Abstract
Everyday discrimination is a potent source of stress for racial minorities, and is associated with a wide range of negative health outcomes, spanning both mental and physical health. Few studies have examined the relationships linking race and discrimination to mortality in later life. We examined the longitudinal association among race, everyday discrimination, and all-cause mortality in 12,081 respondents participating in the Health and Retirement Study. Cox proportional hazards models showed that everyday discrimination, but not race, was positively associated with mortality; depressive symptoms and lifestyle factors partially accounted for the relationship between everyday discrimination and mortality; and race did not moderate the association between everyday discrimination and mortality. These findings contribute to a growing body of evidence on the role that discrimination plays in shaping the life chances, resources, and health of people, and, in particular, minority members, who are continuously exposed to unfair treatment in their everyday lives.
Keywords: everyday discrimination, Health and Retirement Study, epidemiology, health care disparity, mortality, race/ethnicity
Introduction
Racial disparities in health are well-documented, with a broad literature showing racial disparities across a range of outcomes, including heart disease, Type 2 diabetes, physical disability, and stroke (Graham, 2015; Kung, Hoyert, Xu, & Murphy, 2008; Ski, King-Shier, & Thompson, 2014). For several of these conditions, evidence suggests that disparities have either persisted or grown within the past 50 years (Williams & Mohammed, 2009). Many respected scholars argue that the poorer health of non-Hispanic Blacks compared with non-Hispanic Whites (hereafter referred to as Blacks and Whites, respectively) is a function of racism, which is embedded into the structure of the United States, and serves as a vehicle for inequality by shaping opportunities and experiences, including increased exposure to discrimination (Geronimus, 1992; Geronimus, Hicken, Keene, & Bound, 2006; Williams, 1999; Williams, Priest, & Anderson, 2016).
Discrimination, defined as unfair and differential treatment, is a potent source of stress for racial minorities and is consistently associated with a wide range of negative health outcomes, including increased rates of psychological distress, poor self-rated health, breast cancer, cardiovascular disease, physiological dysregulation, and worse well-being (Geronimus et al., 2006; Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009). Repeated exposure to stressors such as everyday discrimination over prolonged periods of time can lead to a dysregulated stress response, which may lead to advanced physiological deterioration at midlife and older ages, thereby contributing to Blacks’ increased risk of morbidity and mortality (Ahmed, Mohammed, & Williams, 2007; McEwen, 1998; Williams & Mohammed, 2009).
The stress process model (Pearlin, 1989; Pearlin, Menaghan, Lieberman, & Mullan, 1981; Turner, 2013) is a helpful framework for hypothesizing about the relationships among race, everyday discrimination, and health. At the heart of the stress process model is the argument that stress exposure and resulting coping responses depend on one’s social status. The inherent connection between social status and stress exposure suggests that stress exposure is more common for lower social status groups (e.g., Blacks) who may also have fewer resources to avert or buffer stress. It is also possible that the negative consequences of stress exposure may be more pronounced for lower social status groups such as Blacks than it is for higher social status groups such as Whites.
Available evidence suggests that Blacks are more likely to experience everyday discrimination than Whites, and despite this continued finding (Barnes et al., 2004; Hatch & Dohrenwend, 2007; Turner & Avison, 2003; Williams, Yu, Jackson, & Anderson, 1997), few studies have sought to examine whether everyday discrimination contributes to racial disparities in health, particularly in midlife and older ages (Sternthal, Slopen, & Williams, 2011; Williams & Mohammed, 2009). Even less is known about the relationships among race, everyday discrimination, and mortality (Ahmed et al., 2007; Williams & Mohammed, 2009).
It is also unclear whether exposure to everyday discrimination has a stronger effect on the mortality risk of Blacks relative to Whites. Some research suggests that Blacks have likely experienced everyday discrimination more intensely and for a longer period of time compared with Whites, and, in turn, may be more susceptible to the negative effects of everyday discrimination through a process called weathering. Coined by Geronimus and colleagues (2006), weathering refers to the earlier onset of physiological wear and tear experienced by Black women compared with White women and suggests that the negative effects of stress may be more pronounced among Blacks than Whites.
Even though consistent evidence links everyday discrimination to negative health outcomes, only three studies to date have examined the association between discrimination and mortality. Barnes and colleagues (2008) found that everyday discrimination was associated with increased risk of all-cause mortality in a racially diverse sample of adults ages 65+, and that the association was stronger for Whites than for Blacks, net of age, gender, race, socioeconomic status (SES), and chronic conditions, suggesting that Whites may be more susceptible to the effects of everyday discrimination. In 2010, Albert and colleagues found that racial/ethnic-based institutional discrimination was not associated with greater mortality risk in the Black Women’s Health Study. Using data from both the Health and Retirement Study (HRS) and the Midlife in the U.S. Study, Sutin, Stephan, and Terracciano (2015) found that everyday discrimination attributed to weight was linked to greater mortality risk. The mixed findings from these studies warrant further investigation into the discrimination–mortality relationship.
Our analyses extend previous research on the association between discrimination and health in three ways. First, we provide new evidence from a nationally representative data source on the relationships among race, everyday discrimination, and all-cause mortality. Second, we include more years of follow-up data and add to the literature on these relationships as they relate to diverse midlife and older adults. Third, we analyze the behavioral and psychological pathways that may mediate the associations tested.
Based on prior work, three overarching aims motivate the current article: (a) to test for a positive association between everyday discrimination and risk of all-cause mortality, (b) to test whether everyday discrimination mediates the relationship between race and risk of all-cause mortality, and (c) to assess whether race moderates the relationship between everyday discrimination and risk of all-cause mortality. Because the current body of research suggests that Blacks at older ages may have extensive experience with everyday discrimination, and developed coping strategies that mitigate the negative health consequences of everyday discrimination (Barnes et al., 2008), additional analyses were conducted to explore whether greater depressive symptoms and lifestyle and health-related factors (e.g., smoking, heavy drinking, vigorous physical activity, body mass index [BMI], chronic conditions) mediated the relationship between everyday discrimination and risk of all-cause mortality. We hypothesized that Blacks would have significantly greater risk of all-cause mortality than Whites; everyday discrimination would be associated with a greater risk of all-cause mortality; and that everyday discrimination would attenuate the relationship between race and risk of all-cause mortality, because of Blacks’ disproportionate exposure to everyday discrimination. Finally, we hypothesized that the association between everyday discrimination and risk of mortality would be stronger among Blacks, relative to Whites, due to weathering. We also hypothesized that more depressive symptoms, risky lifestyle factors, and having more chronic health conditions would account for the relationship between everyday discrimination and risk of all-cause mortality because these are conceptualized as potential pathways linking everyday discrimination to mortality.
Method
HRS
The data from the current study come from respondents participating in the HRS, a nationally representative sample of noninstitutionalized middle-aged and older adults aged 51 and up living in the United States. The HRS began in 1992 and now consists of more than 26,000 respondents. To keep the sample representative, the HRS researchers add new respondents every 6 years. From the start of the HRS, Black and Hispanic populations were oversampled at a 2:1 ratio, but evidence showed that after inclusion of baby boomers, the overall sample sizes for Black and Hispanic populations had declined from sample sizes at 1992, and, thus, from 2010 onward, Black and Hispanic populations were more extensively oversampled (Ofstedal & Weir, 2011). Respondents are interviewed every 2 years and answer questions on sociodemographic, mental and physical health, health-related behaviors, and other information. Beginning in 2006, a rotating random subgroup of 50% of HRS respondents were asked to complete an enhanced face-to-face survey (EFTF), which included a leave-behind questionnaire (Smith et al., 2013). These respondents were then reinterviewed for the EFTF every 4 years. Additional details on the HRS design and administration can be found elsewhere (http://hrsonline.isr.umich.edu).
The leave-behind questionnaire is intended to collect psychosocial data on the respondents, including exposure to everyday discrimination. The 2006 Leave-Behind Questionnaire had a 90% response rate for those who completed the EFTF (Clarke, Fisher, House, Smith, & Weir, 2008). However, after factoring in the response rates of those who completed the core interview for that wave (90%), the overall response rate was 74% (Clarke et al., 2008). The 2008 Leave-Behind Questionnaire had a nearly 89% response rate for those who completed the EFTF (Clarke et al., 2008). However, after factoring in the response rates of those who completed the core interview for that wave (88.4%), the overall response rate was 71% (Clarke et al., 2008).
The current study used a pooled sample of 12,081 respondents who completed either the 2006 or 2008 leave-behind questionnaire and the respective core data to analyze the longitudinal association between race, everyday discrimination, and all-cause mortality by 2014.
Measures
Primary outcome
Waiting time to death
The HRS routinely collects mortality information via reports from the respondent’s proxy in the case of death through an exit interview. In addition, the HRS matches all deaths to the National Death Index. Waiting time to death was measured in months starting from the date when the respondent took the Leave-Behind Questionnaire (either in 2006 or in 2008) and ending, for respondents who subsequently died, at the reported date of death. Respondents who survive until follow-up are treated as censored, and their waiting time ended at the month of their 2014 interview.
Primary predictors
Everyday discrimination
Experiences of everyday discrimination were evaluated using a well-established questionnaire for measuring the frequency with which the respondent reported experiencing different types of interpersonal discrimination (Williams et al., 1997). The psychometrics of this scale were tested in 2006, α = .80, and again in 2008, α = .82 (Smith et al., 2013).
The scale consists of the following five items: (1) You are treated with less courtesy or respect than other people; (2) You receive poorer service than other people at restaurants or stores; (3) People act as if they think you are not smart; (4) People act as if they are afraid of you; and (5) You are threatened or harassed. Responses were coded as: 0 = never, 1 = less than once a year, 2 = a few times a year, 3 = a few times a month, 4 = at least once a week, and 5 = almost every day. The five items are then averaged (range = 0-5, with higher scores suggesting greater frequency of everyday discrimination in the past year). If values of more than three items were missing, then the final score was coded as missing.
Hypothesized mediators at baseline
The first proposed mediator is a measure of depressive symptoms using the eight-item Center for Epidemiological Studies Depression short scale (CESD; range = 0-8; Radloff, 1977). In addition, potential lifestyle-related mediators include a binary indicator of current smoking status (1 = current smoker); a continuous measure of BMI (calculated as weight divided by squared height); current heavy drinking (1 = current heavy drinker), which was defined as >4 drinks per day for men and >3 drinks per day for women, as suggested by the National Institute on Alcohol Abuse and Alcoholism; and a binary indicator for reporting any vigorous physical activity in the past month (1 = reported no vigorous physical activity in the past month).
Physical health conditions at baseline
We also included a count of ever having been told by a doctor that they had any of the following conditions: hypertension, diabetes, arthritis/rheumatism, stroke/transient ischemic attack, heart problems (including heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems), cancer (excluding skin cancer), and lung problems (range = 0-7). Research indicates high reliability of the self-reported measures of physical health conditions in the HRS (Hayward, 2002).
Demographic factors at baseline
Four self-reported key demographic variables were included for the analyses: race (1 = non-Hispanic Black, 0 = non-Hispanic White), age in years (measured continuously), gender (1 = woman), and years of education (range = 0-17, measured continuously).
Analysis
Cox proportional hazard models were estimated to obtain hazard ratios (HRs) for the relationship between the study variables and the risk of death by follow-up in 2014. Graphical and statistical diagnostics suggested that the proportional hazards assumption for age was violated; thus, we stratified on this covariate in all models. For all models, we present the estimated HRs, 95% confidence intervals (CIs), and indications of statistical significance at the level of p < .05. For each variable, an HR less than 1.0 indicates a decreased risk of mortality, and an HR greater than 1.0 indicates an increased risk of mortality.
To test Aim 1, we first estimated a Cox model with the hazard of all-cause mortality regressed on race, gender, and educational attainment. Then, for Aim 2, we estimated a Cox model with the hazard of mortality regressed on everyday discrimination, controlling for race, gender, and educational attainment. Our next model included an interaction term to examine whether race moderated the relationship between everyday discrimination and risk of all-cause mortality. Next, depressive symptoms and lifestyle factors were entered in the equation in two additional models, respectively, to examine the extent to which they mediated the relationship between everyday discrimination and mortality. A final model supplemented the previous specifications by including comorbid health conditions as a robustness check for a potentially confounding factor.
All analyses were weighted to account for the differential probability of being selected into the sample and adjusted for the complex design of the HRS using strata and cluster variables provided by the HRS. All analyses were conducted using Stata, version 14.
Results
Descriptives
The descriptive statistics are displayed in Table 1. In the initial sample of 12,081 respondents, 18.20% of the total sample died by follow-up. The mean age of the sample at baseline was 66.65 ± 9.98 years. At baseline, the sample had a mean everyday discrimination score of 0.67 ± 0.75. As shown, the sample was 9.08% Black and more than half of the sample consisted of women (55.45%). The sample had an average of 13.17 ± 2.64 years of education.
Table 1.
Descriptive Statistics, Total Sample, and Stratified by Race, Health, and Retirement Study.
| Variable | Total sample (n = 12,081) | Black (n = 1,713) | White (n = 10,368) | p value |
|---|---|---|---|---|
| Everyday discrimination (0-5), M (SD) | 0.67 (0.75) | 0.86 (1.12) | 0.65 (0.71) | *** |
| Died (%) | 18.20 | 18.91 | 18.13 | n.s. |
| Age, M (SD) | 66.65 (9.98) | 64.99 (11.55) | 66.82 (9.75) | *** |
| Woman (%) | 55.45 | 60.86 | 54.91 | *** |
| Black (%) | 9.08 | — | — | — |
| Education (0-17), M (SD) | 13.17 (2.64) | 11.94 (3.93) | 13.29 (2.48) | *** |
| Depressive symptoms (0-8), M (SD) | 1.35 (1.89) | 1.82 (2.66) | 1.30 (1.80) | *** |
| Current smoker (%) | 14.22 | 19.78 | 13.66 | *** |
| Heavy drinker (%) | 8.38 | 7.37 | 8.48 | n.s. |
| No vigorous physical activity (%) | 59.47 | 66.57 | 58.76 | *** |
| BMI, M (SD) | 28.29 (5.94) | 30.37 (8.75) | 28.08 (5.62) | *** |
| Chronic conditions (0-7), M (SD) | 1.88 (1.33) | 2.16 (1.71) | 1.86 (1.28) | *** |
Note. BMI = body mass index.
p ≤ .001.
As shown in Table 1, results from descriptive analyses revealed that the sample significantly differed by race on nearly all variables. Black respondents had significantly more exposure to everyday discrimination, 0.86 ± 1.12, compared with White respondents, 0.65 ± 0.71. There were not significant racial differences in those who died by follow-up. The Black respondents were significantly younger at baseline, consisted of a higher proportion of women, and had less education on average than White respondents. Regarding lifestyle characteristics and health status, Blacks had more depressive symptoms, 1.82 ± 2.66, than Whites, 1.30 ± 1.80. In addition, Blacks were more likely to be current smokers and more likely to report no vigorous physical activity in the past month than Whites. Blacks also had significantly higher BMI, 30.37 ± 8.75, than Whites, 28.08 ± 5.62. They also reported more chronic conditions, 2.16 ± 1.71, relative to Whites, 1.86 ± 1.28.
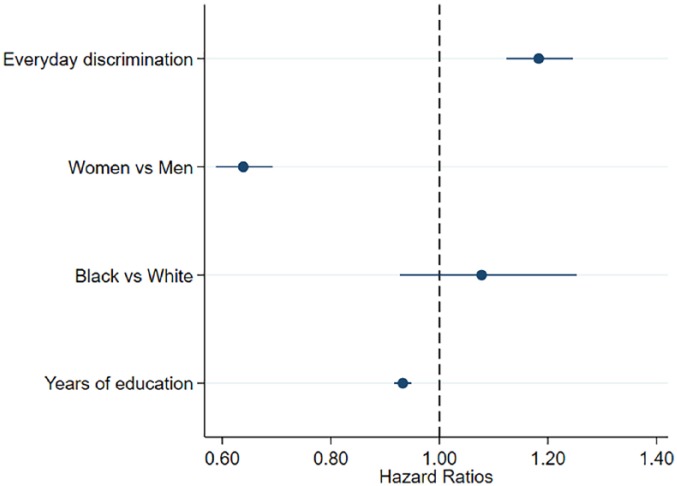
Figure 1 presents the Kaplan–Meier hazard estimates for those by dichotomizing the everyday discrimination score at the scale’s midpoint (2.50). This shows that those with higher everyday discrimination scores were less likely to survive relative to those with lower everyday discrimination scores.
Figure 1.
Kaplan–Meier survival estimates by everyday discrimination (n = 12,081).
Cox Proportional Hazard Regression Results
The results from the Cox proportional hazard regression analyses for Aims 1 to 3 are displayed in Table 2. Model 1 tested the relationship between race and risk of all-cause mortality; Model 2 assessed whether everyday discrimination was associated with the risk of all-cause mortality. Model 3 tested whether race moderated the relationship between everyday discrimination and risk of all-cause mortality. Next, Models 4a and 4b examined the extent to which (a) depressive symptoms and (b) lifestyle factors accounted for the association between everyday discrimination and risk of all-cause mortality. Model 4c was fully adjusted for all lifestyle and health covariates. All models were adjusted for gender, race, education, and stratified by age due to a violation of the assumption of proportionality.
Table 2.
Summary of Hazard Ratios Predicting All-Cause Mortality in the Health and Retirement Study (n = 12,081).
| Race |
Everyday Discrimination |
Race × Everyday Discrimination | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Model 1 | 1.13 | [0.94, 1.34] | ||||
| Model 2 | 1.08 | [0.90, 1.29] | 1.18*** | [1.11, 1.26] | ||
| Model 3 | 1.17 | [0.91, 1.50] | 1.20*** | [1.12, 1.28] | 0.90 | [0.72, 1.14] |
| Model 4a | 1.05 | [0.89, 1.24] | 1.10** | [1.03, 1.17] | ||
| Model 4b | 1.02 | [0.87, 1.20] | 1.08** | [1.02, 1.14] | ||
| Model 4c | 0.99 | [0.84, 1.17] | 1.07* | [1.00, 1.13] | ||
Note. Model 1 tested the association between race and risk of all-cause mortality; Model 2 tested the relationship between everyday discrimination and risk of all-cause mortality; Model 3 tested the Race × Everyday Discrimination interaction on risk of all-cause mortality; Model 4a included depressive symptoms as a potential mediator linking everyday discrimination to risk of all-cause mortality; Model 4b included lifestyle factors as potential mediators; Model 4c included depressive symptoms, lifestyle factors, and chronic health conditions. All models are adjusted for gender, education, and race. They are also stratified by age, because analyses showed that the assumption of proportionality was not met for age. HR = hazard ratio; CI = confidence interval.
p ≤ .05. **p ≤ .01. ***p ≤ .001.
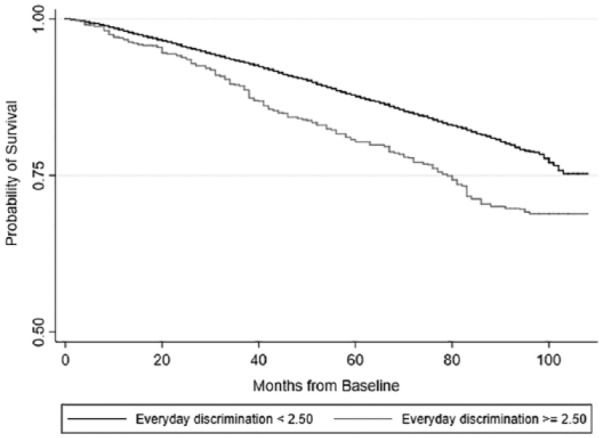
As shown in Model 1 of Table 2, which regressed the risk of all-cause mortality on race, gender, and education, Blacks experienced a higher mortality risk than Whites, but this effect was not statistically significant. Model 2, which adjusted Model 1 for everyday discrimination to assess whether everyday discrimination mediated the relationship between race and all-cause mortality, is presented in Table 2 and Figure 2. This model and corresponding figure show that everyday discrimination was positively associated with risk of all-cause mortality (HR = 1.18, 95% CI = [1.11, 1.26], p ≤ .001), and that the relationship between race and all-cause mortality was attenuated and remained nonsignificant. The analyses suggest that more frequent exposure to everyday discrimination is associated with an increased risk of all-cause mortality.
Figure 2.
Hazard ratios for everyday discrimination and all-cause mortality, adjusted for race, gender, and years of education.
Model 3 tested whether the effect of everyday discrimination on all-cause mortality was stronger for Blacks compared with Whites by including a Race × Everyday Discrimination interaction term to Model 2. The results from this model showed that the Race × Everyday Discrimination interaction effect was not significantly associated with risk of all-cause mortality. This suggests that Blacks are not more susceptible to the adverse effects of discrimination than Whites.
The next set of models (Models 4a-c) examined the extent to which the relationship between everyday discrimination and risk of all-cause mortality was mediated by lifestyle and health characteristics. In particular, Model 4a shows that depressive symptoms at baseline attenuated the association between everyday discrimination and risk of mortality (HR = 1.10, 95% CI = [1.03, 1.17], p ≤ .01). This suggests that the effect of everyday discrimination on all-cause mortality may partially work through increasing depressive symptoms. When baseline measures of heavy drinking, current smoking status, no vigorous physical activity, and BMI were included in Model 4b, the HR for everyday discrimination was reduced to 1.08 (95% CI = [1.02, 1.14], p ≤ .01), net of demographic characteristics. While the association between everyday discrimination and all-cause mortality was attenuated, it remained statistically significant. This suggests that, in addition to increased depressive symptoms, the relationship between everyday discrimination and all-cause mortality may also work through the adoption of negative lifestyle factors (e.g., smoking, heavy drinking) in an effort to offset the resulting stress and depressive symptoms arising from discrimination exposure. Model 4c shows that inclusion of depressive symptoms, lifestyle factors, and chronic health conditions simultaneously attenuated the HR even further toward 1.0 and reduced the association between everyday discrimination and risk of mortality to marginal significance (HR = 1.07, 95% CI = [1.00, 1.13], p ≤ .05).
Discussion
An abundant literature shows that Black–White disparities in health exist for a wide range of health problems. Current projections show that the midlife and older adult population will dramatically increase over the next 50 years, and that along with this growth, this population will also be more diverse than ever (Ortman, Velkoff, & Hogan, 2014). With the rapid growth projected for the midlife and older population in the United States, and particularly because the older population is expected to be more racially diverse, identifying the factors that contribute to older adults’ health may help them age optimally, reduce premature morbidity and mortality, and reduce excess costs to the economy.
A wealth of evidence posits that everyday discrimination—the subjective reporting of day-to-day unfair and differential treatment—is a salient stressor in people’s lives, affecting prevalence of physical and mental health problems, and even dysregulating processes at the physiological level (Williams & Mohammed, 2009). Because racial minorities are disproportionately exposed to discrimination throughout their lives, disentangling whether and how discrimination drives racial disparities in health, particularly in midlife and older populations, is important for both policy and practice. The findings from the present study demonstrated the adverse effects that interpersonal experiences of unfair treatment have on the risk of all-cause mortality in a nationally representative sample of midlife and older adults. A small but increasing body of current work shows that discrimination exposure reduces one’s lifespan as well (Barnes et al., 2008; Williams & Mohammed, 2009). Data from this investigation substantiate prior work linking discrimination to increased risk of mortality.
The results from this article supported the hypothesis for Aim 1, which stated that everyday discrimination would be positively associated with risk of all-cause mortality. This study showed that reporting more frequent everyday discrimination was associated with an increased risk of all-cause mortality, as did Barnes and colleagues (2008). We also found that Blacks reported more frequent exposure to everyday discrimination than Whites did (as shown in Table 1), which suggests that everyday discrimination levies a heavier burden on the aggregate mortality level of Blacks compared with Whites. Much of the available work on discrimination and health shows that frequent exposure to everyday discrimination has negative consequences for health (Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009). First, everyday discrimination exposure directly triggers the hypothalamic–pituitary–adrenal axis (HPA-axis), and, over time, this process becomes dysregulated, ultimately paving the way to poorer health through a number of biological mechanisms such as low-grade inflammation (Glaser & Kiecolt-Glaser, 2005; Jackson, Knight, & Rafferty, 2010; McEwen, 1998; Miller, Cohen, & Ritchey, 2002; Pascoe & Smart Richman, 2009). Next, the results showed that everyday discrimination was likely linked to negative health outcomes due to its influence on mental health, and the coping mechanisms used to buffer the effects of discrimination. For instance, Jackson and colleagues (2010) found that Blacks cope with chronic stress through increased use of unhealthy behaviors (e.g., eating high-fat and high-calorie comfort foods, alcohol use, smoking). While these behaviors work to lessen the psychological effects of chronic stress, they may simultaneously play a role in producing worse physical health outcomes for Blacks.
Next, the findings did not support the hypothesis for Aim 2, which stated that everyday discrimination would mediate the relationship between race and risk of all-cause discrimination. While the estimated racial disparity in mortality was reduced when adjusting for exposure to everyday discrimination, the effect of race on the rate of mortality was not statistically significant in either model. Although discrimination is consistently described as a mechanism driving racial disparities in health, few empirical investigations have tested the extent to which exposure to everyday discrimination accounts for racial disparities (Williams & Mohammed, 2009). The results from this study are inconsistent with work by Sternthal, Slopen, and Williams (2010), who found that increased exposure to stressors (including everyday discrimination) accounted for racial disparities in self-rated health, depressive symptoms, diagnosis of chronic conditions, and functional limitations. The reason for the null finding may be due to higher mortality rates for Blacks at earlier ages (i.e., mortality selection). In a review, Williams and Mohammed (2009) call for more studies to empirically test whether discrimination exposure explains racial disparities in health, because this is an underexplored research area.
The results also did not support the hypothesis for Aim 3. Similar to Barnes et al. (2008), our study found that race did not moderate the everyday discrimination–mortality relationship meaning that everyday discrimination had a similar effect on the risk for mortality for Black and White adults. To more comprehensively understand whether experiences of discrimination make Blacks more vulnerable to risk of mortality than Whites, replicating this study on younger, nationally representative samples is warranted. It is also possible that the attribution of everyday discrimination is more salient for health than the frequency by which everyday discrimination occurs. For instance, a limited area of empirical interest focuses on the role that race-based versus nonrace-based attributions of discrimination matter for health. This area has received mixed support: Some studies find that attribution matters for health (Grollman, 2012, 2014; Van Dyke, Vaccarino, Quyyumi, & Lewis, 2016), whereas others demonstrate that discrimination is associated with poor health regardless of the attribution (Kershaw et al., 2016; Lewis et al., 2006; Mouzon, Taylor, Keith, Nicklett, & Chatters, 2017). This remains a fruitful area for future research.
Finally, while not one of the overarching aims of this article, the present study also sought to examine some of the potential lifestyle and health-related pathways linking everyday discrimination to risk of all-cause mortality. The findings indicated that the association between everyday discrimination and mortality was only partially accounted for by increased depressive symptoms and negative lifestyle factors (i.e., current smoking, no vigorous physical activity in the past month, and higher BMI at baseline). Overall, the results from this study are in line with previous work by Barnes and colleagues (2008), who found the association between discrimination and mortality was partially explained by depressive symptoms. Unlike their study, however, the present study found that lifestyle factors also explained part of the association between everyday discrimination and risk of mortality. Perceptions of discrimination are associated with poorer mental health, such as increased depressive symptoms and anxiety, which may then trigger maladaptive health behaviors in an effort to buffer the negative effects of discrimination-associated stress. However, as a result, unhealthy behaviors may reduce the effect that discrimination has on mental health outcomes (e.g., depression), but their utilization comes at a price—they result in physiological wear and tear, leading to increased rates of morbidity and mortality (Jackson et al., 2010).
Additional research is needed to examine the relationship between discrimination and risk of mortality more comprehensively. These analyses could focus on whether certain attributions for discrimination further increase risk of mortality, and whether attributing discrimination to more than one characteristic (e.g., race, gender, class, and age simultaneously) places individuals, particularly minorities, at an even greater risk of death (Lewis & Van Dyke, 2018). Because the adults in this sample were older, they might be experiencing age-based discrimination for the first time in their lives, along with discrimination on the basis of other characteristics (Barnes et al., 2008). Furthermore, because this sample is older and grew up during a historical time when discrimination was more overt and socially acceptable, there may also be cohort effects in the relationships among race, discrimination, and mortality. Specifically, older Black adults who grew up at different points before, during, and after the Civil Rights movement may have very different perceptions of everyday discrimination, and these differences in perceptions of discrimination may translate to health in unique ways (Barnes et al., 2008; Lewis & Van Dyke, 2018; Versey & Curtin, 2016).
Future research should also focus on examining additional mechanisms responsible for the relationship linking everyday discrimination to mortality because the exact mechanisms have yet to be determined. For example, everyday discrimination may increase depressive symptoms, which then lead to greater participation in negative lifestyle factors (as coping mechanisms) and, in turn, contribute to greater risk of mortality. Special attention to biological mechanisms responsible for these pathways would be useful, as some work suggests that discrimination is associated with allostatic load, an indicator of physiological dysregulation (Brody et al., 2014; Upchurch et al., 2015), and this might be one biological mechanism linking discrimination to mortality.
There are several strengths to the current investigation: First, the sample was drawn from a nationally representative study on midlife and older adults. This allows the results from the study to be generalized to the noninstitutionalized population of adults above 50 years of age residing in the United States. Furthermore, the associations among race, everyday discrimination, and risk of all-cause mortality were captured over a longer follow-up period than prior work. In assessing the relationship between everyday discrimination and all-cause mortality, this work can provide insight into the pervasiveness of everyday discrimination on health by advancing our understanding of how discrimination is related to a clinical end point for all conditions, collectively, because the literature suggests that discrimination exposure is associated with an increased risk of health-relevant outcomes which span mental health, physical health, self-reported health, and health-damaging behaviors.
Despite these strengths and potentially noteworthy findings, this study is not without its limitations. There is some debate on whether the everyday discrimination scale can adequately capture important dimensions of everyday discrimination that may be critically related to whether discrimination adversely affects health, including the stressfulness and severity of the encounters (Krieger, 1999; Williams & Mohammed, 2009). In addition, the study’s results cannot be generalized to adults younger than 51 years of age. The majority of the variables were attained through self-report, including everyday discrimination. Self-reports may be biased due to social desirability and availability and quality of healthcare. Nevertheless, Fisher, Faul, Weir, and Wallace (2005) and Hayward (2002) demonstrate in their review of the literature that self-reported data, such as those in the HRS, are reliable measures. Finally, with any study on racial disparities in health in the midlife and older population, there is the possibility of mortality selection, where those who may have experienced the most frequent everyday discrimination may also consequently be those who died prior to the study.
Findings from this study provide a deeper understanding of the way that racial inequalities in mortality are created. These findings contribute to a growing body of evidence on the role that discrimination plays in shaping the life chances, resources, and health of people, and, in particular, minority members, who are continuously exposed to unfair treatment in their everyday lives. Future work should aim to address the psychosocial, biological, and behavioral mechanisms linking race and everyday discrimination to risk of mortality in diverse samples of midlife and older adults to better address the needs of the increasingly diverse older population.
Footnotes
Authors’ Note: Heather R. Farmer and Jason R. Thomas are now affiliated to Duke University, Durham, USA and Ohio State University, Columbus, USA
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded in part by the National Institute on Aging (NIA) Training Grant (T32-AG000029) for Dr. Farmer.
References
- Ahmed A. T., Mohammed S. A., Williams D. R. (2007). Racial discrimination & health: Pathways & evidence. Indian Journal of Medical Research, 126, 318-327. [PubMed] [Google Scholar]
- Albert M. A., Cozier Y., Ridker P. M., Palmer J. R., Glynn R. J., Rose L., . . . Rosenberg L. (2010). Perceptions of race/ethnic discrimination in relation to mortality among Black women: Results from the Black Women’s Health Study. Archives of Internal Medicine, 170, 896-904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes L. L., De Leon C. F. M., Lewis T. T., Bienias J. L., Wilson R. S., Evans D. A. (2008). Perceived discrimination and mortality in a population-based study of older adults. American Journal of Public Health, 98, 1241-1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes L. L., De Leon C. F. M., Wilson R. S., Bienias J. L., Bennett D. A., Evans D. A. (2004). Racial differences in perceived discrimination in a community population of older blacks and whites. Journal of Aging and Health, 16, 315-337. [DOI] [PubMed] [Google Scholar]
- Brody G. H., Lei M. K., Chae D. H., Yu T., Kogan S. M., Beach S. R. (2014). Perceived discrimination among African American adolescents and allostatic load: A longitudinal analysis with buffering effects. Child Development, 85, 989-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., Fisher G., House J., Smith J., Weir D. (2008). Guide to the content of the HRS psychosocial leave-behind participant lifestyle questionnaires: 2004 & 2006. Ann Arbor: Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Fisher G. G., Faul J. D., Weir D. R., Wallace R. B. (2005). Documentation of chronic disease measures in the Health and Retirement Study (HRS/AHEAD). Ann Arbor: Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Geronimus A. T. (1992). The weathering hypothesis and the relationship of maternal age to birth outcome: Evidence and speculations. Ethnicity & Disease, 2, 207-221. [PubMed] [Google Scholar]
- Geronimus A. T., Hicken M., Keene D., Bound J. (2006). “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health, 96, 826-833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser R., Kiecolt-Glaser J. K. (2005). Stress-induced immune dysfunction: Implications for health. Nature Reviews Immunology, 5, 243-251. [DOI] [PubMed] [Google Scholar]
- Graham G. (2015). Disparities in cardiovascular disease risk in the United States. Current Cardiology Reviews, 11, 238-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grollman E. A. (2012). Multiple forms of perceived discrimination and health among adolescents and young adults. Journal of Health and Social Behavior, 53, 199-214. [DOI] [PubMed] [Google Scholar]
- Grollman E. A. (2014). Multiple disadvantaged statuses and health: The role of multiple forms of discrimination. Journal of Health and Social Behavior, 55, 3-19. [DOI] [PubMed] [Google Scholar]
- Hatch S. L., Dohrenwend B. P. (2007). Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. American Journal of Community Psychology, 40, 313-332. [DOI] [PubMed] [Google Scholar]
- Hayward M. D. (2002). Using the health and retirement survey to investigate health disparities. (Review paper presented for the Data Monitoring Committee). Retrieved from http://hrsonline.isr.umich.edu/sitedocs/dmc/hrs_healthdisparities_hayward.pdf
- Jackson J. S., Knight K. M., Rafferty J. A. (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100, 933-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw K. N., Lewis T. T., Roux A. V. D., Jenny N. S., Liu K., Penedo F. J., Carnethon M. R. (2016). Self-reported experiences of discrimination and inflammation among men and women: The multi-ethnic study of atherosclerosis. Health Psychology, 35, 343-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. (1999). Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services, 29, 295-352. [DOI] [PubMed] [Google Scholar]
- Kung H. C., Hoyert D. L., Xu J., Murphy S. L. (2008). Deaths: Final data for 2005. National Vital Statistics Report, 56(10), 1-120. [PubMed] [Google Scholar]
- Lewis T. T., Everson-Rose S. A., Powell L. H., Matthews K. A., Brown C., Karavolos K., . . . Wesley D. (2006). Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: The SWAN Heart Study. Psychosomatic Medicine, 68, 362-368. [DOI] [PubMed] [Google Scholar]
- Lewis T. T., Van Dyke M. E. (2018). Discrimination and the health of African Americans: The potential importance of intersectionalities. Current Directions in Psychological Science, 27, 176-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B. S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338, 171-179. [DOI] [PubMed] [Google Scholar]
- Miller G. E., Cohen S., Ritchey A. K. (2002). Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid-resistance model. Health Psychology, 21, 531-541. [DOI] [PubMed] [Google Scholar]
- Mouzon D. M., Taylor R. J., Keith V. M., Nicklett E. J., Chatters L. M. (2017). Discrimination and psychiatric disorders among older African Americans. International Journal of Geriatric Psychiatry, 32, 175-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse Alcoholism. Moderate & binge drinking. Retrieved from http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
- Ofstedal M. B., Weir D. R. (2011). Recruitment and retention of minority participants in the health and retirement study. The Gerontologist, 51(suppl_1), S8-S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortman J. M., Velkoff V. A., Hogan H. (2014). An aging nation: The older population in the United States. Washington, DC: U.S. Census Bureau, 25-1140. [Google Scholar]
- Pascoe E. A., Smart Richman L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135, 531-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L. I. (1989). The sociological study of stress. Journal of Health and Social Behavior, 30, 241-256. [PubMed] [Google Scholar]
- Pearlin L. I., Menaghan E. G., Lieberman M. A., Mullan J. T. (1981). The stress process. Journal of Health and Social Behavior, 22, 337-356. [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385-401. [Google Scholar]
- Ski C. F., King-Shier K. M., Thompson D. R. (2014). Gender, socioeconomic and ethnic/racial disparities in cardiovascular disease: A time for change. International Journal of Cardiology, 170, 255-257. [DOI] [PubMed] [Google Scholar]
- Smith J., Fisher G., Ryan L., Clarke P., House J., Weir D. (2013). Psychosocial and lifestyle questionnaire, 2006-2010. Ann Arbor: Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Sternthal M. J., Slopen N., Williams D. R. (2011). Racial disparities in health. Du Bois Review: Social Science Research on Race, 8, 95-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Stephan Y., Terracciano A. (2015). Weight discrimination and risk of mortality. Psychological Science, 26, 1803-1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner R. J. (2013). Understanding health disparities: The relevance of the stress process model. Society and Mental Health, 3, 170-186. [Google Scholar]
- Turner R. J., Avison W. R. (2003). Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior, 44, 488-505. [PubMed] [Google Scholar]
- Upchurch D. M., Stein J., Greendale G. A., Chyu L., Tseng C. H., Huang M. H., . . . Seeman T. (2015). A longitudinal investigation of race, socioeconomic status, and psychosocial mediators of allostatic load in midlife women: Findings from the study of women’s health across the nation. Psychosomatic Medicine, 77, 402-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dyke M. E., Vaccarino V., Quyyumi A. A., Lewis T. T. (2016). Socioeconomic status discrimination is associated with poor sleep in African-Americans, but not Whites. Social Science & Medicine, 153, 141-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Versey H. S., Curtin N. (2016). The differential impact of discrimination on health among Black and White women. Social Science Research, 57, 99-115. [DOI] [PubMed] [Google Scholar]
- Williams D. R. (1999). Race, socioeconomic status, and health: The added effects of racism and discrimination. Annals of the New York Academy of Sciences, 896, 173-188. [DOI] [PubMed] [Google Scholar]
- Williams D. R., Mohammed S. A. (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32, 20-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Priest N., Anderson N. B. (2016). Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology, 35, 407-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Yu Y., Jackson J. S., Anderson N. B. (1997). Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology, 2, 335-351. [DOI] [PubMed] [Google Scholar]