ABSTRACT
In the period from January 2013 to July 2014, three process change initiatives were undertaken at a major UK hospital to improve the patient discharge process. These initiatives were inspired by the findings of a study of the discharge process using Soft Systems Methodology. The first initiative simplified time-consuming paperwork and the second introduced more regular reviews of patient progress through daily multi-disciplinary “Situation Reports”. These two initiatives were undertaken in parallel across the hospital, and for the average patient they jointly led to a 41% reduction between a patient being declared medically stable and their being discharged from the hospital. The third initiative implemented more proactive alerting of Social Care Practitioners to patients with probable social care needs at the front door, and simplified capture of important patient information (using a “SPRING” form). This initiative saw a 20% reduction in total length of stay for 88 patients on three wards where the SPRING form was used, whilst 248 patients on five control wards saw no significant change in total length of stay in the same period. Taken together, these initiatives have reduced total length of stay by 67% from 55.8 days to 18.6 days for the patients studied.
KEYWORDS: Patient discharge process, complex needs, Health Needs Assessment, Soft Systems Methodology
1. Introduction
The process of discharging patients from acute hospitals is characterised by a range of patient circumstances and needs. Discharge planning for older patients is particularly challenging (Bauer et al., 2009; Mitchell, Gilmour, & Mclaren, 2010; Victor, Healy, Thomas, & Seargeant, 2000), as these patients often have a broad range of needs relating to their health and any care that is needed to support them in their own homes or in community care homes. Previous studies have found discharge processes to be inefficient for such patients (Connelly et al., 2009; National Audit Office, 2003). This paper describes the effects of three process change initiatives that were implemented at a major acute hospital in 2013–2014 in an attempt to improve the discharge process.
The paper makes the following three contributions. Firstly, the paper shows that removing the requirement to complete Health Needs Assessments as part of the discharge process and implementing daily Sit Reps on all wards significantly reduces delays. Secondly, it shows that more proactive planning for discharge (commencing on a patient’s arrival to the hospital) and better sharing of information can significantly reduce the total length of stay. Thirdly, the interventions implemented in this study were based on a previous study using Soft Systems Methodology (SSM). As such, this paper serves as a case study supporting the usefulness of SSM in a health care context.
The remainder of this paper is organised as follows. The next section explains the relevant background literature including how systems thinking has been applied in the health sector and the previous attempts to understand and improve the discharge process. This is followed by a case study, including a description of the methods employed – a summary of the systems thinking study and the subsequent interventions implemented. We next present the results obtained from the interventions, before discussing the implications of these in the context of the objectives and the findings of previous literature, and finally offer our conclusions.
2. Background literature
2.1. Systems thinking for health
Advocates of systems thinking have long been promoting its value for the design of interventions in the healthcare sector (Checkland & Scholes, 1990; Patching, D, 1990). There is now also growing recognition amongst healthcare practitioners that a systems approach is necessary to deliver effective health and social care services for a growing, and ageing population (Department of Health, 2003).
Reports to help recognise and promote systems thinking in the health sector have been published by professional bodies, such as the Royal Academy of Engineering (2017) and think tanks, such as the King’s Fund (Welbourn, Warwick, Carnall, & Fathers, 2012). There is also now evidence of the recognition of systems thinking within NHS England. For example, the requirement to introduce “place-based plans” for future health and care services, delivered through “Strategic Transformation Partnerships”, is an attempt to improve the performance of the system as a whole by encouraging more integrated working across organisations (NHS England, 2015).
In a system, the whole is recognised to be more than the sum of its parts, as interactions between the elements of a system lead to emergence – “properties, capabilities, and behaviours evident in the whole system that are not exclusively ascribable to any of its parts” (Hitchins, 2003). For a complex organisation or endeavour, whole system performance cannot be optimised simply by splitting the system into parts and optimising the parts (Kauffman, 1980). For large, “complicated” projects, such as developing new aircraft, the techniques of operational research and hard systems engineering are relevant, helping to solve the objective functions in a way that maximises performance; systems thinking pervades modern techniques in logistics (Forrester, 1958) and manufacturing (Deming, 1982; Ohno, 1988). Lean thinking (Womack, Jones, & Roos, 1990) has become increasingly popular in this context with its preoccupation with efficient use of resources and the reduction of waste.
Adapting Deming’s work on quality management, Seddon (2005) and Seddon and Caulkin (2007) merge aspects of lean with more explicit aspects of systems thinking, proposing a “Check, Plan, Do” cycle for systems thinking. Here, the first stage (“Check”) involves understanding the organisation as a system, the second stage (“Plan”) identifies levers for effective change, and the third stage (“Do”) implements direct action on the system. Since it is a cycle, the process is never complete. Some applications of this approach to the public sector in Wales are described in a report by the Lean Enterprise Research Centre (Zokaei et al., 2010).
Public sector problems and the projects undertaken to address them are often “complex”, however, with diverse stakeholders that disagree on the nature of the requirements (and also on how best to address them). The application of systems thinking here goes beyond efficiency and the reduction of waste, and focuses instead on effectiveness – delivering enduring performance improvements to the system’s stakeholders. With ambiguous requirements, problem structuring methods, such as SSM (Checkland, 1981; Checkland & Poulter, 2006; Checkland & Scholes, 1990; Wilson, 2001; Wilson & van Haperen K, 2015) are necessary to ensure that any interventions made are built upon a foundation of a clear understanding of the problem situation (Checkland, 1981).
SSM is a “systems-based methodology for tackling real-world problems in which known-to-be-desirable ends cannot be taken as given” Checkland (1981: 318). SSM studies commence with a situation that is considered problematic. Various interpretations of the situation are then sought from relevant stakeholders to try to understand the factors contributing to the problem, and the context within which any potential improvements must reside. The action of the stakeholders in the problem space can be understood by seeing them as part of “purposeful activity systems” with corresponding philosophies or “worldviews” governing their behaviour. These purposeful activity systems form the basis of conceptual models, which through comparison with the real world are used to identify possible improvements. SSM crucially consists of both analysis in the real world and systems thinking about the real world (Wilson & van Haperen K, 2015).
Measures of performance or performance criteria for SSM (Table 1) are an important part of exploring purposeful activity models (Kotiadis et al., 2013). Studies typically involve discussions of efficacy, efficiency and effectiveness (Checkland, 1981; Checkland & Scholes, 1990), and are sometimes extended to include ethicality and elegance (Kotiadis et al., 2013).
Table 1.
SSM measures of performance (Kotiadis et al., 2013).
| Measure | Description |
|---|---|
| Efficacy | The extent to which the transformation (as described in the conceptual model) is producing the outputs expected |
| Efficiency | The extent to which the output of the transformation process is obtained with minimum use of resources |
| Effectiveness | The extent to which the transformation meets the longer-term goals as outlined in the worldview |
| Ethicality | The extent to which the transformation process is morally correct |
| Elegance | The extent to which the transformation is aesthetically pleasing |
A more extensive review of the literature on the application of SSM in the health sector is described by Emes, Smith, Ward, Smith, and Ming (2017).
3. Discharge planning
Discharging patients from acute hospitals is known to be challenging (Department of Health, 2003, 2010; National Audit Office, 2003; National Health Service and Community Care Act, 1990), especially in the context of limited resources and an ageing population (Oliver, Foot, & Humphries, 2014). Many options have been considered for improving the financing and delivery of healthcare (Thomson, Foubister, & Mossialos, 2009). These include methods targeted at improving efficiency, such as reducing duplication, avoiding errors, changing the balance of services between acute hospitals and community care, simplifying administration, and introducing uniform standards (Hurley et al., 2009; Miani et al., 2014). Length of stay is often used as a measure of hospital efficiency (OECD (2012) Health at a Glance, 2012), and reducing the length of stay is thought to improve both operational efficiency (eg, reducing waste) and allocative efficiency (making sure the care is provided in the most appropriate setting) (Miani et al., 2014). Average length of stay has consistently fallen across European Union member states from around 8 days in 2000 to around 7 days in 2010 (OECD (2012) Health at a Glance, 2012). In a similar period, mean length of stay in acute hospitals in England fell steadily from 8 days in 2002–3 to around 5 days in 2011–12. Older patients (aged 75 years and above), however, stayed on average around twice this long, with their mean length of stay falling from 16 days to 10 days in this period (Miani et al., 2014), or to 12 days in 2014–15 according to another study based on emergency admissions only (National Audit Office, 2016). A range of measures has been investigated to reduce length of stay for older patients, such as comprehensive or structured discharge planning (Parker, 2005; Shepperd et al., 2003) and comprehensive geriatric assessment (Ellis, Whitehead, Robinson, O’neill, & Langhorne, 2011). Miani et al.’s (2014) study into organisational interventions to reduce length of stay found two primary studies investigating geriatric interdisciplinary care with explicit length of stay data reported. The first of these conducted by Deschodt et al. (2011) in Belgium, for patients aged 65 and over that had suffered traumatic hip fracture, found a mean length of stay of around 55 days for patients transferred to a geriatric or rehabilitation unit. The second study by Harari, Martin, Buttery, O’neill, and Hopper (2007), for a population of 95 patients (46 before intervention, 49 after) aged 70 and over with a broad range of needs, reported a mean length of stay of 18 days (SD = 27.2) including long-stay outliers. Following the introduction of a screening intervention – a comprehensive geriatric assessment – this fell to a mean of 11.4 days (SD = 12.3).
Particularly for patients with complex needs, effective communication is a key enabler of the discharge process: “hospital discharge planning for frail older people can be improved if interventions address family inclusion and education, communication between health care workers and family, interdisciplinary communication and ongoing support after discharge” (Bauer et al., 2009: 2539). The term “complex needs” has been interpreted in many different ways, but we follow Maramba, Richards, and Larrabee (2004) definition, seeing them as “multiple inter-connected needs that span medical and social issues”. Although complex needs are often associated with older patients, not all elderly patients have complex needs. Complex needs often have both breadth and depth, and have emergent properties where the whole is more than the sum of the parts (Rankin & Regan, 2004: 7). Effective discharges are necessarily multi-disciplinary efforts and many interventions should commence well before discharge. Nevertheless, forward planning is sometimes lacking (Bauer et al., 2009). This is particularly problematic for patients who might be medically ready to leave hospital quite soon after admission, since this compresses the time available for practitioners to understand a patient’s needs and develop an appropriate discharge plan (Cummings, 1999; Cummings & Cockerham, 1997; Maramba et al., 2004; Payne, Kerr, Hawker, Hardey, & Powell, 2002). Achieving timely access to post-acute care services such as care homes is particularly challenging, as these are in high demand and have limited capacity (Katsaliaki, Brailsford, Browning, & Knight, 2005). The extent to which discharge planning should be individualised has been reviewed in various studies (Shepperd et al., 2003; Gonçalves-Bradley et al., 2016. These report overall a relatively modest benefit, concluding that “a structured discharge plan tailored to the individual probably brings about a small reduction in hospital length of stay and unscheduled readmission for elderly patients with a medical condition” (Gonçalves-Bradley et al., 2016: 18).
Ten steps to achieve safe and timely discharge from acute hospitals are identified by the UK Department of Health (2010). These steps can be grouped into three broad themes as in Table 2 (Emes et al., 2017). Although many previous studies have targeted a reduction in length of stay, few have applied systems thinking to investigate discharge planning to this end (Department of Health, 2003; Kotiadis, Tako, & Vasilakis, 2014; Mukotekwa & Carson, 2007).
Table 2.
Summary of UK Department Of Health Guidance (Emes et al., 2017).
| Theme | Description |
|---|---|
| Proactivity | Planning for discharge should start on or before admission, and practitioners should identify early those patients with complex needs. A clinical management plan should be developed for each patient within 24 h of admission, with an expected date of discharge within 24–48 h of admission. |
| Effective communication | Discharge should be coordinated through effective leadership and handover of responsibilities, with the clinical management plan reviewed with the patient and carers each day. |
| Keeping the process moving | Decisions to discharge should be made each day, with discharges planned to take place over seven days and a checklist used 24–48 h before discharge to make sure everything’s in place. Although simple checklists may be useful, it is also recognised by some studies that much of the paperwork for discharge planning is overly complex. This not only delays discharge but also reduces the sense of professionalism of staff (Connelly et al., 2009). |
4. Case study
4.1. Background
The focus of this study (“the hospital”) is a leading general hospital in the UK National Health Service (NHS) and a specialist tertiary centre for cancer, oral and maxillo-facial surgery and pathology. It serves a population of over 300,000 for emergency and general hospital services, and is the lead specialist centre for cancer patients for the wider region serving a population of over one million. The hospital became a foundation trust in 2009, and as such is accountable to its local community. It has over 500 beds, 14 operating theatres and employs around 3,000 staff.
In 2012, two of the authors were working in the hospital, and wanted to investigate whether systems thinking could be applied to help improve the process of discharging patients with complex needs. They made contact with the remaining authors to form a cross-disciplinary team covering social care, occupational therapy and systems engineering to investigate this question as part of a lean green belt initiative supported by Patients First (a major transformation programme established in May 2008 to use tools, such as lean and Six Sigma to deliver improved patient care). A Discharge Hub had been set up in the hospital in June 2012 to improve communication between Social Care Practitioners, Physiotherapists, Occupational Therapists and Discharge Coordinators. By co-locating these functions in a Discharge Hub, it was believed that inter-disciplinary discussions and paperwork, such as “Health Needs Assessments” (HNAs) could be completed more easily. The research described here was undertaken in the context of trying to make the most of this facility to improve the discharge process.
In the hospital, major delays were associated with (a) the completion of paperwork (in particular HNAs) used to assess the needs of the patients post discharge, and (b) finding beds in community hospitals post discharge. Before the start of the project, it was known that, across the hospital as a whole, referral to social care took an average of 8.5 days from a patient’s admission. Furthermore, there was limited capture of shared information from social care, therapy and community health perspectives and limited information provided – either to ward staff (if the patient were admitted), or to community health and social care services (if the person were discharged).
The HNA form is used to record information needed to understand the level of support (medical or social) that the patient is likely to need on discharge from hospital. The process for completing these forms at the hospital was for a Social Care Practitioner to issue an HNA to the relevant ward for each patient that was expected to require ongoing support on discharge. HNAs would be completed mainly by Doctors, but some sections were completed by Nurses, Social Care Practitioners, Occupational Therapists and Physiotherapists. The completed HNAs would then be returned to the social care team to inform the process of finding appropriate post-discharge support services. Since these were paper-based not electronic forms, their completion was a sequential task. Their completion was often not prioritised by Doctors, who saw direct patient contact as their primary concern (Emes et al., 2017). Since the databases containing information on patient admission and discharge dates were not integrated with the social care database used for tracking HNAs, gathering data on length of stay for patients that received HNAs was a manual task.
In the period June 2012 to January 2013, the mean time taken to complete HNAs in the hospital was 12.7 days (standard deviation (SD) = 7.5) for the population of 93 patients – all patients that had HNAs issued within the period). Since the hospital’s management team had set a target of three days for completion of HNAs, this was recognised as a major source of delay. The distribution of times taken for HNAs to be processed at the start of the project is shown in Figure 1. The mean time between an HNA being issued (corresponding with the time that a patient becomes medically stable) and discharge was 47.8 days (SD = 26.1) for the 54 patients that were discharged in the period. Average time between admission and issuing of an HNA was known to be 8 days, giving a mean length of stay for this sample at the start of the project of 55.8 days (SD = 27.3).
Figure 1.
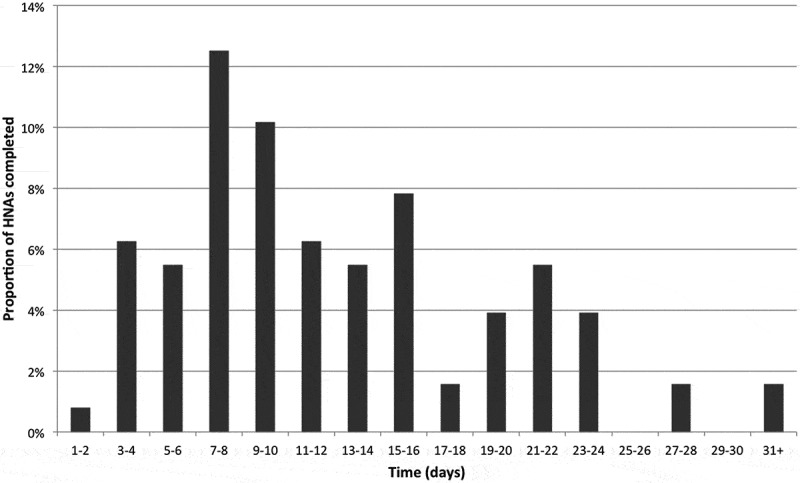
Time taken to complete HNA.
Prior to the start of this project, the only data capture of delays across the hospital was through the Situation Report (“Sit Rep”) that was collated by “Discharge Coordinators”. The Sit Rep was based on the Discharge Coordinators’ information gathered from wards each day and delays were identified where target times were exceeded (for completion of assessments once patients were considered medically stable).
The average number of delays reported on each Sit Rep was 18. With no clear benchmark to define when a delay had occurred, there was a degree of subjectivity in this reporting. Pro-active work to address the identified delays was hampered by the lack of an internal escalation process within the hospital and by a lack of knowledge of what resources were available to help.
5. Understanding the problem through soft systems methodology
Between October 2012 and October 2013, the authors conducted a study in the hospital using SSM (Checkland, 1981) to understand causes of delays to patient discharge. A systems approach to the problem was expected from the start of the research as indicated earlier. The Problem Structuring Methods of Strategic Options Development and Analysis (SODA) and the Strategic Choice Approach (SCA) were considered but rejected for this study, since from an early stage in the process, they would have required interactive workshops, usually with multiple participants at a time (Rosenhead, 1996). These would have been difficult to organise given the time pressures that existed for the practitioners we hoped to involve in the study. Instead, one-to-one interviews were used as the primary means of capturing the many stakeholder perspectives that we felt were relevant to the problem situation. Two of the authors had experience of successfully applying Checkland’s seven-stage process for SSM (Checkland, 1981). We felt that it would be a practical and effective approach for understanding the problem and identifying possible interventions; it was therefore selected to form the basis for our study.
Through a series of 20 structured interviews, problems encountered in the discharge process were found to include “ineffective communication, slow processing of paperwork, limited forward planning, no clear ownership of the process and delays in finding care in the community” (Emes et al., 2017). The study identified two worldviews – health professionals’ natural inclination to care for the patients in front of them, and the need for operational efficiency and responsibility to the wider community – to offer beds and treatment when they are needed. Following the normal SSM process (Checkland, 1981; Wilson, 2001), the essence of the discharge process from each worldview was formally defined using a root definition in the form “a system to do P by Q in order to achieve R”, elaborated by identifying the Customer, Actor, Transformation, Worldview, Owner and Environmental Constraints. Each root definition was then developed into a distinct conceptual model, showing the sequence of logical steps that needed to occur to enable the transformation at the heart of the discharge process. The two conceptual models were named “Care” and “Flow”, and the transformation and worldview associated with each model are given in Table 3.
Table 3.
Transformation and worldview in two models of discharge process.
| Care Model | Flow Model | |
|---|---|---|
| Transformation | Medically stable patients receiving care in the hospital → Medically stable patients no longer receiving care within the hospital | Patients admitted to the hospital in need of acute care → Patients outside the hospital no longer needing acute care |
| Worldview | Keeping the patient in the safe hospital environment and starting discharge planning only when the patient is medically stable avoids wasted practitioner time (since the patient’s condition may change) and minimises the risk of readmission | Discharging planning starts on admission so that patients spend the minimum amount of time in the hospital possible (whilst suitably managing the risk of readmission); this best serves the needs of the patient and the wider community |
The identified tension between the two worldviews reinforced previous findings reported by Connelly et al. (2009). All practitioners recognised the relevance of both models to some extent, with the sympathy for the model varying across the range of practitioners involved in the study. We found that the Care philosophy was more strongly held by Doctors and Social Care Practitioners, whilst the Flow philosophy was more strongly held by Occupational Therapists, Managers and Discharge Coordinators. On average, however, there was significantly stronger support for the Flow model across the group than for the Care model. What this greater support for the Flow model means in practice is not yet understood. The fact that practitioners recognised the principle of planning ahead and thinking strategically to manage the discharge process better was significant in shaping the proposed interventions described below, and the performance measures outlined below are therefore largely aligned with the aspirations of the Flow worldview. Further details of the approach and findings of the systems thinking study have been published previously (Emes et al., 2017) and will therefore not be discussed further here. This paper reports on the design and results of the interventions that followed this study.
6. Initiatives to improve the discharge process
Following the systems thinking study described above, three initiatives were proposed with the following focuses:
“HNA”: Reducing the time taken to complete Health Needs Assessments (HNAs). The average time taken to complete HNAs at the start of the project was 12.7 days, whilst the hospital target was three days. This addressed the “keeping the process moving” theme in Table 2.
“Sit Rep”: Extending the daily Situation Report or Sit Rep of delays within the hospital by involving other practitioners and collating daily resource availability. This initiative aligned with the “effective communication” theme in Table 2.
“Front Door”: Developing an integrated model of working to establish early intervention and improved patient flow from front door to discharge, seven days a week, inspired by the “Proactivity” theme in Table 2.
These initiatives and the specific interventions involved for each are outlined in the sections below. The results of the three initiatives are given together in the Results section below.
7. Initiative 1: HNA
The “HNA” initiative sought to ensure that processing of HNAs was not a barrier to the timely discharge of patients. The performance criterion or Key Performance Indicator (KPI) for this aspect was therefore (reduced) mean time between a patient being declared medically stable and the patient being discharged from hospital (denoted here TMS →DIS). It was assumed that checks were in place to ensure that patients could not be discharged before it was appropriate.
7.1. Intervention 1.1: HNA training for nurses
In January–February 2013, training was given to Nurses on a care of the elderly ward and a cardiology ward, to give clearer information on how to complete HNAs (consisting of a checklist and a model HNA to illustrate the standard required).
7.2. Intervention 1.2: removal of HNAs
In March and April 2013, a radical approach was taken to reduce the number of HNAs being completed on a care of the elderly ward and an orthopaedic ward (these wards were selected as they had a high level of referrals for HNA completion and were struggling to meet demand). It was agreed that, on these wards, HNAs would only be completed for patients that were being discharged to care homes. For patients with complex needs that were returning home, a checklist rather than an HNA was used to assess the level of support that they would require. The checklist assessed a patient’s needs across 12 domains and was used to determine whether the patient reached the threshold for (funded) continuing health care. Social Care Practitioners completed the checklist with patients, their relatives and other member of the Multi Disciplinary Team as necessary. It was a simpler process, requiring less time to complete than an HNA.
8. Initiative 2: sit rep
Daily Situation Reports or Sit Reps were previously conducted by Discharge Coordinators, but they had limited impact. The objective of the Sit Rep initiative was to identify and overcome any barriers or anticipated delays to a patient’s timely and safe discharge, primarily by increasing involvement of other members of the discharge team. The KPI for this initiative was again mean time between a patient being declared medically stable and the patient being discharged from hospital (T MS→DIS) .
8.1. Intervention 2.1: daily review of delayed patients
A daily (five days per week) meeting was held with the hospital’s Deputy Director of Operations for Access and Support, to look at the Discharge Coordinators’ list of the patients they believed were being delayed across the hospital. From 1st July, a pilot was carried out on two wards to trial an IT process on the hospital’s patient information system to enable key staff to update patient lists electronically each day to highlight delays across the hospital. In parallel, daily meetings were held on the wards involving the discharge team, social care and therapy teams to review patient progress.
8.2. Intervention 2.2: resource availability database
A working group (with representatives from the hospital, social care, and community health) was established and aimed to create a single point of access database for resource availability, to be updated daily. This would provide information on availability of community health beds, intermediate care, and reablement and respite care. The possibility of adding social care contract bed availability would be investigated.
9. Initiative 3: front door
The Front Door initiative aimed to develop a collaborative model of working to establish early intervention and improved patient flow from front door to discharge, seven days a week. In addition, it sought to capture and share information more effectively, avoiding the need for patients to answer the same question multiple times with different practitioners.
The KPIs for this initiative were: (1) reduced time taken (denoted here T AD →SOC) between admission and referral to the social care team for patients that are expected to have social care needs, (2) reduced overall length of stay (denoted here T AD →DIS).
9.1. Intervention 3.1: integrated discharge team with social care practitioners
An “Integrated Discharge Team” had been operating at the hospital for some time. This was a team of Nurses and Occupational Therapists that provided a rapid-response service so that as many patients as possible could receive the treatment they needed within 72 h of admission without being admitted to wards. These patients had priority over ward patients for placements or community beds. As part of the new seven-day working practice in the hospital, this Front Door initiative added Social Care Practitioners to the Integrated Discharge Team to help identify patients with social care needs as early as possible.
9.2. Intervention 3.2: SPRING form
A shared pro-forma for information gathering (SPRING) was created and implemented on three wards from March 10 2014 (two “care of the elderly” wards and a “diabetes and young adults” ward). Five control wards were identified that continued to use the existing process (respiratory ward, breast surgery and gynaecology ward, stroke and neurology ward, cardiology ward, gastroenterology ward). This form was used when patients came through A&E/assessment units and were referred to the Integrated Discharge Team. The pro-forma included information on social care circumstances, therapy needs and goals and community health involvement. It provided a snapshot of a patient’s circumstances prior to admission and gave recommendations for on-going treatment/support, either on the ward or back in the community if admission were not needed. The advantages of the SPRING format were that:
The patient only had to answer questions about his/her circumstances once.
It reduced the time taken to refer for social care support and for social care to be aware of the need; the previous average across the hospital of 8.5 days for a person to be referred to the social care team represented an unnecessary delay.
It was believed that by improving communication between practitioners by implementing a clearly understood process, timely discharge was more likely, as supported by previous research (Baumann et al., 2007).
10. Results
The results of the various interventions are described in turn in the sections below. In each case, the impact of the interventions was judged by looking at anonymised data provided to the authors from the hospital database, including key dates, such as date of admission, date of referral for social care, date at which patient was considered medically stable and date of discharge. For each intervention, the null hypothesis H0 is that the mean value of the relevant KPI (for example, length of stay) is unaffected by the intervention. The alternative hypothesis Ha for each intervention is that there is a non-zero reduction in the mean value of the relevant KPI. We reject the null hypothesis if the p-value calculated for each hypothesis test is less than 0.05.
10.1. Results of intervention 1.1: HNA training for nurses
The training given to Nurses on how to complete an HNA had no measurable impact in this study. Very early indications had suggested that there had been no significant improvement from this training; the decision was therefore taken by senior executives to trial removal of HNAs on the wards in question before significant data could be captured to confirm this. The null hypothesis therefore cannot be rejected for this intervention.
10.2. Results of intervention 1.2: removal of HNAs
A trial of removing HNAs on two wards was first conducted involving 24 patients across two wards over a six-month period from February 2013 to August 2013. Given that the population standard deviation and mean were not known, and we had reason to believe that the standard deviation of the two samples might change as a result of removing HNAs, we analysed the data using a two-sample t-test with unequal variance (Welch’s t-test). The t-statistic, and degrees of freedom, df, are given by the following equations, where x 1 and x 2 are the means of the first and second samples respectively, s 1 and s 2 are the standard deviations of the two samples, and n 1 and n 2 are the number of patients in each of the two samples (Coombs, Algina, & Oltman, 1996).
The patients with HNAs spent an average x 1 of 37.9 days (SD s 1 = 10.2) between being declared medically stable and being discharged. When the HNAs were subsequently removed on the same wards, the interval between being declared medically stable and being discharged fell to an average x 2 of 28.1 days (SD s 2 = 10.1). With a t-statistic of 2.22, and corresponding degrees of freedom df = 14.1, we have a one-tailed p-value of 0.022. The null hypothesis is therefore rejected for this intervention. It is worth noting that the two wards on which the trial ran both had a high proportion of elderly patients. They were therefore used to dealing with patients with complex needs and had well-developed processes for conducting daily multi-disciplinary team meetings. Nevertheless, during the trial, the time taken to discharge patients was reduced by 26% (from medically stable to discharge) by using checklists instead of HNAs.
To address the mixed picture and inconsistency of processes for handling HNAs, referrals to social care, checklists and decision support tools across the five acute NHS Trusts in Surrey, the Director of Adult Social Care held a “Rapid Improvement Event” with the Trust Chief Executives in August 2013. Guided by the positive results of the trial described above, the decision was taken at this event to remove HNAs across the hospital from October 2013 (some of the other hospitals had already stopped using HNAs on individual wards, but none had previously taken them out across the whole hospital).
In the period October 2013 to June 2014, a population of 77 patients across 12 wards was reviewed by Social Care Practitioners and ultimately discharged without using HNAs. The average time taken from medically stable to discharge was 28.2 days (SD = 15.3). This is a reduction of 41% from the 47.8 days taken at the start of the project (Figure 2). Using again a two-sample t-test with unequal variance, this gives a t-statistic of 4.95, df of 78.4 and a one-tailed p-value of 2.1 × 10−6.
Figure 2.
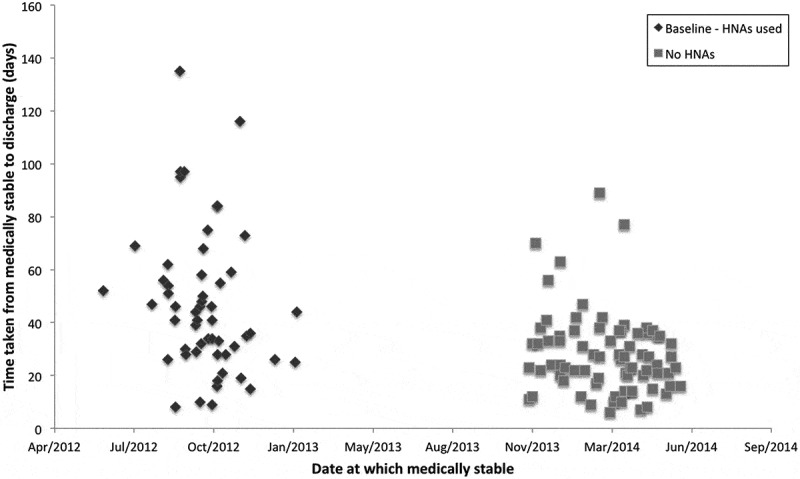
Time taken between medically stable and discharge (ALL WARDS).
11. Results of intervention 2.1: daily review of delayed patients
The trial using the new IT process for Sit Reps proved unsuccessful as too much staff time was required to complete the review, especially because the staff were not familiar with the software used. The pilot was therefore abandoned and was superseded by Consultant-led daily “board meetings” on each ward, where each patient’s situation was reviewed daily using the whiteboard as a focus for discussion. In 2012, before the start of the study, the practice of using whiteboards to capture and discuss in multi-disciplinary teams the information relating to patient progress varied significantly from ward to ward. By the end of the study in mid 2014, examples of good practice had been shared, and use of the whiteboard as a major focus for patient progress reviews had become standardised across the hospital.
The daily discharge team meetings were held at 11 am each weekday and involved the Social Care Manager, Occupational Therapy Manager and Discharge Coordinator to review patient progress across the hospital. This was initially a paper-based exercise but was developed into a database-based system populated by Nurses on an ad hoc basis, which was reviewed three times a week by the multi-disciplinary team. As the trial progressed, it became clear that Nurses had insufficient time to maintain the database, so the multi-disciplinary team took responsibility for populating the database three times a week. This evolved to include meetings twice a week on all medical wards (taking just over two hours each) covering six functions: social care, community hospitals, physiotherapy, occupational therapy, nursing (Matron for Medicine), and discharge coordination. The ultimate aim was not just to avoid delays to the progress of individual patients, but also to try to identify common themes that were causing regular delays.
A RAG (Red, Amber, Green) system was developed to escalate delays to the senior managers in the hospital and a process established to address delays (a high-level weekly discharge meeting with action taken on a daily basis as appropriate).
Although introducing Sit Reps was felt to be an important initiative, we were unable in this study to control the format of the Sit Reps on each ward. The wards started at different levels of maturity, and different Consultants had their own ideas about how best to implement the daily reviews. Furthermore, chronologically, the introduction of Sit Reps overlapped with the removal of HNAs. We are therefore unable conclusively to separate out the effects of the two interventions. We can infer the relative importance of the two initiatives, however, from the findings of the trial in which HNAs were removed on two wards that both already had strong processes for daily patient reviews in place (reported in the “Results of intervention 1.2” section). Here, the average time from medically stable to discharge fell from 37.9 days to 28.1 days for the two trial wards, whereas the results for the hospital as a whole saw the time reduce from 47.8 days to 28.2 days. This suggests that the introduction of Sit Reps and the removal of HNAs were of about equal significance, reducing the time between patients” being medically stable and being discharged by about 10 days each.
11.1. Results of intervention 2.2: resource availability database
Data was previously stored on the social care information drive, which was not accessible to staff in the hospital or in community health. The working group proposed that read-only access should be given to key staff in the hospital and in community health where agreed with Surrey County Council Social Care Managers (with a suitable protocol for access).
The “Effective Data & Information Sharing Across Health & Social Care” project, is now being set up as part of the Public Service Transformation (PST) programme, and aims to deliver:
Shared understanding across the Surrey health and social care system, of the importance of data and information sharing, the barriers and how these will be overcome.
Jointly agreed Surrey data and information sharing protocol(s) between health and social care partners.
Active sharing of data and information between health and social care partners.
This intervention did not have an impact within the time scale of the study. We are therefore unable to reject the null hypothesis for this intervention.
12. Results of intervention 3.1: integrated discharge team with social care practitioners
At various times, between one and three Social Care Practitioners were added to the Integrated Discharge Team. Since this ran concurrently with the introduction of the SPRING form, the impact of the two interventions cannot be separated.
12.1. Results of intervention 3.2: SPRING form
When the SPRING form was used, Social Care Practitioners, Physiotherapists, Occupational Therapists, and Nurses had mini multi-disciplinary team meetings every day to decide if a social care referral were needed.
The SPRING form was placed in the healthcare records (in a newly designed A&E information pack), scanned in to the Adult Social Care database, and any therapy goals identified and treatment plans used to inform the reablement team or intermediate care team post discharge if the patient were not admitted. If the patient were ultimately admitted to a ward, the SPRING form replaced the Section 2 form (which was seen as bureaucratic by health and social care practitioners at the hospital and contributed to a blame culture for delays). The SPRING form was then used to inform any on-going involvement of social care or therapy and intermediate care teams.
Before the SPRING forms were introduced, from the start of January to the end of February 2014, 207 patients across the eight wards under investigation had Section 2 forms produced to indicate they had social care needs and were later discharged from the hospital. Date of admission, date of referral for social care and date of discharge for these patients were recorded. The average length of time from admission to referral to social care (using Section 2 forms) was 8.2 days (SD = 8.3), which is slightly lower than the previous average across the hospital of around 8.5 days, perhaps reflecting the positive impact of other initiatives, such as including Social Care Practitioners in the Integrated Discharge Team. Average length of stay (T AD →DIS), ie, date of discharge – date of admission) for all eight wards was 23.3 days (SD = 15.8).
Eighty-eight patients of the 207 were on the three wards chosen to apply SPRING forms; these patients had an average time between admission and social care referral of 7.6 days (SD = 10.2) and average length of stay of 23.1 days (SD = 16.0). The lower time for social care referral is expected here, since two out of the three wards were “care of the elderly” wards, where referral to social care is common. 119 patients on the five control wards had an average time for social care referral of 8.6 days (SD = 6.6) and an average length of stay of 23.6 days (SD = 15.7).
After the SPRING form was introduced, average length of stay for 93 patients admitted to the three wards between 10th March and July 10 2014 fell from 23.1 to 18.6 days (SD = 11.1) – a reduction of 20%. The t-statistic for the two-sample t-test with unequal variance was 2.19, df was 154 and the one-tailed p-value was 0.015. The null hypothesis is therefore rejected for the length of stay KPI. Average time taken for social care referral using the SPRING forms fell 17% from 7.6 days to 6.3 days (SD = 4.3), with t = 1.11, df = 116, p = 0.135. The null hypothesis cannot be rejected for the time taken for social care referral KPI. The distribution of results for the population is shown in Figure 3. In the same period, average time taken for social care referral using Section 2 forms on the five control wards remained unchanged at 8.6 days (SD = 10.8) and length of stay was 23.5 days (SD = 22.5) for 248 patients (cf. 23.6 days before the SPRING form was introduced).
Figure 3.
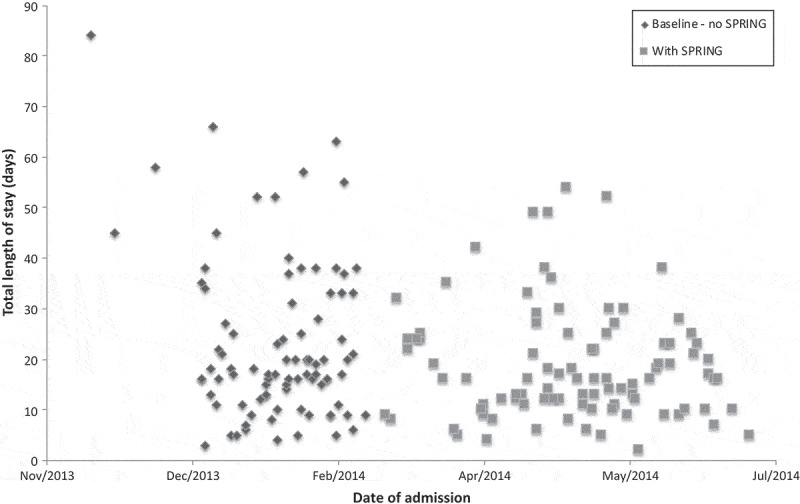
Effect of spring forms on length of stay (TRIAL ON 3 WARDS).
The results of the interventions made over the course of the project are summarised in Figure 4.
Figure 4.
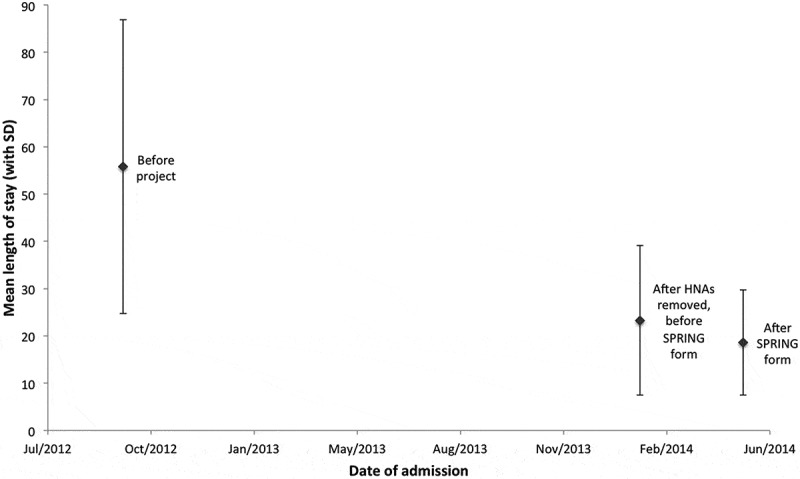
Impact of the interventions on length of stay.
Mean length of stay fell 67% from 55.8 to 18.6 days for the sample population of patients with complex needs (involving health and social care aspects) over the course of this two-year project. Note that the authors did not have access at the start of the project to patient-level values of time between admission to issuing of an HNA, although the mean time was known to be 8 days. Not knowing the standard deviation of this value, a conservative estimate was taken to assume a bimodal distribution with half of patients referred immediately, and half after 16 days. This gave the required mean of 8 days, and a standard deviation of 8 for the 54 patients considered in the sample. When two independent normally distributed variables are added, the mean of the distribution is given by the sum of the two means and the variance is given by the sum of the two variances. The mean total length of stay is therefore given by the sum of the mean time between admission to issuing of an HNA (8 days), plus the mean time between issuing of HNA and discharge (47.8 days). The standard deviation in length of stay is given by the square root of 26.12 plus 82, giving an overall standard deviation of 27.3. The two-sample t-test with unequal variance therefore has a t-value of 9.6, df of 63.3 and p of 3.5 × 10−14. The results of the hypothesis tests are summarised in Table 4 below.
Table 4.
Summary of results of hypothesis tests.
| Intervention | KPI | x1 | x2 | s1 | s2 | n1 | n2 | t | df | p | Null hypothesis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.1 | TMS→DIS | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Retain |
| 1.2 | TMS→DIS | 37.9 | 28.1 | 10.2 | 10.1 | 16 | 8 | 2.22 | 14.1 | 0.022 | Reject |
| 1.2/2.1 | TMS→DIS | 47.8 | 28.2 | 26.1 | 15.3 | 54 | 77 | 4.95 | 78.4 | 2.1 × 10−6 | Reject |
| 2.2 | TMS→DIS | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Retain |
| 3.1/3.2 | TAD→DIS | 23.1 | 18.6 | 16.0 | 11.1 | 88 | 93 | 2.19 | 154 | 0.015 | Reject |
| 3.1/3.2 | TAD→SOC | 7.6 | 6.3 | 10.2 | 4.3 | 88 | 93 | 1.11 | 116 | 0.14 | Retain |
| Overall | TAD→DIS | 55.8 | 18.6 | 27.3 | 11.1 | 54 | 93 | 9.56 | 63.3 | 3.5x10−14 | Reject |
Based on the results summarised in Table 4, we are able to reject the null hypothesis and confirm that removing HNAs (Intervention 1.2) and conducting daily Sit Reps (Intervention 2.1) together led to a reduction in the mean time between medically stable and discharge (T MS →DIS), and confirm that conducting the Sit Reps on their own also led to a significant reduction in T MS →DIS. We can also reject the null hypothesis and say that adding Social Care Practitioners to the Integrated Discharge Team (Intervention 3.1) and implementing the SPRING form (Intervention 3.2) together led to a reduction in length of stay (T AD →DIS). Finally, we can reject the null hypothesis for the project overall, and conclude that the full set of interventions collectively led to a significant reduction in length of stay. The hypothesis test results allow us to verify the statistical significance of the interventions, but we can also confirm the substantive significance of the key results using confidence intervals (CIs) (Seltman, 2015). For Interventions 1.2 and 2.1 (removing HNAs and conducting daily Sit Reps), we can say with 95% confidence that the time between being medically stable and being discharged is reduced by the interventions by an amount between 11.7 and 27.5 days, ie, the 95% CI is [11.7, 27.5]. For Interventions 3.1 and 3.2 (addition of Social Care Practitioners and implementing the SPRING forms), the 95% CI is [0.44, 8.56]. The interventions’ overall reduction in length of stay had a 95% CI of [29.4, 45.0].
13. Discussion
The average time taken between patients’ becoming medically stable and being discharged fell by 41% in the sample group (by a minimum of 25% with 95% confidence) when HNAs were removed across the hospital and daily Sit Reps were introduced on all wards. When the SPRING forms were also introduced, overall length of stay was reduced by 67% (by a minimum of 53% with 95% confidence). The research project was started on the assumption that patients with complex needs were spending longer on the wards than necessary. The authors therefore expected to see a reduction in the overall length of stay through the interventions that were implemented. It was surprising to see such a large overall improvement in the mean length of stay, however. Comparison with other studies suggests that the hospital may still be able to make further improvements, though, as the average length of stay in the UK for older patients was reported to be 12 days (National Audit Office, 2016). Whilst there have been many studies previously investigating discharge planning, limited data exists that reports on the effectiveness of initiatives to improve the situation, and most previous studies report relatively modest gains. For example, reviews of the effectiveness of introducing individualised discharge plans have found that these reduce length of stay by an average of just one day Shepperd et al. (2016, 2003).
In our study, each of the three main interventions undertaken: removing HNAs, better management of barriers to discharge through regular patient Situation Reports, and earlier identification of patients with social care needs at the front door, provided a statistically and substantively significant improvement. Focusing on the removal of HNAs, comparison with the other four acute hospitals across Surrey shows a mixed picture. For example, one hospital removed HNAs on four wards and one completely removed HNAs; both of these hospitals replaced HNAs with a simpler checklist process, with variable results. The two other hospitals kept the HNA process in place.
Proactive management of patients at the “front end” has been a long-standing ambition of hospitals as they seek to reduce admission to wards where possible (Department of Health, 2010; Purdy, 2010), and the initiative described here to include SPRING forms to alert Social Care Practitioners of patients with probable social care needs at the front door proved very effective. Time taken for social care referral using SPRING fell by 17%, and total length of stay with SPRING fell by 20% (by a minimum of 1.9% with 95% confidence), whilst on the control wards, time taken for social care referral using Section 2 forms and total length of stay were unchanged. At the same time as the SPRING forms were introduced (Intervention 3.2), Social Care Practitioners were added to the Integrated Discharge Team (Intervention 3.1). Since these interventions were made concurrently, it is not yet known what relative contribution each of these interventions made. By way of comparison, the study by Harari et al. (2007) mentioned previously achieved a 37% reduction in length of stay (from 18 to 11.4 days) for elderly patients by introducing a (multi-disciplinary) comprehensive geriatric assessment to screen acute medical admissions.
The positive results of our interventions mean that the systems thinking study (Emes et al., 2017) that preceded the implementation of the interventions can be seen as a case study for the effective impact of SSM in the health sector. In this study, the authors identified a tension between the practitioners’ concerns with the health of the patients on the ward (the so called “care” philosophy), and their concerns with keeping things moving and responding to the needs of the wider population (the “flow” philosophy). It was suggested that the care philosophy might be the instinctive or natural way of thinking in a hospital, aligned to Daniel Kahneman’s (2011) “System 1” way of thinking, with the flow philosophy requiring more time and cognitive effort (“System 2” thinking). The results of our study are consistent with this concept: care comes naturally in a hospital setting, but especially when resources are limited, achieving flow requires a deliberate change to protocols. Some of these changes (such as removing the default requirement to complete Health Needs Assessments) could be considered cost-neutral “nudging” behaviours (Perry, Chhatralia, Damesick, Hobden, & Volpe, 2015; Thaler & Sunstein, 2012; Voyer, 2015), and our results support findings of other studies on changing paperwork requirements (Messing, 2015). Other changes, such as adding staff to the Integrated Discharge Team, will require some investment. In terms of the performance criteria for SSM studies (referring to the definitions provided in Tables 1 and 3), the efficacy of the interventions is clear since the discharge process is successfully transforming patients admitted to the hospital in need of acute care into patients outside the hospital no longer needing acute care (and overall length of stay has been reduced). The efficiency is less clear, however, since the discharge process after the interventions required additional resources to enable the transformation; interventions 1.2 and 2.1 required greater frequency of Sit Reps with involvement from more practitioners than had previously been the case across the hospital, and interventions 3.1 and 3.2 required additional Social Care Practitioners to be added to the Integrated Discharge Team to facilitate the SPRING form initiative. The real financial cost of this has not been quantified, however.
Effectiveness relates to the extent to which the higher-level purpose or longer-term aim is achieved by the transformation or process under investigation (Checkland, 1981; Kotiadis et al., 2013). In this case, it was found through the interviews (Emes et al., 2017) that measures of effectiveness include number of re-admissions (which might indicate premature discharge or inappropriate support after discharge) the average time between a patient being declared medically stable and being discharged, and average length of stay. We want to minimise length of stay for two reasons. Firstly, longer stays in hospital can lead to worse health outcomes and can increase patients’ long-term care needs as they rapidly lose mobility and the ability to complete everyday tasks, such as bathing and dressing (National Audit Office, 2016). Secondly, with limited bed-space and funding (Department of Health, 2010), there is an economic argument for discharging patients as soon as they are medically ready to go. Unfortunately, we cannot from this study yet draw firm conclusions on effectiveness; although average time between a patient being declared medically stable and being discharged and average length of stay have both been reduced by the interventions, we have no data on readmissions and have not measured the long-term impacts on patients or the ultimate economic costs. Ethicality and elegance are difficult concepts to quantify and relate to the way in which the other measures are achieved. Whilst the removal of wasteful processes, such as HNAs in this case seems elegant, there are clearly ethical challenges associated with a pressure to discharge patients too early, when there may be an increased risk of readmission (Dobrzanska, 2004; Glasby, Martin, & Regen, 2008; Start, 1998).
Integrated service delivery and commissioning has become a major focus for healthcare at a national level – such as in the UK through the Better Care Fund and through the Five Year Forward View (NHS England, 2014a; NHS England, 2014b) and internationally (Accenture, 2018). The pressures and tensions of maintaining a high level of individual patient care whilst delivering a timely and value-for money service to the wider community are clear and this project has provided evidence on the efficacy of interventions aimed at improving the quality of delivery by removing sources of inefficiency without compromising patient care in an acute hospital in the UK.
14. Limitations
14.1. Threats to internal validity
The study included two key interventions: the removal of HNAs (Intervention 1.2) and the introduction of SPRING forms (Intervention 3.2).
For Intervention 1.2, Hospital management was keen to address the issues with high length of stay quickly, and took the decision to implement the trial of removing HNAs on both pilot wards concurrently without giving the researchers prior warning or access to any data from other wards that could have been used as a control. This intervention, and the subsequent roll-out of the removal of HNAs to all wards (where no control was possible) was therefore a non-experimental design. The results of these uncontrolled before and after studies should therefore be interpreted with caution (Eccles, Grimshaw, Campbell, & Ramsay, 2003).
Intervention 3.2 was a quasi-experimental, controlled before and after design, in which the SPRING form was introduced on three wards, whilst five control wards were selected, with 548 patients involved in total (207 before, 341 after).
Table 5 describes the expected impact of threats to internal validity for the two interventions, with the most relevant confounding factors being the possibility of Hawthorne effect (Mccambridge, Witton, & Elbourne, 2014) and regression to the mean (RTM) (Linden, 2013) . The control study of Intervention 3.2 suggests the Hawthorne effect was very small, however, and although RTM may have influenced the results of the pilot phase of Intervention 1.2, the subsequent roll-out was conducted across the whole Hospital so RTM will not have been relevant to the final results.
Table 5.
Threats To Internal Validity (Adapted From Robson, Shannon, Goldenhar, And Hale (2001), TABLE 3.1).
| Threat to internal validity | Description | Likely impact for Intervention 1.2 | Likely impact for Intervention 3.2 |
|---|---|---|---|
| Dropout | Overall characteristics of intervention group change due to some participants dropping out, possibly affecting outcome | Several patients died during the study period and their data was excluded from the relevant datasets. This is not expected to affect the overall result. There were no other dropouts. | Several patients died during the study period and their data was excluded from the relevant datasets. This is not expected to affect the overall result. There were no other dropouts. |
| Hawthorne | Involvement of outsiders could affect outcome independent of the main intervention component (eg, because participants know they are being observed) | Pilot phase: Staff on the trial wards during the pilot could have tried especially hard to avoid discharge delays because they knew there was a trial underway, although some of the staff involved in the discharge process will have been unaware of the trial. Rollout phase: It is unlikely that the staff involved felt they were being measured. |
If the Hawthorne effect significantly influenced the length of stay results, we would expect to see this most strongly near the start of the study, as sensitivity to being observed is likely to fall over time (Robson et al., 2001). In fact, we find the reverse – that average length of stay is lower in the second half of the period in which the SPRING form is introduced than in the first. |
| History | Other events may take place during the trial and influence the results | There were no known initiatives (other than those described in this paper) during the hospital at the time that could be expected to have directly impacted length of stay. Seasonal variations and secular trends in length of stay were explored in the control wards and found to be negligible as discussed below | There were no known initiatives (other than those described in this paper) during the hospital at the time that could be expected to have directly impacted length of stay. Seasonal variations and secular trends in length of stay were explored in the control wards and found to be negligible as discussed below. |
| Instrumentation | Measurement method or its validity changes during the intervention | Measurement method and its validity were constant throughout the study. | Measurement method and its validity were constant throughout the study. |
| Maturation | Intervention group develops in ways independent of the intervention, possibly affecting the outcome | This was not relevant in this study. | This was not relevant in this study. |
| Placebo | Participants believe that an intervention has material efficacy, even where is none | This was not relevant in this study. | This was not relevant in this study. |
| Regression to the mean (RTM) | Basis for choosing the intervention group is a greater need for the intervention; this would be expected to naturally change towards a normal value | Pilot phase: There is potential for RTM, since the two wards selected for the pilot were known to have been experiencing particular problems processing HNAs in a timely manner. Rollout phase: Since the intervention was implemented across the whole hospital, RTM should not be relevant. | The three wards chosen to implement the SPRING form showed fairly typical performance before the trial, with mean length of stay of 23.1 days (SD = 16.0); for all eight wards, the mean was 23.3 days (SD = 15.8). We therefore expect the RTM effect to be negligible in this case. |
| Testing | Taking measurements could have an effect on the outcome | This was not relevant in this study. | This was not relevant in this study. |
14.2. Seasonal variations and secular trend in length of stay
The pre-intervention measurements of length of stay were made during the winter months (January to February 2014), whilst the post-intervention measurements were made in late spring/early summer (10th March to 20th July). We therefore expected to find a change in length of stay over this period due to seasonal factors. In addition, we anticipated that there might be a small change due to secular (non-periodic) drift, since hospitals across Europe have seen a gradual reduction in length of stay since 2002 as discussed previously (Miani et al., 2014). In fact, analysis of the control group shows that there was no change in length of stay over this period (23.5 days for 248 patients after the intervention, compared to 23.6 days for 119 patients before the intervention). Since we would expect both of these factors to tend to reduce length of stay, we conclude that neither can be significant for our study.
14.3. External validity
Since the study was carried out in just one hospital, the external validity of our findings is unclear. We cannot be certain that the significant improvements to length of stay that we observed were not in some part influenced by factors specific to the hospital. Although we have no reason to believe that the hospital was particularly unusual when compared to other major UK hospitals, we do know that the average length of stay measured at the start of the study was very high, so there could be expected to be a significant RTM effect if we were to attempt to use the results to predict what might be achieved in other hospitals.
15. Conclusions
Through improved integrated working and the removal of non-value adding paperwork (Health Needs Assessment forms), this project has achieved a significant reduction in length of stay for patients with health and social care needs. This will have an impact not only on the patient experience on the wards, but also on the ability of the hospital to cater for the health needs of the wider community. Many other UK hospitals are now also removing Health Needs Assessments, and the SPRING form, which anticipates future patient needs at the front door, has now been rolled out across the hospital that was the focus of this study. Further work is needed to understand how the presence of Social Care Practitioners in the Integrated Discharge Team impacts performance, since this intervention ran concurrently with the introduction of the SPRING form.
The interventions implemented in this study were founded on a study that used SSM to understand the perceptions of a range of different health and social care practitioners in the hospital. The success of the interventions highlights the importance of engaging with a broad range of stakeholders when undertaking a process change initiative. It also shows the value of applying systems thinking when tackling complex problems.
Over time we will gain a better understanding of the impacts of the initiatives undertaken to reduce length of stay. In particular, one might expect to see an increase in readmission rates if length of stay were reduced too far (Dobrzanska, 2004; Glasby et al., 2008; Start, 1998). The part of the study that examined removal of Health Needs Assessments was an uncontrolled before and after experiment, and the RTM effect may explain some of the reduction in length of stay observed here. Nevertheless, the extent of the decrease was so significant that we can be confident that length of stay can indeed be reduced by removing Health Needs Assessments, particularly where the process for completing them is not strictly defined. In these circumstances, HNAs are seen as non-critical paperwork and their completion is given a low level of priority (Emes et al., 2017). Although this work was carried out in just one UK hospital that was known to have a particular problem with length of stay for patients with complex needs, recent decisions by other UK hospitals to partially or completely remove HNAs suggests that others have come to similar conclusions on the effectiveness of this change.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Accenture (2018) Connected health: The drive to integrated healthcare delivery [Online]. Available: https://www.accenture.com/us-en/insight-making-case-connected-health [Accessed 20 Sep 2018].
- Bauer M., Fitzgerald L., Haesler E., & Manfrin M. (2009). Hospital discharge planning for frail older people and their family. Are we delivering best practice? A review of the evidence. Journal of Clinical Nursing, 18, 2539–2546. [DOI] [PubMed] [Google Scholar]
- Baumann M., Evan S., Perkins M., Curtis L., Netten A., Fernandez J.-L., & Huxley P. (2007). Organisation and features of hospital, intermediate care and social services in English sites with low rates of delayed discharge. Health & Social Care in the Community, 15, 295–305. [DOI] [PubMed] [Google Scholar]
- Gonçalves-Bradley D., Lannin N., Clemson L., Cameron I., & Shepperd S. (2016). Discharge planning from hospital (Review). Cochrane Database of Systematic Reviews [Web]. Available:https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000313.pub5/full [Accessed 21 Sep 2018.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checkland P., & Poulter J. (2006). Learning for action: A short definitive account of soft systems methodology and its use for practitioners, teachers and students. Chichester: Wiley. [Google Scholar]
- Checkland P., & Scholes J. (1990). Soft Systems Methodology in Action. Chichester: Wiley. [Google Scholar]
- Checkland P. B. (1981). Systems Thinking, Systems Practice. Chichester: Wiley. [Google Scholar]
- Connelly M., Grimshaw J., Dodd M., Cawthorne J., Hulme T., Everitt S., … Deaton C. (2009). Systems and people under pressure: The discharge process in an acute hospital. Journal of Clinical Nursing, 18, 549–558. [DOI] [PubMed] [Google Scholar]
- Coombs W. T., Algina J., & Oltman D. (1996). Univariate and multivariate omnibus hypothesis tests selected to control type I error rates when population variances are not necessarily equal. Review of Educational Research, 66, 137–179. [Google Scholar]
- Cummings C., & Cockerham C. (1997). Ethical dilemmas in discharge planning for patients with Alzheimer’s disease. Health and Social Work, 22, 101–108. [DOI] [PubMed] [Google Scholar]
- Cummings S. (1999). Adequacy of discharge plans and rehospitalisation among hospitalised dementia patients. Health and Social Work, 24, 249–259. [DOI] [PubMed] [Google Scholar]
- Deming W. E. (1982). Out of the crisis. Cambridge, Massachussetts: MIT Press. [Google Scholar]
- Department of Health (2003). Discharge from hospital: Pathway process and practice [Online]. Available: http://www.wales.nhs.uk/sitesplus/documents/829/DoH%20-%20Discharge%20Pathway%202003.PDF [Accessed 21 Sep 2018]. [Google Scholar]
- Department of Health (2010) Ready to go? Planning the discharge and the transfer of patients from hospital and intermediate care.
- Deschodt M., Braes T., Broos P., Sermon A., Boonen S., Flamaing J., & Milisen K. (2011). Effect of an inpatient geriatric consultation team on functional outcome, mortality, institutionalization, and readmission rate in older adults with hip fracture: a controlled trial. Journal of the American Geriatrics Society, 59, 1299–1308. [DOI] [PubMed] [Google Scholar]
- Dobrzanska L. (2004). Readmissions ‐ An evaluation of reasons for unplanned readmissions of older people: A United Kingdom and international studies literature review. Quality in Ageing and Older Adults, 5, 20–28. [Google Scholar]
- Eccles M., Grimshaw J., Campbell M., & Ramsay C. (2003). Research designs for studies evaluating the effectiveness of change and improvement strategies. BMJ Quality & Safety, 12, 47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis G., Whitehead M. A., Robinson D., O’neill D., & Langhorne P. (2011). Comprehensive geriatric assessment for older adults admitted to hospital: Meta-analysis of randomised controlled trials BMJ, 343. doi:10.1136/bmj.d6553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emes M. R., Smith S., Ward S., Smith A., & Ming T. (2017). Care and flow: Applying soft systems methodology to understand the patient discharge process. Health Systems, 6, 260–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- England N. H. S. (2014a) Better Care Fund [Online]. Available: http://www.england.nhs.uk/ourwork/part-rel/transformation-fund/bcf-plan/[Accessed 5thNovember 2014].
- Forrester J. W. (1958). Industrial dynamics: A major breakthrough for decision makers. Harvard Business Review, 36, 37–66. [Google Scholar]
- Glasby J., Martin G., & Regen E. (2008). Older people and the relationship between hospital services and intermediate care: Results from a national evaluation. Journal of Interprofessional Care, 22, 639–649. [DOI] [PubMed] [Google Scholar]
- Harari D., Martin F. C., Buttery A., O’neill S., & Hopper A. (2007). The older persons’ assessment and liaison team ‘OPAL’: Evaluation of comprehensive geriatric assessment in acute medical inpatients. Age and Ageing, 36, 670–675. [DOI] [PubMed] [Google Scholar]
- Hitchins D. K. (2003). Advanced systems thinking, engineering and management. Norwood MA: Artech House. [Google Scholar]
- Hurley E., Mcrae I., Bigg I., Stackhouse L., Boxall A.-M., & Broadhead P. (2009). The australian health care system: he potential for efficiency gains. Canberra: National Health and Hospitals Reform Commission. [Google Scholar]
- Kahneman D. (2011). Thinking, fast and slow. New York, Farrar: Straus and Giroux. [Google Scholar]
- Katsaliaki K., Brailsford S., Browning D., & Knight P. (2005). Mapping care pathways for the elderly. Journal of Health Organization and Management, 19, 57–72. [DOI] [PubMed] [Google Scholar]
- Kauffman D. L. (1980). Systems one: An introduction to systems thinking. St Paul MN: TLH Associates. [Google Scholar]
- Kotiadis K., Tako A. A., Rouwette E. A. J. A., Vasilakis C., Brennan J., Gandhi P., … Webb P. (2013). Using a model of the performance measures in soft systems methodology (SSM) to take action: A case study in health care. Journal of the Operational Research Society, 64, 125–137. [Google Scholar]
- Kotiadis K., Tako A. A., & Vasilakis C. (2014). A participative and facilitative conceptual modelling framework for discrete event simulation studies in healthcare. Journal of the Operational Research Society, 65, 197–213. [Google Scholar]
- Linden A. (2013). Assessing regression to the mean effects in health care initiatives. BMC Medical Research Methodology, 13, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maramba P., Richards S., & Larrabee J. (2004). Discharge planning process: Applying a model for evidence-based practice. Journal of Nursing Care Quality, 19, 123–129. [DOI] [PubMed] [Google Scholar]
- Mccambridge J., Witton J., & Elbourne D. R. (2014). Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. Journal of Clinical Epidemiology, 67, 267–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messing J. (2015). Improving handover from intensive care to ward medical teams with simple changes to paperwork BMJ Quality Improvement Reports, 4(1). doi: 10.1136/bmjquality.u206467.w2913 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miani C., Ball S., Pitchforth E., Exley J., King S., Roland M., … Nolte E. (2014). Organisational interventions to reduce length of stay in hospital: A rapid evidence assessment In Health services and delivery Research (pp. 2). Southampton, UK: NIHR Journals Library. [PubMed] [Google Scholar]
- Mitchell F., Gilmour M., & Mclaren G. (2010). Hospital discharge: A descriptive study of the patient journey for frail older people with complex needs. Journal of Integrated Care, 18, 30–36. [Google Scholar]
- Mukotekwa C., & Carson E. (2007). Improving the discharge planning process: A systems study. Journal of Research in Nursing, 12, 667–686. [Google Scholar]
- National Audit Office (2003). Ensuring the effective discharge of older patients from NHS acute hospitals. London: The Stationery Office. [Google Scholar]
- National Audit Office (2016) Discharging older patients from hospital.
- National Health Service and Community Care Act (1990). Chapter 19. London: The Stationery Office. [Google Scholar]
- NHS England (2014b) Five Year Forward View.
- NHS England (2015) Delivering the Forward View: NHS planning guidance.
- OECD (2012) Health at a Glance (2012). OECD Indicators. Paris: Organisation for Economic Co-operation and Development. [Google Scholar]
- Ohno T. (1988). Toyota Production System. Portland, Oregon: Productivity Press. [Google Scholar]
- Oliver D., Foot C., & Humphries R. (2014) Making our health and care systems fit for an ageing population [Online]. The King’s Fund. Available: https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/making-health-care-systems-fit-ageing-population-oliver-foot-humphries-mar14.pdf.
- Parker S. (2005). Do current discharge arrangements from inpatient hospital care for the elderly reduce readmission rates, the length of inpatient stay or mortality, or improve health status?. Copenhagen: World Health Organization Regional Office for Europe. [Google Scholar]
- Patching, D (1990). Practical soft systems analysis. London: Pitman. [Google Scholar]
- Payne S., Kerr C., Hawker S., Hardey M., & Powell J. (2002). The communication of information about older people and social care practitioners Age and Ageing, 31(2), 107-117 . [DOI] [PubMed] [Google Scholar]
- Perry C., Chhatralia K., Damesick D., Hobden S., & Volpe L. (2015) Behavioural insights in health care. The Health Foundation [Online]. Available: https://www.health.org.uk/publication/behavioural-insights-health-care.
- Purdy S. (2010) Avoiding hospital admissions: What does the research evidence say? [Online]. The King’s Fund. Available: http://www.kingsfund.org.uk/sites/files/kf/Avoiding-Hospital-Admissions-Sarah-Purdy-December2010.pdf.
- Rankin J., & Regan S. (2004) Meeting complex needs: The future of social care [Online]. Institute of Public Policy Research and Turning Point. Available: http://www.ippr.org/files/images/media/files/publication/2011/05/Meeting_Complex_Needs_full_1301.pdf?noredirect=1.
- Robson L. S., Shannon H. S., Goldenhar L. M., & Hale A. R. (2001) Guide to evaluating the effectiveness of strategies for preventing work injuries: How to show whether a safety intervention really works. National Institute for Occupational Safety and Health [Online]. Available: https://www.cdc.gov/niosh/docs/2001-119/pdfs/2001-119.pdf.
- Rosenhead J. (1996). What’s the problem? an introduction to problem structuring methods. Interfaces, 26, 117–131. [Google Scholar]
- Royal Academy of Engineering (2017). Engineering better care: A systems approach to health and care design and continuous improvement [Online]. Available: https://www.raeng.org.uk/publications/reports/engineering-better-care [Accessed 21 Sep 2018]. [Google Scholar]
- Seddon J. (2005). Freedom from command and control: Rethinking management for lean service. New York: Productivity Press. [Google Scholar]
- Seddon J., & Caulkin S. (2007). Systems thinking, lean production and action learning Action Learning Research and Practice, 4(1), 9-24. [Google Scholar]
- Seltman H. (2015). Experimental Design and Analysis. Carnegie Mellon University [Online] Available: http://www.stat.cmu.edu/~hseltman/309/Book/Book.pdf [Accessed 21 Sep 2018]. [Google Scholar]
- Shepperd S., Lannin N. A., Clemson L. M., Mccluskey A., Cameron I. D., & Barras S. L. (2003). Discharge planning from hospital to home. Cochrane Database of Systematic Reviews [Online] Available: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000313.pub4/full [Accessed 21 Sep 2018]. [Google Scholar]
- Start K. (1998). A study of readmissions in two acute trusts: Quantitative aspects of the readmission study in barking, dagenham and havering. public health research report no 67. barking and havering health authority. Romford (United Kingdom): Directorate of Public Health. [Google Scholar]
- Thaler R. H., & Sunstein C. R. (2012). Nudge: Improving decisions about health, wealth and happiness. London: Penguin. [Google Scholar]
- Thomson S., Foubister T., & Mossialos E. (2009). Financing health care in the european union: Challenges and policy responses. Copenhagen: European Observatory on Health Systems and Policies. [Google Scholar]
- Victor C. R., Healy J., Thomas A., & Seargeant J. (2000). Older patients and delayed discharge from hospital. Health & Social Care in the Community, 8, 443–452. [DOI] [PubMed] [Google Scholar]
- Voyer B. G. (2015). ‘Nudging’ behaviours in healthcare: Insights from behavioural economics. British Journal of Healthcare Management, 21, 130–135. [Google Scholar]
- Welbourn D., Warwick R., Carnall C., & Fathers D. (2012). Leadership of whole systems. The King’s Fund [Online] Available:https://pdfs.semanticscholar.org/cfe3/87436467b6669df884bd86b78e4f1b496d95.pdf [Accessed 21 Sep 2018] [Google Scholar]
- Wilson B. (2001). Soft systems methodology: Conceptual model building and its contribution. Chichester: John Wiley & Sons Ltd. [Google Scholar]
- Wilson B., & van Haperen K., (2015). Soft systems thinking, methodology and the management of change. London: Palgrave. [Google Scholar]
- Womack J. P., Jones D. T., & Roos D. (1990). The Machine that Changed the World. New York: Macmillan. [Google Scholar]
- Zokaei K., Elia S., O’donovan B., Samuel D., Evans B., & Goodfellow J. (2010). Lean and Systems Thinking in the Public Sector in Wales. Lean Enterprise Research Centre [Online] Available: https://www.lgcplus.com/download?ac=1213980 [Accessed 21 Sep 2018] [Google Scholar]


