Abstract
Background
Familial hypercholesterolemia (FH) can lead to premature coronary heart disease. Anticardiolipin antibody may be a contributor for thrombosis. Here, we report an adult with possible FH suffered from premature myocardial infarction that may be triggered by transient increased anticardiolipin antibody.
Case presentation
A 29-year-old male had presented with a history of 2-h chest pain and numbness of left upper arm before 5 days. The electrocardiogram (ECG) had demonstrated inferior wall myocardial infarction (MI). Five days later he was admitted to our hospital and diagnosed as acute MI and possible FH (premature coronary heart disease, low density lipoprotein cholesterol of 5.90 mmol/L) with increased anticardiolipin antibody (up to 120 RU/ml). Other auto-antibodies including β2-glicoprotein antibodies IgM, IgA, IgG, lupus anticoagulant (LA), antinuclear antibodies, anti-myocardial antibody were normal. Coronary artery angiography (CAG) showed right coronary artery was total occlusion from the middle segment. Then he underwent percutaneous coronary intervention with a stent. Four days later, he was discharged with complete recovery. CAG showed intra-stent restenosis and anticardiolipin antibody level was normal and the patient had no any symptoms at 6-month follow-up.
Conclusions
Transient elevated anticardiolipin antibody may be a trigger or biomarker of cardiac thrombotic events in younger atherosclerotic patients.
Keywords: Familial hypercholesterolemia, Thrombosis, Myocardial infarction, Anticardiolipin antibody
Background
It is well known that the incidence of premature cardiovascular disease (CVD) is low. Previous studies have revealed that patients aged less than 40 years old only account for 1.2% of all patients with MI [1, 2]. Numerous studies have reported that multiple risk factors relate to ST segment elevated MI (STEMI) including male, smoking state, family history of CVD, dyslipidemia, hypertension, and diabetes mellitus (DM) in patients aged < 40 years [3–7]. Familial hypercholesterolemia (FH) as a type of dyslipidemia is one of the most common risk factors in patients with premature atherosclerotic cardiovascular disease (ASCVD) [8, 9]. In addition, previous evidence has proved that the presence of antiphospholipid antibodies (aPL) increases the thrombotic risk and the decreased titers or the disappearance of aPL closely relates to better prognosis [10–13]. Thus, a transient increase of anticardiolipin antibody induced by bacteria or viruses infection may contribute to the risk of thrombosis in patient with possible FH [14, 15].
Case presentation
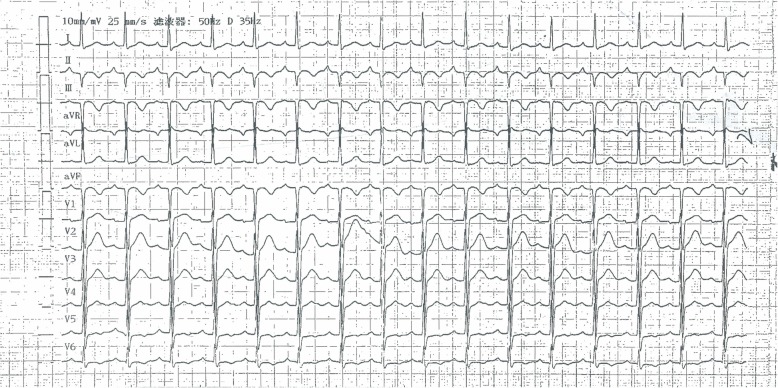
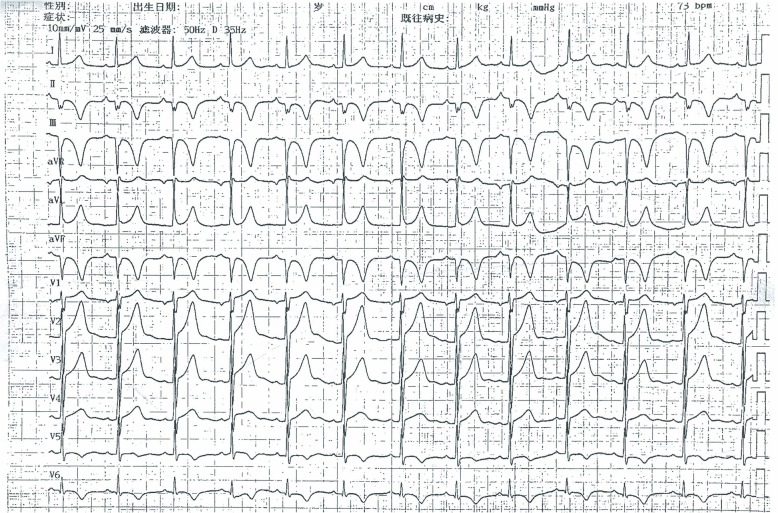
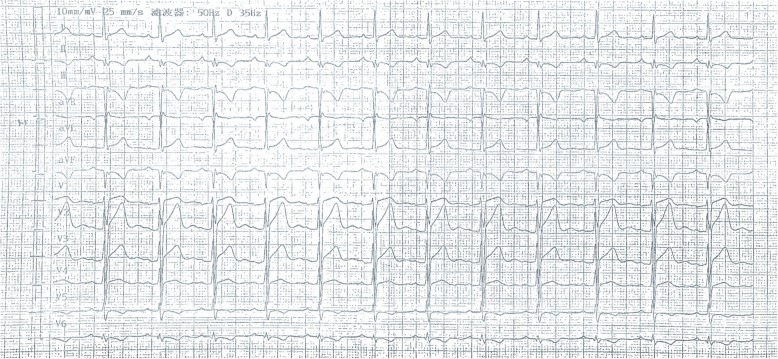
A 29-year-old male patient had presented with a history of 2-h chest pain and numbness of left upper arm before 5 days. The electrocardiogram (ECG) indicated acute inferior wall myocardial infarction (MI) and he refused any treatment at that time. Five days later he was admitted to our hospital for further examination. Physical examination showed no abnormal including arcus corneae and xanthelasma in eyelid, extensor tendon and achilles tendons. He had no histories of diabetes mellitus, hyperthyroidism, heart disease, hepatic or renal disease and no family history of FH. The ECG showed deep Q wave and inverted T wave in leads II, III and aVF (Fig. 1) and the echocardiogram revealed the diastolic dysfunction of left ventricular with a decreased LV ejection fraction (EF, 48%). The lower extremities ultrasound revealed atherosclerotic plaque in the posterior wall of right common femoral artery. Blood tests showed CK-MB of 21.4 U/L, lactate dehydrogenase of 452 U/L, hs-CRP of 71.2 ng/L, triglyceride (TG) (Triglyceride Kit method) of 0.88 mmol/L, total cholesterol (TC) of 6.87 mmol/L (Cholesterol Kitmethod), low density lipoprotein cholesterol (LDL-C) of 5.90 mmol/L and high density lipoprotein cholesterol (HDL-C) of 1.09 mmol/L (Direct Method-Surfactant Clearance Method).Further laboratory tests revealed highly elevated anticardiolipin antibody (ELISA method) of more than 120RU/ml (0-12RU/ml) and no other abnormal auto-antibodies, including β2-glicoprotein antibodies IgM, IgA, IgG, lupus anticoagulant (LA). DNA analysis for antiphospholipid antibody syndrome (APS) was not performed. Coronary artery angiography (CAG) demonstrated predominant right coronary artery (RCA) and diffuse lesions in the middle and distal segments of the left anterior descending (LAD) artery with the stenosis up to 40~50% (Fig. 2a) and total occlusive RCA from the middle segment (Fig. 2b) with LAD-RCA collateral circulation. With the treatments of anticoagulation (heparin), double antiplatelets (aspirin and ticagrelor) and lipid-modulating (rosuvastatin), he was implanted a stent at the middle segment of the RCA (Fig. 2c). Four days later, he was discharged without any complication. The ECG at discharge showed that the inverted T waves were deeper than those at admission in leads II, III and aVF (Fig. 3). At 6-month follow-up, the laboratory test showed the level of anticardiolipin antibody (ELISA method) was less than 2.0 RU/ml (0-12RU/ml). Lipid profile revealed TG of 0.98 mmol/L, TC of 6.22 mmol/L, LDL-C of 5.53 mmol/L and HDL-C of 0.99 mmol/L.CAG showed 70% in-stent restenosis of the RCA. ECG revealed deep Q waves and inverted T waves (Fig. 4). The patient looked good without any activity restriction and discomfort. At 8-month follow-up, the level of anticardiolipin antibody is less than 2.0 RU/ml and the lipid profile showed TG 0.64 mmol/L, TC 4.15 mmol/L, LDL-C 3.47 mmol/L and HDL-C 1.01 mmol/L.
Fig. 1.
Electrocardiogram at admission
Fig. 2.
Coronary artery angiography and percutaneous coronary intervention (PCI). a. Left anterior descending artery (LAD); b. Right coronary artery (RCA); c. Implantation of stent in the middle right coronary artery
Fig. 3.
Electrocardiogram at discharge
Fig. 4.
Electrocardiogram at 6-month follow-up
Discussion and conclusions
FH is a risk factor for premature ASCVD [16, 17] and antiphospholipid antibody is a contributor of thrombosis for myocardial infarction [14, 18]. According to the Dutch Lipid Clinic Network (DLCN) Diagnostic criteria (DLCN) [19], the patient was confirmed as possible FH with 5 scores including the premature coronary heart disease (2 points) and LDL-C level of 5.90 mmol/L (3 points). With the International Consensus Statement for Definite APS [20], we could not give a definite diagnosis of APS for this patient. However, the antiphospholipid antibodies can be present in the common population with bacterial or viral infection including HIV, HBV, HCV, herpes virus and parvovirus B19 [15, 21]. Infection-related antibodies will totally disappear once the infection is gone [22]. Although this patient did not have an obvious infectious manifestation before his admission, some occult infections could not be completely excluded. Therefore, transient elevation of anticardiolipin antibody could be a trigger or biomarker for MI in patients with FH [14, 18]; however, the causative effects of transient increased anticardiolipin antibody and MI still need further study.
Limitations
We did not perform the genetic testing about the APS and the test of anticardiolipin antibody at 12-week follow-up.
Acknowledgements
Not Applicable.
Abbreviations
- AMI
Acute myocardial infarction
- aPL
Antiphospholipid antibody
- APS
Antiphospholipid antibody syndrome
- ASCVD
Atherosclerotic cardiovascular disease
- CAD
Coronary artery disease
- CK-MB
Creatine kinase isoenzyme
- ECG
Electrocardiograph
- FH
Familial hypercholesterolemia
- HDL-C
High-density lipoprotein cholesterol
- hs-CRP
High-sensitivity C-reactive protein
- LDL-C
Low-density lipoprotein cholesterol
- LDLR
LDL receptor
- TC
Total cholesterol
- TG
Triglyceride
Authors’ contributions
XS, AQW were involved in the patient management and manuscript writing. HZ, HLS, YCD and SLW collected information and collated pictures of the patient. MZ and YH focused on error correction. XZ and YSC performed interventional therapy for the case and revised the manuscript attentively. All the authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81460072) and CAS “Light of West China” Program where the publication fees are from.
Availability of data and materials
All the data in this study are included in the manuscript.
Ethics approval and consent to participate
The study is approved by Ethics committee of Gansu Provincial Hospital.
Consent for publication
We have obtained written informed consent from the patient for the publication.
Competing interests
The authors have no any conflicts of interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xin Su, Email: sxin2017@126.com.
Aqian Wang, Email: aqianwang2@126.com.
Hai Zhu, Email: cardiozhuhai@sina.com.
Hongling Su, Email: 384011782@qq.com.
Yichao Duan, Email: 1947714830@qq.com.
Shanlian Wu, Email: 13679491692@163.com.
Min Zhang, Email: sallyzhangmin@126.com.
Yan Huang, Email: huangyanden@163.com.
Xing Zhou, Email: xingzhoulzu@163.com.
Yunshan Cao, Email: yunshancao@126.com.
References
- 1.Trzeciak P, Gierlotka M, Gasior M, Osadnik T, Hawranek M, Lekston A, Zembala M, Polonski L. In-hospital and 12-month outcomes after acute coronary syndrome treatment in patients aged<40 years of age (from the polish registry of acute coronary syndromes) Am J Cardiol. 2014;114(2):175–180. doi: 10.1016/j.amjcard.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Puricel S, Lehner C, Oberhansli M, Rutz T, Togni M, Stadelmann M, Moschovitis A, Meier B, Wenaweser P, Windecker S, et al. Acute coronary syndrome in patients younger than 30 years--aetiologies, baseline characteristics and long-term clinical outcome. Swiss Med Wkly. 2013;143:w13816. doi: 10.4414/smw.2013.13816. [DOI] [PubMed] [Google Scholar]
- 3.Yunyun W, Tong L, Yingwu L, Bojiang L, Yu W, Xiaomin H, Xin L, Wenjin P, Li J. Analysis of risk factors of ST-segment elevation myocardial infarction in young patients. BMC Cardiovasc Disord. 2014;14:179. doi: 10.1186/1471-2261-14-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hosseini SK, Soleimani A, Karimi AA, Sadeghian S, Darabian S, Abbasi SH, Ahmadi SH, Zoroufian A, Mahmoodian M, Abbasi A. Clinical features, management and in-hospital outcome of ST elevation myocardial infarction (STEMI) in young adults under 40 years of age. Monaldi archives for chest disease = Archivio Monaldi per le malattie del torace. 2009;72(2):71–76. doi: 10.4081/monaldi.2009.331. [DOI] [PubMed] [Google Scholar]
- 5.Prajapati J, Joshi H, Sahoo S, Virpariya K, Parmar M, Shah K: AGE-Related Differences of Novel Atherosclerotic Risk Factors and Angiographic Profile Among Gujarati Acute Coronary Syndrome Patients. Journal of clinical and diagnostic research : JCDR 2015, 9(6):Oc05–09. [DOI] [PMC free article] [PubMed]
- 6.Migliaresi P, Celentano A, Palmieri V, Pezzullo S, Martino S, Bonito M, Guillaro B, Brancati C, Di Minno G. Knowledge of cardiovascular risk factors and awareness of non-pharmacological approach for risk prevention in young survivors of acute myocardial infarction. The cardiovascular risk prevention project "help your heart stay young". Nutrition, metabolism, and cardiovascular diseases : NMCD. 2007;17(6):468–472. doi: 10.1016/j.numecd.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Callachan EL, Alsheikh-Ali AA, Wallis LA. Analysis of risk factors, presentation, and in-hospital events of very young patients presenting with ST-elevation myocardial infarction. J Saudi Heart Assoc. 2017;29(4):270–275. doi: 10.1016/j.jsha.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vallejo-Vaz AJ, Kondapally Seshasai SR, Cole D, Hovingh GK, Kastelein JJ, Mata P, Raal FJ, Santos RD, Soran H, Watts GF, et al. Familial hypercholesterolaemia: A global call to arms. Atherosclerosis. 2015;243(1):257–259. doi: 10.1016/j.atherosclerosis.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Pang J, Poulter EB, Bell DA, Bates TR, Jefferson VL, Hillis GS, Schultz CJ, Watts GF. Frequency of familial hypercholesterolemia in patients with early-onset coronary artery disease admitted to a coronary care unit. Journal of clinical lipidology. 2015;9(5):703–708. doi: 10.1016/j.jacl.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Salazar-Paramo M, Jara LJ, Ramos A, Barile L, Machado G. Garcia-De La Torre I: longitudinal study of antinuclear and anticardiolipin antibodies in pregnant women with systemic lupus erythematosus and antiphospholipid syndrome. Rheumatol Int. 2002;22(4):142–147. doi: 10.1007/s00296-002-0207-x. [DOI] [PubMed] [Google Scholar]
- 11.Turiel M, Sarzi-Puttini P, Peretti R, Rossi E, Atzeni F, Parsons W, Doria A. Thrombotic risk factors in primary antiphospholipid syndrome: a 5-year prospective study. Stroke. 2005;36(7):1490–1494. doi: 10.1161/01.STR.0000170645.40562.09. [DOI] [PubMed] [Google Scholar]
- 12.Ruffatti A, Del Ross T, Ciprian M, Bertero MT, Sciascia S, Scarpato S, Montecucco C, Rossi S, Caramaschi P, Biasi D, et al. Risk factors for a first thrombotic event in antiphospholipid antibody carriers: a prospective multicentre follow-up study. Ann Rheum Dis. 2011;70(6):1083–1086. doi: 10.1136/ard.2010.142042. [DOI] [PubMed] [Google Scholar]
- 13.Reynaud Q, Lega JC, Mismetti P, Chapelle C, Wahl D, Cathebras P, Laporte S. Risk of venous and arterial thrombosis according to type of antiphospholipid antibodies in adults without systemic lupus erythematosus: a systematic review and meta-analysis. Autoimmun Rev. 2014;13(6):595–608. doi: 10.1016/j.autrev.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Schreiber K, Sciascia S, de Groot PG, Devreese K, Jacobsen S, Ruiz-Irastorza G, Salmon JE, Shoenfeld Y, Shovman O, Hunt BJ. Antiphospholipid syndrome. Nature reviews Disease primers. 2018;4:18005. doi: 10.1038/nrdp.2018.5. [DOI] [PubMed] [Google Scholar]
- 15.Cruz-Tapias P, Blank M, Anaya JM, Shoenfeld Y. Infections and vaccines in the etiology of antiphospholipid syndrome. Curr Opin Rheumatol. 2012;24(4):389–393. doi: 10.1097/BOR.0b013e32835448b8. [DOI] [PubMed] [Google Scholar]
- 16.Li S, Zhang Y, Zhu CG, Guo YL, Wu NQ, Gao Y, Qing P, Li XL, Sun J, Liu G, et al. Identification of familial hypercholesterolemia in patients with myocardial infarction: a Chinese cohort study. Journal of clinical lipidology. 2016;10(6):1344–1352. doi: 10.1016/j.jacl.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 17.Risk of fatal coronary heart disease in familial hypercholesterolaemia. Scientific Steering Committee on behalf of the Simon Broome Register Group. BMJ (Clinical research ed) 1991, 303(6807):893–896. [DOI] [PMC free article] [PubMed]
- 18.Zuckerman E, Toubi E, Shiran A, Sabo E, Shmuel Z, Golan TD, Abinader E, Yeshurun D. Anticardiolipin antibodies and acute myocardial infarction in non-systemic lupus erythmatosus patients: a controlled prospective study. Am J Med. 1996;101(4):381–386. doi: 10.1016/S0002-9343(96)00226-4. [DOI] [PubMed] [Google Scholar]
- 19.Defesche JC, Lansberg PJ, Umans-Eckenhausen MA, Kastelein JJ. Advanced method for the identification of patients with inherited hypercholesterolemia. Seminars in vascular medicine. 2004;4(1):59–65. doi: 10.1055/s-2004-822987. [DOI] [PubMed] [Google Scholar]
- 20.MIYAKIS S., LOCKSHIN M. D., ATSUMI T., BRANCH D. W., BREY R. L., CERVERA R., DERKSEN R. H. W. M., DE GROOT P. G., KOIKE T., MERONI P. L., REBER G., SHOENFELD Y., TINCANI A., VLACHOYIANNOPOULOS P. G., KRILIS S. A. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS) Journal of Thrombosis and Haemostasis. 2006;4(2):295–306. doi: 10.1111/j.1538-7836.2006.01753.x. [DOI] [PubMed] [Google Scholar]
- 21.Sene D, Piette JC. Cacoub P: [antiphospholipid antibodies, antiphospholipid syndrome and viral infections] La Revue de medecine interne. 2009;30(2):135–141. doi: 10.1016/j.revmed.2008.05.020. [DOI] [PubMed] [Google Scholar]
- 22.Lieby P, Soley A, Knapp AM, Cerutti M, Freyssinet JM, Pasquali JL, Martin T. Memory B cells producing somatically mutated antiphospholipid antibodies are present in healthy individuals. Blood. 2003;102(7):2459–2465. doi: 10.1182/blood-2003-01-0180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data in this study are included in the manuscript.