Abstract
Objective
The Acute Physiology and Chronic Health Evaluation (APACHE) severity of disease classification system, which is one of the most widely used scoring systems to predict mortality, is used for intensive care units (ICU) patients. This study aimed to evaluate the predictive ability of APACHE II for mortality in patients after undergoing cardiac surgery. We studied if APACHE II could successfully predict the outcome in post-cardiac surgery patients.
Methods
This study involved retrospective data collection of all adult patients who were admitted to Ordu State Hospital cardiovascular surgery ICU following cardiac surgery from August 2013 to December 2015. Area under the receiver operating characteristic (ROC) curve (AUC) values were calculated for the APACHE II model.
Results
During the two years of data collection, we included 600 patients with a mean age of 64.77±10.148 years. Of these, 180 (30.0%) were females. The ICU mortality rate was 8.33%, and the mean length of ICU stay was 4.210±6.913 days. The mean pre-operative EuroSCORE was 3.890±2.565, and the mean pre-operative APACHE II score was 6.790±3.617. The AUC values for APACHE II and EuroSCORE were 0.743 and 0.767, respectively.
Conclusion
The APACHE II model can be used to predict mortality in a Turkish population of patients who have undergone cardiac surgery.
Keywords: APACHE II, cardiac surgery, EuroSCORE
Introduction
To help physicians objectively judge patients’ conditions, a post-operative scoring system is required. Such a system should support disease severity evaluation and therapeutic decisions (1).
Several pre-operative risk stratification models, such as the ‘additive European System for Cardiac Operative Risk Evaluation’ (EuroSCORE), are in daily use after cardiac surgery. The first such scoring system used after cardiac surgery was the Parsonnet scoring system, which was developed in 1989 (2). EuroSCORE was developed in 1999 and was used for predicting post-operative mortality following open heart surgery (3). EuroSCORE has gained wide acceptance in Europe and in Turkey as it can predict in-hospital mortality after cardiac surgery (4). The use of the EuroSCORE model in the adult Turkish cardiac surgery population is obligatorily practiced by the national health authority and the Turkish Social Security Agency (4).
However, EuroSCORE is limited to pre-operative variables and does not include intra- or post-operative circumstances. The APACHE II model has been developed in intensive care units (ICUs) and been applied in the research and risk stratification of critically ill patients (5, 6). This model uses the lowest values of 12 measured physiological variables during the first 24 h after admission in the ICU, with the evaluation of the patient’s chronic health and the diagnosis at admission, to predict mortality (5). It is simple to calculate this score from data that are routinely available during the first 24 h after admission, and the model has been extensively studied in general ICU populations.
In the present study, we retrospectively analysed the charts of 600 patients who underwent surgery and who were post-operatively admitted to the ICU at Ordu State Hospital. We evaluated the predictive ability of APACHE II in patients following open heart surgery.
Methods
We included 600 consecutive adult patients admitted to the ICU following open heart surgery from August 2013 to December 2015 in our retrospective study. Those who were re-admitted to the ICU were excluded. The study was retrospective and thus did not need approval of the local ethics committee.
The patients were transferred from the operating room directly to the ICU, where they were post-operatively monitored for two days; they were then sent to the recovery ward. No data were missing. All patients signed written informed consent and the study complied with the Declaration of Helsinki.
The APACHE II score was calculated on the first post-operative day. The following data were collected: age; medical history; systolic and mean arterial blood pressure; heart rate; respiratory rate; body temperature; oxygenation; arterial pH; serum sodium, potassium and creatinine levels, haematocrit; white blood cell count; platelet count; and Glasgow Coma Scale score. APACHE II score calculation was based on the lowest values of the above parameters documented during the first 24 h following admission to the ICU.
Statistical analysis
Data obtained analysed using the MedCalc program (MedCalc version 18.6, MedCalc Software bvba). For data evaluation, number, percentage, mean and standard deviation were used. Estimation of the data values was tested by analysis of ROC. P-values of <0.05 were considered significant.
The area under the receiver operating characteristic (ROC) curve (AUC) value was calculated to compare the predictive power. AUC is meaningless for values under 0.7; a value between 0.7 and 0.8 is acceptable, that between 0.8 and 0.9 is very good and that of 0.9 is excellent.
Results
The mean age of the 600 patients was 64.77±10.148 years. Of these, 420 (70.0%) were males and 180 (30.0%) were females. Most patients had undergone isolated coronary artery bypass grafting (400 patients) (66.67%); isolated valve surgery was the second most common procedure that the patients had undergone (88 patients) (14.67%). The descriptive features of the patients are presented in Table 1.
Table 1.
Descriptive features
| Tables | Groups | Frequency (n) | (%) |
|---|---|---|---|
|
| |||
| Gender | M | 420 | 70.0 |
| F | 180 | 30.0 | |
| Total | 600 | 100.0 | |
| Operations | AAR | 40 | 6.7 |
| AVR | 32 | 5.3 | |
| AVR+AAR | 24 | 4.0 | |
| AVR+CABG | 16 | 2.7 | |
| AVR+MVR | 12 | 2.0 | |
| Bentall | 8 | 1.3 | |
| MVR+CABG | 12 | 2 | |
| CABGx1 | 20 | 3.3 | |
| CABGx2 | 88 | 14.7 | |
| CABGx3 | 144 | 24.0 | |
| CABGx4 | 132 | 22.0 | |
| CABGx5 | 16 | 2.7 | |
| MVR | 56 | 9.3 | |
| Total | 600 | 100.0 | |
AAR: ascending aortic replacement; AVR: aortic valve replacement; CABG: coronary artery bypass grafting; F: female; M: male; MVR: mitral valve replacement
The mean length of ICU stay was 4.210±6.913 days, and the mean length of hospital stay was 6.950±4.105 days. Because one patient has stayed in the ICU for 70 days and another for 59 days and as they both died, the mean length of ICU stay was high and may be inconsistent with the discharge duration.
The overall mortality was 8.33%, with the deaths of 50 patients recorded during the study period. The predicted mortality according to EuroSCORE was 11.3%, whereas the predicted mortality according to APACHE II was 10.2%. The difference between the observed and predicted rates was not significant.
Table 2 shows the average of the studied parameters.
Table 2.
Average of the parameters
| N | Minimum | Maximum | Mean | Standard deviation | |
|---|---|---|---|---|---|
|
| |||||
| EuroSCORE | 600 | 0 | 13 | 3.89 | 2.565 |
| APACHE II | 600 | 0 | 18 | 6.79 | 3.617 |
| ICU stay, days | 600 | 0 | 70 | 4.21 | 6.913 |
| Discharge from hospital, days | 600 | 0 | 25 | 6.95 | 4.105 |
| Age, years | 600 | 28 | 88 | 64.77 | 10.148 |
ICU: intensive care unit
The AUC value was 0.743 for APACHE II and 0.767 for EuroSCORE. The results of ROC analysis for APACHE II and EuroSCORE are shown in Figure 1 and Figure 2.
Figure 1.
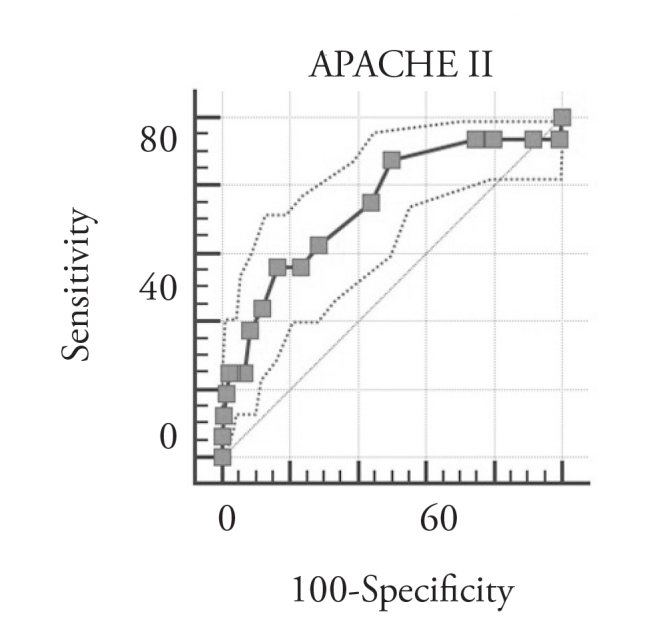
ROC analysis of the APACHE II Score
Figure 2.
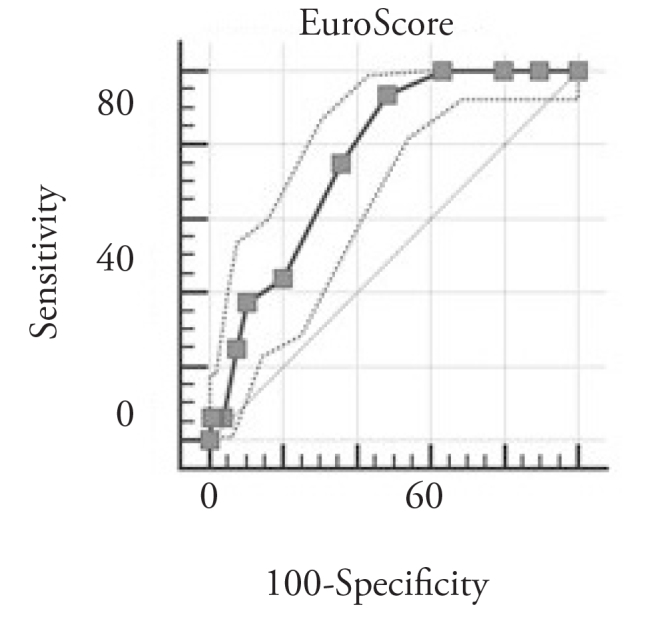
ROC analysis of the EuroSCORE
Table 3 shows the significance of the APACHE II and EuroSCORE ROC curves. The area under the ROC curves was a statistically significant parameter in both APACHE II and EuroSCORE.
Table 3.
Significance of the APACHE II ROC curve
| Area under the ROC curve (AUC) | 0.743 |
| Standard error | 0.0352 |
| 95% confidence interval | 0.706 to 0.778 |
| z statistic | 6.907 |
| P (Area=0.5) | <0.0001 |
| Significance of the EuroSCORE ROC Curve | |
| Area under the ROC curve (AUC) | 0.767 |
| Standard error a | 0.0239 |
| 95% confidence interval b | 0.731 to 0.800 |
| z-statistic | 11.181 |
| P (Area=0.5) | <0.0001 |
Table 4 shows sensitivity and specificity values according to APACHE II score. Table 5 shows sensitivity and specificity values according to EuroSCORE.
Table 4.
Sensitivity and specificity values according to APACHE II scoring criteria and coordinates
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | 95% CI | −LR | 95% CI |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| ≥0 | 100.00 | 94.4–100.0 | 0.00 | 0.0–0.7 | 1.00 | 1.0 | ||
| >0 | 93.75 | 84.8–98.3 | 0.75 | 0.2–1.9 | 0.94 | 0.9–1.0 | 8.38 | 2.1–32.7 |
| >2 | 93.75 | 84.8–98.3 | 8.21 | 6.0–10.9 | 1.02 | 1.0–1.1 | 0.76 | 0.3–2.0 |
| >3 | 93.75 | 84.8–98.3 | 20.15 | 16.8–23.8 | 1.17 | 1.1–1.3 | 0.31 | 0.1–0.8 |
| >4 | 93.75 | 84.8–98.3 | 25.37 | 21.7–29.3 | 1.26 | 1.2–1.4 | 0.25 | 0.09–0.6 |
| >5 | 87.50 | 76.8–94.4 | 50.00 | 45.7–54.3 | 1.75 | 1.5–2.0 | 0.25 | 0.1–0.5 |
| >6 | 75.00 | 62.6–85.0 | 55.97 | 51.7–60.2 | 1.70 | 1.4–2.0 | 0.45 | 0.3–0.7 |
| >7 | 62.50 | 49.5–74.3 | 71.64 | 67.6–75.4 | 2.20 | 1.7–2.8 | 0.52 | 0.4–0.7 |
| >8 | 56.25 | 43.3–68.6 | 76.87 | 73.1–80.4 | 2.43 | 1.9–3.2 | 0.57 | 0.4–0.8 |
| >9 | 56.25 | 43.3–68.6 | 83.58 | 80.2–86.6 | 3.43 | 2.6–4.6 | 0.52 | 0.4–0.7 |
| >10 | 43.75 | 31.4–56.7 | 88.06 | 85.0–90.7 | 3.66 | 2.6–5.3 | 0.64 | 0.5–0.8 |
| >11 | 37.50 | 25.7–50.5 | 91.79 | 89.1–94.0 | 4.57 | 3.0–7.0 | 0.68 | 0.6–0.8 |
| >12 | 25.00 | 15.0–37.4 | 93.28 | 90.8–95.3 | 3.72 | 2.2–6.3 | 0.80 | 0.7–0.9 |
| >13 | 25.00 | 15.0–37.4 | 97.01 | 95.2–98.3 | 8.38 | 4.4–15.9 | 0.77 | 0.7–0.9 |
| >14 | 25.00 | 15.0–37.4 | 97.76 | 96.1–98.8 | 11.17 | 5.5–22.5 | 0.77 | 0.7–0.9 |
| >15 | 18.75 | 10.1–30.5 | 98.51 | 97.1–99.4 | 12.56 | 5.3–29.6 | 0.82 | 0.7–0.9 |
| >16 | 12.50 | 5.6–23.2 | 99.25 | 98.1–99.0 | 16.75 | 5.2–54.1 | 0.88 | 0.8–1.0 |
| >17 | 6.25 | 1.7–15.2 | 100.00 | 99.3–100.0 | 0.94 | 0.9–1.0 | ||
| >18 | 0.00 | 0.0–5.6 | 100.00 | 99.3–100.0 | 1.00 | 1.0 | ||
Table 5.
Sensitivity and specificity values according to euroscore criteria and coordinates
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | 95% CI | −LR | 95% CI |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| ≥0 | 100.00 | 94.4–100.0 | 0.00 | 0.0–0.7 | 1.00 | 1.0–1.0 | ||
| >0 | 100.00 | 94.4–100.0 | 10.45 | 8.0–13.4 | 1.12 | 1.1–1.1 | 0.00 | |
| >1 | 100.00 | 94.4–100.0 | 20.15 | 16.8–23.8 | 1.25 | 1.2–1.3 | 0.00 | |
| >2 | 100.00 | 94.4–100.0 | 36.57 | 32.5–40.8 | 1.58 | 1.5–1.7 | 0.00 | |
| >3 | 93.75 | 84.8–98.3 | 51.49 | 47.2–55.8 | 1.93 | 1.7–2.2 | 0.12 | 0.05–0.3 |
| >4 | 75.00 | 62.6–85.0 | 64.18 | 60.0–68.2 | 2.09 | 1.7–2.5 | 0.39 | 0.3–0.6 |
| >5 | 43.75 | 31.4–56.7 | 79.85 | 76.2–83.2 | 2.17 | 1.6–3.0 | 0.70 | 0.6–0.9 |
| >6 | 37.50 | 25.7–50.5 | 89.55 | 86.6–92.0 | 3.59 | 2.4–5.4 | 0.70 | 0.6–0.8 |
| >7 | 25.00 | 15.0–37.4 | 92.54 | 90.0–94.6 | 3.35 | 2.0–5.6 | 0.81 | 0.7–0.9 |
| >8 | 6.25 | 1.7–15.2 | 96.27 | 94.3–97.7 | 1.67 | 0.6–4.7 | 0.97 | 0.9–1.0 |
| >9 | 6.25 | 1.7–15.2 | 98.51 | 97.1–99.4 | 4.19 | 1.3–13.5 | 0.95 | 0.9–1.0 |
| >10 | 6.25 | 1.7–15.2 | 99.25 | 98.1–99.8 | 8.37 | 2.1–32.7 | 0.94 | 0.9–1.0 |
| >13 | 0.00 | 0.0–5.6 | 100.00 | 99.3–100.0 | 1.00 | 1.0–1.0 | ||
The optimum cut-off value for APACHE II was >9. Sensitivity and specificity values at the cut off point line were 56.25 and 83.58, respectively. The Youden index 0.3983.
The optimum cut-off value for EuroSCORE was >3. Sensitivity and specificity values at the cut off point line were 93.75 and 51.9, respectively. The Youden index was 0.4524.
Discussion
In the present study, we evaluated the mortality predictive ability of the APACHE II scoring system after cardiac surgery. Based on our study results, APACHE II may be an acceptable scoring system for predicting hospital mortality.
Despite advances in cardiac surgery, mortality remains high; several scoring systems have been developed and successfully implemented to predict mortality (7, 8). Risk scores depend on the population for which they were developed and the characteristics of their population. Risk scores in surgical practice measure not only risk but also analyse and compare results. The primary objectives of these systems are to predict operative mortality and evaluate peri-operative cardiac care. They are based on pre-operative general risk factors to predict intra- and peri-operative mortality.
EuroSCORE has been used in the past decade to estimate both in-hospital mortality and morbidity in a large number of cardiac surgery centres worldwide (9–11). In a large study including 6222 cardiac surgery patients and comparing 19 scoring systems, the discriminatory power for 30-day mortality was highest for EuroSCORE (12). We found that EuroSCORE overestimates the risk of mortality. The observed mortality was 8.33%, while the predicted mortality with EuroSCORE was 12.3%. This rate may be influenced by the type of procedure that the patients have undergone (only 64% of the patients underwent isolated coronary artery bypass grafting), patient sub-groups and different surgeons performing the surgery.
Outcome estimation scoring systems are being increasingly used in intensive care medicine, but most have not been developed for use in patients who have undergone cardiac surgery. Such post-operative models are not based on pre or peri-operative variables but only take into consideration parameters after admission to the ICU. The most commonly used post-operative scoring systems in cardiac ICUs in central Europe are APACHE II, SAPS II and the Sequential Organ Failure Assessment (13). At Ordu State Hospital, we use APACHE II.
The APACHE scoring system was designed in general ICUs; this system has been the gold standard for years to assess disease severity and estimate hospital mortality. The first version, which assessed disease severity on the basis of 34 physiological parameters, was presented by Knaus et al. (14). The next version, APACHE II, was published in 1985, and the hospital death risk was calculated (5). Subsequent versions were also developed.
The parts of APACHE II are as follows: a) 12 acute physiological parameters (acute physiology score), b) patient age and c) chronic diseases and surgical procedures. The score was confirmed in specific patient populations, including surgical (15) and trauma patients, as well as among patients with general critical illnesses (16, 17). There is a benefit in predicting mortality in critically ill trauma patients (18), transplant patients (19) and sepsis patients (20).
However, the subset of patients who underwent cardiac surgery was excluded during the development of several general scoring systems such as APACHE and the Simplified Acute Physiology Score. Even so, most of these scoring systems are used in cardiac surgery ICUs because of the lack of an appropriate risk index for this patient subset (21).
The oldest APACHE II system still predicts mortality well (22). APACHE III and IV are newer versions but are not widely accepted. All APACHE models are based on the most abnormal values of the parameters measured during the first 24 h after admission to the ICU. We calculated all APACHE scores on the first post-operative day.
Exarchopoulos et al. (23) found CASUS to be the most reliable and beneficial score in cardiac surgery patients. Doerr et al. (21) reported that APACHE II did not perform well in terms of calibration and discrimination statistics in a study of 2801 patients. They evaluated the APACHE II score on all ICU days. However, we used the score obtained only on the first post-operative day. Argyriou et al. (24) reported that the APACHE II score has good and comparable discriminative ability to predict the outcome in cardiac ICUs. They found the best predictive ability (AUC=0.926) for mortality. In our study, APACHE II was found to be acceptable for predicting mortality after patients underwent open heart surgery (AUC=0.743). We found the optimum cut-off value for APACHE II to be >9. However, the median APACHE II score was 6 in our study population. Apache II may be separately computed for patients who die and those who remain alive.
Some specific factors belonging to cardiac surgery mean that some scoring systems cannot be effectively used. The relatively long mechanical ventilation time (25) and post-operative sedation limiting the use of Glasgow Coma Scale score as a prognostic parameter (26) are examples of these.
The values of post-operative scoring systems can be affected because of electrolyte and blood glucose imbalance, long mechanical ventilation time, post-operative sedation after cardiac surgery and, mainly, cardiopulmonary bypass use (27, 28).
The use of intra-aortic balloon pumps and ventricular assist devices and low cardiac output syndrome (LCOS) occurring post-operatively (29) are important parameters affecting outcomes in patients. Unfortunately, most scoring systems ignore these parameters (21). All these factors have an effect on the prognosis.
The present study was based on retrospective single-centre data of patients in a small hospital in Turkey. The major limitations of this study are the small sample size and single-centre design, which limit the extrapolation of the findings to generalised conclusions to the Turkish cardiac surgery population. The variety of cases and quality of care may have influenced the results. For further validating our findings, multicentre-studies are needed.
Conclusion
We retrospectively collected data of adult patients admitted to our ICU after undergoing cardiac surgery and evaluated the mortality predictive ability of the APACHE II scoring system.
Scoring systems are an important part of current cardiac surgical practices; they assess operative mortality and morbidity. More verification tests are needed globally for different patient populations due to changes in the cardiac case variety, surgical techniques and clinical outcomes. Based on the findings of our study, EuroSCORE and the APACHE II risk model had moderately acceptable AUC values (0.743 for APACHE II and was 0.767 for EuroSCORE) for predicting mortality. However, larger studies are required to confirm our results.
Footnotes
Ethics Committee Approval: Authors declared that the research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”, (amended in October 2013).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Y.A.; Design - K.T.; Supervision - Y.A.; Resources - M.Y., E.G., S.Y.; Materials - S.Y.; Data Collection and/or Processing - M.Y., E.G.; Analysis and/or Interpretation - M.Y., M.Ü.; Literature Search - M.Y., M.Ü., K.T.; Writing Manuscript - M.Y.; Critical Review - Y.A.; Other - K.T.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Hekmat K, Kroener A, Stuetzer H, Schwinger RH, Kampe S, Bennink GB, et al. Daily assessment of organ dysfunction and survival in intensive care unit cardiac surgical patients. Ann Thorac Surg. 2005;79:1555–62. doi: 10.1016/j.athoracsur.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 2.Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk factor evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79:3–12. [PubMed] [Google Scholar]
- 3.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–22. doi: 10.1016/S1010-7940(99)00106-2. [DOI] [PubMed] [Google Scholar]
- 4.Kunt AG, Kurtcephe M, Hidiroglu M, Cetin L, Kucuker A, Bakuy V, et al. Comparison of original EuroSCORE, EuroSCORE II and STS risk models in a Turkish cardiac surgical cohort. Interact Cardiovasc Thorac Surg. 2013;16:625–9. doi: 10.1093/icvts/ivt022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working group on Sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 7.Geissler HJ, Hölzl P, Marohl S, Kuhn-Régnie RF, Mehlhorn U, Südkamp M, et al. Risk stratification in heart surgery: comparison of six score systems. Eur J Cardiothorac Surg. 2000;17:400–6. doi: 10.1016/S1010-7940(00)00385-7. [DOI] [PubMed] [Google Scholar]
- 8.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/S1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 9.Tsaousi G, Pitsis AA, Ioannidis GD, Pourzitaki CK, Giannacou-Peftoulidou MN, Vasilakos DJ. Implementation of EuroSCORE II as an adjunct to APACHE II model and SOFA score, for refining the prognostic accuracy in cardiac surgical patients. J Cardiovasc Surg. 2015;56:919–27. [PubMed] [Google Scholar]
- 10.Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:882–3. doi: 10.1016/S0195-668X(02)00799-6. [DOI] [PubMed] [Google Scholar]
- 11.Nashef SA, Roques F, Hammill BG, Peterson ED, Michel P, Grover FL, et al. Validation of European System for Cardiac Operative Risk Evaluation (EuroSCORE) in North American cardiac surgery. Eur J Cardiothorac Surg. 2002;22:101–5. doi: 10.1016/S1010-7940(02)00208-7. [DOI] [PubMed] [Google Scholar]
- 12.Nilsson J, Algotsson L, Hoglund P, Luhrs C, Brandt J. Comparison of 19 pre-operative risk stratification models in open-heart surgery. Eur Heart J. 2006;27:867–74. doi: 10.1093/eurheartj/ehi720. [DOI] [PubMed] [Google Scholar]
- 13.Niewiński G, Starczewska M, Kański A. Prognostic scoring systems for mortality in intensive care units-The APACHE model. Anaesthesiology Intensive Therapy. 2014;46:46–9. doi: 10.5603/AIT.2014.0010. [DOI] [PubMed] [Google Scholar]
- 14.Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981;9:591–7. doi: 10.1097/00003246-198108000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Giangiuliani G, Mancini A, Gui D. Validation of a severity of illness score (APACHE II) in a surgical intensive care unit. Intensive Care Med. 1989;15:519–22. doi: 10.1007/BF00273563. [DOI] [PubMed] [Google Scholar]
- 16.Rutledge R, Fakhry S, Rutherford E, Muakkassa F, Meyer A. Comparison of APACHE II, trauma score, and injury severity score as predictors of outcome in critically injured trauma patients. Am J Surg. 1993;166:244–7. doi: 10.1016/S0002-9610(05)80966-3. [DOI] [PubMed] [Google Scholar]
- 17.Moreau R, Soupison T, Vauquelin P, Derrida S, Beaucour H, Sicot C. Comparison of two simplified severity scores (SAPS and APACHE II) for patients with acute myocardial infarction. Crit Care Med. 1989;17:409. doi: 10.1097/00003246-198905000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Hwang SY, Lee JH, Lee YH, Hong CK, Sung AJ, Choi YC. Comparison of the sequential organ failure assessment. Acute physiology and chronic health evaluation II scoring system, and trauma and injury severity score method for predicting the outcomes of intensive care unit trauma patients. Am J Emerg Med. 2011;30:749–53. doi: 10.1016/j.ajem.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 19.Basile-Filho A, Nicolini EA, Auxiliadora-Martins M, Alkmim-Teixeira GC, Martinez EZ, Martins-Filho OA, et al. Comparison of acute physiology and chronic health evaluation II death risk, child-pugh, Charlson, and model for end-stage liver disease indexes to predict early mortality after liver transplantation. Transplant Proc. 2011;43:1660–4. doi: 10.1016/j.transproceed.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 20.Bohnen J, Mustard RA, Oxholm SE, Schouten BD. APACHE II score and abdominal sepsis: a prospective study. Arch Surg. 1988;123:225. doi: 10.1001/archsurg.1988.01400260113014. [DOI] [PubMed] [Google Scholar]
- 21.Doerr F, Badreldin A, Heldwein M, Bossert T, Richter M, Lehmann T, et al. A comparative study of four intensive care outcome prediction models in cardiac surgery patients. J Cardiothorac Surg. 2011;6:1–8. doi: 10.1186/1749-8090-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strand K, Flaatten H. Severity scoring in the ICU: a review. Acta Anaesthesiol Scand. 2008;52:467–78. doi: 10.1111/j.1399-6576.2008.01586.x. [DOI] [PubMed] [Google Scholar]
- 23.Exarchopoulos T, Charitidou E, Dedeilias P, Charitos C, Routsi C. Scoring Systems for Outcome Prediction in a Cardiac Surgical Intensive Care Unit: A Comparative Study. Am J Crit Care. 2015;24:327–34. doi: 10.4037/ajcc2015500. [DOI] [PubMed] [Google Scholar]
- 24.Argyriou G, Vrettou C, Filippatos G, Sainis G, Nanas S, Routsi C. Comparative evaluation of Acute Physiology and Chronic Health Evaluation II and Sequential Organ Failure Assessment scoring systems in patients admitted to the cardiac intensive care unit. J Crit Care. 2015;30:752–7. doi: 10.1016/j.jcrc.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 25.Rady MY, Ryan T, Starr NJ. Perioperative determinants of morbidity and mortality in elderly patients undergoing cardiac surgery. Crit Care Med. 1998;26:225–35. doi: 10.1097/00003246-199802000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Marik PE, Varon J. Severity scoring and outcome assessment. Computerized predictive models and scoring systems. Crit Care Clin. 1999;15:633–46. doi: 10.1016/s0749-0704(05)70076-2. [DOI] [PubMed] [Google Scholar]
- 27.Ryan TA, Rady MY, Bashour CA, Leventhal M, Lytle B, Starr NJ. Predictors of outcome in cardiac surgical patients with prolonged intensive care stay. Chest. 1997;112:1035–42. doi: 10.1378/chest.112.4.1035. [DOI] [PubMed] [Google Scholar]
- 28.Weiss YG, Merin G, Koganov E, Ribo A, Oppenheim-Eden A, Medalion B, et al. Postcardiopulmonary bypass hypoxemia: a prospective study on incidence, risk factors, and clinical significance. J Cardiothorac Vasc Anesth. 2000;14:506–13. doi: 10.1053/jcan.2000.9488. [DOI] [PubMed] [Google Scholar]
- 29.Higgins TL, Estafanous FG, Loop FD, Beck GJ, Lee JC, Starr NJ, et al. ICU admission score for predicting morbidity and mortality risk after coronary artery bypass grafting. Ann Thorac Surg. 1997;64:1050–8. doi: 10.1016/S0003-4975(97)00553-5. [DOI] [PubMed] [Google Scholar]


