Abstract
Purpose
The Salter innominate osteotomy (SIO) in children is traditionally stabilized by Kirschner-wires, which have issues regarding stability, infection and the need to be extracted. To counter these disadvantages, we present a surgical method to stabilize SIO with modern resorbable poly lactic-co-glycolic acid screws. Using a case series of 21 patients treated with SIO for developmental dysplasia of the hip or Legg-Calvé-Perthes disease we evaluate the feasibility of the method.
Methods
The integrity of the osteotomy was interpreted by radiological measurements of acetabular index, centre-edge angle and Reimer’s index. Perioperative and postoperative complications were evaluated.
Results
Radiographic evaluation revealed a stable osteotomy and favourable development in all measured parameters with the exception of one patient who fell out of bed the first day postoperatively. No other perioperative surgical complications were observed and there were no local reactions to the resorbable screws.
Conclusion
Modern resorbable screws carry multiple benefits both for the patient and the surgeon. In our case series the implants provided sufficient stability and the implants caused no local reactions. The use of resorbable implants gave the surgeon a wider range of possible screw placements and avoided the need for implant removal.
Level of evidence
Level IV – Case series
Keywords: hip dysplasia, Legg-Calvé-Perthes disease, osteotomy, absorbable implants
Introduction
In 1961, Salter introduced the innominate osteotomy that has since lent his name.1 This basic surgical method has remained remarkably unaltered over the decades. The Salter innominate osteotomy (SIO) is a feasible option for many cases resistant to nonoperative treatment in both developmental dysplasia of the hip (DDH) and Legg-Calvé-Perthes disease (LCPD) as well as in various other conditions affecting hip development in children.
The SIO entails a transverse osteotomy proximal to the acetabulum with a subsequent mobilization of the distal part of the osteotomy in a lateral and anterior direction to achieve a better coverage for the femoral head. A bone wedge harvested from the iliac crest is used to maintain the achieved correction of the osteotomy. In the original method, the osteotomy is stabilized by metal Kirschner (K)-wires or Steinmann pins. In most cases, a spica cast is applied postoperatively at six to eight weeks and the K-wires are removed under full anaesthesia at the time of cast removal. Fixation using plates or screws have also been described but is rarely used.
The use of K-wires has, however, been associated with relatively frequent complications. Pin migration, including migration into the pelvic cavity, has been reported2-4 and pin-related infections are not uncommon (6.5% reported by Gür and Sarlak).5 Moreover, mechanical pin failure with deformed or broken pins may greatly impair the stability of the osteotomy and present difficulties for pin removal. Repeated anaesthesia, needed for pin removal, may also be harmful for a growing child.6 A modified osteotomy not requiring internal fixation has been suggested7 but the method has not gained popularity, as surgeons probably feel uneasy leaving the osteotomy without fixation.
To overcome these limitations, thin (1.5 mm to 2 mm) resorbable pins for SIO have been used to replace the K-wires and have shown good results in a few studies.8-10 To our knowledge, however, resorbable pins have not gained widespread use. Screws are inherently more stable than pins and K-wires and poly-L-lactide acid (PLLA) screws provide equivalent stability compared to metal screws, at least in in vitro models for periacetabular osteotomies (PAO).11 In adults, PLLA screws have been used for rotational acetabular osteotomies with promising results but a few local reactions have been noted.12-14 Different biodegradable materials do, however, have markedly different traits. Modern poly lactic-co-glycolic acid (PLGA) implants degrade faster than PLLA but still have the desired stability and cause fewer local reactions.15
The main advantage of using resorbable screws is that it eliminates the need for implant removal. This reduces risks associated with general anaesthesia and time spent in hospital, as well as costs. Eliminating the need for removal also enables the surgeon to optimize the placement of the screws in ways that are not possible if an implant needs extraction. Better stability and decreased risk for infection compared with K-wires are additional potential benefits.
The aim of the present study is to present a novel surgical method in a case series of SIO in children using modern resorbable PLGA screws for fixation.
Patients and methods
All patients with DDH or LCPD, who between the years 2011 and 2016 underwent the presented modified SIO performed by one orthopaedic surgeon (TL), were included in this case series (n = 21). Patients with neurological, metabolic or joint-affecting general conditions (n = 3) and patients who had earlier undergone a SIO procedure using K-wires on the same hip (n = 1) were excluded. SIO performed during the same time-period by other surgeons were also excluded (n = 2).
Before 2011 K-wires were used for fixation in all SIOs within the department. In 2011 the department transitioned to the use of resorbable screws, using Activa Screw (Bioretec, Tampere, Finland); a 4.5-mm PLGA polymer screw. The 21 patients included are presented in Table 1.
Table 1.
Patient characteristics. Ages are presented as median range
| All | LCPD | DDH | |
|---|---|---|---|
| Boys, n | 13 | 12 | 1 |
| Girls, n | 8 | 1 | 7 |
| Total, n | 21 | 13 | 8 |
| Age, yrs | 6.6 (3.6 to 11.2) | 7.1 (4.8 to 9.7) | 5.7 (3.6 to 11.2) |
| SIO and simultaneous proximal femur osteotomy, n | 7 | 7 | 0 |
LCPD, Legg-Calvé-Perthes disease; DDH, developmental dysplasia of the hip; SIO, Salter innominate osteotomy
Surgical methods
The surgical procedure was performed in accordance with the original description of the SIO with two exceptions; the site of bone harvesting and the fixation method. Psoas tenotomy was not deemed necessary in the patients included in this study.
Following the assumption that a larger angle between the fixation material and the osteotomy line provides better mechanical stability, the bone graft was harvested in a more vertical direction compared with the original method. Thereby one fixating screw could be placed through the resulting grafting cleft at an angle closer to perpendicularity towards the osteotomy surface. An additional small bone graft was removed from the anterior iliac crest to facilitate closure of the apophysis after the completion of the osteotomy procedure.
After insertion of the bone graft wedge into the redirected osteotomy, the osteotomy was temporarily stabilized with two 1.6-mm K-wires under fluoroscopy. At least one of the K-wires was placed through the bone graft wedge, usually inserted through the cleft from where the bone graft originally was harvested. The second K-wire was inserted through either the outer or the inner aspect of the iliac bone depending on which direction of fixation provided superior support.
After inspecting the position of the K-wires by fluoroscopy, the screw lengths were estimated. The screw channels were drilled and threaded along the K-wires, and thereafter the selected resorbable screws were inserted using the K-wires as guides. Finally, the K-wires were removed and the excessive parts of the resorbable screws were cut with the hot cautery along the bone surface. Figures 1 to 4 demonstrate a case series with pre-, peri- and postoperative radiographs.
Fig. 1.
Preoperative radiograph of five-year-old boy with developmental dysplasia of the hip (patient 20) featuring a steep acetabular index and insufficient coverage of the femoral head.
Fig. 2.
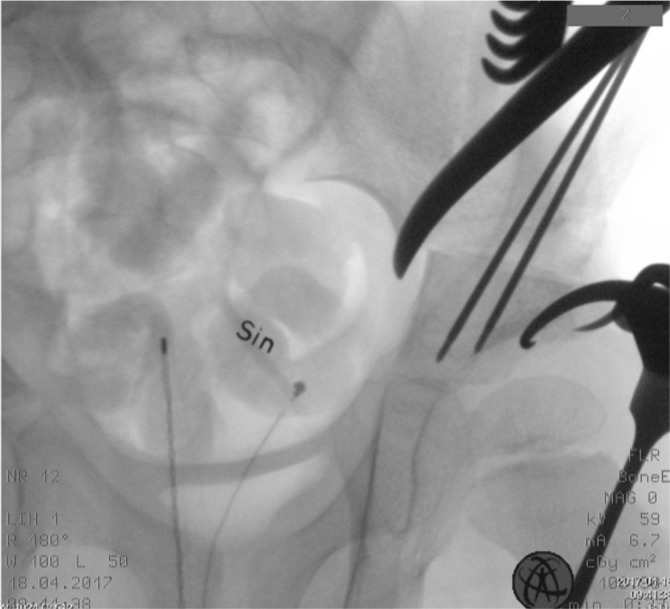
Perioperative fluoroscopy. Note two Kirschner-wires inserted to guide the drill and the bone tap before insertion of the absorbable 4.5-mm Activa Screw. The bone wedge has been harvested from the iliac crest and is subsequently stabilized by both screws.
Fig. 3.

First postoperative radiograph three days postoperatively. The bone wedge is in place and the acetabular coverage and inclination has markedly improved.
Fig. 4.

Radiograph six months postoperative. The acetabular coverage remains improved and the osteotomy has healed.
Most patients (62%) did not receive a postoperative cast immobilization but were instructed to avoid full weight-bearing for six weeks. The remaining patients (38%) who received a cast were immobilized for six weeks before mobilization was initiated. The screw fixation was considered stable enough and therefore a cast was applied only to patients who were expected to benefit from it, such as some patients with LCPD.
Radiographic evaluation
Pelvic radiographs were obtained from the hospital’s picture archive and communication system. The radiograph preceding surgery (0 to four months preoperatively) was used as baseline preoperative radiographs. All postoperative radiographs within 180 days were evaluated. A pelvic osteotomy in a paediatric patient generally shows clear callus formation three to four weeks postoperatively, and 180 days postoperatively was deemed sufficient for a proper evaluation of the short-term radiographic outcome and the integrity of the osteotomy.
The radiographs were evaluated by a senior orthopaedic surgeon (PL) using the AGFA Enterprise Imaging Xero Viewer (AGFA health care, version 8.1.3, Mortsel, Belgium) programme using established methods for assessment of acetabular index (AI), Reimer’s index and centre-edge (CE) angle.16-18 Intraobserver reliability was evaluated by repeated measurements of six of the patients, three weeks after the first measurement and blinded to the earlier results. Also, all radiographs were, at a later stage, evaluated qualitatively to see if any signs of movement in the osteotomy could be detected and to evaluate the presence of callus formation. This was performed by senior radiologists and surgeons in consensus.
The integrity of the osteotomies is graphically presented as well as in a table. Implant failure can be suspected if, for example, a patient’s AI is markedly increased after the first postoperative radiograph.
Data collection of complications
Electronic hospital charts were reviewed for length of hospital stay, surgery time, postoperative complications and clinical result.
Intraobserver reliability
SPSS Statistics (IBM Corp, released 2017. IBM SPSS Statistics for Mac, Version 25.0. Armonk, New York: IBM Corp v25.0.0.0) was used to calculate one-way, absolute agreement average measures intra-class correlation coefficients (ICC). An ICC above 0.8 was considered excellent.19
Results
Clinical results and surgical complications
No perioperative complications or iatrogenic injuries were observed and no screw breakage occurred during insertion. No patients experienced postoperative infection, fistula formation or dermatitis during the healing process. One patient (patient 3) fell out of bed the first day postoperatively and landed on his hip, sustaining a collapse of the osteotomy suggesting implant failure. He was a hyperactive boy, who had not received cast immobilization postoperatively.
The mean operating time (time for surgical intervention) for isolated SIO (n = 14) was one hour 34 minutes (1 hour 13 minutes to 2 hours 0 minutes) which is in line with normal operating time in recent papers using K-wires.20 The mean measured bleeding for isolated SIO cases was 194 ml (50 ml to 400 ml). Patients were discharged from the hospital after on average seven days (4 to 8 days), including the night spent at hospital before surgery.
Radiological results
The relevant parameters for the DDH and LCPD subgroups are presented numerically in Tables 2 and 3 and graphically in Figures 5 and 6.
Table 2.
Pre- and postoperative measurements
| Acetabular index, ° | Reimer’s index, % | CE angle, ° | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | Sex | Diagnosis | Preop | First postop | Second postop | Preop | First postop | Second postop | Preop | First postop | Second postop |
| 1 | M | LCPD | 16.0 | 11.2 | 9.1 | 39.0 | 25.0 | 35.0 | 2.5 | 9.4 | 10.7 |
| 2 | F | DDH | 27.8 | 9.3 | 11.3 | 14.0 | N/A | 0.0 | 16.4 | 37.0 | 37.8 |
| 3 | M | LCPD | 24.0 | 21.8 | 23.2 | 30.0 | 29.0 | 30 | 6.7 | 14.8 | 12.9 |
| 4 | M | LCPD | 12.9 | 3.0 | 6.1 | 34.0 | 17.0 | 16.0 | 15.8 | 24.6 | 27.6 |
| 5 | F | DDH | 24.0 | 16.1 | 17.9 | 23.0 | 9.0 | 17.0 | 16.4 | 25.2 | 20.8 |
| 6 | M | LCPD | 12.5 | 8.5 | 2.9 | 24.0 | 0.0 | 24.0 | 28.0 | 33.6 | 30.8 |
| 7 | M | LCPD | 12.8 | 8.2 | 5.6 | 27.0 | 8.0 | 11.0 | 23.4 | 28.0 | 35.7 |
| 8 | M | LCPD | 12.1 | 4.3 | -3.2 | 32.0 | N/A | 7.0 | 16.9 | N/A | 32.7 |
| 9 | M | LCPD | 14.9 | -1.4 | -8.9 | 14.0 | 0.0 | 10.0 | 18.2 | 38.4 | 36.9 |
| 10 | F | DDH | 26.7 | 10.7 | 7.6 | 18.0 | 0.0 | 0.0 | 19.6 | 31.7 | 38.7 |
| 11 | F | DDH | 26.4 | 20.6 | 13.4 | 40.0 | 18.0 | 24.0 | 10.6 | 19.2 | 20.8 |
| 12 | M | LCPD | 7.6 | -1.20 | -1.4 | 21.0 | 0.0 | 18.0 | 19.8 | 25.7 | 28.9 |
| 13 | M | LCPD | 10.2 | 4.5 | 7.6 | 16.0 | 0.0 | 0.0 | 27.2 | 33.7 | 30.0 |
| 14 | F | DDH | 31.5 | 16.3 | 16.3 | 28.0 | 19.0 | 0.0 | 16.4 | 28.5 | 36.7 |
| 15 | M | LCPD | 27.0 | 17.3 | 15.8 | 36.0 | 22.0 | 19.0 | 10.6 | 16.1 | 22.7 |
| 16 | F | LCPD | 7.1 | 3.8 | 1.0 | 13.0 | 10.0 | 17.0 | 26.7 | 34.0 | 38.0 |
| 17 | M | LCPD | 18.2 | 2.5 | 7.3 | N/A | N/A | 37.0 | 8.7 | 23.6 | 12.8 |
| 18 | F | DDH | 16.2 | -0.4 | 0.5 | 28.0 | 21.0 | 14.0 | 17.0 | 27.8 | 37.3 |
| 19 | M | LCPD | 18.1 | 8.2 | 4.8 | 29.0 | 20.0 | 17.0 | 11.2 | 24.7 | 32.8 |
| 20 | M | DDH | 33.0 | 22.0 | 17.6 | 37.0 | 21.0 | 26.0 | 7.1 | 15.9 | 16.6 |
| 21 | F | DDH | 25.5 | 15.2 | 13.2 | N/A | N/A | 9.0 | N/A | N/A | 23.0 |
First and second postop measurements were performed within one week after surgery and after a minimum of 180 days, respectively. M, male; F, female; CE, centre-edge angle; preop, preoperative; postop, postoperative; LCPD, Legg-Calvé-Perthes disease; DDH, developmental dysplasia of the hip; N/A, suboptimal projections making reliable measurements difficult
Table 3.
Mean measurements for pre- and postoperative radiographs
| DDH | LCPD | ||
|---|---|---|---|
| AI, ° | Preoperative | 26.4 | 14.9 |
| Last postoperative | 12.2 | 5.4 | |
| Change | -14.2 | -9.5 | |
| CE angle, ° | Preoperative | 14.8 | 16.6 |
| Last postoperative | 29.0 | 27.1 | |
| Change | 14.2 | 10.5 | |
| Reimer’s index, % | Preoperative | 26.9 | 26.3 |
| Last postoperative | 11.3 | 18.5 | |
| Change | -15.6 | -7.8 |
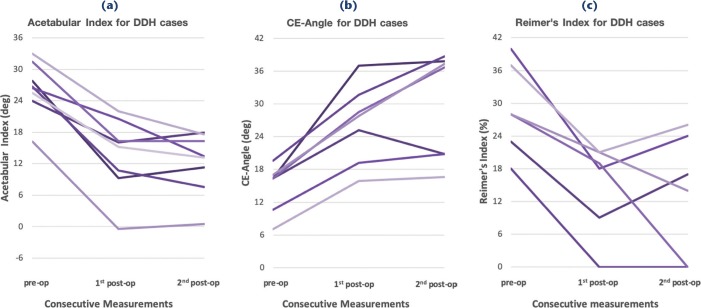
Fig. 5.
Development of longitudinal measurements for the developmental dysplasia of the hip (DDH) group. (a) Showing predictable decline of acetabular index (AI), and (b, c) visualizing predictable increase in centre-edge (CE) angle and a decrease of Reimer’s migration percentage. There are no signs of instability in the osteotomy.
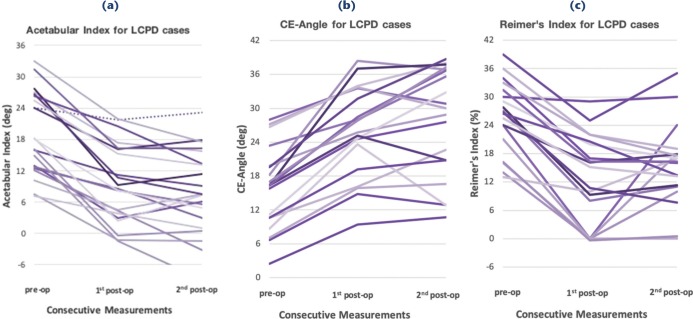
Fig. 6.
Development of longitudinal measurements for the Legg-Calvé-Perthes disease (LCPD) group. In (a) it can be noted that all patients have a predictable decline in acetabular index (AI), except for patient 3 (fall from bed). Patient 3 is marked with a dotted line, and stands out with an increase in acetabular index (AI), postoperatively visualizing a collapse of the osteotomy. There are no signs of instability in the osteotomy with the exception of patient 3. (b, c) The centre-edge (CE) angle and Reimer’s index also exhibit a predictable development with a slightly higher variation which is consistent with the LCPD diagnosis. The collapse of the osteotomy is not as clearly obvious for patient 3 in these parameters.
It can be observed in Figures 5 and 6 that all patients have a stable AI throughout the postoperative period with the exception of patient 3 (marked in Fig. 6a). For all patients, predictable development with minor variations was also noted as evaluated by the CE angle and Reimer’s index in Figures 5b–c and 6b–c. Subjective expert interpretation of the radiographs yielded that all osteotomies (including patient 3) had healed at the time of the last radiograph. Mean measurements are presented in Table 3.
Reproducibility of radiograph measurements
The ICC results, calculated as described above, for AI, Reimer’s index and CE angle were 0.98, 0.96 and 0.99, respectively. These results show excellent intraobserver reliability.
Discussion
We present a novel surgical method to stabilize a SIO with modern resorbable screws with a case series to demonstrate the feasibility of the method and the implant used. Our series of postoperative radiographs verify the integrity of the osteotomy using both quantitative measurements and expert analysis. We thus conclude that the PLGA screws appear to be strong and durable enough to stabilize the osteotomy as well as or better than K-wires. The ability to insert the screws from optimal angles to stabilize the bone wedge and osteotomy, without having to consider implant removal, was greatly appreciated by the surgeon. The additional surgical time needed for screw insertion never exceeded more than a few minutes and presented no technical difficulties. According to our hospital’s economic department the cost of two 4.5-mm Activa Screws is approximately €430 including disposable instruments for insertion while the cost of a minor day-care surgical procedure including anaesthesia and ward time amounts to a minimum of €800. Using resorbable screws and avoiding a second surgery is thus also feasible from a cost-benefit point of view.
The aim of this method was not to present the quality of our SIO per se but rather to demonstrate the feasibility of the method and the stability of the fixation. Nonetheless, the correction achieved by the osteotomy (Tables 2 and 3) is in line with expected results compared with contemporary publications.21,22 The smaller correction seen in the LCPD group can be expected since surgery should be performed at an early stage, before major femoral head deformation or pronounced acetabular dysplasia is seen.
The majority of our SIO patients did not receive a postoperative cast immobilization and the implants were therefore subject to mechanical stress but still remained stable. A pelvic osteotomy subject to a 1-m direct fall on the pelvis will probably lead to implant breakage regardless of the type of implant. Thus, our implant failure in patient 3 rather supported the kind of force needed to break the resorbable screws. Our clinical lesson learned from this patient was to pay better attention to hyperactivity disorders when making decisions on postoperative cast immobilization.
The general stability of the osteotomy presented in this case series is in line with results from Periacetabular osteotomies (PAO) in an adult population using PLLA screws.12,13,23 The paediatric pelvis and SIO as a method are, however, markedly different from an adult pelvis and PAO-osteotomies in many ways. We have found no previous scientific papers on resorbable screws for SIO and our results are thus of potential general interest. The benefits of using resorbable screws in children are more obvious since no hardware needs to be removed and a second anaesthesia and surgery can therefore be avoided. Using resorbable pins is, in our opinion, a less than optimal choice since they probably provide equivalent or even inferior stability as compared to K-wires and with no inherent pull-out strength.
We had no local reactions to the PLGA screws as opposed to a few isolated cases noted by colleagues using PLLA screws for adult pelvic osteotomies13,14,24 nor any radiological signs of osteolysis. This result is in line with the resorption pattern of PLGA screws, which degrade more quickly than PLLA but more slowly than PGA and with few local reactions.25,26 Early generations of polyglycolide (PGA) implants led to initial caution in the use of resorbable screws due to low strength and durability as well as local reactions and sinus formations.27 These difficulties have diminished in later generations of implants using mainly PLLA and PLGA, which degrade slower than PGA.28,29 PLLA implants provide good stability and cause only moderate local reactions but take years to biodegrade and are thus probably less suitable for growing individuals.
Our study has obvious limitations as a retrospective case series of 21 patients with two different diagnoses. As a proof of concept and feasibility we find our results promising enough to warrant continued clinical application and further research. Many factors influence the radiographic measurements of the parameters in question. Tilting of the pelvis or sub-optimal angles of the radiographs can have a significant impact on the measured values. It has been shown that qualified radiologists have adequate but variable agreement on standardized values like the AI.30,31 These factors combined indicate that any given measurement may not be a completely reliable representation of the anatomy of the pelvis even if the ICC in our series is excellent. We do, however, find our series of measurements reliable as the general trend is obvious in descriptive graphs. Minor inconsistencies are likely to represent a suboptimal radiograph or difficulties in measuring due to healing and callus formation.
Conclusion
We present a surgical method on how PLGA screws can be used to stabilize a SIO. In our case series, the implants provided sufficient stability and caused no local reactions. Moreover, the use of resorbable implants gave the surgeon a wider range of possible screw placements and avoided the need for implant removal.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
The study was financed by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement ALFGBG-792231.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was not needed for individual participants included in the study as per advice by the Swedish ethical committee reviewing and approving this retrospective study (Dnr 836-15).
ICMJE Conflict of interest statement
None declared.
Author Contributions
H. Hedelin: Main author of manuscript, study design, data collection and analysis.
P. Larnert: Radiographic analysis, manuscript revision, data analysis, second author.
H. Hebelka: Design of radiographic analysis, radiographic interpretation of study material, manuscript revision.
H. Brisby: Senior advisor on study design and execution, manuscript revision.
K. Lagerstrand: Data analysis and interpretation, design of randomization process for radiographs, manuscript revision.
T. Laine: Research design and results, senior author.
References
- 1.Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Bone Joint J 1961;43-B:518-539. [PubMed] [Google Scholar]
- 2.Aktekin CN, Ozkurt B, Altay M, et al. Unusual Kirschner wire migration as a late complication of Salter innominate osteotomy in developmental dislocation of the hip. Eur J Orthop Surg Traumatol 2008;18:545-548. [Google Scholar]
- 3.Li R Chen B, Wang G, et al. Removal of an intra-abdominal Kirschner wire under digital subtraction angiography: a pediatric case report. J Pediatr Orthop B 2012;21:164-166. [DOI] [PubMed] [Google Scholar]
- 4.Karaman I, Kafadar IH, Oner M, Halici M. Intrapelvic pin migration after Salter innominate osteotomy and laparoscopic removal: a case report. J Pediatr Orthop B 2013;22:533-535. [DOI] [PubMed] [Google Scholar]
- 5.Gür E, Sarlak O. The complications of Salter innominate osteotomy in the treatment of congenital dislocation of hip. Acta Orthop Belg 1990;56:257-261. [PubMed] [Google Scholar]
- 6.Yan J, Li YR Zhang Y, Lu Y, Jiang H. Repeated exposure to anesthetic ketamine can negatively impact neurodevelopment in infants: a prospective preliminary clinical study. J Child Neurol 2014;29:1333-1338. [DOI] [PubMed] [Google Scholar]
- 7.Eren A, Pekmezci M, Demirkiran G, et al. Modified Salter osteotomy for the treatment of developmental dysplasia of the hip: description of a new technique that eliminated the use of pins for internal fixation. J Bone Joint Surg [Br] 2007;89-B:1375-1378. [DOI] [PubMed] [Google Scholar]
- 8.Kremli M. Bioabsorbable rods in Salter’s osteotomy. J Pediatr Orthop B 2002;11:104-109. [DOI] [PubMed] [Google Scholar]
- 9.Xie X, Tang X, Jiang X, Peng M, Liu L. Application of absorbable pins for reconstructing pelvic stability in Salter innominate. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013;27:428-431. (Article in Chinese) [PubMed] [Google Scholar]
- 10.Dawson PH, O’Briain DE, Connolly PJ, McCormack D. Bioabsorbable pins for bone fixation in the less invasive innominate osteotomy. J Pediatr Orthop B 2014;23:426-429. [DOI] [PubMed] [Google Scholar]
- 11.Kashima N, Shiramizu K, Nakamura Y, Moriyama S, Naito M. Biomechanical comparison of the fixation after curved periacetabular osteotomy using titanium and bioabsorbable screws. Hip Int 2015;25:164-167. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura S, Ninomiya S, Takatori Y, et al. Polylactide screws in acetabular osteotomy. 28 dysplastic hips followed for 1 year. Acta Orthop Scand 1993;64:301-302. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura S, Takatori Y, Morimoto S, et al. Rotational acetabular osteotomy using biodegradable internal fixation. Int Orthop 1999;23:148-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasegawa Y, Sakano S, Kawabe K. Ectopic bone formation around the poly-L-lactide screw head in rotational acetabular osteotomy for hip dysplasia. J Orthop Sci 2004;9:551-554. [DOI] [PubMed] [Google Scholar]
- 15.Park S, Kim JH, Kim IH, et al. Evaluation of poly(lactic-co-glycolic acid) plate and screw system for bone fixation. J Craniofac Surg 2013;24:1021-1025. [DOI] [PubMed] [Google Scholar]
- 16.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 1980;184:1-100. [DOI] [PubMed] [Google Scholar]
- 17.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special references to the complication of osteoarthritis. Acta Chir Scand 1939;58. [Google Scholar]
- 18.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res 1976;119:39-47. [PubMed] [Google Scholar]
- 19.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420-428. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura Y, Kimura M, Ohishi H, Kishiya M, Toh S. Salter innominate osteotomy using T-saw for developmental dysplasia of the hip. Curr Orthop Pract 2011;22:447-445. [Google Scholar]
- 21.Kitoh H, Kaneko H, Ishiguro N. Radiographic analysis of movements of the acetabulum and the femoral head after Salter innominate osteotomy. J Pediatr Orthop 2009;29:879-884. [DOI] [PubMed] [Google Scholar]
- 22.Vengust R, Antolic V, Srakar F. Salter osteotomy for treatment of acetabular dysplasia in developmental dysplasia of the hip in patients under 10 years. J Pediatr Orthop B 2001;10:30-36. [PubMed] [Google Scholar]
- 23.Ito H, Minami A, Tanino H, Matsuno T. Fixation with poly-L-lactic acid screws in hip osteotomy: 68 hips followed for 18-46 months. Acta Orthop Scand 2002;73:60-64. [DOI] [PubMed] [Google Scholar]
- 24.Seino D, Fukunishi S, Yoshiya S. Late foreign-body reaction to PLLA screws used for fixation of acetabular osteotomy. J Orthop Trauma 2007;8:188-191. [Google Scholar]
- 25.Middleton JC, Tipton AJ. Synthetic biodegradable polymers as orthopedic devices. Biomaterials 2000;21:2335-2346. [DOI] [PubMed] [Google Scholar]
- 26.Sabir I, Xu X, Li L. A review on biodegradable polymeric materials for bone tissue engineering applications. J Mater Sci 2009;44:5713-5724. [Google Scholar]
- 27.Weiler A, Helling HJ, Kirch U, Zirbes TK, Rehm KE. Foreign-body reaction and the course of osteolysis after polyglycolide implants for fracture fixation: experimental study in sheep. J Bone Joint Surg [Br] 1996;78-B:369-376. [PubMed] [Google Scholar]
- 28.Mukherjee DP, Pietrzak WS. Bioabsorbable fixation: scientific, technical, and clinical concepts. J Craniofac Surg 2011;22:679-689. [DOI] [PubMed] [Google Scholar]
- 29.Zamora R, Jackson A, Seligson D. Correct techniques for the use of bioabsorbable implants in orthopaedic trauma. Curr Orthop Pract 2016;27:469-473. [Google Scholar]
- 30.Broughton NS, Brougham DI, Cole WG, Menelaus MB. Reliability of radiological measurements in the assessment of the child’s hip. J Bone Joint Surg [Br] 1989;71-B:6-8. [DOI] [PubMed] [Google Scholar]
- 31.Omeroglu H, Biçimoglu A, Aguş H, Tümer Y. Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skeletal Radiol 2002;31:25-29. [DOI] [PubMed] [Google Scholar]