Abstract
Aim: To study the prevalence and cumulative incidence of arrhythmias in the general population of adults aged 60 and older over a 6-year period. Study Design and Setting: Data were taken from the Swedish National Study on Aging and Care (SNAC), a national, longitudinal, multidisciplinary study of the general elderly population (defined as 60 years of age or older). A 12-lead resting electrocardiography (ECG) was performed at baseline and 6-year follow-up. Results: The baseline prevalence of atrial fibrillation (AF) was 4.9% (95% confidence interval [CI] = [4.5%, 5.5%]), and other arrhythmias including ventricular premature complexes (VPCs), supraventricular tachycardia (SVT), and supraventricular extrasystole (SVES) were seen in 8.4% (7.7%, 9.0%) of the population. A first- or second-degree atrioventricular (AV) block was found in 7.1% of the population (95% CI = [6.5%, 7.7%]), and there were no significant differences between men and women in baseline arrhythmia prevalence. The 6-year cumulative incidence of AF was 4.1% (95% CI = [3.5%, 4.9%]), or 6.9/1,000 person-years (py; 95% CI = [5.7, 8.0]). The incidence of AF, other arrhythmias, AV block, and pacemaker-induced rhythm was significantly higher in men in all cohorts except for the oldest. Conclusion: Our data highlight the prevalence and incidence of arrhythmias, which rapidly increase with advancing age in the general population.
Keywords: epidemiology, public health/public policy, cardiovascular diseases and risk, chronic diseases
Background
Population aging is a global issue and related medical costs increase exponentially along with the population (Culebras, Messé, Chaturvedi, Kase, & Gronseth, 2014). Aging affects the cardiovascular system in multiple ways and may cause different arrhythmias (Chow, Marine, & Fleg, 2012). Arrhythmia can lead to a 10% to 20% reduction in cardiac output (Deshmukh, Sharma, & Gobal, 2011), and whereas some patients can be asymptomatic, many experience a wide variety of symptoms, including palpitations, dyspnea, fatigue, dizziness, angina, and congestive heart failure. Arrhythmia can also be associated with hemodynamic dysfunction, tachycardia-induced cardiomyopathy, and systemic embolism such as stroke (Kirchhof et al., 2016). The incidence and prevalence of most cardiovascular disorders (CVDs) increase with age, and cardiovascular disease is the leading cause of death and major disability in adults 75 years of age. Despite the high prevalence, morbidity, and mortality of CVD in older adults, most randomized clinical trials have either explicitly excluded older adults or enrolled only relatively healthy older patients with few comorbidities or functional impairments. As a result, the generalizability of the results of most major clinical trials to older patients, especially those >75 years of age with multimorbidity, is uncertain (Herrera et al., 2010). Existing earlier studies, describing the prevalence of arhythmias, found both supraventricular (24%) and ventricular (49%) complex arrhythmias in a majority of healthy subjects aged 60 to 85 years, and that nearly all these arrhythmias were asymptomatic (Mozaffarian et al., 2016). Arrhythmias, particularly atrial fibrillation (AF), appear to be common in the population (Friberg & Bergfeldt, 2013) and may have important health implications such as stroke (Diener, Easton, Hankey, & Hart, 2013) and syncope (Rafanelli, Brignole, & Kenny, 2017). Older persons aged 75 years have been markedly underrepresented in most major cardiovascular trials, and data from the general older population are lacking. Because interventions such as medical treatment—anticoagulants, for example, can prevent or forestall negative outcomes, it is important to be aware of the prevalence and incidence of arrhythmias in especially the oldest population. We, therefore, in this study, determine the prevalence and incidence of arrhythmias in persons 60 years of age and older.
Method
This study is performed within the ongoing Swedish National Study on Aging and Care (SNAC), as described previously (Lagergren et al., 2004). SNAC is a national, longitudinal, multidisciplinary study conducted at four research centers across Sweden, aiming to describe the aging process from a variety of aspects. The study began in 2001 and has ethical approval from the Regional Ethics Review Boards at the Karolinska Institutet (KI dnr 00-446) and University of Lund (LU dnr 650-00 and LU dnr 744-00), and is conducted in accordance with the Declaration of Helsinki. All SNAC participants gave written informed consent and agreed to the release of their medical records. The characteristics of the total SNAC sample closely reflects the general older population in Sweden and may, therefore, be perceived as representative of the Swedish elderly population. Participants are randomly selected from the National Municipality Registry across nine different age cohorts (aged 60, 66, 72, 78, 81, 84, 87, 90, and 93+ years). Participating individuals are regularly followed, the younger age cohorts (age < 78 years) are followed every 6 years, the older cohort (age 78+ years) are followed every 3 years, and, in addition, new cohorts of 60- and 81-year-old individuals are added to the study population at the 6-year follow-up.
In this study, a total of 8,462 (66.3% of invited) persons participated. Data were collected through physical examinations, patient records, and questionnaires. The majority of the examinations were performed at outpatient clinics in Malmö, Karlskrona, and Kungsholmen in Stockholm and Nordanstig. In all, 1,558 (18.4%) of the 8,462 subjects in baseline were too sick to attend the clinics and were offered examination in their homes or nursing homes. These individuals were excluded from the present study due to the absence of electrocardiography (ECG). Excluded persons per age group was as follows: in Group 60, 66, n = 516; in Group 72, 78, n = 332; in Group 81, 84, 87, n = 404; and in age Group 90+, n = 306 (p = .00; Figure 1).
Figure 1.
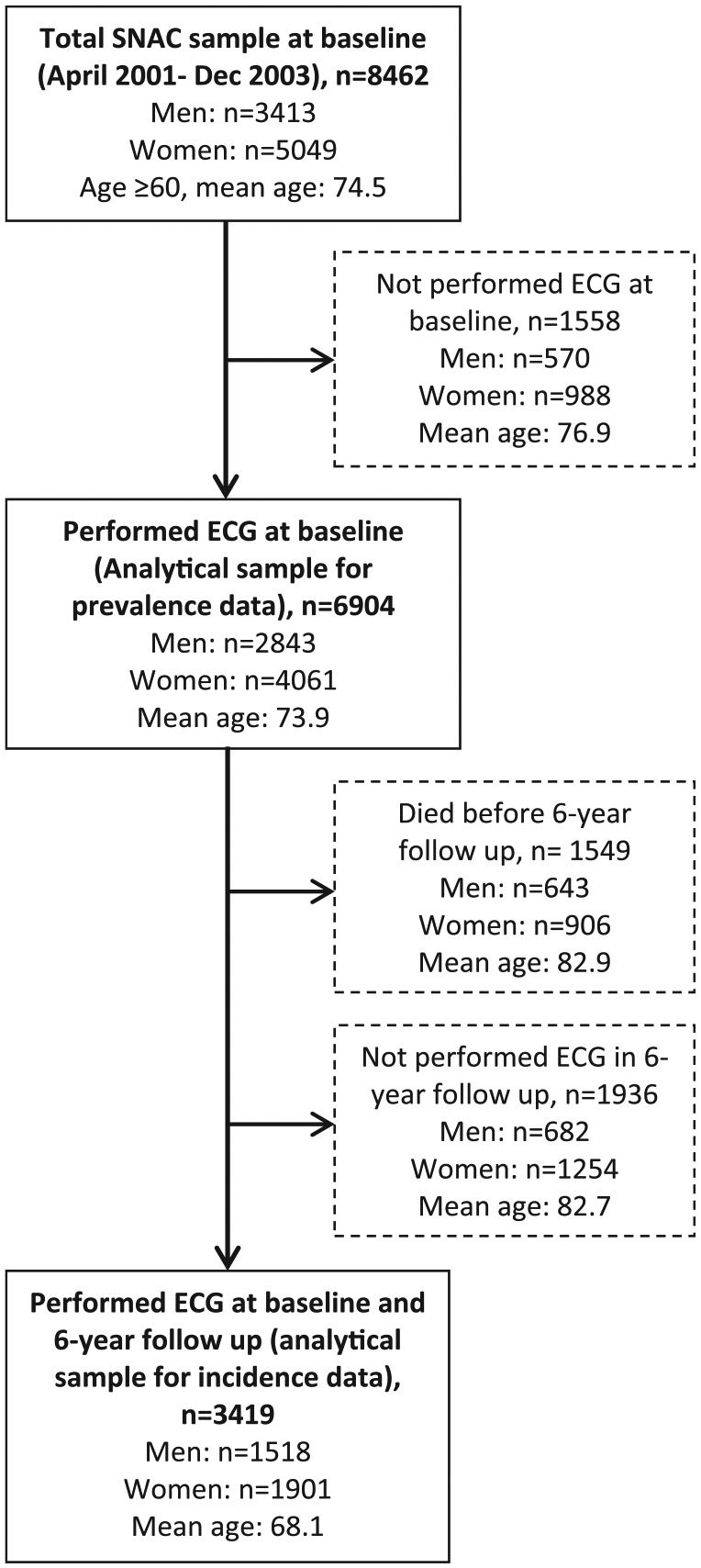
Flowchart of study population.
A resting 12-lead ECG acquired during the physical examination was a requirement for inclusion in the study. Arrhythmia was defined by the ECG examination data based on the Minnesota Code Manual of Electrocardiographic Findings, and the recordings were manually interpreted by different interpreters at the four sites. New cases of arrhythmias were forwarded to specialist health care. Sociodemographic data (age, gender) and relevant medical history (stroke, cardiovascular risk factors, and medication use) were collected during the examinations. ECG findings were categorized as basic heart rhythm (sinus rhythm), AF, pacemaker-induced rhythm, atrioventricular block (AV block), bundle branch block (BB block), and other arrhythmias such as ventricular premature complexes (VPCs), supraventricular tachycardia (SVT), and supraventricular extrasystole (SVES). Follow-up of the death registry was made at 6 years.
Data Analysis
In this study, a total of 8,462 persons participated in the baseline examination, and the prevalence of arrhythmias is based on this group. After 6 years, the same group was examined again, and persons with arrhythmias in baseline were excluded. This gave a sample of 3,419 persons, on which incidence figures are calculated. The data were characterized with descriptive statistics. The age- and sex-specific prevalence of overall and specific arrhythmias was estimated using the baseline examination data, and we estimated arrhythmia incidence by following the cohort of individuals without baseline arrhythmias. A chi-square test was used to test for significant differences between persons with and without arrhythmias by age and gender. Age- and gender-specific incidence was calculated as new cases per 1,000 person-years (py) of follow-up among those with a sinus rhythm at baseline. Data were analyzed using SPSS 23.0 (IBM SPSS Inc., Chicago, IL, USA).
Results
The average age of all 6,904 participants was 73.9 years (SD = 10.7 years) and 4,061 (58.8%) were women. The mean age for women was 75.2 years (SD = 10.9 years, range = 60-105 years) and 72.2 years (SD = 10.1 years, range = 60-101 years) for men. In all, 3,419 of 6,904 subjects aged 66 to 105 years with an ECG examination at baseline (49.6%) completed an ECG at the 6-year follow-up visit. A total of 1,549 (22.4%) subjects died before follow-up examination and 1,936 (28%) did not perform an ECG due to the necessity of home or nursing home visits. The sample was divided into the following four age cohorts to compare the younger and older segments of the population: 60 and 66 years; 72 and 78 years; 81, 84, and 87 years; and >90 years of age at baseline examination. Table 1 summarizes the smoking and medical histories of the participants according to availability of baseline ECG examination and at both baseline and 6-year follow-up.
Table 1.
Smoking and Health History of Study Participants According to Availability of ECG Examination at Baseline and at Both Baseline and Follow-Up Examinations.
| Smoking and medical history | Total sample | ECG examination at baseline | ECG examinations at both baseline and 6-year follow-up | ||||
|---|---|---|---|---|---|---|---|
| (n = 8462) n (%) | No (n = 1,558) n (%) |
Yes (n = 6,904) n (%) |
p | No (n = 3,485) n (%) |
Yes (n = 3,419) n (%) |
p | |
| Current/former smoker | 4,155 (49.1) | 572 (36.7) | 3,507 (50.8) | .050 | 1,575 (45.2) | 1,877 (54.9) | .000 |
| Diabetes | 668 (7.9) | 170 (10.9) | 497 (7.2) | .315 | 335 (9.6) | 205 (6.0) | .008 |
| Stroke/TIA | 711 (8.4) | 245 (15.7) | 4,695 (6.8) | .000 | 390 (11.2) | 154 (4.5) | .000 |
| Vascular disease | 2,902 (34.3) | 673 (43.2) | 2,223 (32.2) | .836 | 1,384 (39.7) | 981 (28.7) | .000 |
| Congestive heart failure | 465 (5.5) | 122 (7.8) | 345 (5.0) | .000 | 275 (7.9) | 68 (2.0) | .000 |
| Hypertension | 2,395 (28.3) | 478 (30.7) | 1,919 (27.8) | .314 | 1,140 (32.7) | 834 (24.4) | .000 |
Note. ECG = electrocardiography; TIA = transient ischemic attack.
Prevalence of Arrhythmias
There was no significant difference between men and women (not age adjusted) regarding sinus rhythm as basic rhythm (p = .154). The prevalence of essential arrhythmias was 4.9% (95% confidence interval [CI] = [4.5, 5.5]) for AF with no significant sex difference (p = .195), and 8.4% (95% CI = [7.7, 9.0]) of the total sample had episodes of other arrhythmias (such as VPC, SVT, and SVES) also with no significant sex difference (p = .597). First- or second-degree AV block was found in 7.1% (95% CI = [6.5, 7.7]) of the population, whereas 1.3% (95% CI = [1.0, 1.6]) had pacemaker-induced rhythm, with no significant difference between men and women (p = .535). In the age group 81, 84, 87 years, the highest proportion of all measured arrhythmias was found (Table 2). In baseline 341 (4.9%) had AF and 152 (44.5 %) received medical treatment (anticoagulants) for their condition, due to earlier diagnoses.
Table 2.
Age- and Gender-Specific Prevalence of Various Arrhythmias Among Old Adults in Sweden.
| Characteristics | Total (n = 6,904) n (%) | Atrial fibrillation n (%) |
AV block n (%) | Other arrhythmias n (%) |
Pacemaker rhythm n (%) |
|---|---|---|---|---|---|
| Total | 6,904 (100) | 341 (4.9) | 488 (7.1) | 579 (8.4) | 88 (1.3) |
| Men | 2,843 (41.2) | 147 (5.2) | 194 (6.8) | 232 (8.2) | 39 (1.4) |
| Women | 4,061 (58.8) | 194 (4.8) | 294 (7.2) | 347 (8.5) | 49 (1.2) |
| Age, years | |||||
| 60, 66 | 2,832 (41.0) | 84 (3.0) | 170 (6.0) | 204 (7.2) | 25 (0.9) |
| Men | 1,345 (47.5) | 35 (2.6) | 67 (5.0) | 92 (6.8) | 11 (0.8) |
| Women | 1,487 (52.5) | 49 (3.3) | 103 (6.9) | 112 (7.5) | 14 (0.6) |
| 72, 78 | 1,695 (24.6) | 94 (5.5) | 122 (7.2) | 159 (9.4) | 20 (1.2) |
| Men | 696 (41.0) | 47 (6.8) | 53 (7.6) | 83 (11.9) | 10 (1.4) |
| Women | 999 (59.0) | 47 (4.7) | 69 (6.9) | 96 (9.6) | 10 (1.0) |
| 81, 84, 87 | 1,687 (24.4) | 124 (7.4) | 140 (8.3) | 172 (10.2) | 31 (1.8) |
| Men | 629 (37.3) | 55 (8.7) | 54 (8.6) | 65 (10.3) | 13 (2.0) |
| Women | 1,058 (62.7) | 69 (6.5) | 86 (8.1) | 107 (10.1) | 18 (1.7) |
| 90+ | 690 (10.0) | 39 (5.7) | 56 (8.1) | 44 (6.4) | 12 (1.7) |
| Men | 173 (25.1) | 15 (8.7) | 20 (11.6) | 12 (6.9) | 5 (2.9) |
| Women | 517 (74.9) | 24 (4.6) | 36 (7.0) | 32 (6.2) | 7 (1.4) |
Note. AV = atrioventricular.
Incidence of Arrhythmias
The 6-year cumulative incidence of AF was 4.1% (95% CI = [3.5, 4.9]), and the overall incidence was 6.9/1,000 py, 9.9/1,000 py for men and 4.4/1,000 py for women. The 6-year cumulative incidence of other arrhythmias was 6.9% (95% CI = [6.2, 7.9]), and the incidence was 11.6/1,000 py in the total sample. Other arrhythmia incidence was significantly higher among men in the total sample (p < .001). AV block was found in 7.3% (95% CI = [6.5, 8.3]), 12.2/1,000 py in the total sample, with a significantly higher incidence for men. Pacemaker rhythm was found in 1.3% of the population (95% CI = [1.0, 1.8]), 2.2/1,000 py, and the incidence was also significantly higher in men (p < .001; Table 3). In the 6-year follow-up, 43.3% of the participants with AF received medical treatment (anticoagulants) for their condition, due to earlier diagnoses.
Table 3.
Six-Year Cumulative Incidence (%) and Incidence Per 1,000 Person-Years (95% CI) of Various Arrhythmias by Age and Sex Among Older Adults in Sweden.
| Total sample, n (%) | Total person-years | AF, n (%) | AF, incidence rate (95% CI) | p * | Other arrhythmias, n (%) | Other arrhythmias, incidence rates (95% CI) | p * | AV block, n (%) | AV block, incidence rate (95% CI) | p * | Pacemaker rhythm, n (%) | Pacemaker, incidence rate (95% CI) | p * | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 3,419 (100) | 20,514 | 142 (4.1) | 6.9 [5.7, 8.0] | 239 (6.9) | 11.6 [10.1, 13.0] | 251 (7.3) | 12.2 [10.7, 13.7] | 46 (1.3) | 2.2 [1.5, 2.8] | ||||
| Men n (%) | 1,518 (44.4) | 9,108 | 91 (5.9) | 9.9 [7.8, 11.9] | .000 | 130 (8.6) | 14 [11.6, 16.4] | .001 | 152 (10) | 16 [13.4, 18.6] | .000 | 26 (1.7) | 2.8 [1.7, 3.9] | .053 |
| Women n (%) | 1,901 (55.6) | 11,406 | 51 (2.7) | 4.4 [3.1, 5.6] | 109 (5.7) | 9.5 [7.7, 11.3] | 99 (5.2) | 8.6 [6.9, 10.3] | 21 (1.1) | 1.8 [1.0, 2.5] | ||||
| Age at baseline | ||||||||||||||
| 60, 66 n (%) | 2,122 (62) | 12,732 | 47 (2.2) | 3.7 [2.6, 4.7] | 106 (4.9) | 8.3 [6.7, 9.8] | 105 (4.9) | 8.2 [6.6, 9.7] | 14 (0.7) | 1.0 [0.45, 1.5] | ||||
| Men n (%) | 984 (46.4) | 5,904 | 35 (3.5) | 5.9 [3.9, 7.9] | .000 | 65 (6.6) | 11 [8.3, 13.6] | .001 | 71 (7.2) | 12 [9.2, 14.7] | .000 | 7 (0.7) | 1.1 [0.25, 1.95] | .600 |
| Women n (%) | 1,138 (53.6) | 6,828 | 12 (1.0) | 1.7 [0.72, 2.6] | 41 (3.6) | 6.0 [4.1, 7.8] | 34 (3.0) | 4.9 [3.2, 6.5] | 7 (0.6) | 1.0 [0.25, 1.75] | ||||
| 72,78 n (%) | 873 (25.5) | 5,238 | 47 (5.3) | 8.9 [6.3, 11.4] | 92 (10.5) | 17.5 [13.9, 21.0] | 88 (10.0) | 16.8 [13.3, 20.2] | 21 (2.4) | 4.0 [2.3,5.7] | ||||
| Men n (%) | 354 (40.5) | 2,124 | 27 (7.6) | 12 [7.4, 16.6] | .013 | 50 (14.1) | 23 [16.6, 29.3] | .004 | 48 (13.5) | 22 [15.7, 28.2] | .003 | 13 (3.7) | 6 [2.7, 9.3] | .013 |
| Women n (%) | 519 (59.5) | 3,114 | 20 (3.8) | 6 [3.3, 8.7] | 42 (8.0) | 13 [9.0, 16.4] | 40 (7.7) | 13 [9.0, 16.4] | 8 (1.5) | 2 [0.43, 3.57] | ||||
| 81,84,87 n (%) | 376 (10.9) | 2,265 | 45 (11.9) | 20 [14.2, 25.7] | 35 (9.3) | 15.4 [10.3, 20.4] | 54 (14.3) | 23.0 [16.8, 24.1] | 10 (2.6) | 4.4 [7.1, 16.7] | ||||
| Men n (%) | 167 (44.4) | 1,002 | 27 (16.1) | 27 [16.9, 37] | .024 | 14 (8.3) | 14 [6.7, 21.3] | .498 | 31 (18.5) | 30 [19.4, 40.5] | .022 | 6 (3.6) | 6 [1.2, 10.8] | .485 |
| Women n (%) | 209 (55.6) | 1,254 | 18 (8.6) | 14 [7.5, 20.5] | 21 (10) | 16 [9, 23] | 23 (11) | 18 [10.6, 25.4] | 4 (1.9) | 3 [0, 6.0] | ||||
| 90+ n (%) | 28 (0.8) | 168 | 3 (10.7) | 18 (0.8, 26.7] | 3 (10.7) | 18 [0.8, 26.7] | 2 (7.1) | 11.9 [5.2, 18.6] | 1 (3.5) | 5.9 [1.1, 10.6] | ||||
| Men n (%) | 5 (17.9) | 30 | 1 (20) | 33 [0, 96.9] | .459 | 0 (0) | 0 (0) | .333 | 1 (20) | 33 [0, 96.9] | .226 | 0 (0) | 0(0) | .671 |
| Women n (%) | 23 (82.2) | 138 | 2 (8.6) | 14 [0, 33.6] | 3 (13) | 21 [0, 44.4] | 1 (4.3) | 7.2 [0, 21.3] | 1 (4.3) | 7.2 [0, 21.3] | ||||
Note. CI = confidence interval; AF = atrial fibrillation; AV = atrioventricular.
p value is for test of sex differences.
Discussion
We assessed the prevalence and incidence of arrhythmias in persons 60 years and older using a large data set from a nationally representative sample of the general population of elderly persons in Sweden. We found an overall prevalence of AF of 4.9% across all included ages detected by a resting ECG. Arrhythmias are very often paroxysmal and, thereby, difficult to detect using a single 12-lead recording. As a consequence, data of these kind will almost exclusively detect permanent arrhythmias. Many arrhythmias, such as AF, AV block, and pacemaker treatment, will be paroxysmal/intermittent. When it comes to AF, paroxysmal type is the most common, making the prevalence noted on a single ECG recording falsely low. AF prevalence was strongly associated with age, and increased in parallel with age from 3% in those aged 60 to 66 years, to 5.5% in those from 72 to 78 years, and to 7.4% in those aged 81, 84, and 87 years. However, the prevalence of AF among the oldest individuals (age 90+) was surprisingly low (5.7%). Survival effects and a selection toward healthier participants in the SNAC study based on the inclusion criteria may have influenced this result. A relatively high prevalence of AF in Sweden compared with other European countries has been reported previously (Zoni-Berisso, Lercari, Carazza, Domenicucci, & others, 2014). This is probably due to the fact that Sweden also has a relatively older population, along with an improved ability to detect and diagnose AF. Previous studies from Sweden have reported prevalence between 2.9% and 3.9%. A study of the general population in Sweden (Friberg & Bergfeldt, 2013) reported a mean prevalence of 2.9%, rising from 0.6% in a <60 years age group to 13.4% in an 80 to 89 years age group, and decreasing to 9.0% in individuals 90 years of age and above. Andersson, Löndahl, Abdon, and Terent (2012) reported a prevalence of 3.9% among the entire population of Northern Hälsingland in Sweden. Both studies were consistent with the results reported here, showing increasing prevalence with age and a relatively low prevalence in the oldest individuals.
The prevalence of AF also increased with age in the Rotterdam study (Heeringa et al., 2006), from 0.7% in the 55 to 59 years age group to 17.8% in those aged 85 years and above. Our reported prevalence was significantly lower in the oldest age group. A review of European studies (Zoni-Berisso et al., 2014), including studies from Iceland, Italy, Germany, England, and Sweden reported that AF prevalence is more than double than reported just one decade earlier. Their prevalence results were similar to those in the present study, at 0.12% to 0.16% for people younger than 49 years, 3.7% to 4.2% for people aged 60 to 70 years, and 10% to 17% for those aged 80 years or older. They also reported a lower age-adjusted AF prevalence and incidence in women than in men in both developed and developing countries (Chugh et al., 2014; SBU, 2013). This is in contrast to our study showing no difference in AF prevalence between men and women across all age cohorts. This result should be taken into account that there were more women than men in the sample, which gives potential bias for sex-specific estimates and that the effect of age is not controlled. A systematic review of 70 studies from developing countries (Nguyen, Hilmer, & Cumming, 2013) showed that prevalence figures range from 0.03% to 1.25% in community-based studies and vary from 0.7% to 55.7% in hospital-based studies. Murakoshi and Aonuma (2013) reported a relatively low prevalence in their review from Asian countries. Another systematic review including 184 studies primarily from Western Europe and North America reports that the prevalence of AF is increasing in both developed and developing countries (Chugh et al., 2014). Other studies estimate that the number of people aged 55 years and above with AF in the European Union will more than double between 2010 and 2060 (Krijthe et al., 2013). The wide range of reported prevalence rates across other studies leads to uncertainty about the actual prevalence in the general population. Differences in earlier prevalence figures may be related to the fact that most published studies are based on data from registers or hospital populations with substantial variation in age and setting, such as inpatient or outpatient cohorts, or developed or developing country. Results regarding AF prevalence in different settings and countries are summarized in Table 4.
Table 4.
Prevalence of AF in Different Settings and Countries: A Summary of Major Literature.
| Author, year, country | Setting | Study population | AF diagnose | Prevalence (%) |
|---|---|---|---|---|
| Andersson, Löndahl, Abdon, & Terent, 2012, Sweden | Medical records/Register Auricula | N = 65,532; age > 35, M age = 74.3; 42.6% women | Resting ECG or Holter | 3.9 |
| Norberg et al., 2013, Sweden | Swedish Patient Register | N = 75,945; age > 30, M age = 77; 43% women | Resting ECG | 3.0 |
| Friberg & Bergfeldt., 2013, Sweden | Swedish Patient Register | N = 7,232,006; age ≥ 20, M age = 75.2; 45% women | AF diagnose resting ECG | 2.9 |
| Heeringa et al., 2006, Rotterdam, The Netherlands | Population-based cohort | N = 6,808; age ≥ 55, M age = 59.5; 59% women | History of AF diagnose or resting ECG | 5.5 |
| Schnabel et al., 2012, Mainz, Germany | Population study | N = 5,000; age = 35-74, M age = 52.2; 50.6% women | History of AF diagnose or resting ECG | 2.5 |
| Wilke et al., 2013, Germany | Insurance register/AF diagnose | N = 8,298,896; all ages, M age = 73.1; 44.5% women | History of AF diagnose | 2.1 |
| Murphy et al., 2007, Glasgow, Scotland/the United Kingdom | General practitioners | N = 362,155; age = 45-75, 49% woman | — | 9.4 |
| Stefansdottir et al., 2011, Iceland | Database with AF diagnose | N = 145,907; age > 20, M age 73 | Resting ECG | 2.0 |
| Cea-Calvo et al., 2007, Spain | Physician list of patients | N = 7,108; age 60-84, M age 71.9; 53.6 % women | History of AF diagnose or resting ECG | 8.5 |
| Bonhorst et al., 2010, Portugal | Population study | N = 10,447; age > 40, M age 58; 55% women | Resting ECG | 2.5 |
Note. AF = atrial fibrillation; ECG = electrocardiography.
There is limited information available on the incidence of arrhythmias in older adults, especially the oldest individuals. One of the first studies to investigate AF incidence was the Framingham study, reporting an overall AF incidence at 2/1,000 py for ages 32 to 65 years (Kannel, Abbott, Savage, & McNamara, 1982). A study of the general population in Scotland reported an AF incidence ranging from 3.8/1,000 for people aged 65 to 74 years to 8.6/1,000 for people aged 85 years and older (Murphy et al., 2007), and the AF incidence reported in a German study was 4.4/1,000 py for men and 3.9/1,000 py for women (Wilke et al., 2013). The Rotterdam study reported an overall incidence of 9.9/1,000 py (Heeringa et al., 2006). Together, the results from these studies are generally in line with our findings; 4.1% of the study population developed AF during the 6 years of follow-up in the present study. The overall AF incidence was 6.9/1,000 py, and there was an increase in the incidence with age, with the exception of those older than 90 years. Similar findings were reported in other studies from both Europe (Heeringa et al., 2006; Murphy et al., 2007) and the United States (Lloyd-Jones et al., 2004), reporting a lifetime risk at age 80 of 22.7% in men and 21.6% in women. Our analysis showed that there was a lower AF incidence compared with the adjacent age group in the >90 years age group. This age group has not typically received separate consideration in the literature. Knowledge of gender differences in common arrhythmias that affect the elderly is important for health care with an aging population (Vallurupalli & Paydak, 2013). Only 44.5% of the participants with AF, in baseline, received medical treatment (anticoagulants) for their condition, due to earlier diagnoses. After 6 years, these numbers had not raised (43.3%) even though treatments for AF reduce the risk of stroke and all-cause mortality. Trials have not assessed whether treatment of screen-detected asymptomatic older adults results in better health outcomes than treatment after detection by usual care or after symptoms develop (Jonas et al., 2018).
Important strengths of the population-based design of this study include the screening of a cross section of older outpatient adults and the inclusion of the oldest individuals. It is reasonable to assume that people with asymptomatic arrhythmias do not typically seek care and are likely to be undiagnosed and undertreated. Screening can identify 1.4% of the population ≥65 years with previously undiagnosed AF. Many of those identified would be eligible for, and benefit from oral anticoagulation (OAC) to prevent stroke. Given this incidence, community AF screening strategies in at-risk older age groups could potentially reduce the overall health burden associated with AF (Lowres, Neubeck, Redfern, & Freedman, 2013). The European Society of Cardiology (ESC) guidelines states,
Diagnosing AF before the first complications occur is a recognized priority for the prevention of strokes and therefore recommend that, in patients aged 65 years or over, opportunistic screening for AF by pulse palpation, followed by recording of an ECG to verify diagnosis, should be considered for the early detection of AF (Kirchhof et al., 2016).
The guidelines highlight the importance of screening programs including ECG recordings or pulse palpation in the general population. Hence, although screening with single time point 12-lead ECG can detect previously unknown cases of AF, it has not been shown to detect more cases than screening focused on pulse palpation (Jonas et al., 2018). The findings in this study contribute to the understanding of the increasing occurrence of arrhythmias in the older population, as well as the high number of untreated cases of arrhythmias posing a challenge for health care. The development of effective strategies for arrhythmia prevention, detection, and treatment is essential. There are also some limitations of the present study. Medical history was self-reported and data of preexisting diagnoses were not available in baseline, which could indicate that some of the health conditions are underreported. In addition, the characteristics of the participants who performed an ECG at the baseline examination and those excluded from the analysis were different. More women than men were excluded due to not performed ECG. This is a potential bias for sex-specific estimates as the results showed no difference in AF prevalence between men and women across all age cohorts. People who were excluded were too sick to attend the clinics and were offered examination in their homes or nursing homes, and it is reasonable to assume that healthier individuals were included in the analysis and, therefore, that the prevalence and incidence of arrhythmias are likely underestimated.
Conclusion
We found that the prevalence and incidence of arrhythmias increase rapidly with advancing age in this population-based study of older adults, in line with studies from both Europe and the United States. The findings contribute to the knowledge regarding increasing arrhythmia occurrence in the older population, and the high number of untreated cases of AF, which pose health care challenges. They also highlight the present lack of knowledge regarding AF in the oldest old population. Technological advancements make it possible to conduct screening and follow-up of patients diagnosed with arrhythmias, and to, thus, facilitate improved health care resource use. There are clearly large benefits of identifying individuals with undiagnosed AF. Such identification would reduce suffering, lower the stroke incidence, and be cost effective for health care.
Acknowledgments
We are grateful to the study participants and the participating counties and municipalities.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: SNAC was supported by grants from the Swedish Ministry of Health and Social Affairs; the county councils of Gävleborg, Stockholm, Blekinge, and Skåne; the municipalities of Nordanstig, Stockholm, Karlskrona, Malmö, Osby, Ystad, and Hässleholm; and Blekinge Institute of Technology.
ORCID iD: Terese Lindberg  https://orcid.org/0000-0003-3166-0274
https://orcid.org/0000-0003-3166-0274
References
- Andersson P., Löndahl M., Abdon N.-J., Terent A. (2012). The prevalence of atrial fibrillation in a geographically well-defined population in Northern Sweden: Implications for anticoagulation prophylaxis. Journal of Internal Medicine, 272, 170-176. [DOI] [PubMed] [Google Scholar]
- Bonhorst D., Mendes M., Adragao P., De Sousa J., Primo J., Leiria E., et al. (2010). Prevalence of atrial fibrillation in the Portuguese population aged 40 and over: the FAMA study. Rev Port Cardiol Orgao Of Soc Port Cardiol Port J Cardiol Off J Port Soc Cardiol, 29:331-350. [PubMed] [Google Scholar]
- Cea-Calvo L., Redón J., Lozano J.V., Fernández-Pérez C., Martí-Canales J.C., Llisterri J.L., et al. (2007). Prevalence of atrial fibrillation in the Spanish population aged 60 years or more. The PREV-ICTUS study. Rev Esp Cardiol, 60(6), 616-624. [DOI] [PubMed] [Google Scholar]
- Chow G. V., Marine J. E., Fleg J. L. (2012). Epidemiology of arrhythmias and conduction disorders in older adults. Clinics in Geriatric Medicine, 28, 539-553. doi: 10.1016/j.cger.2012.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chugh S. S., Havmoeller R., Narayanan K., Singh D., Rienstra M., Benjamin E. J., . . . Murray C. J. (2014). Worldwide epidemiology of atrial fibrillation: A global burden of disease 2010 study. Circulation, 129, 837-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culebras A., Messé S. R., Chaturvedi S., Kase C. S., Gronseth G. (2014). Summary of evidence-based guideline update: Prevention of stroke in nonvalvular atrial fibrillation Report of the Guideline Development Subcommittee of the American Academy of neurology. Neurology, 82, 716-724. doi: 10.1212/WNL.0000000000000145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshmukh A., Sharma S., Gobal F., Singla S., Hebbar P., Paydak H. (2011). Atrial tachyarrhythmias in pulmonary hypertension. Europace, 13 (suppl_3). Retrieved from http://europace.oxfordjournals.org/content/13/suppl_3/NP.10 [Google Scholar]
- Diener H. C., Easton J. D., Hankey G. J., Hart R. G. (2013). Novel oral anticoagulants in secondary prevention of stroke. Best Practice & Research Clinical Haematology, 26, 131-139. [DOI] [PubMed] [Google Scholar]
- Friberg L., Bergfeldt L. (2013). Atrial fibrillation prevalence revisited. Journal of Internal Medicine, 274, 461-468. [DOI] [PubMed] [Google Scholar]
- Heeringa J., van der Kuip D. A., Hofman A., Kors J. A., van Herpen G., Stricker B. H. C., . . . Witteman J. C. (2006). Prevalence, incidence and lifetime risk of atrial fibrillation: The Rotterdam study. European Heart Journal, 27, 949-953. [DOI] [PubMed] [Google Scholar]
- Herrera A. P., Snipes S. A., King D. W., Torres-Vigil I., Goldberg D. S., Weinberg A. D. (2010). Disparate inclusion of older adults in clinical trials: Priorities and opportunities for policy and practice change. American Journal of Public Health, 100(S1), S105-S112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas D. E., Kahwati L. C., Yun J. D. Y., Middleton J. C., Coker-Schwimmer M., Asher G. N. (2018). Screening for atrial fibrillation with electrocardiography: Evidence report and systematic review for the US preventive services task force. Journal of the American Medical Association, 320, 485-498. doi: 10.1001/jama.2018.4190 [DOI] [PubMed] [Google Scholar]
- Kannel W. B., Abbott R. D., Savage D. D., McNamara P. M. (1982). Epidemiologic features of chronic atrial fibrillation: The Framingham study. New England Journal of Medicine, 306, 1018-1022. [DOI] [PubMed] [Google Scholar]
- Kirchhof P., Benussi S., Kotecha D., Ahlsson A., Atar D., Casadei B., . . . Zeppenfeld K. (2016). 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. European Journal of Cardio-Thoracic Surgery, 50, e1-e88. [DOI] [PubMed] [Google Scholar]
- Krijthe B. P., Kunst A., Benjamin E. J., Lip G. Y., Franco O. H., Hofman A., . . . Heeringa J. (2013). Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. European Heart Journal, 34, 2746-2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagergren M., Fratiglioni L., Hallberg I. R., Berglund J., Elmståhl S., Hagberg B. others. (2004). A longitudinal study integrating population, care and social services data. The Swedish National Study on Aging and Care (SNAC). Aging Clinical and Experimental Research, 16, 158-168. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D. M., Wang T. J., Leip E. P., Larson M. G., Levy D., Vasan R. S., . . . Benjamin E. J. (2004). Lifetime risk for development of atrial fibrillation the Framingham heart study. Circulation, 110, 1042-1046. [DOI] [PubMed] [Google Scholar]
- Lowres N., Neubeck L., Redfern J., Freedman S. B. (2013). Screening to identify unknown atrial fibrillation. Thrombosis and Haemostasis, 110, 213-222. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D., Benjamin E. J., Go A. S., Arnett D. K., Blaha M. J., Cushman M., . . . Fullerton H. J. (2016). Heart disease and stroke statistics-2016 update: A report from the American Heart Association. Circulation, 133(4), e38-e48. [DOI] [PubMed] [Google Scholar]
- Murakoshi N., Aonuma K. (2013). Epidemiology of arrhythmias and sudden cardiac death in Asia. Circulation Journal, 77, 2419-2431. [DOI] [PubMed] [Google Scholar]
- Murphy N. F., Simpson C. R., Jhund P. S., Stewart S., Kirkpatrick M., Chalmers J., . . . McMurray J. J. V. (2007). A national survey of the prevalence, incidence, primary care burden and treatment of atrial fibrillation in Scotland. Heart, 93, 606-612. doi: 10.1136/hrt.2006.107573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T. N., Hilmer S. N., Cumming R. G. (2013). Review of epidemiology and management of atrial fibrillation in developing countries. International Journal of Cardiology, 167, 2412-2420. [DOI] [PubMed] [Google Scholar]
- Norberg J., Bäckström S., Jansson J-H., Johansson L. (2013). Estimating the prevalence of atrial fibrillation in a general population using validated electronic health data. Clin Epidemiol, 5, 475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafanelli M., Brignole M., Kenny R. A. (2017). Syncope and unexplained falls in the elderly. In Ungar A., Marchionni N. (Eds.), Cardiac management in the frail elderly patient and the oldest old (pp. 71-86). Cham: Springer. doi: 10.1007/978-3-319-43468-1_7 [DOI] [Google Scholar]
- SBU. Swedish Agency for Health Technology Assessment and Assessment of Social Services. (2013). Förmaksflimmer—förekomst och risk för stroke (Atrial fibrillation—The occurrence and risk of stroke). Stockholm: Swedish Agency for Health Technology Assessment and Assessment of Social Services-Statens beredning för medicinsk och social utvärdering. [Google Scholar]
- Schnabel R.B., Wilde S., Wild P.S., Munzel T., Blankenberg S. (2012). Atrial fibrillation: its prevalence and risk factor profile in the German general population. Dtsch Ärztebl Int, 109:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefansdottir H., Aspelund T., Gudnason V., Arnar D.O. (2011). Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. Europace, 13:1110–1111. [DOI] [PubMed] [Google Scholar]
- Vallurupalli S., Paydak H. (2013). Gender differences in cardiac arrhythmias in the elderly. Current Cardiovascular Risk Reports, 7, 485-489. [Google Scholar]
- Wilke T., Groth A., Mueller S., Pfannkuche M., Verheyen F., Linder R., . . . Breithardt G. (2013). Incidence and prevalence of atrial fibrillation: An analysis based on 8.3 million patients. Europace, 15, 486-493. [DOI] [PubMed] [Google Scholar]
- Zoni-Berisso M., Lercari F., Carazza T., Domenicucci S. (2014). Epidemiology of atrial fibrillation: European perspective. Clinical Epidemiology, 6, 213-220. [DOI] [PMC free article] [PubMed] [Google Scholar]


