (Pate et al., 2008; Reilly, 2010), and low levels of PA have been shown to be related to underdeveloped CVF in early childhood (Bürgi et al., 2011; Leppänen et al., 2016). Despite the association between PA and CVF, interventions focused on improving PA rarely examine concurrent change in CVF outcomes in young children (Ward et al., 2010), and several studies describe the correlation between PA and CVF as low (Bürgi et al., 2011; Carson et al., 2017), suggesting that tangential factors related to PA may also influence improvements in CVF.
CVF is also hypothesized to be related to higher levels of motor competence (MC) in young children through both physiological (i.e., improved neuromuscular function) and behavioral (i.e., motivation and activity participation choices) processes (Robinson et al., 2015). Although the mechanisms themselves have yet to be tested, several systematic reviews already support the association between CVF and MC in children (Figueroa and An, 2017; Logan et al., 2015) and adolescents (Cattuzzo et al., 2016). Additionally, multiple environmental factors (Cools et al., 2011) have been shown to be related to MC in preschool age children, including factors found in the home and ECECs (O'Neill et al., 2014). The relationship between these findings suggest that a child's environment may contribute to the increases in CVF though both increases in PA and improvements in MC.
To date, only one review has examined the literature related to the improvements in CVF in young children (3 to 12-years-old) and was limited in scope by selecting only PA-related randomized controlled trials (Pozuelo-Carrascosa et al., 2018). Moreover, several sizable CVF intervention studies in preschoolers were excluded. The current review adds to the literature by focusing specifically on studies that included very young children (2.5 to 5.5-years-old), examining additional study designs, and focusing on intervention components that are hypothesized to affect CVF outcomes.
Multi-level, comprehensive school-based PA programs that include the child's home and community are recommended for PA promotion within school systems (Centers for Disease Control and Prevention, 2013). Ecological models, like the Ecological Model of Physical Activity (EMPA), often serve as a framework for examining pathways across multiple environments (microsystems) of influence that create interactions (exosystems, mesosystems, and macrosystems connections) to affect PA (Spence and Lee, 2003), and can also provide guidance for exploring indirect pathways related to CVF. In addition, several ECEC-based studies have used ecological frameworks when intervening to influence CVF (Tan et al., 2017; Puder et al., 2011; Eliakim et al., 2007), which suggests that they would aid as a roadmap for assessing indirect factors that may also contribute to its improvement. Therefore, the purposes of this study were to 1) systematically review the literature on ECEC-based interventions designed to increase CVF and 2) determine ecologic environmental factors related to increases in CVF in preschool-aged children.
2. Methods
2.1. Protocol and registration
This systematic review and meta-analysis was registered with the International Prospective Register of Systematic Reviews (PROSPERO; Registration no. CRD42018099115; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=99115). It was conducted and reported following the Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2009).
2.2. Data sources and search strategy
Literature searches were conducted in June of 2018 using seven electronic databases, including PubMed, Web of Science, Cochrane Library Trials, CINHAL, Science Direct, PsychINFO and SPORTDiscus. Advance-searching options were used, and identical search strings were entered into each database. All possible search terms were entered into each search string, using the Boolean operators “AND” and “OR” to connect terms. The search string used to identify articles was (preschool OR day care OR pre-k OR early care and education) AND (school-based intervention OR before school intervention OR after school intervention) AND (fitness OR physical fitness OR cardiorespiratory fitness OR cardiovascular fitness OR aerobic fitness OR aerobic capacity OR aerobic power OR physical work capacity OR maximal oxygen consumption). No search limits were set for study year or country where the study took place. Only articles in English were reviewed. One author (JS) completed initial searches, compiled a list of all article titles and removed the duplicates. Two authors (JS, EL) reviewed the title list independently, with duplicates removed, for inclusion into the study. Results were compared, and discrepancies were discussed until a consensus was reached. In the event that the two reviewers could not reach consensus, a third reviewer (REL) was asked to resolve the conflict. Once titles that definitively did not match the PICO (Population: preschool-aged children, Intervention: ECEC-based, Comparison: control group included, Outcome: CVF) were removed, reviewers repeated the review process a second time reviewing abstracts and full texts based on all eligibility criteria to determine the final studies to be included in this review. When searches identified multiple articles that described different aspects of the same study (e.g., follow up, different outcome measures, subgroup analysis), data from all articles were included into the review if articles contributed additional information related to CVF. This systematic review's precise search strategy was supplemented by identifying articles through reference lists and additional searches that took place as part of dissertation literature review to improve sensitivity.
2.3. Eligibility criteria
For inclusion in this review, studies had to be published in peer-reviewed journals, written in English, and meet the following inclusion criteria: (1) study reported mean age of participants between two and a half and five and a half years old enrolled in a pre-primary school, (2) interventions were either randomized controlled trials or quasi-experimental interventions with a control group; (3) interventions must have occurred immediately before, during, or immediately after school; (4) CVF must have been assessed either directly or through a field-based estimate (e.g., timed runs or distance runs); (5) participating children must have been apparently healthy with no known cognitive or motor skills deficit at recruitment.
2.4. Data extraction
Research articles were critically reviewed several times. Main study characteristics were extracted and recorded in an excel spreadsheet for summarization, interpretation, rating, and comparison of study results. Study information related to effectiveness or possible intervention components was extracted from the article and included the following: (1) intervention length; (2) intervention setting (before, during, or after school); (3) age and number of participants included in the study; (4) country in which the study took place; (5) intervention characteristics; (6) methods of CVF measurement; (7) description of study findings; (7) inclusion of follow-up data (if applicable); (8) study design; and (9) characteristics needed for a rating of study quality.
2.5. Study quality assessment
Study quality was rated using a Quality Index Score (QIS), a well-established and previously validated scale developed for use in both randomized and non-randomized controlled trials (Downs and Black, 1998). QIS scores range from 0 to 28 (higher scores equal stronger quality) and when previously validated had high levels of internal consistency, test re-test reliability (r = 0.88), inter-rater reliability (r = 0.75), and criterion validity (r = 0.90). The QIS reports on several aspect of bias including quality of reporting, external validity, measurement/intervention bias, subject selection bias, and whether the study was appropriately powered. Two independent observers (JS, EL) completed the QIS and discrepancies were discussed until a consensus was reached. In the event consensus could not be reached a third reviewer (REL) helped to resolve the conflict.
2.6. Data synthesis
A narrative synthesis was created for all studies. Results were synthesized by study design, region where the study took place, study quality, method of measurement for CVF, and intervention components included from each ecological level (individual, interpersonal, institutional, community, and policy) (McLeroy et al., 1988). Additionally, the number of studies within each synthesized category were tabulated and examined in an attempt to identify patterns within each tabulated group. Last, overall completeness, quality of the evidence, and potential biases in the review process were documented and discussed.
2.7. Meta-analysis
Pre-post intervention means and their standard deviations/standard errors were extracted from each study and transformed into mean differences and pooled standard deviations based on the units they were reported in (e.g., laps, stages, seconds). When multiple measures of CVF were present within one article the outcome measure that was most closely related to the definition of CVF (2018 Physical Activity Guidelines Advisory Committee, 2018) was selected. Studies that analyzed data subsamples separately (normal weight vs. obese), or made multiple measures within one test (heart rate at multiple workloads), were combined to create one effect size and weighted according to the number of participants in each group. When additional information was needed to determine effect size, authors were contacted up to three times in attempt to retrieve the data. If an author could not be reached, effect sizes were estimated from graphs as opposed to table values. Each study only contributed one effect size to the meta-analysis, despite the number of articles included in the review.
Hedge's g, a measure of effect size that corrects for the impact of small sample sizes and standard errors, was calculated for each sample that provided data (Borenstein et al., 2009). In the event two articles reported the same sample, the primary outcome paper was used to compute effect size. In addition, because interventions occurred in the ECEC setting, a design effect was applied that took into account the average number of subjects per classroom. An estimated clustering effect was used to correct the Hedge's g standard error for studies that did not originally control for clustering in their analyses. Puder et al. found an intraclass correlation (ICC) of 0.07 for measures of CVF in 40 preschool classrooms, while Kriemler et al. and Meyer et al. found ICCs between 0.02 and 0.04 in elementary children (Puder et al., 2011; Kriemler et al., 2010; Meyer et al., 2014). An ICC of 0.07 was used when adjusting for clustering, as it provided the most conservative estimate.
Meta-analyses were conducted, and a forest plot was created in the Cochrane database review manager (Revman5) using adjusted effect sizes and their 95% confidence intervals (Review Manager (RevMan) [Computer Program]. Version 5.3, 2014). A summary effect was provided based on a random effects meta-analysis. Heterogeneity was estimated using Cohran's Q and a random effects meta-analysis was used, as it incorporates both within study and between study variance and provides a better estimate in cases where studies have high heterogeneity or low sample sizes. Sub-analyses were conducted to compute effect sizes for each of the following groups in an attempt to examine explain heterogeneity: study design (randomized controlled trials vs. quasi-experimental), length of intervention (one academic year vs. less than one academic year), world region where the study took place (North America vs. Middle East vs. China vs. Asia), method of CVF measurement (heart rate vs. shuttle runs vs. distance runs), and number of ecological levels included in the intervention (3+ vs. <3). Last, a funnel plot was created using the Cochrane database review manager and visually inspected to examine potential publication bias based on methodological quality. Statistical tests were underpowered to detect publication bias, thus, were not used (Egger et al., 1997; Begg and Mazumdar, 1994). A p-value of <0.05 was considered significant for the primary meta-analysis and all sub analyses.
3. Results
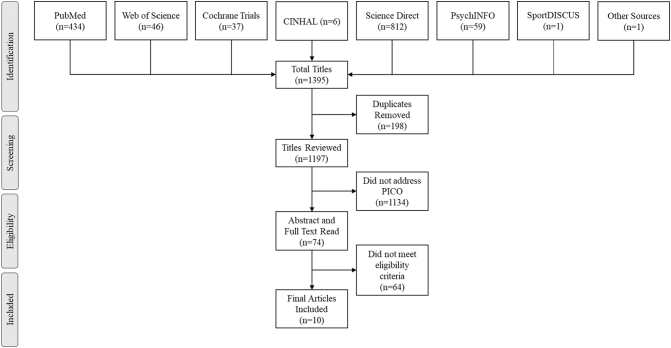
The search process returned 1197 individual titles that were reviewed for inclusion in the study. Seventy-four abstracts and full texts were read based on their title matching the PICO, and ten articles met all eligibility criteria and were considered acceptable for final review (Fig. 1). Of the ten articles, eight contributed individual effect size data (Tan et al., 2017; Puder et al., 2011; Eliakim et al., 2007; Zhou et al., 2014; Latorre-Román et al., 2018; Nemet et al., 2011a; Nemet et al., 2011b; Alpert et al., 1990). One article was a follow-up study (Nemet et al., 2013), and another was a secondary data analysis (Niederer et al., 2013). Of the eight studies that contributed individual data, three were almost identical interventions by the same research team, but the intervention was tested in three separate populations (Eliakim et al., 2007; Nemet et al., 2011a; Nemet et al., 2011b).
Fig. 1.
Study selection process. Review conducted in June 2018.
Data extracted from the articles can be found in Table 1. Sample sizes ranged from 24 to 795 children. All of the studies occurred during the school day, and interventions lasted between eight weeks and one full academic year. Seven of the eight studies had an experimental study design (Tan et al., 2017; Puder et al., 2011; Eliakim et al., 2007; Latorre-Román et al., 2018; Nemet et al., 2011a; Nemet et al., 2011b; Alpert et al., 1990), whereas one (Zhou et al., 2014) used a quasi-experimental study design. Three studies took place in the Middle East (Eliakim et al., 2007; Nemet et al., 2011a; Nemet et al., 2011b); two occurred in Asia (Tan et al., 2017; Zhou et al., 2014); two were conducted in Europe (Puder et al., 2011; Latorre-Román et al., 2018); and one occurred in North America (Alpert et al., 1990). Four studies used shuttle runs as their primary method of measurement for CVF (Tan et al., 2017; Puder et al., 2011; Nemet et al., 2011a; Nemet et al., 2011b); three used a timed run (Eliakim et al., 2007; Zhou et al., 2014; Latorre-Román et al., 2018); and one (Alpert et al., 1990) used heart rate response at multiple progressive workloads. In addition, one study used heart rate measurements before and after a specified workload as a secondary measure of CVF (Tan et al., 2017). The use of each level of the ecological model as an intervention components for each study can be found in Table 2.
Table 1.
ECEC-based intervention studies that examine cardiovascular fitness outcomes in preschool children.
| Author, year | Intervention setting; length | Population | Country | PA intervention components | Fitness measurement | Findings | Follow-up findings |
|---|---|---|---|---|---|---|---|
| Alpert et al. 1990 (Alpert et al., 1990) | During school; 8 weeks | n = 24 children 3- to 5-years-old (mean age 44 months) | USA | 30 min daily designed to increase HR to 60–80% HR max. Children exercised with music and imagery. HR was monitored every 10-min. Stickers were given for achieving HR goals. | Cycle ergometer test at three workloads (12.5, 25, and 37.5 watts). Change in exercise HR. | HRs were significantly lower at post-test compared to pretest for all workloads in the X group compared to the O group. Workload 1: O (+9 bpm) vs. X (−17 bpm). Workload 2: O (+7 bpm) vs. X (−16 bpm). Workload 3: O (+5 bpm) vs. X (−20 bpm). | N/A |
| Eliakim et al., 2007 | During school; 14 weeks |
n = 101 upper-middle SES 5–6-year-old |
Israel | 2 parent orientation sessions. Teachers implemented sessions 4× per week and youth coaches implemented sessions 2× per week for 45 min/session (80% running games; 20% sports activities). | 600-m run | O group significantly increased endurance run time by 6 s, while X group decreased by 14 s. Overweight and obese O increased by 7 s, while X decreased by 7 s. | N/A |
| Nemet et al., 2011a; Nemet et al., 2013 | During school; one school year | n = 342 low SES 4.2–6.5-year-old | Israel | 2 parent orientation sessions. Teachers implemented sessions 5× per week and youth coaches implemented sessions 1× per week for 45 min/session (80% running games; 20% sports activities). | 10-m shuttle run test | O group decreased total number of laps by 10.2 ± 1.6 (males −7; females −14), while X group increased by 11.6 ± 1.4 laps (males +11; females +13); overweight and obese O decreased by 12 and 2 laps respectively, while overweight and obese X participants increased by 7 and 18 laps respectively.a | Nemet et al. (2014) n = 203 (59%); Both O and X had more laps 1 year later. The X remained significantly higher than the O. |
| Nemet et al., 2011b | During school; one school year | n = 795 low SES 3.8–6.8-year-old | Israel | 2 parent orientation sessions. Teachers implemented sessions 5× per week and youth coaches implemented sessions 1× per week for 45 min/session (80% running games; 20% sports activities) | 10-m shuttle run test | O group decreased total number of laps by 3 (males 0; females −5), while X group increased by 18 laps (males +20; females +17); overweight and obese O decreased by 2 and 3 laps respectively, while overweight and obese X participants increased by 17 and 18 laps respectively.a | N/A |
| Niederer et al., 2013b | Normal weight X group improved shuttle run (+1.8 stages) compared to O (+1.5 stages). Overweight X children did not significantly improve shuttle run (+1.7 stages) compared to O (+1.3 stages). Low fit X group did not improve shuttle run (+1.8 stages) compared to O (+1.6 stages). Normal fit X group improved shuttle run (+1.7 stages) compared to O (+1.4 stages). Neither weight nor fitness level were not found to modify intervention effects for the shuttle run. |
N/A | |||||
| Puder et al., 2011 | During school; 1 academic year | n = 652 migrant 5.2 ± 0.6-years-old preschool children | Switzerland | Four 45-min PA sessions/wk. Implementers gave 1 PA session/wk. Reduced to 2×/month after 4 months. Other sessions ran by teachers after two workshops. Every 2nd wk. children took home a PA card. Parents joined 3 discussions. Play equipment installed/provided to classrooms. | 20-m shuttle run test | X group significantly increased shuttle run (1.7 stages) compared to O group shuttle run (1.4 stages). | N/A |
| Latorre-Román et al., 2018 | During school; 10 weeks | n = 111 children aged 4.28 ± 0.61-years-old | Spain | Three 30 min training sessions/wk. Sessions included aerobic games that increased from a total of 15–18 min in duration over the 10 weeks. | 10 × 20 m shuttle run | Time decreased by 8.5 s in the X group and decreased by 3.6 s in the O group. Group by time interactions were not statistically significant. | N/A |
| Tan et al., 2017 | During school; 10 weeks | n = 104 children 5-year-old | China | 5 one hour supervised sessions/wk. 10 min warm-up and cool down. 40 min of moderate PA (walking, running, jumping, rope skipping, semisquatting, crawling) in 4 min intervals followed by 1 min rest. Exercise occurred at 50% of HR max (monitored by HR monitor). | 20-m shuttle run test; HR Index-HR response to a workload (30 squats in 30 s). Formula: resting HR + end exercise HR + recovery HR at 1 min–200) ÷ 10 |
Obese X group increased their 20-m shuttle 1.05 laps compared to a 0.33 lap increase in obese O. Lean X group increased by 1.06 laps compared to a 0.32 increased in lean O. Results not significant. Obese X group decreased HR index by −0.96, while obese O HR index decreased −0.24. Lean X group decreased HR index −1.17, while lean O decreased by −0.12. Results were significant (p < 0.001) for both groups. |
N/A |
| Zhou et al., 2014 | 12 months | n = 357 children ages 3–5-years-old | China | New outdoor play policy (60–90 min with 10-min exercise session). Teacher received bi-weekly training (20 h total). Outdoor play curriculum developed and monitored daily. New outdoor play equipment. Monthly education webinars and newsletters for families. Internet resource website. Family events and new play equipment for families. Renovation of neighborhood playgrounds, including new equipment. Neighborhood events. | 20-m agility run | Children at the intervention center significantly decreased their 20 m agility run time (−1.22 s) compared to control (−0.59 s). | N/A |
Review conducted in June 2018.
Bpm-beats per minute; HR-heart rate; O-control; PA-physical activity; SES-socioeconomic status; X- experimental.
Lap changes are estimated from a graph where a standard deviation is not reported. Exact values are not reported in the manuscript.
Same Study as Puder et al. 2011. Analysis of intervention effects by weight (overweight vs. normal weight) and fitness (low fitness vs. normal fitness).
Table 2.
Intervention components at each level of the ecological model.
| Study | Individual | Interpersonal | Institutional | Community | Policy | Total number of levels |
|---|---|---|---|---|---|---|
| Alpert et al., 1990 | 1 | 0 | 0 | 0 | 0 | 1 |
| Eliakim et al., 2007 | 1 | 1 | 1 | 0 | 0 | 3 |
| Latorre-Román et al., 2018 | 1 | 0 | 0 | 0 | 0 | 1 |
| Nemet et al., 2011a | 1 | 1 | 1 | 0 | 0 | 3 |
| Nemet et al., 2011b | 1 | 1 | 1 | 0 | 0 | 3 |
| Puder et al., 2011 | 1 | 1 | 1 | 0 | 0 | 3 |
| Tan et al., 2017 | 1 | 0 | 0 | 0 | 0 | 1 |
| Zhou et al., 2014 | 1 | 1 | 1 | 1 | 1 | 5 |
Review conducted in June 2018.
1 = Level of the model included in the intervention; 0 = level of the model not included in the intervention.
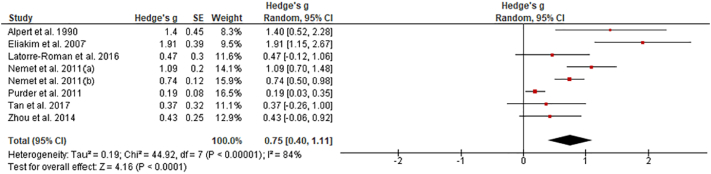
Results from the random effects meta-analysis suggested a moderate-to-large effect size for the ECEC-based interventions on CVF (Fig. 2). Due to high heterogeneity between study effects (Cohran's Q = 44.92; p < 0.001), subgroup analyses were conducted to explore differences. Randomized controlled trials had a larger effect size (g = 0.81 95%CI [0.41–1.21]; n = 7) (Tan et al., 2017; Puder et al., 2011; Eliakim et al., 2007; Latorre-Román et al., 2018; Nemet et al., 2011a; Nemet et al., 2011b; Alpert et al., 1990), than quasi-experimental study designs (g = 0.43 [−0.06–0.92]; n = 1; p = 0.24) (Zhou et al., 2014). Study interventions that occurred for one full academic year (g = 0.60 [0.18–1.02]; n = 4) (Tan et al., 2017; Eliakim et al., 2007; Latorre-Román et al., 2018; Alpert et al., 1990) were less effective than those occurring for only a partial year (g = 1.00 [0.27–1.72]; n = 4; p = 0.35). (Puder et al., 2011; Zhou et al., 2014; Nemet et al., 2011a; Nemet et al., 2011b) The study that occurred in North America (g = 1.40 [0.52–2.28]; n = 1) (Alpert et al., 1990) had the largest effect size, followed by those that occurred in the Middle East (g = 1.13 [0.61–1.66]; n = 3) (Eliakim et al., 2007; Nemet et al., 2011a; Nemet et al., 2011b), Asia (g = 0.41 [0.02–0.79]; n = 2) (Tan et al., 2017; Zhou et al., 2014), and Europe (g = 0.21 [0.06–0.36]; n = 2; p < 0.01)[27, 39]. When examining methods of measurement, the study that used heart rate response to a set workload (g = 1.40 [0.52–2.28]; n = 1) (Alpert et al., 1990) showed the strongest intervention effect, followed by those that measured CVF using timed runs (g = 0.89 [0.06–1.73]; n = 3) (Eliakim et al., 2007; Zhou et al., 2014; Latorre-Román et al., 2018) and shuttle run tests (g = 0.60[0.16–1.03]; n = 4; p = 0.26) (Tan et al., 2017; Puder et al., 2011; Nemet et al., 2011a; Nemet et al., 2011b). Last, studies which included three or more components of the ecological model in their intervention (g = 0.79 [0.34–1.25]; n = 5) (Puder et al., 2011; Eliakim et al., 2007; Zhou et al., 2014; Nemet et al., 2011a; Nemet et al., 2011b) were more effective than studies that intervened only at the individual level (g = 0.67 [0.12–1.22]; n = 3; p = 0.73) (Tan et al., 2017; Latorre-Román et al., 2018; Alpert et al., 1990). None of the sub-analyses completely explained the heterogeneity in the results (ps > 0.05).
Fig. 2.
Forrest plot of the effect sizes for ECEC-based interventions on cardiovascular fitness outcomes (random effects meta-analysis). Review conducted in June 2018.
3.1. Assessment of study quality
Quality assessments of each study can be found in Table 3. Overall, the study quality was moderate, with an average of 17.9 ± 4.3 (63.9%) of twenty-eight items on the checklist being met. Studies demonstrated the lowest quality rating on power analysis and external validity criteria. Only one of eight studies reported a power analysis, and, on average, just over one (1.3, 43.3%) of three of the external validity items were reported. Other areas of bias had substantially better scores. On the reporting subscale, the average study reported 7.6 (69.1%) of 11 items: 5.0 (71.4%) of the 7 internal validity and 3.9 (65.0%) of the 6 selection bias items. The one quasi-experimental study included had comparable levels of bias with other studies, and, thus, should not have impacted the results of this review.
Table 3.
Quality rating index scores.
| Study | Study type | Total QRI scorea (28 possible) |
Reporting score (11 possible) |
External validity (3 possible) |
Internal validity (7 possible) |
Selection bias (6 possible) |
Power analysisb (1 possible) |
|---|---|---|---|---|---|---|---|
| Alpert et al., 1990 | E | 19 | 6 | 3 | 6 | 4 | 0 |
| Eliakim et al., 2007 | E | 17 | 8 | 1 | 3 | 5 | 0 |
| Latorre-Román et al., 2018 | E | 18 | 8 | 1 | 5 | 4 | 0 |
| Nemet et al., 2011a | E | 13 | 5 | 1 | 4 | 3 | 0 |
| Nemet et al., 2011b | E | 13 | 5 | 1 | 4 | 3 | 0 |
| Puder et al., 2011 | E | 26 | 11 | 1 | 7 | 6 | 1 |
| Tan et al., 2017 | E | 21 | 10 | 1 | 5 | 5 | 0 |
| Zhou et al., 2014 | QE | 16 | 8 | 1 | 6 | 1 | 0 |
| Mean (SD) | 17.9 ± 4.3 | 7.6 ± 2.2 | 1.3 ± 0.7 | 5.0 ± 1.3 | 3.9 ± 1.6 | 0.1 ± 0.4 |
Review conducted in June 2018.
QE = Quasi-experimental; E = Experimental; SD = Standard Deviation.
Total QRI score is a composite of the 5 subscales.
Power Analysis was reported in the manuscript (1 = yes; 0 = no).
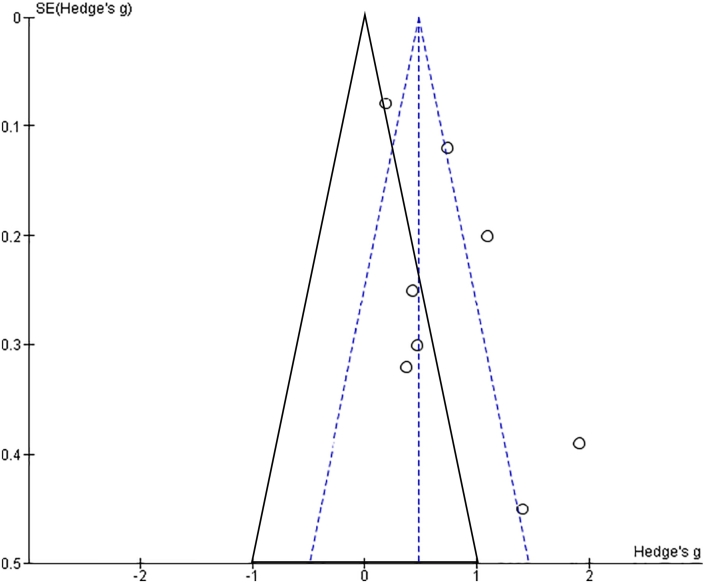
Results from the funnel plot are depicted in Fig. 3. Interventions with large sample sizes (low standard errors) were dispersed evenly around the average effect size with several studies indicating small to no effect. Smaller studies (high standard errors) were skewed to the right, above the 95% confidence interval on the distribution, suggesting that there may be some evidence of publication bias related to these studies. Due to the small number of studies, statistical tests were not used.
Fig. 3.
Funnel plot of intervention effect sizes (x-axis) and their corresponding standard errors (y-axis). Solid triangle represents predicted distribution and 95% confidence interval of effect sizes based on a null hypothesis. Dashed triangle represents the actual distribution and related 95% confidence intervals. Review conducted in June 2018.
4. Discussion
Overall, this study found that interventions focused on improving the CVF profiles of young children impart a moderate-to-large effect on CVF. Interpersonal and institutional factors included in these studies focused on training and incorporation of teachers into intervention delivery, whereas parents were included through newsletters, discussions, orientation sessions, webinars, and family homework. In addition, PA equipment (e.g., posters, climbing walls, PA games, portable toys) was installed into classrooms and play areas of ECECs. The one intervention that included both community and policy level intervention components focused on center-level play policies, improved curricula and curricular monitoring, improvement of neighborhood play equipment, and neighborhood events for families (Zhou et al., 2014). Strategies implemented by these studies are consistent with the literature on improving PA and supported by the EMPA, which posits that interventions that occur within multiple environments have linkages that allow transfer effects (Spence and Lee, 2003).
Hypothesized transfer linkages are a potential explanation for the slightly larger effect size of interventions that included three or more environmental levels found in this systematic review. In addition, the finding that multi-component interventions are more effective for improving CVF aligns with the current recommendations for including multiple environments in school-based interventions to improve PA, although effect sizes for school-based interventions on PA are smaller than those found for CVF in this meta-analysis (Van Sluijs et al., 2007; Beets et al., 2009; Wechsler et al., 2000). Two previous reviews that examined the relationship between school-based PA interventions and CVF in children, including older children, discovered that PA interventions only created small effects on CVF profiles (Pozuelo-Carrascosa et al., 2018; Beets et al., 2009). Smaller effect sizes could potentially be due to a dilution effect related to grouping all children, aged 3–12 years-old, into one analysis, as environments and developmental patterns in younger children differ from older children (Malina, 2001; Ortega et al., 2007). In addition, the potential publication bias suggested by the funnel plot in this review could be responsible for the larger effect sizes found in this group of studies.
Several of the sub-analyses from this meta-analysis revealed interesting results. First, sub-analyses showed that full academic year interventions had smaller effect sizes than interventions that occurred for a partial year. Although this finding appears counterintuitive, intervention frequency (3×-6× per week), duration, and type (structured vs. unstructured) varied substantially across studies and may be responsible for these results. Previous research has shown that higher intensity, longer duration per session, and higher frequency of sessions per week have all been related to improved CVF levels (Wenger and Bell, 1986). Many of the studies in the current review address frequency per week and duration per session, but differences in exercise intensity and type (aerobics, sport, free play, structure) preclude from defining a program prescription to compare across studies. In addition, it is unclear if the changes made within each intervention expanded upon time for PA (i.e., replaced sedentary activities with PA), extended the amount of time available for PA, or enhanced the quality of current opportunities to be physically active, which may be related to the effectiveness of each intervention (Beets et al., 2016). Future studies that address CVF should include and report measures of frequency, intensity, duration, and modes of PA to facilitate comparisons across studies and describe the patterns of PA present before the intervention occurred.
Second, sub-analyses revealed that effects varied substantially based on the measure used to discern CVF (g = 0.44–1.40), and that the strongest intervention effects were found with the use of heart rate monitoring (Alpert et al., 1990). Although heart rate is important to measure in relationship to CVF, submaximal exercise heart rate has been found to be variable in preschool-aged children (Nguyen et al., 2011). In addition, issues related to pacing or motivation may prevent children from reaching maximal exercise intensity. There is no gold-standard, field-based measure for CVF, and previous reviews suggest that a shuttle run test with a pacesetter may be the best option (Ortega et al., 2015; Ruiz et al., 2011). However, this test may be influenced by factors other than the cardiovascular system (weight, motivation, motor competence, perceived motor competence, listening skills). Future studies that validate field-based measures of CVF in preschool-aged children and/or develop new measures are needed to advance the field.
Overall, subgroup analyses from this study should be viewed as exploratory (i.e., hypothesis generating) as they were generated in an attempt to explain heterogeneity, not created a priori. Due to the small number of studies, some of the subgroup analyses contained only one study per subgroup. Thus, effect sizes for that subgroup represent the effect from a single study and not a body of literature. Subgroup analysis results by nature are observational and should be viewed with caution.
4.1. Strengths
A strength of this meta-analysis lies in the choice of a narrowly defined age range. By selecting only studies with young children, environmental intervention components specific to this age group can be analyzed. Pre-primary children often face a unique set of environmental circumstances compared to elementary-aged children including shorter school weeks, higher levels of teacher engagement in activity lessons, and higher initial levels of PA (Chow et al., 2015; Ishii et al., 2015). In addition, preschool teachers often have more flexibility in how to implement PA interventions within the classroom (Howie et al., 2016). By examining only preschool-aged children, findings from this study have increased applicability to young children's early care and education and, thus, are more likely to be successfully implemented, resulting in higher levels of CVF. Furthermore, CVF has been found to have higher inter-age correlations than PA in childhood, suggesting that children who improve their CVF early on in life may sustain improved CVF into later childhood (Malina, 2001). Future research should determine whether CVF intervention effects in childhood can be maintained as children age.
A second strength of this meta-analysis was the high methodological quality (mean QRI score = 17.9) of this group of studies compared to other studies that have examined health-related interventions (Downs and Black, 1998; Prince et al., 2008; Warburton et al., 2010). Initial testing during the design process found an average QRI score of 14 for a randomized controlled health care intervention, while an average score for a quasi-experimental study was 11 (Downs and Black, 1998). Subsequent use of the QRI in two PA interventions revealed that 11 and 12 of (~75–80%) the items were reported, although several scales were modified to remove less relevant items (Prince et al., 2008; Warburton et al., 2010). In this group of studies, all but two (Nemet et al., 2011a; Nemet et al., 2011b) of the randomized controlled trials and quasi-experimental studies scored at least 14 or higher on the QRI checklist, which suggest a high level of scientific rigor for the studies included in this review.
4.2. Limitations
Despite the strong methodological quality overall, only one study reported a power analysis and controlled for clustering related to having multiple classrooms in their analysis (Puder et al., 2011). Three studies (Tan et al., 2017; Zhou et al., 2014; Latorre-Román et al., 2018) determined that there was a significant intervention effect, which was later erased when an estimated design effect was applied. On average, fewer than half of the items were reported in relationship to external validity, which limits the generalizability of these findings to larger and more diverse populations. Despite the limitations related to power and external validity, scores for reporting, internal validity, and selection bias were high suggesting that this body of research applied rigorous study designs with high internal consistency. Although potential publication bias may have increased the overall quality of studies included in this review, the finding from these studies are likely real effects and not due to poor methodology or flawed research practices within individual studies.
When interpreting the evidence presented in this review several factors should be considered. First, this meta-analysis found a high level of heterogeneity in the studies, suggesting that studies were more different from one another than similar. Based on the small number of studies and the variety of characteristics of the studies included in this meta-analysis, an increased amount of heterogeneity is to be expected. Characteristics that may have contributed to the heterogeneity are inclusion of both experimental and quasi-experimental study designs, use of multiple measures of CVF, interventions with varying numbers of intervention components, multiple countries with differences in early childhood education systems, and lack of reporting on external validity. Further, this analysis was unable to compare sociodemographic differences between study populations. Although some explanations for heterogeneity were explored through stratified analysis, interaction among several factors could have still occurred which allowed increased levels of heterogeneity to remain. Furthermore, multi-component interventions were delivered as a package, and reporting on implementation of specific intervention components was scarce. Due to limited data on which components of the intervention were delivered, no attempt was made to determine which intervention components were most effective for increasing CVF. Lack of reporting on implementation fidelity has been shown to be a problem in comprehensive school-based PA interventions and more studies aimed at increasing CVF are needed to determine the extent to which implementation plays a role in the improvement of CVF in early childhood (Naylor et al., 2015).
A second element that should be considered when interpreting the results of this meta-analysis is the choice of measure used to determine CVF. The majority (7/8 studies) of studies in this review used field-based measures of CVF, including shuttle and distance runs, while only one study examined the effects of CVF interventions on a physiological outcome. CVF is the ability to perform large-muscle, whole-body exercise at moderate to high intensities for extended periods of time and is best measured by physiological responses to exercise in lab-based conditions (2018 Physical Activity Guidelines Advisory Committee, 2018; Armstrong et al., 2011). Only one study in this meta-analysis measured heart rate, a physiological component related to CVF, while other studies use performance on field-based tests, which estimate CVF through prediction equations. Field-based tests and related prediction equations can be a useful tool in the community-based or school setting. However, the field-based tests for CVF used in this review have not been validated for use in young children (< 6 years old), and, thus, may be related to constructs (PA, MC, motivation) other than CVF (Ortega et al., 2015). Of the tests used, the 20-m shuttle run has been shown to be reliable (r = 0.84), but none of the timed runs (i.e., 10 × 20 m shuttle, 600 m run, 20-m agility run), the modified shuttle run, or the heart rate response to a set workload have been shown to be reliable in preschool-aged children (Ortega et al., 2015). This sentiment is further supported by Ruiz et al. who reported that run/walk tests are not an accurate measure of CVF in young children as there is a major challenge in developing pacing (Nguyen et al., 2011). Nevertheless, CVF is an important construct to understand in young children, as it has been shown to be consistently related to improved health profiles in adolescents and adults (Myers et al., 2015b; Ruiz et al., 2016).
5. Conclusion
This meta-analysis suggests a strong effect of ECEC-based interventions on CVF in preschool-aged children, and use of an ecological framework to develop interventions appears to impart some benefit compared to individual level interventions alone. Relative contributions of intervention components at each level of the framework have yet to be determined, but parents and educators can currently utilize components from multiple levels of the ecological model to improve the CVF profiles of their children.
Ethical approval
The research was approved by the institutional review board at Arizona State University.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This research was supported by the National Institutes of Health through the National Institute on Minority Health and Health Disparities cooperative agreement 5U01MD010667-03 awarded to Dr. Rebecca E. Lee, the National Institute of Nursing Research grant 1F31NR017560-01 awarded to Elizabeth Lorenzo, the National Cancer Institute/NIH Grant Grant 2T32CA057712-26 awarded to the University of Texas Health Science Center at Houston School of Public Health Cancer Education and Career Development Program. Partial funding by the Michael Susan Dell Center for Healthy Living for Jacob Szeszulski, the Jonas Scholar Nurse Leader 2016–2018 Cohort awarded to Elizabeth Lorenzo, and a dissertation completion fellowship awarded by Arizona State University's Graduate College to Jacob Szeszulski.
Author contributions
JS completed the search process, conceptualized the analysis, analyzed and interpreted the results, drafted the manuscript and is accountable for all aspects of the content in this manuscript. EL replicated the search process, was a major contributor to the revision of manuscript and approved the final version of this manuscript. GQS, MPB, SVL, SH, and REL provided guidance on the conceptualization of this analysis, were major contributors to the revision of manuscript and approved the final version of this manuscript. RL also obtained funding for this project and provided guidance on the conceptualization of this analysis.
Declaration of Competing Interest
The authors declare there is no conflict of interest.
Acknowledgments
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2019.100915.
Appendix A. Supplementary data
Supplementary material
References
- 2018 Physical Activity Guidelines Advisory Committee . U.S. Department of Health and Human Services; Washington, DC: 2018. Physical Activity Guidelines Advisory Committee Scientific Report.https://health.gov/paguidelines/second-edition/report/pdf/pag_advisory_committee_report.pdf [Google Scholar]
- Alpert B., Field T.M., Goldstein S., Perry S. Aerobics enhances cardiovascular fitness and agility in preschoolers. Health Psychol. 1990;9(1):48. doi: 10.1037//0278-6133.9.1.48. [DOI] [PubMed] [Google Scholar]
- Armstrong N., Tomkinson G., Ekelund U. Aerobic fitness and its relationship to sport, exercise training and habitual physical activity during youth. Br. J. Sports Med. 2011;45(11):849–858. doi: 10.1136/bjsports-2011-090200. Sep 1. [DOI] [PubMed] [Google Scholar]
- Beets M.W., Beighle A., Erwin H.E., Huberty J.L. After-school program impact on physical activity and fitness: a meta-analysis. Am. J. Prev. Med. 2009;36(6):527–537. doi: 10.1016/j.amepre.2009.01.033. Jun 1. [DOI] [PubMed] [Google Scholar]
- Beets M.W., Okely A., Weaver R.G., Webster C., Lubans D., Brusseau T., Carson R., Cliff D.P. The theory of expanded, extended, and enhanced opportunities for youth physical activity promotion. Int. J. Behav. Nutr. Phys. Act. 2016;13(1):120. doi: 10.1186/s12966-016-0442-2. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994:1088–1101. Dec 1. [PubMed] [Google Scholar]
- Borenstein M., Cooper H., Hedges L., Valentine J. The Handbook of Research Synthesis and Meta-analysis. vol. 2. 2009. Effect sizes for continuous data; pp. 221–235. Feb 5. [Google Scholar]
- Bürgi F., Meyer U., Granacher U., Schindler C., Marques-Vidal P., Kriemler S., Puder J.J. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross-sectional and longitudinal study (Ballabeina) Int. J. Obes. 2011;35(7):937. doi: 10.1038/ijo.2011.54. Jul. [DOI] [PubMed] [Google Scholar]
- Carson V., Lee E.Y., Hewitt L., Jennings C., Hunter S., Kuzik N., Stearns J.A., Unrau S.P., Poitras V.J., Gray C., Adamo K.B. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(5):854. doi: 10.1186/s12889-017-4860-0. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattuzzo M.T., dos Santos Henrique R., Ré A.H., de Oliveira I.S., Melo B.M., de Sousa Moura M., de Araújo R.C., Stodden D. Motor competence and health related physical fitness in youth: a systematic review. J. Sci. Med. Sport. 2016;19(2):123–129. doi: 10.1016/j.jsams.2014.12.004. Feb 1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Comprehensive School Physical Activity Programs: A Guide for Schools. 2013. https://www.cdc.gov/healthyschools/professional_development/e-learning/CSPAP/_assets/FullCourseContent-CSPAP.pdf Retrieved from Atlanta, GA.
- Chow B.C., McKenzie T.L., Louie L. Children's physical activity and associated variables during preschool physical education. Advances in Physical Education. 2015;5(1):39. Jan 16. [Google Scholar]
- Cools W., De Martelaer K., Samaey C., Andries C. Fundamental movement skill performance of preschool children in relation to family context. J. Sports Sci. 2011;29(7):649–660. doi: 10.1080/02640414.2010.551540. Apr 1. [DOI] [PubMed] [Google Scholar]
- Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. Sep 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliakim A., Nemet D., Balakirski Y., Epstein Y. The effects of nutritional-physical activity school-based intervention on fatness and fitness in preschool children. J. Pediatr. Endocrinol. Metab. 2007;20(6):711–718. doi: 10.1515/jpem.2007.20.6.711. [DOI] [PubMed] [Google Scholar]
- Figueroa R, An R. Motor skill competence and physical activity in preschoolers: a review. Matern. Child Health J.. 2017 Jan 1;21(1):136–46. Doi: 10.1007/s10995-016-2102-1. [DOI] [PubMed]
- Howie E.K., Brewer A.E., Dowda M., McIver K.L., Saunders R.P., Pate R.R. A tale of 2 teachers: a preschool physical activity intervention case study. J Sch Health. 2016;86(1):23–30. doi: 10.1111/josh.12352. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iruka I.U., Carver P.R. US Department of Education; Washington, DC: 2006. Initial Results from the 2005 NHES Early Childhood Program Participation Survey (NCES 2006–075)https://nces.ed.gov/pubs2006/2006075.pdf National Center for Education Statistics. [Google Scholar]
- Ishii K., Shibata A., Adachi M., Nonoue K., Oka K. Gender and grade differences in objectively measured physical activity and sedentary behavior patterns among Japanese children and adolescents: a cross-sectional study. BMC Public Health. 2015;15(1):1254. doi: 10.1186/s12889-015-2607-3. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriemler S., Zahner L., Schindler C., Meyer U., Hartmann T., Hebestreit H., Brunner-La Rocca H.P., Van Mechelen W., Puder J.J. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. Bmj. 2010;340:c785. doi: 10.1136/bmj.c785. Feb 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latorre-Román P.A., Mora-López D., García-Pinillos F. Effects of a physical activity programme in the school setting on physical fitness in preschool children. Child Care Health Dev. 2018;44(3):427–432. doi: 10.1111/cch.12550. May. [DOI] [PubMed] [Google Scholar]
- Leppänen M.H., Nyström C.D., Henriksson P., Pomeroy J., Ruiz J.R., Ortega F.B., Cadenas-Sánchez C., Löf M. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4-year-old children: results from the ministop trial. Int. J. Obes. 2016;40(7) doi: 10.1038/ijo.2016.54. Jul. [DOI] [PubMed] [Google Scholar]
- Logan S.W., Kipling Webster E., Getchell N., Pfeiffer K.A., Robinson L.E. Relationship between fundamental motor skill competence and physical activity during childhood and adolescence: a systematic review. Kinesiol Rev. 2015;4(4):416–426. Nov. [Google Scholar]
- Malina R.M. Physical activity and fitness: pathways from childhood to adulthood. Am. J. Hum. Biol. 2001;13(2):162–172. doi: 10.1002/1520-6300(200102/03)13:2<162::AID-AJHB1025>3.0.CO;2-T. Feb 1. [DOI] [PubMed] [Google Scholar]
- Malina R.M. Top 10 research questions related to growth and maturation of relevance to physical activity, performance, and fitness. Res. Q. Exerc. Sport. 2014;85(2):157–173. doi: 10.1080/02701367.2014.897592. Apr 3. [DOI] [PubMed] [Google Scholar]
- McGuire S. Institute of medicine (IOM) early childhood obesity prevention policies. Washington, DC: the national academies press; 2011. Adv Nutr. Jan. 2012;3(1):56–57. doi: 10.3945/an.111.001347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ. Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. Dec. [DOI] [PubMed] [Google Scholar]
- Meyer U, Schindler C, Zahner L, Ernst D, Hebestreit H, van Mechelen W, Brunner-La Rocca HP, Probst-Hensch N, Puder JJ, Kriemler S. Long-term effect of a school-based physical activity program (KISS) on fitness and adiposity in children: a cluster-randomized controlled trial. PLoS One. 2014 Feb 3;9(2):e87929. Doi: 10.1371/journal.pone.0087929. [DOI] [PMC free article] [PubMed]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. Aug 18. [DOI] [PubMed] [Google Scholar]
- Myers J., McAuley P., Lavie C.J., Despres J.P., Arena R., Kokkinos P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog. Cardiovasc. Dis. 2015;57(4):306–314. doi: 10.1016/j.pcad.2014.09.011. Jan 1. [DOI] [PubMed] [Google Scholar]
- Myers J., McAuley P., Lavie C.J., Despres J.P., Arena R., Kokkinos P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog. Cardiovasc. Dis. 2015;57(4):306–314. doi: 10.1016/j.pcad.2014.09.011. Jan 1. [DOI] [PubMed] [Google Scholar]
- Naylor P.J., Nettlefold L., Race D., Hoy C., Ashe M.C., Higgins J.W., McKay H.A. Implementation of school based physical activity interventions: a systematic review. Prev. Med. 2015;72:95–115. doi: 10.1016/j.ypmed.2014.12.034. Mar 1. [DOI] [PubMed] [Google Scholar]
- Nemet D., Geva D., Pantanowitz M., Igbaria N., Meckel Y., Eliakim A. Health promotion intervention in Arab-Israeli kindergarten children. J. Pediatr. Endocrinol. Metab. 2011;24:11–12. doi: 10.1515/jpem.2011.387. :10.1515/JPEM.2011.387 Dec 1. 1001-7. [DOI] [PubMed] [Google Scholar]
- Nemet D., Geva D., Eliakim A. Health promotion intervention in low socioeconomic kindergarten children. J. Pediatr. 2011;158(5):796–801. doi: 10.1016/j.jpeds.2010.10.040. May 1. [DOI] [PubMed] [Google Scholar]
- Nemet D., Geva D., Pantanowitz M., Igbaria N., Meckel Y., Eliakim A. Long term effects of a health promotion intervention in low socioeconomic Arab-Israeli kindergartens. BMC Pediatr. 2013;13(1):45. doi: 10.1186/1471-2431-13-45. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T., Obeid J., Timmons B.W. Reliability of fitness measures in 3-to 5-year-old children. Pediatr. Exerc. Sci. 2011;23(2):250–260. doi: 10.1123/pes.23.2.250. May. [DOI] [PubMed] [Google Scholar]
- Niederer I., Bürgi F., Ebenegger V., Marques-Vidal P., Schindler C., Nydegger A., Kriemler S., Puder J.J. Effects of a lifestyle intervention on adiposity and fitness in overweight or low fit preschoolers (Ballabeina) Obesity. 2013;21(3):E287–E293. doi: 10.1002/oby.20119. Mar. [DOI] [PubMed] [Google Scholar]
- O'Neill J.R., Williams H.G., Pfeiffer K.A., Dowda M., McIver K.L., Brown W.H., Pate R.R. Young children's motor skill performance: relationships with activity types and parent perception of athletic competence. J. Sci. Med. Sport. 2014;17(6):607–610. doi: 10.1016/j.jsams.2013.10.253. Nov 1. [DOI] [PubMed] [Google Scholar]
- Ortega F.B., Ruiz J.R., Mesa J.L., Gutiérrez Á., Sjöström M. Cardiovascular fitness in adolescents: the influence of sexual maturation status—the AVENA and EYHS studies. American Journal of Human Biology: Am J Hum Biol. 2007;19(6):801–808. doi: 10.1002/ajhb.20640. Nov. [DOI] [PubMed] [Google Scholar]
- Ortega F.B., Ruiz J.R., Castillo M.J., Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int. J. Obes. 2008;32(1):1. doi: 10.1038/sj.ijo.0803774. Jan. [DOI] [PubMed] [Google Scholar]
- Ortega F.B., Cadenas-Sánchez C., Sánchez-Delgado G., Mora-González J., Martínez-Téllez B., Artero E.G., Castro-Piñero J., Labayen I., Chillón P., Löf M., Ruiz J.R. Systematic review and proposal of a field-based physical fitness-test battery in preschool children: the PREFIT battery. Sports Med. 2015;45(4):533–555. doi: 10.1007/s40279-014-0281-8. Apr 1. [DOI] [PubMed] [Google Scholar]
- Pate R.R., McIver K., Dowda M., Brown W.H., Addy C. Directly observed physical activity levels in preschool children. J Sch Health. 2008;78(8):438–444. doi: 10.1111/j.1746-1561.2008.00327.x. Aug. [DOI] [PubMed] [Google Scholar]
- Pozuelo-Carrascosa D.P., García-Hermoso A., Álvarez-Bueno C., Sánchez-López M., Martinez-Vizcaino V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: a meta-analysis of randomised controlled trials. Br. J. Sports Med. 2018;52(19):1234–1240. doi: 10.1136/bjsports-2017-097600. Oct 1. [DOI] [PubMed] [Google Scholar]
- Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Gorber S.C., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2008;5(1):56. doi: 10.1186/1479-5868-5-56. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puder J.J., Marques-Vidal P., Schindler C., Zahner L., Niederer I., Bürgi F., Ebenegger V., Nydegger A., Kriemler S. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. Bmj. 2011;343:d6195. doi: 10.1136/bmj.d6195. Oct 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly J.J. Low levels of objectively measured physical activity in preschoolers in child care. Med. Sci. Sports Exerc. 2010;42(3):502–507. doi: 10.1249/MSS.0b013e3181cea100. Mar. [DOI] [PubMed] [Google Scholar]
- Review Manager (RevMan) [Computer Program]. Version 5.3. The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2014. [Google Scholar]
- Robinson L.E., Stodden D.F., Barnett L.M., Lopes V.P., Logan S.W., Rodrigues L.P., D'Hondt E. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015;45(9):1273–1284. doi: 10.1007/s40279-015-0351-6. Sep 1. [DOI] [PubMed] [Google Scholar]
- Ruiz J.R., Castro-Piñero J., España-Romero V., Artero E.G., Ortega F.B., Cuenca M.M., Jimenez-Pavón D., Chillón P., Girela-Rejón M.J., Mora J., Gutiérrez Á. Field-based fitness assessment in young people: the ALPHA health-related fitness test battery for children and adolescents. Br. J. Sports Med. 2011;45(6):518–524. doi: 10.1136/bjsm.2010.075341. May 1. [DOI] [PubMed] [Google Scholar]
- Ruiz J.R., Cavero-Redondo I., Ortega F.B., Welk G.J., Andersen L.B., Martinez-Vizcaino V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br. J. Sports Med. 2016;50(23):1451–1458. doi: 10.1136/bjsports-2015-095903. Dec 1. [DOI] [PubMed] [Google Scholar]
- SHAPE America . Author; Reston, VA: 2015. The Essential Components of Physical Education.https://www.shapeamerica.org/upload/TheEssentialComponentsOfPhysicalEducation.pdf [Google Scholar]
- Spence JC, Lee RE. Toward a comprehensive model of physical activity. Psychol. Sport Exerc.. 2003 Jan 1;4(1):7–24. Doi: 10.1016/S1469-0292(02)00014-6. [DOI]
- Stodden D.F., Goodway J.D., Langendorfer S.J., Roberton M.A., Rudisill M.E., Garcia C., Garcia L.E. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest. 2008;60(2):290–306. May 1. [Google Scholar]
- Tan S., Chen C., Sui M., Xue L., Wang J. Exercise training improved body composition, cardiovascular function, and physical fitness of 5-year-old children with obesity or normal body mass. Pediatr. Exerc. Sci. 2017;29(2):245–253. doi: 10.1123/pes.2016-0107. May. [DOI] [PubMed] [Google Scholar]
- Van Sluijs E.M., McMinn A.M., Griffin S.J. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. Bmj. 2007;335(7622):703. doi: 10.1136/bmj.39320.843947.BE. Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warburton D.E., Charlesworth S., Ivey A., Nettlefold L., Bredin S.S. A systematic review of the evidence for Canada's physical activity guidelines for adults. Int. J. Behav. Nutr. Phys. Act. 2010;7(1):39. doi: 10.1186/1479-5868-7-39. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward D.S., Vaughn A., McWilliams C., Hales D. Interventions for increasing physical activity at child care. Med. Sci. Sports Exerc. 2010;42(3):526–534. doi: 10.1249/MSS.0b013e3181cea406. Mar. [DOI] [PubMed] [Google Scholar]
- Wechsler H., Devereaux R.S., Davis M., Collins J. Using the school environment to promote physical activity and healthy eating. Prev. Med. 2000;31(2):S121–S137. Aug 1. [Google Scholar]
- Wenger H.A., Bell G.J. The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports Med. 1986;3(5):346–356. doi: 10.2165/00007256-198603050-00004. Sep 1. [DOI] [PubMed] [Google Scholar]
- Zhou Z., Ren H., Yin Z., Wang L., Wang K. A policy-driven multifaceted approach for early childhood physical fitness promotion: impacts on body composition and physical fitness in young Chinese children. BMC Pediatr. 2014;14(1):118. doi: 10.1186/1471-2431-14-118. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.