Abstract
Objective
Postoperative pain following hip surgery can be severe. Non-steroidal anti-inflammatory drugs are used in the treatment of postoperative pain to reduce opioid consumption. Our aim was to investigate the effect of ibuprofen on postoperative opioid consumption following total hip replacement surgery.
Methods
Patients undergoing elective total hip replacement under general anaesthesia were included into this randomised, prospective and double-blind study. Forty patients classified according to the American Society of Anesthesiologists as Class I and II were randomised to receive 800 mg ibuprofen intravenously (IV) every 6 hours, or placebo. At the end of surgery, all patients were also administered tramadol 100 mg IV and paracetamol 1 gm IV. In the postoperative period, all patients were provided with a morphine PCA device. The PCA device was set to deliver 1 mg bolus dose and had 8 minutes of lockout period and 6 mg 1-hour limit. VAS scores were recorded at 1, 6, 12 and 24 h postoperatively. The incidence of nausea and vomiting, total morphine consumption during the 24 h postoperative period was recorded. The Mann-Whitney U and chi-squared tests were used for statistical analysis.
Results
The VAS score at postoperative 24 h was lower in the ibuprofen group (p=0.006). Morphine consumption at 24 hours was significantly lower at the ibuprofen group compared to the control group (p=0.026) (the mean doses were 16 mg and 24 mg, respectively). Five patients in the control group and 3 patients in the ibuprofen group reported vomiting. No other side effects or complications were observed.
Conclusion
Following total hip replacement surgery, the administration of ibuprofen IV significantly reduced morphine consumption.
Keywords: Ibuprofen, postoperative pain management, total hip replacement
Introduction
Total hip replacement surgery results in severe postoperative pain. Different medications and regional anaesthesia techniques can be used to treat postoperative pain. Multimodal analgesia is defined as the simultaneous use of different classes or modes of analgesics that modulate different pathways and receptors to provide superior pain control (1).
Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID), and its oral form is well known and has a long history of use. The intravenous (IV) form of ibuprofen is relatively new, first approved in 2009, and it has been used to treat both fever and pain (2). Along with opioids, NSAIDs form the cornerstone of pharmacotherapy for the postoperative pain. Moreover, the use of NSAIDs as a multimodal pain management approach has been shown to reduce the opioid consumption and minimise the most feared side effects of opioids, such as respiratory depression and emetic events (3, 4). This prospective, double-blind study was designed to evaluate the efficacy and safety of IV ibuprofen in the treatment of postoperative pain in patients undergoing elective total hip replacement.
Methods
A prospective, double-blind, placebo-controlled study design was used. After obtaining an approval from Kocaeli City Clinical Trials Ethical Comittee (KÜ GOKAEK 2016-189) and written informed consent, we studied 40 patients classified according to the American Society of Anesthesiologists as Class I and II (Figure 1), aged 18–70 years, undergoing elective unilateral total hip replacement surgery under general anaesthesia. Exclusion criteria were the history of allergy or hypersensitivity to any component of NSAIDs, having a renal or hepatic disease, patients with significant cognitive impairment, recent use of opioids, corticosteroids or any analgesic drug.
Figure 1.
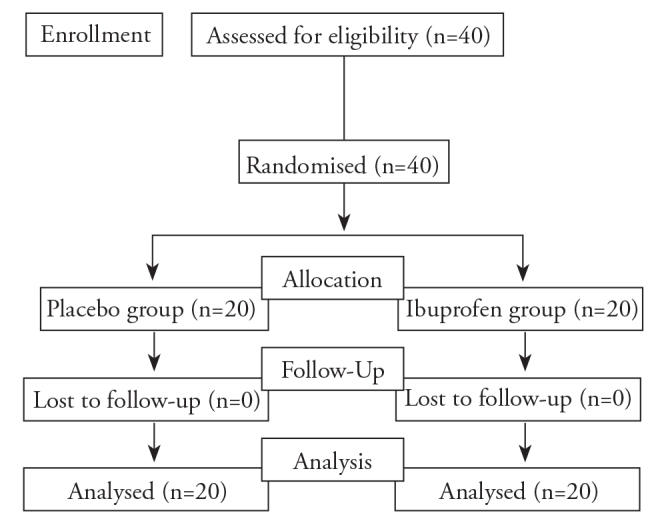
CONSORT flow diagram of study
Randomisation was performed according to computer-generated random number tables, and allocation to a treatment group was done using the sealed-opaque-envelope technique. According to randomisation, patients were divided in two groups to receive either 800 mg IV ibuprofen every 6 hours or placebo.
General anaesthesia was induced with 2–3 mg kg−1 of propofol, 2 μg kg−1 of fentanyl, and rocuronium 0.6 mg kg−1 IV, and it was maintained with desflurane in 60% N20/40% oxygen. At the end of the surgery, all patients received tramadol 100 mg IV, paracetamol 1 gm IV, ondansetron 8 mg IV and ranitidine 50 mg IV.
The first dose of study drug was administered 30 minutes before the end of the surgery, and three subsequent doses were administered every 6 hours within the first 24 hours. In the postoperative period, all patients were provided with a morphine patient-controlled analgesia device (PCA). The PCA device was set to deliver 1 mg bolus dose and had 8 minutes of lockout period and 6 mg 1-hour limit.
Visual analogue scale (VAS) scores for pain (VAS 0=no pain, VAS 10=most severe pain possible) and morphine consumption doses were recorded at 1, 6, 12 and 24 h postoperatively. A blinded pain nurse performed postoperative follow-up of patients. The incidence of nausea and vomiting during the 24 h postoperative period was also recorded.
A preliminary study on the same surgical population in our clinic showed that the mean (SD) morphine consumption in the postoperative 24 h was 25 mg (±9). For the 90% power and an error of 0.05, the sample size necessary to detect a 30% difference in postoperative morphine requirement using IV ibuprofen compared to control group was 18 subjects per group. We included 20 patients in each group to increase the power of the study and also to secure patients’ dropouts for any reason.
Statistical analysis
Was performed using the Statistical Package for the Social Sciences software version 15 (SPSS Inc.; Chicago, IL, USA). Demographic data are presented as mean (SD). Numerical data are presented as median (25.–75. percentiles). A p-value of 0.05 was considered to be statistically significant. The Kolmogorov-Smirnov test was used for normality. The Mann-Whitney U test was used for comparison of VAS scores in movement and morphine consumption between two groups. For comparison of side effects such as nausea and vomiting, a chi-squared test was performed.
Results
A total of 40 patients were recruited. There were no significant differences between the two groups in demographics such as the ASA scores, age, gender, or weight (Table 1).
Table 1.
Demographic data
| Placebo group (n=20) | Ibuprofen group (n=20) | p | |
|---|---|---|---|
|
| |||
| Age (year) | 49±10 | 49±14 | 0.847 |
| Weight (kg) | 78±17 | 77±15 | 0.813 |
| Gender (M/F) | 7/13 | 5/15 | 0.730 |
| ASA status (I/II) | 9/11 | 9/11 | 1.000 |
| Duration of surgery (min) | 128±26 | 141±33 | 0.231 |
Data are presented as the mean±SD and patient numbers
Efficacy
The objective of this study was to determine the efficacy of IV ibuprofen compared with placebo in the treatment of postoperative pain during the first 24 hours following surgery using the VAS score for pain and comparing morphine consumption. Patients receiving IV ibuprofen experienced a significant decrease from the placebo group in the mean VAS (p=0.006) (Table 2) and a 32% decrease in the mean morphine consumption (p=0.026) for the postoperative 24h period (Table 3).
Table 2.
Visual analogue scale scores for pain
| Placebo group (n=20) | Ibuprofen group (n=20) | p | |
|---|---|---|---|
|
| |||
| 1st hour | 5±1.75 | 5 ±2.06 | 0.650 |
| 3rd hour | 4±2.22 | 3 ±2.23 | 0.781 |
| 6th hour | 3±1.97 | 2 ±1.72 | 0.235 |
| 12th hour | 3±1.92 | 1 ±2.52 | 0.070 |
| 24th hour | 2±2.25 | 1 ±1.05* | 0.006 |
Data are presented as the mean±SD.
There was only a statistically significant difference for VAS scores at the 24th hour.
Table 3.
Morphine consumption in the first postoperative 24 hours
| Placebo group (n=20) | Ibuprofen group (n=20) | p | |
|---|---|---|---|
|
| |||
| 1st hour | 2.00±2.21 | 1.07±1.32 | 0.084 |
| 3rd hour | 6.43±4.23 | 4.75±4.43 | 0.277 |
| 6th hour | 9.63±5.53 | 6.91±5.80 | 0.118 |
| 12th hour | 14.86±9.42 | 12.22±9.66 | 0.265 |
| 24th hour | 21.93±11.35 | 14.90±9.33* | 0.026 |
Morphine consumption was statistically significant at the 24th hour.
Safety
Five patients in both groups had nausea. 3 patients in ibuprofen group and 5 patients in placebo group had vomiting.
Discussion
The inadequate treatment of postoperative pain has profound and long-lasting implications and increases the postoperative morbidity (5). The use of agents with different analgesic mechanisms may result in synergistic effects and produce greater efficacy. In addition, the synergism between these agents allow us to use lower doses of each respective agent, limiting dose-related adverse effects such as respiratory depression, nausea and vomiting, which may cause great discomfort (6). Ibuprofen is a well-known NSAID, but the IV form is relatively new, and studies on the treatment of postoperative pain are limited.
The oral use of ibuprofen has been shown to reduce the postoperative morphine consumption 45% in the patients undergo primary hip arthroplasty under spinal anaesthesia than those receiving placebo (7). In that study, patients were observed only for 5 hours. Likewise, in another study, patients went through orthopaedic surgery receiving IV ibuprofen used 30.9% less morphine than those receiving placebo (8). In this study, different orthopaedic surgeries were included. In another study, 800 mg IV ibuprofen was compared with placebo for acute postoperative pain after orthopaedic or abdominal surgeries (9). Studies in the literature have reported that the administration of other NSAIDs reduced opioid consumption and opioid related side effects in patients undergoing major orthopaedic surgeries (10, 11).
To the best of our knowledge, this is the first randomised controlled trial to assess the efficacy of IV ibuprofen in postoperative pain management in a specific major orthopaedic surgery. In our study, the administration of 800 mg IV ibuprofen every 6 hours in the postoperative period reduced 24-hour opioid consumption with a 32% decrease and was effective in the emergence of lower pain scores in the postoperative period.
Like other NSAIDs, ibuprofen may cause gastrointestinal side effects. NSAIDs are related with an increased risk for serious cardiovascular side effects and should be used with caution in patients with congestive heart failure and renal impairment (12). In our study, none of our patients had gastrointestinal side effects.
Although ibuprofen decreased opioid consumption for 32%, and the incidence of vomiting in the ibuprofen group was lower compared to the control group, this decrease did not reach statistical significance. Larger scale studies are needed to detect a potential benefit of ibuprofen to prevent nausea and vomiting. None of our patients had any cardiac or renal adverse effects observed in both groups.
Although NSAIDs may have a possible influence on bone healing, there is no consensus regarding the safety of NSAIDs following orthopaedic procedures. Marquez-Lara et al. (13) recommended that withholding these medications does not have any proven scientific benefit to patients and may cause harm by increasing narcotic requirements. We believe that the NSAIDs impact on bone healing and postoperative pain management should be the subject of future studies.
Conclusion
In this prospective randomised study, we have shown that the administration of 800 mg IV ibuprofen every 6 hours in the postoperative period reduced both pain scores and morphine consumption following total hip replacement surgery.
Footnotes
This study was presented at 36th Annual ESRA Congress, Lugano, Switzerland, 13–16 September 2017- poster presentation
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Kocaeli City Clinical Trials (KÜ GOKAEK 2016-189).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Y.G., H.U.Y.; Design - Y.G., H.U.Y.; Supervision - Y.G., A.K.; Resources - Y.G., H.U.Y.; Materials - H.U.Y., E.I.; Data Collection and/or Processing - H.U.Y., E.I.; Analysis and/or Interpretation - Y.G., H.U.Y., E.I., A.K.; Literature Search - Y.G., H.U.Y., A.K.; Writing Manuscript - H.U.Y., Y.G.; Critical Review - Y.G., H.U.Y., E.I., A.K.; Other - Y.G., H.U.Y., E.I., A.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–40. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 2.Scott LJ. Intravenous ibuprofen: in adults for pain and fever. Drugs. 2012;72:1099–109. doi: 10.2165/11209470-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 3.Buvanendran A, Kroin JS. Multimodal analgesia for controlling acute postoperative pain. Curr Opin Anaesthesiol. 2009;22:588–93. doi: 10.1097/ACO.0b013e328330373a. [DOI] [PubMed] [Google Scholar]
- 4.Carr DB, Gordas LC. Acute pain. Lancet. 1999;353:2051–8. doi: 10.1016/S0140-6736(99)03313-9. [DOI] [PubMed] [Google Scholar]
- 5.Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117(Suppl 3):iii62–iii72. doi: 10.1093/bja/aew362. [DOI] [PubMed] [Google Scholar]
- 6.Martinez V, Beloeil H, Marret E, Fletcher D, Ravaud P, Trinquart L. Non-opioid analgesics in adults after major surgery: systematic review with network meta-analysis of randomized trials. Br J Anaesth. 2017;118:22–31. doi: 10.1093/bja/aew391. [DOI] [PubMed] [Google Scholar]
- 7.Dahl V, Raeder JC, Drøsdal S, Wathne O, Brynildsrud J. Prophylactic oral ibuprofen or ibuprofen-codeine versus placebo for postoperative pain after primary hip arthroplasty. Acta Anaesthesiol Scand. 1995;39:323–6. doi: 10.1111/j.1399-6576.1995.tb04070.x. [DOI] [PubMed] [Google Scholar]
- 8.Singla N, Rock A, Pavliv L. A multi-center, randomized, double-blind placebo-controlled trial of intravenous-ibuprofen (IV-ibuprofen) for treatment of pain in post-operative orthopedic adult patients. Pain Med. 2010;11:1284–93. doi: 10.1111/j.1526-4637.2010.00896.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gago Martínez A, Escontrela Rodriguez B, Planas Roca A, Martínez Ruiz A. Intravenous Ibuprofen for Treatment of Post-Operative Pain: A Multicenter, Double Blind, Placebo-Controlled, Randomized Clinical Trial. PLoS One. 2016;11:e0154004. doi: 10.1371/journal.pone.0154004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onda A, Ogoshi A, Itoh M, Nakagawa T, Kimura M. Comparison of the effects of treatment with celecoxib, loxoprofen, and acetaminophen on postoperative acute pain after arthroscopic knee surgery: A randomized, parallel-group trial. J Orthop Sci. 2016;21:172–7. doi: 10.1016/j.jos.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Oreskovic Z, Bicanic G, Hrabac P, Tripkovic B, Delimar D. Treatment of postoperative pain after total hip arthroplasty: comparison between metamizol and paracetamol as adjunctive to opioid analgesics-prospective, double-blind, randomised study. Arch Orthop Trauma Surg. 2014;134:631–6. doi: 10.1007/s00402-014-1979-7. [DOI] [PubMed] [Google Scholar]
- 12.Gilron I, Milne B, Hong M. Cyclooxygenase-2 inhibitors in postoperative pain management: current evidence and future directions. Anesthesiology. 2003;99:1198–208. doi: 10.1097/00000542-200311000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Marquez-Lara A, Hutchinson ID, Nuñez F, Jr, Smith TL, Miller AN. Nonsteroidal Anti-Inflammatory Drugs and Bone-Healing: A Systematic Review of Research Quality. JBJS Rev. 2016;4 doi: 10.2106/JBJS.RVW.O.00055. pii: 01874474-201603000-00005. [DOI] [PubMed] [Google Scholar]


