Abstract
The Nordic Arthroplasty Register Association (NARA) was established in 2007 by arthroplasty register representatives from Sweden, Norway and Denmark with the overall aim to improve the quality of research and thereby enhance the possibility for quality improvement with arthroplasty surgery. Finland joined the NARA collaboration in 2010.
NARA minimal hip, knee and shoulder datasets were created with variables that all countries can deliver. They are dynamic datasets, currently with 25 variables for hip arthroplasty, 20 for knee arthroplasty and 20 for shoulder arthroplasty.
NARA has published statistical guidelines for the analysis of arthroplasty register data. The association is continuously working on the improvement of statistical methods and the application of new ones.
There are 31 published peer-reviewed papers based on the NARA databases and 20 ongoing projects in different phases. Several NARA publications have significantly affected clinical practice. For example, metal-on-metal total hip arthroplasty and resurfacing arthroplasty have been abandoned due to increased revision risk based on i.a. NARA reports. Further, the use of uncemented total hip arthroplasty in elderly patients has decreased significantly, especially in Finland, based on the NARA data.
The NARA collaboration has been successful because the countries were able to agree on a common dataset and variable definitions. The collaboration was also successful because the group was able to initiate a number of research projects and provide answers to clinically relevant questions. A number of specific goals, set up in 2007, have been achieved and new one has emerged in the process.
Cite this article: EFORT Open Rev 2019;4 DOI: 10.1302/2058-5241.4.180058
Keywords: Nordic Arthroplasty Register Association (NARA), total joint arthroplasty, minimal dataset, statistical analyses, revision surgery
Introduction
The Nordic countries, including Denmark, Sweden, Finland and Norway, all have a long and successful tradition of arthroplasty registers. These registers are characterized by high research activity with a focus on improving the quality of care for patients undergoing arthroplasty surgery. However, the results presented by the Nordic registers have suggested differences among the countries related to variations in data collection systems, variables that are included, variable definitions and statistical methods used. Reports from the Nordic registers have further shown differences regarding the incidence and indication for surgery, characteristics of the joint replacement populations, implants used, fixation methods used and implant survival. Due to these differences, the results from the different Nordic registers have not been fully comparable. Furthermore, although the Nordic registers are population-based, the number of patients included in specific sub-populations (e.g. patients that have undergone joint replacement due to rheumatoid arthritis (RA) or patients operated due to osteonecrosis) or the number of patients incurring specific adverse events after surgery (e.g. revision due to infection or periprosthetic fracture) are relatively small, which limits the statistical precision of risk estimates and the possibility to draw valid conclusions.
The Nordic registers have acknowledged these limitations and the need for collaboration across national borders in order to create common databases, which complete the limitations from each register. Thus, NARA was established in 2007 by arthroplasty register representatives from Sweden, Norway and Denmark. Finland joined the NARA collaboration in 2010. The aim of NARA is to improve the quality of research and understanding of the clinical course of patients undergoing joint replacement surgery and thereby improve the results after joint replacement surgery.
In order to achieve the overall aim of NARA, several specific aims were set. The basic prerequisite for the collaborative work was to create common Nordic minimal datasets in hip, knee and shoulder arthroplasty. With the common datasets, we are able to compare demographics and results of joint replacement surgery among countries, and study results in patient groups, which are too small to be studied in each separate country. NARA aims to promote joint Nordic research on specific problems of common interest. Collaboration between the different national research teams and compilation of big datasets will contribute to a higher quality of the analyses performed. Another specific aim of NARA is to discuss and agree upon methodology and coordinate quality improvements as regards data capture and analyses. In addition, NARA also coordinates a joint Nordic standpoint towards other international register associations.
The NARA steering committee and other representatives from each member country are responsible for overseeing the aims and directing the NARA work. Nowadays, NARA has at least two face-to-face meetings yearly, in addition to frequent teleconferences and web-meetings. NARA consists of people with different academic background, including orthopaedic surgeons, epidemiologists, biostatisticians, PhD students, software developers and registry coordinators. The registers currently involved in NARA are the Danish Hip Arthroplasty Register, the Danish Knee Arthroplasty Register, the Danish Shoulder Arthroplasty Register, the Finnish Arthroplasty Register, the Norwegian Arthroplasty Register, the Swedish Hip Arthroplasty Register, the Swedish Knee Arthroplasty Register and the Swedish Shoulder Arthroplasty Register.
The aim of this paper is to describe the NARA collaboration and review a selection of published NARA projects.
Material and methods
Description of the NARA datasets
The NARA datasets include only variables that all countries can deliver. They are dynamic minimal datasets currently including 25 variables for hip arthroplasty, 20 for knee arthroplasty and 20 for shoulder arthroplasty. Once a year, we merge updated data from all registers to be used for approved projects. The set of variables are closely reviewed and any changes are discussed in the steering committee.
The NARA dataset include all primary hip, knee and shoulder arthroplasty procedures performed in Norway, Denmark, Sweden and Finland since 1995 for hip procedures, since 1997 for knee procedures, and since 2004 for shoulder procedures. Revision operations are linked to primary procedures in the respective national registries. National data are subsequently anonymized and transferred to the common NARA dataset. In all countries, a revision procedure is defined as a surgical procedure including exchange, removal or addition of any implant component.
Statistical analyses
NARA has published statistical guidelines for the analysis of arthroplasty data in registers. The guidelines are divided into two parts: one with an introduction and a discussion of the background for the guidelines; and one with a more technical statistical discussion on how specific problems can be handled. The first part contains: (1) recommendations for the interpretation of methods used to calculate survival; (2) recommendations on how to deal with bilateral observations; and (3) a discussion of problems and pitfalls associated with analysis of factors that influence survival or comparisons between outcomes extracted from different hospitals.1
The second part addresses methodological issues including recommendations about: (1) competing risk problems; (2) detecting and handling departures from the proportional hazards assumption; (3) bilateral observations; and (4) revision rate ranking.2
The projects performed using NARA data have to a large extent applied these statistical methods. The group is continuously working on the improvement of statistical methods and the application of new ones, including propensity score matching in order to reduce confounding, the multiple imputation method which deals with the problem of missing data and the pseudo value approach when taking death as a competing risk into account in order to assess the relative risk.
Validity methods used in NARA
The Nordic countries are world-leading in the field of international quality registers. The results derived from Nordic hip, knee and shoulder registers are frequently cited in the international literature and considered to be ‘role models’ for the efforts to initiate similar registries in other countries. Key points for national registries to have success are relatively small size of the countries - 4.5 to 10 million inhabitants - with uniform healthcare systems, and systems to assign unique personal identity numbers to each citizen, enabling unambiguous linkage within and between registers. Regular rigorous validation processes within the participating registers are prerequisites for high data quality.
For national registers to have success, it is also necessary to be able to follow-up all patients to their death, emigration or reoperation, and to link the index operation to all types of complications and outcomes. Ability to link the database to registers such as National Patient Registers, National Cancer Registers, National Registers for Socioeconomic data and National Prescription database are also of high importance.
The validity of registers is one of the most important tasks which each national register is continuously working on. The validity consists of four major aspects, including: (1) coverage of registers is defined as the proportion of hospitals/departments contributing to the registration of cases to the national register out of the total number of hospitals/departments performing arthroplasty procedures in the country; (2) registration completeness of operations in a register is defined as the proportion of arthroplasty operations registered in the database out of the total number of operations performed in the country (where the total number is defined by a combination of data on all procedures reported to the respective National Patient Register and the respective arthroplasty register); (3) registration completeness of variables: although an operation may be reported to the register, it is further important that all variables included in the registration form are reported for each operation; and (4) it is not only important that all variables are reported, but also that the values of these variables are accurately reported. Accuracy of registered variables is defined as the probability that variables registered in the national register are correctly registered and present what is supposed to present.
In practice, all orthopaedic departments in the Nordic countries report to the national registers, including private hospitals. Thus, the coverage of Nordic hospitals in the NARA database is 100%. The registration completeness of arthroplasty procedures in Nordic national registers is compared with the registration completeness in the Nordic patient registers. Registration completeness of primary arthroplasty procedures is in the range of 90% to 98%, and that of revision arthroplasty 85% to 94% in the four countries. However, the Finnish Arthroplasty Register has completeness of only 60% for shoulder arthroplasty due to missing many fracture patients. Up-to-date registration completeness of each register can be found in the most current annual reports.
Review of selected NARA projects
Hip arthroplasty
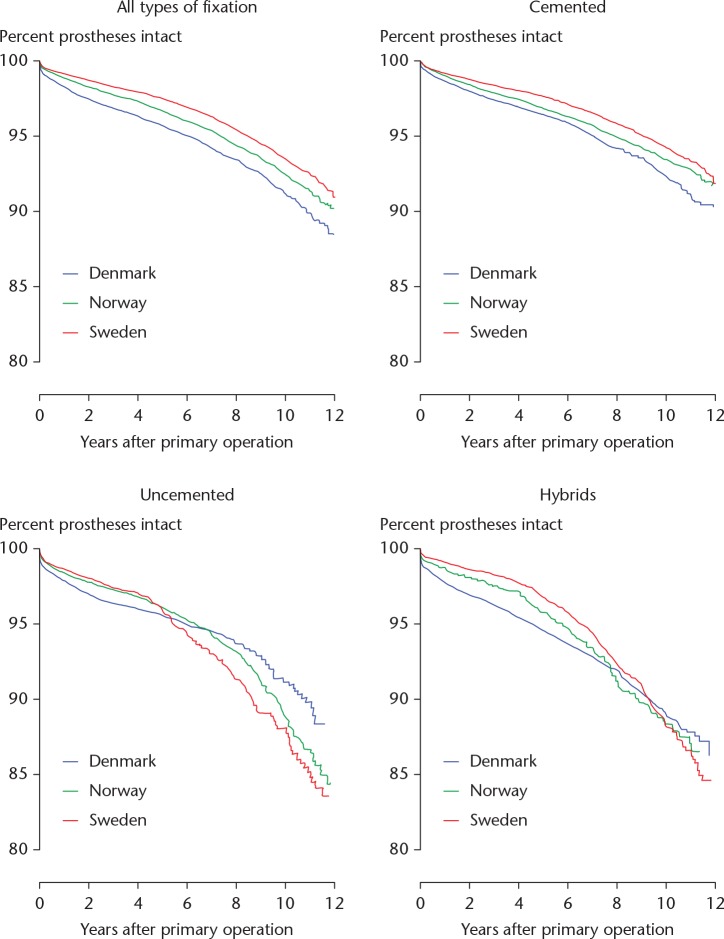
The first peer-reviewed scientific paper from the NARA group was published by Havelin et al. (2009). They assessed 280,201 primary total hip arthroplasty (THA) procedures performed in Sweden, Norway and Denmark from 1995 to 2006. Cemented THAs were used in 46% of patients in Denmark, in 89% of patients in Sweden and in 79% of patients in Norway. Of the 280 201 primary THAs, 9596 (3.4%) had been revised. Calculating ten-year Kaplan–Meier estimates, implant survival was 92% (95% confidence interval (CI) 91.6 to 92.4) in Denmark, 94% (95% CI 93.6 to 94.1) in Sweden and 93% (95% CI 92.3 to 93.0) in Norway (Fig. 1).3
Fig. 1.
Kaplan-Meier estimated curves until revision for any cause, for primary total hip replacements (THAs) in Denmark, Sweden, and Norway 1995–2006. Curves are given for all THAs and also for those classified according to fixation technique as cemented, uncemented, and hybrids (uncemented cup/cemented stem).
Focus on metal-on-metal hip devices
Johanson et al (2010) compared 1638 hip resurfacing arthroplasties in Sweden, Norway and Denmark with 172 554 conventional THA. They found an almost threefold increased revision risk for hip resurfacing arthroplasties (HRA) compared with THA (relative risk (RR) 2.7, 95% CI 1.9 to 3.7), The difference was even greater when HRA was compared with the THA subgroup of cemented THAs (RR 3.8, 95% CI 2.7 to 5.3). For men aged < 50 years, this difference was less pronounced (HRA vs THA: RR 1.9, 95% CI 1.0 to 3.9; HRA vs cemented THA: RR 2.4, 95% CI 1.1 to 5.3), but it was even more pronounced in women of the same age group (HRA vs THA: RR 4.7, 95% CI 2.6 to 8.5; HRA vs cemented THA: RR 7.4, 95% CI 3.7 to 15). The authors concluded that their results did not support continued use of HRA.4
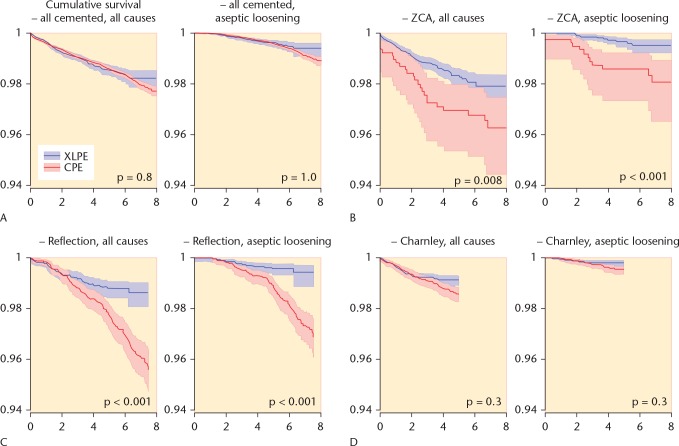
Varnum et al (2015) assessed 32 678 patients who were operated from 2002 through 2010 with cementless stemmed THA with either metal-on-metal bearings (11 567 patients, 35%) or metal-on-polyethylene bearings (21 111 patients, 65%). The cumulative incidence of revision at eight years of follow-up was 7.0% (95% CI 6.0 to 8.1) for metal-on-metal bearings and 5.1% (95% CI 4.7 to 5.6) for metal-on-polyethylene bearings. They concluded that at medium-term follow-up, the survivorship for cementless stemmed metal-on-metal THA was inferior to that for metal-on-polyethylene THA. Further, metal-related problems may cause even higher revision rates for metal-on-metal bearings with longer follow-up (Fig. 2)5.
Fig. 2.
Cumulative incidence for any revision of cementless total hip arthroplasty with metal-on-metal (MoM) bearings and metal-on-polyethylene (MoP) bearings.
Focus on fixation methods of primary THA
Pedersen et al assessed 29 558 primary THRs on patients with osteoarthritis (OA), aged < 55 years, performed from 1995 to 2011 based on the NARA database. They stated that uncemented implants performed better with respect to long-term risk of aseptic loosening in patients aged < 55 years. However, uncemented and hybrid THAs had more short-term revisions compared with cemented implants due to dislocation, periprosthetic fracture and infection.6
Concerning the THA fixation in elderly patients, Mäkelä et al assessed 347 899 THRs performed during 1995 to 2011 based on the NARA database. They found that the proportion of total hip replacements using uncemented implants increased rapidly towards the end of the study period. The ten-year survival of cemented implants in patients aged 65 to 74 years and ⩾ 75 years (93.8%, 95% CI 93.6 to 94.0 and 95.9%, 95% CI 95.8 to 96.1, respectively) was higher than that of uncemented (92.9%, 95% CI 92.3 to 93.4 and 93.0%, 95% CI 91.8 to 94.0), hybrid (91.6%, 95% CI 90.9 to 92.2 and 93.9%, 95% CI 93.1 to 94.5) and reverse hybrid (90.7%, 95% CI 87.3 to 93.2 and 93.2%, 95% CI 90.7 to 95.1) implants. During the first six months, the risk of revision with cemented implants was lower than with all other types of fixation in all age groups. They concluded that implant survival for cemented implants was higher compared with uncemented implants in patients aged ⩾ 65 years. The increased use of uncemented implants in this age group identified in the NARA countries was not supported by these results.7
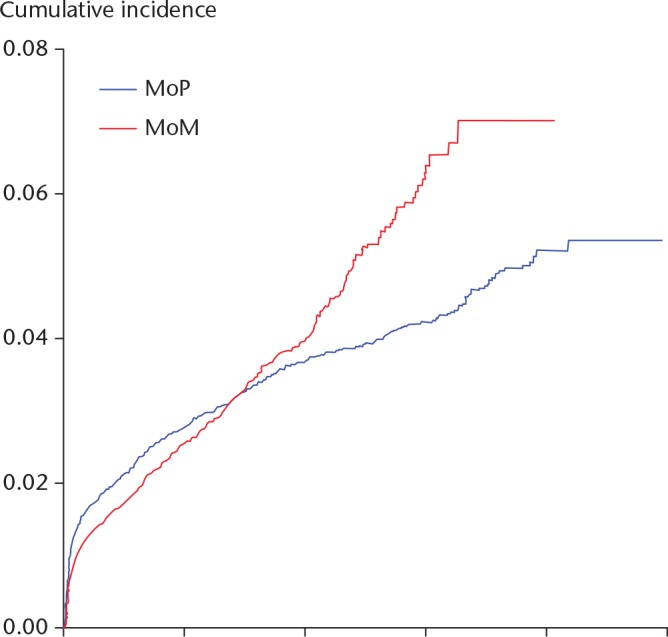
The association between hydroxyapatite (HA) coating and revision risk has been investigated for both acetabular and femoral components. Hailer et al found that the presence of HA coating on the femoral stem did not alter risk of stem revision due to aseptic loosening (hazard ratio (HR) 0.8, 95% CI 0.5 to 1.3). They concluded that uncemented HA-coated stems had similar results to those of uncemented stems with porous coating and rough sand-blasted stems. The use of HA coating on stems that were available both with and without this surface treatment had no clinically relevant effect on their outcome (Fig. 3).8 Lazarinis et al investigated three different cup types with or without HA coating that were inserted due to OA (n = 28 605). Thirteen-year survival for cup revision due to aseptic loosening was 97.9% (95% CI 96.5 to 99.4) for uncoated and 97.8% (95% CI 96.3 to 99.4) for HA-coated cups. Since HA-coated cups had a similar risk of aseptic loosening as uncoated cups, the authors suggested the use of HA coating does not confer any added value in terms of implant stability.9
Fig. 3.
Survival of non-HA-coated and HA-coated Bimetric stems for females aged 60–74 with a diagnosis of osteoarthritis, with the endpoint stem revision for aseptic loosening in an adjusted Cox regression model.
Focus on total joint infections
Dale et al assessed THAs revised due to infection from 1995 to 2009. In total, 2778 (0.6%) of the primary THAs were revised due to infection. Compared with the period 1995 to 1999, the risk of revision due to infection was 1.1 (95% CI 1.0 to 1.2) in 2000 to 2004 and 1.6 (95% CI 1.4 to 1.7) in 2005 to 2009. No change in risk factors in the NARA dataset could explain this increase. The authors suggested that there has been an actual increase in the incidence of prosthetic joint infections after THA.10
Schrama et al assessed 13 384 patients undergoing THA due to RA and 377 287 patients undergoing THA due to OA from 1995 to 2010. They found a slightly higher overall risk of revision for infection in RA patients than in patients with OA, but the difference was only present after 2001. In THAs with antibiotic-loaded cement, the risk of very early and late infections leading to revision was higher in RA compared with OA patients11.
Focus on periprosthetic fractures of the hip
Thien et al used the NARA database to evaluate whether age, sex, preoperative diagnosis, fixation and implant design influence the risk of revision arthroplasty due to periprosthetic fracture within two years from operation of a primary THR. A total of 325 730 cemented femoral stems and 111 899 uncemented femoral stems inserted from 1995 to 2009 were included. Seven frequently used stems (two cemented stems (Exeter and Lubinus SP II) and five uncemented stems (Bi-Metric, Corail, CLS Spotorno, ABG I, and ABG II)) were specifically studied. The authors observed that the risk for revision due to early periprosthetic fracture increased during the period 2003 to 2009 compared with the period 1995 to 2002, both before and after adjustment for demographic factors and fixation (RR 1.4, 95% CI 1.2 to 1.7). Uncemented implants had more periprosthetic fractures than cemented ones, especially in the older age groups.12
Focus on hip diagnosis
Engesæter et al compared the survival of primary THAs performed during the period 1995 to 2009 due to childhood hip disease (developmental dysplasia of the hip, slipped capital femoral epiphysis, Perthes’ disease) with primary OA. After adjustment for differences in age, sex, and type of fixation of the prosthesis, no difference in the risk of revision was found for primary THAs performed due to paediatric hip diseases and those performed due to primary OA.13
Bergh et al assessed 416 217 hips with primary OA and 11 589 with femoral head necrosis. After adjusting for covariates, the relative risk of revision for any reason was higher in patients with femoral head necrosis for both periods studied (up to two years: RR 1.4, 95% CI 1.3 to 1.5 and 2 to 16 years: RR 1.25, 95% CI 1.1 to 1.4). They concluded that the increased risk persisted over the entire period of observation and that all of the four most common reasons for revision were more frequent in the femoral head necrosis cases.14
Focus on structural indicators
Glassou et al examined if hospital procedure volume was associated with the risk of revision after primary THA in the Nordic countries from 1995 to 2011. This study showed a consistent and strong association between hospital procedure volume and long-term risk of revision after primary THA - primarily based on an association in the large group of cemented THAs. Hospitals with < 50 procedures per year had an increased risk of revision at two, five, ten and 15 years after primary cemented THA. There may also be an association between hospital volume and the risk of revision in uncemented THAs; however, based on this study the association seems less pronounced.15
Five years after the first NARA report on ten-year THA survival, Mäkelä et al reported the 15-year survival for THAs, with the use of any revision as endpoint. In Denmark, it was 86% (95% CI 86 to 87), in Sweden, it was 88% (95% CI 88 to 88), in Norway, it was 87% (95% CI 87 to 87) and in Finland, it was 84% (95% CI 83 to 84). The observed differences with a maximum of 4% were regarded as considerable and could at least partly be explained by different implant selection (Fig. 4).16
Fig. 4.
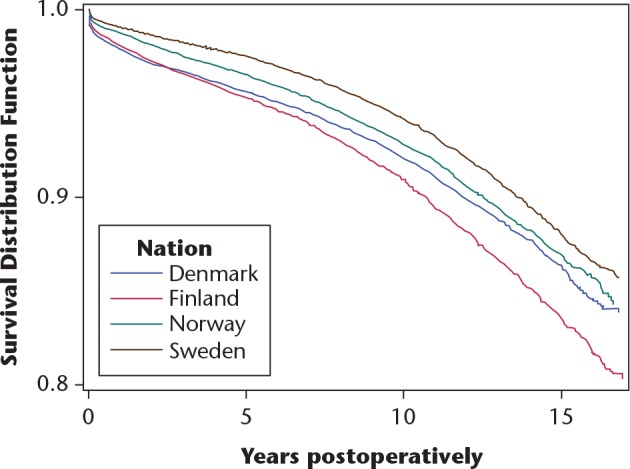
Kaplan-Meier survival for all total hip replacements in the NARA database (by country), with any reason for revision as endpoint.
Focus on methods and implant brands
Wangen et al extracted data on reverse hybrid THAs from 1 January 2000 until 31 December 2013 from the NARA database. A total of 38 415 such hips were studied and compared with cemented THAs. The authors found a higher rate of revision for reverse hybrids than for cemented THAs, with an adjusted relative risk of revision (RR) of 1.4 (95% CI 1.3 to 1.5). At ten years, the survival rate was 94% (95% CI 94 to 95) for cemented THAs and 92% (95% CI 92 to 93) for reverse hybrids. The results for the reverse hybrid THAs were inferior to those for cemented THAs in patients aged ⩾ 55 years (RR 1.1, 95% CI 1.0 to 1.3; p < 0.05). They found a higher rate of early revision due to periprosthetic femoral fracture for reverse hybrids than for cemented THAs in patients aged ⩾ 55 years (RR 3.1, 95% CI 2.2 to 4.5; p < 0.001). The authors concluded that reverse hybrid THAs had a slightly higher rate of revision than cemented THAs in patients aged ⩾ 55. The difference in survival was mainly caused by a higher incidence of early revision due to periprosthetic femoral fracture in the reversed hybrid THAs (Fig. 5).17
Fig. 5.
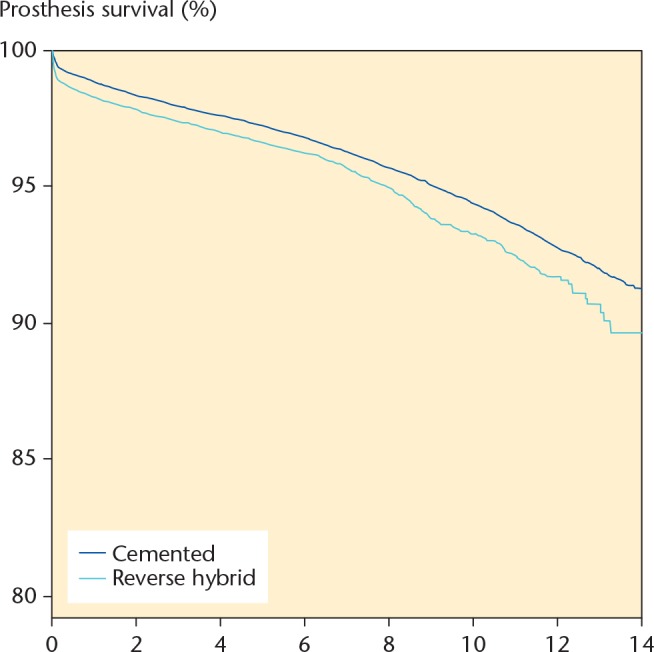
Cox survival analysis with adjustment for age, sex, time period, and diagnosis, and with any revision of the implant as endpoint. RR = 1.4 (CI: 1.3 to 1.5; p < 0.001).
Junnila et al performed a brand-level comparison of cemented THAs based on the NARA database. They found that Spectron EF THA (89.9% (95% CI 89.3 to 90.5)) and Elite THA (89.8% (95% CI 89.0 to 90.6)) had the lowest ten-year survivorship. Lubinus (95.7% survival, 95% CI 95.5 to 95.9), MS 30 (96.6%, 95% CI 95.8 to 97.4) and C-stem THA (95.8%, 95% CI 94.8 to 96.8) had a ten-year survivorship of at least 95%. Lubinus (RR 0.77, 95% CI 0.73 to 0.81), Müller (RR 0.83, 95% CI 0.70 to 0.99), MS-30 (RR 0.73, 95% CI 0.63 to 0.86), C-stem (RR 0.70, 95% CI 0.55 to 0.90) and Exeter Duration THA (RR 0.84, 95% CI 0.77 to 0.90) had a lower risk of revision than Charnley THA, the reference implant. The authors concluded that the Spectron EF THA and the Elite THA had a lower implant survival than the Charnley, Exeter and Lubinus THAs. Implant survival of the Müller, MS 30, CPT and C-stem THAs was above the acceptable limit for ten-year survival.18
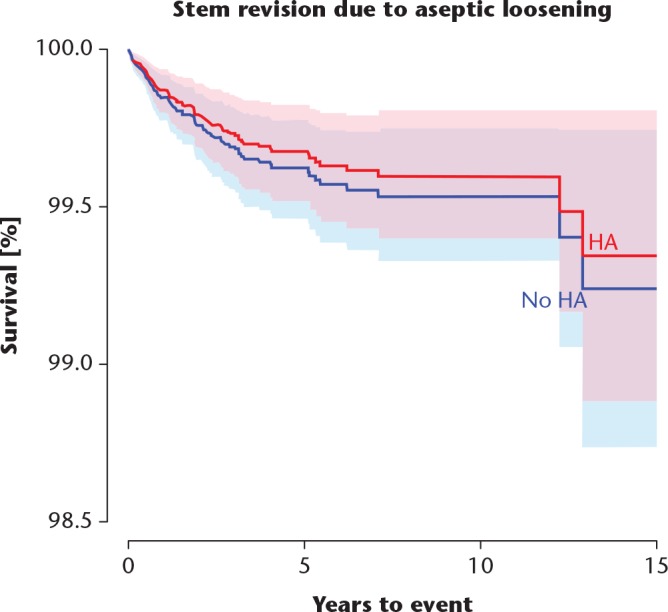
Johanson et al compared the risk of cup and/or liner revision for specific cup and liner designs made of either cross-linked polyethylene (XLPE) or conventional polyethylene (CPE), regarding revision for any reason and revision due to aseptic loosening and/or osteolysis. They found that the CPE version of the ZCA cup had a risk of revision for any reason similar to that of the XLPE version (p = 0.09) but showed a sixfold higher risk of revision for aseptic loosening (p < 0.001). The CPE version of the Reflection All Poly cup had an eightfold elevated risk of revision for any reason (p < 0.001) and a fivefold increased risk of revision for aseptic loosening (p < 0.001). The Charnley Elite Ogee/Marathon cup and the Trilogy cup did not show such differences. The authors concluded that whether XLPE has any advantage over CPE regarding revision risk may depend on the properties of the polyethylene materials being compared, as well as the respective cup designs, fixation type and follow-up times (Fig. 6).19
Fig. 6.
Kaplan-Meier cumulative survival curves with 95% confidence intervals for all cemented designs (panel A), ZCA (B), Reflection All Poly (C), and Charnley Elite Ogee/Marathon (D) cups. The follow-up time ended when there were 100 cases at risk in the smallest group (always XLPE). P-values from log-rank test.
Knee arthroplasty
Robertsson et al published the first peer-reviewed study based on the NARA knee dataset, comparing the national knee registers in terms of patient characteristics, diagnostic indication for the surgeries and operation techniques. The study showed considerable differences between the countries. Norway had the lowest number of procedures per hospital: less than half that of Sweden and Denmark. The preferences for implant brands varied and only three total brands, and one unicompartmental brand, were common in all three countries. Use of the patellar button for total knee arthroplasty (TKA) was popular in Denmark (76%) but not in Norway (11%) or Sweden (14%). Uncemented or hybrid fixation of components was also more frequent in Denmark (22%) than in Norway (14%) and Sweden (2%). The authors concluded that further classification and standardization work was needed to permit more elaborate studies.20
Niemeläinen et al compared the incidences of knee arthroplasty among the four Nordic countries. Using the NARA database, they analysed the differences between age and sex groups. They included patients aged > 30 years who were operated with TKA or unicompartmental knee arthroplasty (UKA) during the period 1997 to 2012. The average annual increase in the incidence of TKA was statistically significant in all countries. The incidence of TKA was higher in women than in men in all four countries. It was highest in Finland in patients aged ⩾ 65 years. At the end of the study period in 2012, Finland’s total incidence was double that of Norway, 1.3 times that of Sweden and 1.4 times that of Denmark. The incidence was lowest in the youngest age groups (< 65 years) in all four countries. The proportional increase in incidence was highest in patients who were aged < 65 years. The authors concluded that the incidence of knee arthroplasty steadily increased in the four countries over the study period. The differences between the countries were considerable, with the highest incidence being in Finland. Patients aged ⩾ 65 years contributed to most of the total incidence of knee arthroplasty.21
Badawy et al assessed 14 496 cases of cemented medial Oxford III UKA in 126 hospitals in the four countries from 2000 to 2012. Hospitals were divided by quartiles into four annual procedure volume groups (⩽ 11, 12 to 23, 24 to 43 and ⩾ 44). They concluded that low volume hospitals performing ⩽ 11 Oxford III UKAs per year were associated with an increased risk of revision compared with higher volume hospitals, and unexplained pain as the revision cause was more common in low volume hospitals.22
Shoulder arthroplasty
The first peer-reviewed publication based on the NARA shoulder database was presented by Rasmussen et al. This study presented the successful merge of data from the Nordic national registers into one common dataset; however, the set of details was reduced. They found considerable differences between Sweden, Denmark and Norway regarding the incidence and demographics of shoulder arthroplasty. For example, the average incidence in the studied period was different, with 13.3/100 000 per year in Denmark, 7.1/100 000 in Norway and 9.1/100 000 in Sweden (p < 0.001). The proportion of women was 66% in Sweden, 69% in Denmark and 72% in Norway (p < 0.001). The mean age was 69 years in Denmark and Sweden and 70 years in Norway (p < 0.001).23
Recently, Rasmussen et al found that resurfacing shoulder hemi-arthroplasty and stemmed hemi-arthroplasty had an increased risk of revision compared with anatomical total shoulder arthroplasty.24 Lehtimäki et al found further that the overall mid-term risk of revision after reverse shoulder arthroplasty for rotator cuff tear arthropathy was low (5%). The most common reason for early revision was infection. Male sex was associated with a significantly increased risk of revision.25
Overall
Currently there are 31 published peer-reviewed research papers based on NARA databases. Twenty manuscripts have either been submitted or are in preparation, with a focus on, for example, dual mobility THA devices, revision due to dislocation after THA, and duration of thromboprophylaxis and THA mortality study with included co-morbidity data. In addition, a collaboration project with the Dutch Arthroplasty Register has been initiated. The amount of peer-reviewed publications based on the NARA hip database is higher than that of the NARA knee database. The harmonization of the NARA knee database has taken longer compared with that of the NARA hip database. The quality of the data in the NARA minimal datasets is as good as the national registers are able to provide. The NARA shoulder dataset is much younger than that in hips and knees; therefore, there are still fewer publications.
Discussion and perspectives
The primary aim of NARA is to improve the quality of research and thereby enhance the possibility for quality improvement with arthroplasty surgery. To assess to what extent NARA has succeeded in this mission is not straightforward. The collaboration has yielded a large body of research addressing clinically relevant questions. Through the respective registers network of orthopaedic surgeons, knowledge generated from these studies have been discussed at local, regional, national and international levels. We strongly believe that this has contributed to several changes in research and clinical practice as exemplified below.
Through our collaboration with regular meetings and networking, the data quality in the respective national registries has improved.26 Thus, a more valid basis for quality monitoring and research has been achieved. Variations in variable definitions and reporting standards have been discussed, resulting in a minimum dataset with common variable definitions and standards for reporting. For example, before NARA, various calculation methods on completeness of registration and revision outcome have been used. Through our internal collaboration, initiatives have been taken in order to improve registration systems in the Danish and Finish registers using experience from Sweden and Norway. The Finish registration system was restructured and the register has passed from a paper-based to an electronic registration system. Currently, implant data are gathered electronically using reference code reading from all hospitals in Finland. A similar system is under reconstruction in Denmark with initial funding from NARA. Thus, a substantial work on harmonization of implant reporting and data collection in general has been done.
NARA collaborates closely with organizations outside the Nordic countries, for example with ISAR (International Society of Arthroplasty Registries), ICOR (International Consortium of Orthopaedic Registries) and NORE (Network Orthopaedic Registries of Europe). NARA also contributes to quality improvement through research projects answering clinically important and up-to-date questions and considerations. Our publications have already significantly affected clinical practice. For example, metal-on-metal THA and resurfacing arthroplasty have been abandoned due to increased revision risk.4,5 Further, the use of uncemented THA in elderly patients has decreased significantly, at least in Finland.7 NARA projects have further contributed to the education of young researchers and awareness of evidence-based decision-making. The group received a large grant from the NordForsk for the period 2014 to 2016.
Conclusion
In conclusion, the NARA collaboration has been successful because countries were able to agree on a common dataset and variable definitions, and merge data. Most important for the continuous success is respectful open discussions during meetings and the willingness to compromise. In addition, the group has to follow the rules of code of conduct for research integrity. The collaboration was also successful because the group was able to initiate a number of research projects and provide answers to clinically relevant questions. Several specific goals, set up in 2007, have been achieved and new ones have emerged in the meantime.
Footnotes
ICMJE Conflict of interest statement: CR declares payments from Zimmer-Biomet, Depuy, Johnson & Johnson, Swemac, outside the submitted work.
AE declares institutional research funding from Zimmer Biomet and DePuy Synthes and payments from Zimmer Biomet, outside the submitted work.
RH declares payments from Zimmer Biomet, outside the submitted work.
SO declares grants from Zimmer Biomet, Heraeus and payments from Johnson & Johnson, outside the submitted work.
All other authors declare no conflict of interest.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Ranstam J, Kärrholm J, Pulkkinen P, et al. ; NARA study group. Statistical analysis of arthroplasty data. I. Introduction and background. Acta Orthop 2011;82:253-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ranstam J, Kärrholm J, Pulkkinen P, et al. ; NARA study group. Statistical analysis of arthroplasty data. II. Guidelines. Acta Orthop 2011;82:258-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Havelin LI, Fenstad AM, Salomonsson R, et al. The Nordic Arthroplasty Register Association: a unique collaboration between 3 national hip arthroplasty registries with 280,201 THRs. Acta Orthop 2009;80:393-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johanson PE, Fenstad AM, Furnes O, et al. Inferior outcome after hip resurfacing arthroplasty than after conventional arthroplasty. Evidence from the Nordic Arthroplasty Register Association (NARA) database, 1995–2007. Acta Orthop 2010;81:535-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Varnum C, Pedersen AB, Mäkelä K, et al. Increased risk of revision of cementless stemmed total hip arthroplasty with metal-on-metal bearings. Acta Orthop 2015;86:491-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pedersen AB, Mehnert F, Havelin LI, et al. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age. Results from the Nordic Arthroplasty Register Association. Osteoarthritis Cartilage 2014;22:659-667. [DOI] [PubMed] [Google Scholar]
- 7. Mäkelä KT, Matilainen M, Pulkkinen P, et al. Failure rate of cemented and uncemented total hip arthroplasty: a register study of combined Nordic database of four nations. BMJ 2014;348:f7592. [DOI] [PubMed] [Google Scholar]
- 8. Hailer N, Lazarinis S, Mäkelä KT, et al. Hydroxyapatite coating does not improve uncemented stem survival after total hip arthroplasty! Acta Orthop 2015;86:18-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lazarinis S, Mäkelä KT, Eskelinen A, et al. Does hydroxyapatite coating of uncemented cups improve long-term survival? An analysis of 28,605 primary total hip arthroplasty procedures from the Nordic Arthroplasty Register Association (NARA). Osteoarthritis Cartilage 2017;25:1980-1987. [DOI] [PubMed] [Google Scholar]
- 10. Dale H, Fenstad AM, Hallan G, et al. Increasing risk of prosthetic joint infection after total hip arthroplasty. Acta Orthop 2012;83:449-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schrama J, Fenstad AM, Dale H, et al. Increased risk of revision for infection in rheumatoid arthritis patients with total hip replacements. Acta Orthop 2015;86:469-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Thien T, Chatziagorou G, Garellick G, et al. Periprosthetic fracture within 2 years after THR. Analysis of 437629 operations in the Nordic Arthroplasty Registry Assiciation database. J Bone Joint Surg [Am] 2014;96-A:e167. [DOI] [PubMed] [Google Scholar]
- 13. Engesæter LB, Engesæter IO, Fenstad AM, et al. Low revision rate after total hip arthroplasty in patients with pediatric hip diseases. Acta Orthop 2012;83:436-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bergh C, Fenstad AM, Furnes O, et al. Increased risk of revision in patients with non-traumatic femoral head necrosis. Acta Orthop 2014;85:11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glassou EN, Hansen TB, Mäkelä K, et al. Association between hospital procedure volume and risk of revision after total hip arthroplasty: a population-based study within the Nordic Arthroplasty Register Association database. Osteoarthritis Cartilage 2016;24:419-426. [DOI] [PubMed] [Google Scholar]
- 16. Mäkelä K, Matilainen M, Pulkkinen P, et al. Countrywise results of total hip arthroplasty – an analysis of 438,733 hips based on the Nordic Arthroplasty Register Association database. Acta Orthop 2014;85:107-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wangen H, Havelin LI, Fenstad AM, et al. Reverse hybrid total arthroplasty - results from the Nordic Arthroplasty Register Association. Acta Orthop 2017;88:248-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Junnila M, Laaksonen I, Eskelinen A, et al. Implant survival of the most common cemented total hip devices from the Nordic Arthroplasty Register Association database. Acta Orthop 2016;87:546-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johanson PE, Furnes O, Havelin IL, et al. Outcome in design-specific comparisons between highly crosslinked and conventional polyethylene in total hip arthroplasty. Acta Orthop 2017;88:363-369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Robertsson O, Bizjajeva S, Fenstad AM, et al. Knee arthroplasty in Denmark, Norway and Sweden. A pilot study from the Nordic Arthroplasty Register Association. Acta Orthop 2010;81:82-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Niemeläinen M, Mäkelä K, Robertsson O, et al. Different incidences of knee arthroplasty in the Nordic countries. Acta Orthop 2017;88:173-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Badawy M, Fenstad AM, Bartz-Johannessen CA, et al. Hospital volume and the risk of revision in Oxford unicompartmental knee arthroplasty in the Nordic countries. –an observational study of 14 496. BMC Musculoskelet Disord 2017;18:388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rasmussen JV, Brorson S, Hallan G, et al. Is it feasible to merge data from national shoulder registries? A new collaboration within the Nordic Arthroplasty Register Association. J Shoulder Elbow Surg 2016;25:e369-e377. [DOI] [PubMed] [Google Scholar]
- 24. Rasmussen JV, Hole R, Metlie T, et al. Anatomical total shoulder arthroplasty used for glenohumeral osteoarthritis has higher survival rates than hemiarthroplasty: a Nordic registry-based study. Osteoarthritis Cartilage 2018;26:659-665. [DOI] [PubMed] [Google Scholar]
- 25. Lehtimäki K, Rasmussen JV, Mokka J, et al. Risk and risk factors for revision after primary reverse shoulder arthroplasty for cuff tear arthropathy and osteoarthritis: a Nordic Arthroplasty Register Association study. J Shoulder Elbow Surg 2018;27:1596-1601. [DOI] [PubMed] [Google Scholar]
- 26. No authors. https://thl.fi/far/#index. FAR open access reporting pages (date last accessed 5 March 2019).