Abstract
Within the realm of clubfoot deformities, teratologic and complex (or atypical) clubfeet stand out as the most difficult. Exemplarities of the teratologic types of clubfoot are those associated with arthrogryposis multiplex congenita.
Treatment of arthrogrypotic clubfoot deformities has been controversial; many different procedures have been advocated, with variable success rates. These clubfeet have a high recurrence rate, regardless of treatment type. Often, the high recurrence rate has led to a high repeat surgery rate, and poor outcomes. Treatment strategies should highlight care that avoids the development of a stiffened foot and allows for a variety of options to regain correction when a relapse occurs. Modifications of the Ponseti method for idiopathic clubfeet have been successful in managing the deformity. The equinocavus variant of the arthrogrypotic clubfoot should be distinguished from the classic clubfoot, as it requires a different treatment method. The equinocavus clubfoot is very similar to the complex or atypical clubfoot.
The complex, or atypical, clubfoot also requires a different treatment strategy compared with the typical idiopathic congenital clubfoot. The complex clubfoot appears to be idiopathic in some cases and iatrogenic (due to slipping stretching casts) in others. Dr. Ponseti’s modification of his protocol has been effective in treating the deformity. The high recurrence rate suggests the difficulty in maintaining the deformity after correction. The author’s preferred treatment for each deformity is included, with an emphasis on minimally invasive methods.
Level of Evidence
Level V, expert opinion
Keywords: arthrogryposis, arthrogryposis multiplex congenita, arthrogrypotic clubfoot, complex clubfoot, atypical clubfoot, Ponseti, clubfeet
Introduction
In the nearly six decades since IV Ponseti published his first article on his technique for serial cast management of idiopathic clubfeet,1 the method, and more importantly the overall concept, has been expanded and modified to address the non-idiopathic (syndromic) clubfoot or clubfoot-associated conditions. Ponseti originally doubted the applicability of his method to the syndromic clubfoot deformities, as these differed from the idiopathic ones by originating much earlier in utero, therefore, having much less pliability of the soft tissues and greater muscle imbalances, leading to persistent and recurrent deformity.2 Over time, the method, often with small changes in approach, proved to be successful in these teratologic clubfeet. As the range of syndromes with associated clubfoot deformities is vast, we will limit our discussion to clubfeet associated with arthrogryposis multiplex congenita, although many of the concepts are relevant for the other syndromic clubfeet. Then, we will discuss the challenging atypical or complex clubfoot deformity, which Ponseti recognized late in his career, and provided important guidance on how to correct.3
Arthrogryposis multiplex congenita
Arthrogryposis multiplex congenita, or arthrogryposis, is a term that describes a collection of more than 400 conditions with the affected baby born with contractures of at least two or more joints in multiple body areas.4,5 What these conditions have in common is foetal akinesia, the lack of spontaneous movement intra-uterinely, usually due to nerve or muscle abnormalities, or constricting soft tissues. The contractures are secondary to the intrauterine lack of movement (foetal akinesia) of the developing joint, following which the normally pliant soft tissues surrounding the joints undergo fibrosis.4 The incidence of arthrogryposis is approximately one out of every 3000 live births, with amyoplasia, the most common or classic form, occurring in one of every 10 000 births.4
There are essentially two forms of arthrogrypotic clubfoot deformities, the ‘classic’ clubfoot (Fig. 1) and the equinocavus clubfoot variant (Fig. 2). For completeness, the congenital vertical talus is the third arthrogrypotic foot deformity.
Fig. 1.

The ‘classic’ arthrogrypotic clubfoot. Both feet of this two-month-old boy have severe heel varus, supination and adductus.
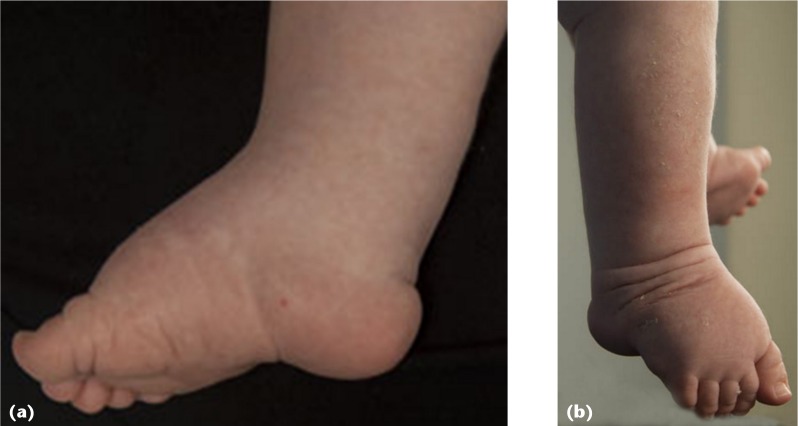
Fig. 2.

Equinocavus clubfoot variant: (a) lateral view of the left foot depicting the severe hindfoot equinus and deep transverse cavus. The toes are mildly flexed in this uncorrected foot; (b) dorsal view of the same foot, showing relatively mild forefoot adductus
Classic clubfoot
The classic clubfoot is the most common and tends to be more rigid and severe than the idiopathic clubfoot.6–10 To make the most of the suppleness of the newborn, it is usually recommended to start treatment early. Historically treatment has been surgical, with progressively more extensive procedures advocated as both primary and secondary interventions, particularly soft-tissue releases and talectomies.
Soft-tissue releases
Soft-tissue procedures range from the simple Achilles tenotomy to the ‘radical’ soft-tissue release.6,7,10–20 Satisfactory results reportedly range from 100% to 21% for different soft-tissue procedures, with the suggestion that better results have been obtained by operating at an earlier age with more aggressive procedures. However, longer follow-ups have often indicated less favourable results. Drummond and Cruess7 reported on 23 patients who underwent posterior releases at an average age of 2.7 years, of which only six were satisfactory at an average ten-year follow-up. Similarly, Niki et al14 described a 73% relapse rate at an average of nearly ten years for 41 clubfeet in 22 patient with amyoplasia, following posteromedial releases at an average age of 7.3 months; 22 feet underwent subsequent serial casting of which eight responded well. Only 25% of Guidera and Drennan’s11 28 feet in 15 patients that had undergone posteromedial releases were considered successful at an average 12-year follow-up. Carlson et al6 found that, of their 26 patients who underwent clubfoot surgery at a mean of 3.6 years, 73% required an additional 2.5 procedures on average per foot. Södergård and Ryöppy18 performed soft-tissue releases on 52 of 72 arthrogrypotic clubfeet, at an average of three weeks of age, with a success rate of 48% at a follow-up of one to 36 years, whereas the other 20 had a 75% success rate with casting alone. Kowalczyk and Felus21 found that 28% of their 39 feet that underwent soft-tissue releases had unsatisfactory outcomes at nine-year follow-up, with a complication rate of 23%; 74% of feet required an average of 1.4 further procedures. Menelaus9 theorized that insufficient release of the medial soft tissues lead to the high rate of relapse, along with the lack of adaptive changes of the medial tarsal bones, which remain wedged apart medially rather than moulding conformingly to each other.
Talectomy
Talectomies and arthrogrypotic clubfeet have a long history together, both as a primary procedure7,9,11,22–25 and for salvage after recurrences.7,11,22–28 The procedure achieves correction by creating laxity in the hindfoot, allowing it to roll out of equinus and varus, and positioning the calcaneus within the ankle mortise for a stable neojoint.9,22,23,28 Talectomies, though, do not adequately addressed the forefoot deformity.26,28 Spontaneous calcaneotibial arthrodeses occur, which may lead to rigid foot positioning, often in equinus, point loading on skin and decubiti formation.23,25,29–31 The literature presents a complex and fragmented picture, as most studies group primary and salvage talectomy procedures together. Cassis and Capdevila22 described results in 16 primary and 85 salvage talectomies done at an average age of 4.3 years, with mean follow-up of six years. They reported 65% good results, which they generously defined as < 15° of equinus and adductus. Green et al,27 however, noted that relapses occurred two to six years after the operation in their average 11-year follow-up of 34 feet in 18 patients. Their success rate was 56%, with half the cases done as a primary talectomies. D’Souza et al32 also had an average 11-year follow-up, on 11 children with 21 talectomies, eight of which were the primary procedure. The talectomies were performed at a mean age of 3.5 years, with a satisfactory rate (< 10° equinus) of 74%. Sølund et al30 reviewed 14 feet in eight children that underwent talectomy as a salvage procedure at a mean age of eight years, with an average 13-year follow-up, and found a success rate of 64%. Some authors have suggested that talectomies should be the primary procedure for all arthrogrypotic clubfeet, but those authors base their recommendations on one or two patients in their studies, with limited documented follow-up.11,30 Larger series report the satisfactory rate of primary talectomies as only 45% to 50%.7,15,23,24
External fixator correction
The earliest articles on correcting severe clubfoot deformities with the Ilizarov frame were published by Franke et al33 and Grill and Franke.34 They avoided osteotomies, relying instead on soft-tissue distraction to facilitate correction. Only one of five patients in their initial series had arthrogryposis. Surgery was done at an average age of 11 years, and all feet were plantargrade at the three-year follow-up, although stiffness of the subtalar and midfoot joints was common.34 Their subsequent article included four similarly treated arthrogrypotic clubfeet with a five-year follow-up. All feet were plantargrade and all participants were satisfied to wear normal shoes.33 Brunner et al35 used a soft-tissue distraction Ilizarov frame to correct the equinus of 16 arthrogrypotic clubfeet. Their success rate was 63% at 34 months, with a number of the failures requiring talectomies. Choi et al36 also used Ilizarov soft-tissue distraction to correct 12 recurrent arthrogrypotic clubfeet, at a mean age of five years. At a mean follow-up of 35 months, all but two of the feet were plantargrade. El Barbary et al37 had 23 arthrogrypotic clubfeet treated at an average of 8.5 years of age with soft-tissue distraction using an Ilizarov frame. They reported all feet were plantargrade, despite a few with mild adductus, at an average of 40 months.
Serial casting
A number of studies have demonstrated that the Ponseti method is effective in treating arthrogrypotic clubfeet.21,38–44 Boehm et al41 treated 24 clubfeet in 12 babies born with distal arthrogryposis. At a minimum two-year follow-up, six feet had relapsed, of which four were corrected with casting and the other two required extensive soft-tissue releases. Morcuende et al39 treated 32 clubfeet in 16 patients with arthrogryposis, with an average four-year follow-up. Five patients required extensive soft-tissue release, either due to lack of correction or relapse. Janicki et al38 reviewed a mixed group of non-idiopathic clubfeet treated with the Ponseti method, including eight arthrogrypotic feet in five patients. Two patients had a good result, two more had bilateral failures requiring surgery, and one had bilateral recurrences treated with casting. Kowalczyk and colleagues reported on two series of pediatric patients treated for their clubfeet with the Ponseti method. The first study43 was on five children (ten feet) with an average follow-up of nearly three years. Three children used standard Ponseti-style foot abduction braces (FAB), the other two used ankle-foot orthoses (AFO) or dorsiflexion AFOs, all adhering to the wear schedule of day and night for three months, then nighttime alone thereafter, as well as whatever was needed for daytime ambulation. Three feet required repeat Achilles tenotomies at an average of 12 months post-treatment and six feet required more invasive surgical correction for recurrence, also performed on average 12 months after initial treatment. The second study45 evaluated nine children (18 feet) with an average 7.3-year follow-up. At an average of 27 months after correction, 16 feet required further corrective but non-ablative surgeries. Matar et al44 reviewed 17 feet of ten children with arthrogryposis, of which 11 did not require surgical intervention in the 5.8-year follow-up.
Author’s preference
In 2009, we published a small series, our first 19 clubfeet in ten patients with arthrogryposis corrected with the Ponseti technique.40 At an average 38-month follow-up, eight feet had relapses, requiring repeat casting, and two patients (four feet) required posterior ankle releases. Since that time, my practice has evolved to a caseload of approximately 75% arthrogryposis patients, the majority of which require clubfoot casting, amounting to several hundred arthrogrypotic clubfeet (Fig. 3). With that volume of cases and length of experience, it has become clear that most arthrogrypotic clubfeet have a penchant for relapse, regardless if the initial treatment was surgical or serial casting. Rather than treat the relapses with intensive procedures, I have moved towards repeated serial casting, with percutaneous Achilles tenotomies as needed. We inform parents at our first meeting of the recurrent nature of this foot deformity and attempt to space the time between casting series by at least a year, usually two to four years, so long as the foot can be comfortably braced, and the deformity does not hinder ambulation. We find that as a child grows, relapses become less frequent, and the feet essentially stop recurring somewhere between eight and 12 years of age.
Fig. 3.
22-month-old girl with bilateral classic arthrogrypotic clubfeet, had initial and incomplete casting as an newborn: (a) right foot pre-casting anterior view demonstrating the severe adductus; (b) lateral view of the same foot, with severe equinus and cavus; (c) plantar view of the same foot, with severe forefoot adductus and supination and hindfoot varus; (d) plantar view of the right foot, one month later, immediately prior to Achilles tenotomy; (e) lateral view just prior to Achilles tenotomy; (f) lateral view just after tenotomy; after removal of the post-tenotomy cast, 10° of dorsiflexion was possible.
In our original series, I would perform an initial percutaneous Achilles tenotomy on all patients. Now, only feet with severe equinus, typically greater than 40°, will undergo a percutaneous Achilles tenotomy just prior to the first cast. In the severe equinus position, the calcaneus is ‘locked’ behind the tibia, and cannot swing out of varus, so the tenotomy is not meant to directly improve ankle dorsiflexion, but allow rotation of the calcaneus out of varus. In approximately half the cases, a second Achilles tenotomy is required prior to the final cast.
Arthrogrypotic clubfeet are stiffer than idiopathic ones, and many of the children we treat are older than infants. Therefore, more corrective pressure is needed, which translates to more pressure at the pivot point, the lateral head of the talus, to counter the abduction forces of stretching and casting. This could cause skin injury with the standard of thumb or finger pressure directly over the lateral head of the talus. In such cases, the pressure should be more widely and evenly distributed by applying the flat of the stabilizing hand over the anterolateral aspect of the ankle/foot dorsum. It is important to avoid pressure over the lateral malleolus. Alternatively, the flexed knee can be held firmly, so that when abducting the forefoot, the ankle mortise stabilizes the talus.
Other authors have also noted that the standard Ponseti style FAB, important for idiopathic clubfeet, is not effective for arthrogrypotic ones.43–45 When I began treating arthrogryposis clubfeet, I too used the standard FAB, but was frustrated with the very rapid relapses. Children with arthrogryposis do not kick like those with idiopathic clubfeet, which is important for stretching the ankles and preventing the recurrence of equinus. Also, the hips often have external rotational and abduction contractures and knees have flexion contractures, making effective positioning of the brace difficult. Therefore, once correction is obtained and the final cast comes off after three to four weeks, an AFO is applied, moulded to correct heel varus and forefoot adductus, with the anterior ankle strap starting inside laterally, to roll the ankle in to valgus. The braces are usually made with removable medial and lateral dorsiflexion straps to stretch the ankles at nighttime, dubbed a dual purpose AFO (Fig. 4).
Fig. 4.
Left dual purpose ankle foot orthosis moulded for correction of hindfoot varus and forefoot adductus, the anterior ankle strap originating in the inner lateral aspect of the brace: (a) perspective from directly anterior, demonstrating the straight medial border. Further corrective pads are often placed at the lateral supramalleolar and medial forefoot areas; (b) medial view, with leaf spring ankle visible; (c) anterior perspective with removable dorsiflexion straps in position. The lateral one is tensioned more than the medial, to maintain pronation; (d) medial view with dorsiflexion straps.
These strategies have worked well, even in those patients referred after relapses following aggressive soft-tissue releases or talectomies, and with neglected arthrogrypotic clubfeet in older children, even into the teenage years. Something that I only came to understand in the last few years is that many of these patients have severe external torsion of their tibias. So, once the foot appears to be corrected, the forefoot is still much more medially directed compared with the outwardly turned talus. This is often inconsequential, so long as the foot aligns well with the knee, and recurrences are not excessive. But in cases where the corrected foot is severely externally rotated, or recurrences are hard to control, a derotational osteotomy of the tibia may be needed.
The ‘soft-tissue Ilizarov frame’ has been effective for the occasional teenager with a severely rigid deformity, without bony ankylosis. Initial casting may decrease the deformity enough to make frame application less taxing. I have only used this for children 12 years or older, with little growth remaining. Essentially the external fixator is applied to the foot without soft-tissue releases or osteotomies, with subsequent correction mimicking the Ponseti method of abduction stretching.33–37 In severe feet with iatrogenic bony coalitions, osteotomies are necessary to allow the foot to reorientate; using an external fixator in these cases allow for a non-shortening correction.
In the past ten years, I have not performed extensive clubfoot procedures such as posterior medial releases, talectomies or decancellations on any clubfoot I treat, be it idiopathic or arthrogrypotic. In the occasional case, some procedures may be necessary at skeletal maturity to improve stability or comfort, including a lateral sliding calcaneal osteotomy (reverse Koutsogiannis), to correct heel varus,29 or a shaving down of the prominent base of the fifth metatarsal, which can be a painful lateral or plantar bump.
Equinocavus foot
The equinocavus foot is a variant of the typical clubfoot, but with important treatment implications. The feet have equinus and complete midfoot cavus as the major deformities, with a medial-to-lateral plantar midfoot skin crease. Heel varus, forefoot supination and adductus are relatively minor components (Fig. 2). The foot appears strikingly similar to the ‘atypical’ or ‘complex’ clubfoot,3 discussed in the next section, often including the hammertoe/shortened position of the great toe. One of the differences is that all the toes tend to have flexion contractures, which are often very resistant to stretching. I had treated a number of these with the standard Ponseti method before recognizing their significance – this led to ugly equino-valgus-adductus feet with mid-foot breaks that were challenging to reverse. The appropriate stretching method is similar to that of the atypical clubfoot, where the index and forefingers of both hands are placed on the dorsum of the midfoot, just anterior to the ankle joint, the thumbs are positioned under the metatarsal heads. The goal initially is to correct the midfoot cavus, with gradual upwards pressure on the metatarsal heads relative to the midfoot (Fig. 5). Once the cavus is fully corrected, the Achilles tenotomy is performed, but not before, as it is difficult to stabilize the hindfoot during stretching after the Achilles tenotomy. After correction, a dual purpose AFO is used. It is my impression that the equinocavus feet seem to have a lower tendency to relapse, if well braced, although the toe flexion contractures may need flexor tenotomies in time.
Fig. 5.
Equinocavus clubfoot variant in a two-month-old girl: (a) plantar view of left foot, demonstrating medial to lateral plantar crease; (b) medial view showing severe ankle and midfoot equinus, with plantarflexed great toe; (c) the ‘four finger’ technique, the index and long fingers of both hands are positioned over the midfoot to act as a fulcrum, while the thumbs apply dorsiflexion pressure under the heads of the metatarsals. The intact Achilles tendon acts as a counter force, therefore, an Achilles tenotomy should be delayed until full correction of the midfoot cavus; (d) the same foot dorsal view, weight-bearing at seven years’ follow-up; (e) plantar view. The only other treatment she required was percutaneous toe flexor tenotomies at three years of age.
Complex or atypical clubfoot
In 2006, Ponseti et al3 reported for the first time on what they termed the ‘complex’ clubfoot, one that was in severe equinus and supination, with a shortened and stubby appearance to the forefoot, a forefoot that was mildly adducted but in significant equinus relative to the mid foot, with a deep medial to lateral plantar crease at the midfoot. The big toe was often in a hammertoe position, which made it appear shorter, with a characteristic dorsal crease at the base of the toe (Fig. 6). The authors accredited Turco with describing the deformity in 1994,46 calling it the ‘atypical idiopathic clubfoot’, and the entity has since been referred to interchangeably in the literature as ‘complex’ and ‘atypical’. Turco, after describing the condition, warned against operating on it, as it could result in a ‘grotesquely deformed foot’.
Fig. 6.
three-month-old girl with an idiopathic clubfoot, but with ten previous casts prior to presentation; (a) medial view of right foot, demonstrating high midfoot cavus, deep plantar and posterior ankle ceases and a foreshortened great toe; (b) dorsal view of the same foot with a deep crease at the base of the great toe.
It is unclear from the limited literature on the complex or atypical clubfoot what its overall incidence is. In their international study at five centres, Ponseti et al3 identified 50 children, half who were bilaterally affected, from the pool of 762 children with clubfeet, for an incidence of 6.5%. A total of 17% of the children referred to Dragoni et al47 after failed cast treatment elsewhere had complex clubfeet. In the Bangladesh Clubfoot Project, the incidence was calculated as 13% of 1040 patients in one study, and 21% of 400 randomly selected patients from their ten largest clinics in a follow-up series.48,49 Van Praag et al50 noted a 9% incidence in 77 patients and Yoshioka et al51 found a 13% incidence in 837 patients. In many of these articles, it is unclear how many patients were diagnosed with the complex clubfoot prior to any treatment, which is important to know when trying to distinguish idiopathic from iatrogenic deformities.
Many of the complex clubfeet appear to be idiopathic, present at birth, deformities. In all, 19 of the 50 patients featured in Ponseti et al’s3 original article had no prior treatment before being evaluated at one of the authors’ five centres, whereas the other 31 initially had treatment elsewhere and the authors could not verify the foot shape at birth. Therefore, in their study, at least 38% were idiopathic. Matar et al52 described 11 patients with 17 complex clubfeet, although three of those patients had originally undergone treatment elsewhere, and may have instead presented to the authors with an acquired complex clubfoot. Huertas and Rosselli42 described in a case report, supported with illustrative photographs, a ten-day old baby born with clubfeet bearing the traits of an idiopathic complex clubfoot, including a deep transverse plantar and posterior ankle creases, and a shortened first ray. Two articles have suggested a neurological dysfunction of the peroneal nerve as possibly related to the complex clubfoot. Edmonds and Frick53 described nine patients with clubfeet and absent anterior and lateral compartment function, epitomized by the lack of toe extension. Two of their patients had recurrent cast slippage, subsequently developing atypical clubfeet. Yoshioka et al51 found that eight of their 111 patients with complex clubfeet (ten feet) had findings of peroneal nerve dysfunction, varying from weak to absent ankle and/or toe dorsiflexion/extension. It is important to note that only five of those children had idiopathic clubfeet, the others had arthrogryposis or chromosomal abnormalities, and all had undergone extensive cast treatment elsewhere (average of 15 casts) prior to presentation. Two patients had partial peroneal nerve recovery. One patient was found to have nerve dysfunction after treatment at the authors’ institution, which they thought might be due to pressure of the peroneal nerve in cast.
Many of the complex clubfeet appear to be iatrogenic, occurring after the typical idiopathic clubfoot slips in its stretching casts. Göksan et al54 reported that approximately half of their cases of complex clubfeet (seven of 15 feet) were known to be iatrogenic. Dragoni et al47 observed a series of 54 idiopathic clubfeet treated unsuccessfully elsewhere, of which 26 had slippage in casts, and nine of those were complex. In the Bangladeshi programme, the authors noted that the incidence of complex clubfeet was likely higher than the 13% reported, due to poor early recognition of the deformity.48 Complications were more common with the complex clubfeet, including slipped casts, foot oedema and pressure sores, which, if interpreted another way, could indicate that ill-fitting casts led to the development of the complex deformity. The slipping of casts leads to forced forefoot plantarflexion relative to the midfoot, resulting in the severe midfoot cavus. This is occasionally accompanied by an appearance of apparent cast-induced anterior tibial bowing, but which actually is compression of the posterior calf musculature anteriorly, likely due to pressure of the cast on the posterior compartment. This pressure probably occurs at the region where the posterior knee crease of the slipped cast comes into contact with the posterior musculature. It may be in that same process that the peroneal nerve suffers compression in those cases with acquired nerve palsy. Interestingly, the complex clubfoot has some similarities to the images of feet that had undergone foot-binding in China.
Treatment, as discussed in the section on arthrogrypotic equinocavus clubfeet, was detailed by Ponseti et al,3 and is occasionally referred to as the ‘four finger technique’. The index and long fingers of both hands are positioned over the dorsum of the foot just anterior to the ankle joint, creating a fulcrum of the head of the talus. Both thumbs then push upwards on the metatarsal heads, dorsiflexing the forefoot relative to the hindfoot, through the midfoot (Fig. 5). Ponseti recommended flexing the knee at least 110°, and not abducting the foot past 40°. An Achilles tenotomy is usually necessary just prior to placing the last cast, after the midfoot equinus is corrected. After completion of serial casting, the foot is placed in a standard FAB, with the affected foot only externally rotated 40°. A few authors have noted that the complex clubfoot required more casts on average than the typical clubfoot.3,52,54
Relapse occurred often, 14% in Ponseti’s series at an average of 1.5 months after correction.3 All of their relapses were treated with repeat casting and Achilles tenotomies as necessary. Dragoni et al47 had a 55% relapse rate of their complex clubfeet, which they treated with Achilles tenotomy/lengthening and/or transfer of the anterior tibialis tendon. Yoshioka et al51 noted a 37% relapse rate, which responded well to repeat casting, other than one patient that required an anterior tibialis tendon transfer. Matar et al52 treated their 53% relapses with repeat casting, most with second Achilles tenotomies, but approximately half of the relapsed feet required soft-tissue releases.
Author’s preference
Dr. Ponseti’s modified technique for casting the complex clubfoot is a testament to his deep understanding of foot mechanics, and his knowledge of how to counter deforming forces. I find that the ‘four finger technique’ is very reliable; occasionally, some amount of forefoot abduction is required early on, as intoned by Ponseti, to correct adductus, but this should be done judiciously, to prevent overcorrection into a grotesque and stubborn abductus deformity. I no longer flex the knee past 90°, as I found that trying for hyperflexion could mould the posterior calf musculature into an embarrassing (although reversible) appearance suggestive of an anterior tibial bow. Worse, the hyperflexion, by limiting the posterior upper boundary of the cast behind the knee, could actually lead to cast slippage, as the upper calf settled into the recess behind the knee of the cast. Instead, we place a well-fitting cast, flattening the upper anterior thigh of the cast to prevent kicking of the knee, and moulding well behind the knee itself without placing undo pressure in the popliteal fossa (Fig. 7). I now treat my complex clubfeet with a dorsiflexion AFO, rather than a FAB. Anecdotally, we seem to have fewer relapses of our complex clubfeet than we do of our typical clubfeet.
Fig. 7.
Cast moulding to prevent cast slippage. The upper anterior thigh region is made flat, if not actually concave, to prevent kicking of the knee. The proximal tibia is pushed posteriorly on the femur and the anterior border of the tibial section is flat.
Conclusion
Arthrogrypotic clubfoot deformities are challenging both to obtain and to maintain correction. Relapse rates are high and should be expected regardless of the method of treatment. A ‘one and done’ solution would naturally be preferred, but at this time no such procedure is known. I consider serial casting to be the best overall treatment strategy, especially since the relapsed clubfoot can usually be corrected repeatedly by casting with little morbidity to the foot. Those that are more challenging to maintain correction may have external tibial torsion that needs to be corrected.
The complex or atypical idiopathic clubfoot probably occurs both spontaneously as well as iatrogenically. In spontaneous cases, a thorough neurological workup should be done, particularly to rule out abnormalities of the neurological structures of the anterior and lateral calf compartments. The iatrogenic complex clubfoot should be suspected in cases of frequent slipping in casts and should be addressed by changing casting technique to the modified Ponseti technique.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: This work did not involve human participants and/or animals.
Informed consent: No informed consent was required.
ICMJE Conflict of interest statement
The author declares that he has no conflict of interest.
References
- 1.Ponseti IV, Smoley EN. Congenital club foot: The results of treatment. J Bone Joint Surg [Am] 1963;45-A:261–275. [Google Scholar]
- 2.Ponseti IV. Congenital clubfoot: fundamentals of treatment. New York, NY: Oxford University Press Inc, 1996. [Google Scholar]
- 3.Ponseti IV, Zhivkov M, Davis N, et al. . Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res 2006;451:171–176. [DOI] [PubMed] [Google Scholar]
- 4.Hall JG. Arthrogryposis multiplex congenita: etiology, genetics, classification, diagnostic approach, and general aspects. J Pediatr Orthop B 1997;6:159–166. [PubMed] [Google Scholar]
- 5.Bevan WP, Hall JG, Bamshad M, et al. . Arthrogryposis multiplex congenita (amyoplasia): an orthopaedic perspective. J Pediatr Orthop 2007;27:594–600. [DOI] [PubMed] [Google Scholar]
- 6.Carlson WO, Speck GJ, Vicari V, Wenger DR. Arthrogryposis multiplex congenita. A long-term follow-up study. Clin Orthop Relat Res 1985;194:115–123. [PubMed] [Google Scholar]
- 7.Drummond DS, Cruess RL. The management of the foot and ankle in arthrogryposis multiplex congenita. J Bone Joint Surg [Br] 1978;60-B:96–99. [DOI] [PubMed] [Google Scholar]
- 8.Hall JG, Reed SD, Driscoll EP. Part I. Amyoplasia: a common, sporadic condition with congenital contractures. Am J Med Genet 1983;15:571–590. [DOI] [PubMed] [Google Scholar]
- 9.Menelaus MB. Talectomy for equinovarus deformity in arthrogryposis and spina bifida. J Bone Joint Surg [Br] 1971;53-B:468–473. [PubMed] [Google Scholar]
- 10.Zimbler S, Craig CL. The arthrogrypotic foot plan of management and results of treatment. Foot Ankle 1983;3:211–219. [DOI] [PubMed] [Google Scholar]
- 11.Guidera KJ, Drennan JC. Foot and ankle deformities in arthrogryposis multiplex congenita. Clin Orthop Relat Res 1985;194:93–98. [PubMed] [Google Scholar]
- 12.Hahn G. Arthrogryposis. Pediatric review and habilitative aspects. Clin Orthop Relat Res 1985;194:104–114. [PubMed] [Google Scholar]
- 13.Khan MA, Chinoy MA. Treatment of severe and neglected clubfoot with a double zigzag incision: outcome of 21 feet in 15 patients followed up between 1 and 5 years. J Foot Ankle Surg 2006;45:177–181. [DOI] [PubMed] [Google Scholar]
- 14.Niki H, Staheli LT, Mosca VS. Management of clubfoot deformity in amyoplasia. J Pediatr Orthop 1997;17:803–807. [PubMed] [Google Scholar]
- 15.Palmer PM, MacEwen GD, Bowen JR, Mathews PA. Passive motion therapy for infants with arthrogryposis. Clin Orthop Relat Res 1985;194:54–59. [PubMed] [Google Scholar]
- 16.Sells JM, Jaffe KM, Hall JG. Amyoplasia, the most common type of arthrogryposis: the potential for good outcome. Pediatrics 1996;97:225–231. [PubMed] [Google Scholar]
- 17.Simons GW. Complete subtalar release in club feet. Part I—A preliminary report. J Bone Joint Surg [Am] 1985;67-A:1044–1055. [PubMed] [Google Scholar]
- 18.Södergård J, Ryöppy S. Foot deformities in arthrogryposis multiplex congenita. J Pediatr Orthop 1994;14:768–772. [DOI] [PubMed] [Google Scholar]
- 19.Widmann RF, Do TT, Burke SW. Radical soft-tissue release of the arthrogrypotic clubfoot. J Pediatr Orthop B 2005;14:111–115. [DOI] [PubMed] [Google Scholar]
- 20.Williams P. The management of arthrogryposis. Orthop Clin North Am 1978;9: 67–88. [PubMed] [Google Scholar]
- 21.Kowalczyk B, Felus J. Ponseti casting and achilles release versus classic casting and soft tissue releases for the initial treatment of arthrogrypotic clubfeet. Foot Ankle Int 2015;36:1072–1077. [DOI] [PubMed] [Google Scholar]
- 22.Cassis N, Capdevila R. Talectomy for clubfoot in arthrogryposis. J Pediatr Orthop 2000;20:652–655. [DOI] [PubMed] [Google Scholar]
- 23.D’Souza H, Aroojis A, Yagnik MG. Rotation fasciocutaneous flap for neglected clubfoot: a new technique. J Pediatr Orthop 1998;18:319–322. [PubMed] [Google Scholar]
- 24.Segal LS, Mann DC, Feiwell E, Hoffer MM. Equinovarus deformity in arthrogryposis and myelomeningocele: evaluation of primary talectomy. Foot Ankle 1989;10:12–16. [DOI] [PubMed] [Google Scholar]
- 25.Hsu LC, Jaffray D, Leong JC. Talectomy for club foot in arthrogryposis. J Bone Joint Surg [Br] 1984;66-B:694–696. [DOI] [PubMed] [Google Scholar]
- 26.Dias LS, Stern LS. Talectomy in the treatment of resistant talipes equinovarus deformity in myelomeningocele and arthrogryposis. J Pediatr Orthop 1987;7:39–41. [DOI] [PubMed] [Google Scholar]
- 27.Green AD, Fixsen JA, Lloyd-Roberts GC. Talectomy for arthrogryposis multiplex congenita. J Bone Joint Surg [Br] 1984;66-B:697–699. [DOI] [PubMed] [Google Scholar]
- 28.Legaspi J, Li YH, Chow W, Leong JC. Talectomy in patients with recurrent deformity in club foot. A long-term follow-up study. J Bone Joint Surg [Br] 2001;83-B:384–387. [DOI] [PubMed] [Google Scholar]
- 29.Koutsogiannis E. Treatment of mobile flat foot by displacement osteotomy of the calcaneus. J Bone Joint Surg [Br] 1971;53-B:96–100. [PubMed] [Google Scholar]
- 30.Sølund K, Sonne-Holm S, Kjølbye JE. Talectomy for equinovarus deformity in arthrogryposis. A 13 (2–20) year review of 17 feet. Acta Orthop Scand 1991;62:372–374. [DOI] [PubMed] [Google Scholar]
- 31.Nicomedez FP, Li YH, Leong JC. Tibiocalcaneal fusion after talectomy in arthrogrypotic patients. J Pediatr Orthop 2003;23:654–657. [DOI] [PubMed] [Google Scholar]
- 32.D’Souza H, Aroojis A, Chawara GS. Talectomy in arthrogryposis: analysis of results. J Pediatr Orthop 1998;18:760–764. [PubMed] [Google Scholar]
- 33.Franke J, Grill F, Hein G, Simon M. Correction of clubfoot relapse using Ilizarov’s apparatus in children 8–15 years old. Arch Orthop Trauma Surg 1990;110:33–37. [DOI] [PubMed] [Google Scholar]
- 34.Grill F, Franke J. The Ilizarov distractor for the correction of relapsed or neglected clubfoot. J Bone Joint Surg [Br] 1987;69-B:593–597. [DOI] [PubMed] [Google Scholar]
- 35.Brunner R, Hefti F, Tgetgel JD. Arthrogrypotic joint contracture at the knee and the foot: correction with a circular frame. J Pediatr Orthop B 1997;6:192–197. [DOI] [PubMed] [Google Scholar]
- 36.Choi IH, Yang MS, Chung CY, Cho TJ, Sohn YJ. The treatment of recurrent arthrogrypotic club foot in children by the Ilizarov method. A preliminary report. J Bone Joint Surg [Br] 2001;83-B:731–737. [DOI] [PubMed] [Google Scholar]
- 37.El Barbary H, Abdel Ghani H, Hegazy M. Correction of relapsed or neglected clubfoot using a simple Ilizarov frame. Int Orthop 2004;28:183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Janicki JA, Narayanan UG, Harvey B, et al. . Treatment of neuromuscular and syndrome-associated (nonidiopathic) clubfeet using the Ponseti method. J Pediatr Orthop 2009;29:393–397. [DOI] [PubMed] [Google Scholar]
- 39.Morcuende JA, Dobbs MB, Frick SL. Results of the Ponseti method in patients with clubfoot associated with arthrogryposis. Iowa Orthop J 2008;28:22–26. [PMC free article] [PubMed] [Google Scholar]
- 40.van Bosse HJ, Marangoz S, Lehman WB, Sala DA. Correction of arthrogrypotic clubfoot with a modified Ponseti technique. Clin Orthop Relat Res 2009;467:1283–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boehm S, Limpaphayom N, Alaee F, Sinclair MF, Dobbs MB. Early results of the Ponseti method for the treatment of clubfoot in distal arthrogryposis. J Bone Joint Surg [Am] 2008;90-A:1501–1507. [DOI] [PubMed] [Google Scholar]
- 42.Huertas R, Rosselli P. Complex congenital clubfoot: a case report. Acta Ortop Mex 2013;27:197–200. [PubMed] [Google Scholar]
- 43.Kowalczyk B, Lejman T. Short-term experience with Ponseti casting and the Achilles tenotomy method for clubfeet treatment in arthrogryposis multiplex congenita. J Child Orthop 2008;2:365–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matar HE, Beirne P, Garg N. The effectiveness of the Ponseti method for treating clubfoot associated with arthrogryposis: up to 8 years follow-up. J Child Orthop 2016;10:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kowalczyk B, Feluś J. Treatment of foot deformities in arthrogryposis multiplex congenita. JBJS Rev 2015;3:01874474-201503060-00004. [DOI] [PubMed] [Google Scholar]
- 46.Turco VJ. Recognition and management of the atypical idiopathic clubfoot Simons GW, ed. The clubfoot: the present and a view of the future. New York, NY: Springer-Verlag, 1994:76–77. [Google Scholar]
- 47.Dragoni M, Gabrielli A, Farsetti P, et al. . Complex iatrogenic clubfoot: is it a real entity? J Pediatr Orthop B 2018;27:428–434. [DOI] [PubMed] [Google Scholar]
- 48.Ford-Powell VA, Barker S, Khan MS, Evans AM, Deitz FR. The Bangladesh clubfoot project: the first 5000 feet. J Pediatr Orthop 2013;33:e40–e44. [DOI] [PubMed] [Google Scholar]
- 49.Perveen R, Evans AM, Ford-Powell V, et al. . The Bangladesh clubfoot project: audit of 2-year outcomes of Ponseti treatment in 400 children. J Pediatr Orthop 2014;34:720–725. [DOI] [PubMed] [Google Scholar]
- 50.van Praag VM, Lysenko M, Harvey B, Yankanah R, Wright JG. Casting Is Effective for Recurrence Following Ponseti Treatment of Clubfoot. J Bone Joint Surg Am. 2018;100(12):1001–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoshioka S, Huisman NJ, Morcuende JA. Peroneal nerve dysfunction in patients with complex clubfeet. Iowa Orthop J 2010;30:24–28. [PMC free article] [PubMed] [Google Scholar]
- 52.Matar HE, Beirne P, Bruce CE, Garg NK. Treatment of complex idiopathic clubfoot using the modified Ponseti method: up to 11 years follow-up. J Pediatr Orthop B 2017;26:137–142. [DOI] [PubMed] [Google Scholar]
- 53.Edmonds EW, Frick SL. The drop toe sign: an indicator of neurologic impairment in congenital clubfoot. Clin Orthop Relat Res 2009;467:1238–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Göksan SB, Bursali A, Bilgili F, Sivacioğlu S, Ayanoğlu S. Ponseti technique for the correction of idiopathic clubfeet presenting up to 1 year of age. A preliminary study in children with untreated or complex deformities. Arch Orthop Trauma Surg 2006;126:15–21. [DOI] [PubMed] [Google Scholar]