Abstract
Objective
Minor surgical procedures under general anaesthesia require a patent airway without the use of muscle relaxant. Supraglottic airway devices have been widely used for airway management. A study was undertaken to compare first-time insertion success rate, insertion time, sealing pressure and complications between the Baska® mask and I-gel.
Methods
After approval from the institutional ethical committee, a randomised single-blinded study was conducted on 50 American Society of Anesthesiologists’ physical status I and II female patients aged 18–40 years who underwent minor surgical procedures under general anaesthesia. Patients were randomly categorized into two groups of 25 each; group Baska® mask and group I-gel, and the first-time success rate, mean insertion time and sealing pressure were measured. The results were analysed using unpaired t-test, Mann-Whitney U test, Chi-square test and ANOVA. A p value <0.05 was considered to be statistically significant.
Results
The first-time insertion success rate of the Baska® mask was 21/24 (88%) when compared with the I-gel, which was 23/25 (92%) (p=0.585). The insertion time of the Baska® mask was 14.9±6.2 s, whereas that of the I-gel was 14.7±4.4 s (p=0.877). The mean sealing pressure of the Baska® mask was significantly higher when compared with the I-gel (28.9±3.5 vs. 25.9±2.5 cmH2O) (p=0.001).
Conclusion
The Baska® mask had a similar first-time insertion success rate and insertion time as the I-gel. The sealing pressure of the Baska® mask was significantly greater than that of the I-gel. Both devices had complications that were comparable.
Keywords: Airway device, general anaesthesia, minor surgical procedures
Introduction
Minor surgical procedures under general anaesthesia require a patent airway without the use of muscle relaxant (1). For such procedures, various supraglottic airway devices have been designed and are being used exceedingly. Although endotracheal intubation is the gold standard for airway management, it is being replaced by supraglottic airway devices because they are easy to introduce, better tolerated and results in a lesser haemodynamic response. Further these devices have lesser implications on airway and respiratory mechanics (2–5).
The I-gel (Intersurgical Ltd, Wokingham, Berkshire, UK) is a supraglottic airway device with an anatomically designed non-inflatable mask that snugly fits onto the perilaryngeal framework. The device has a buccal cavity stabiliser with an airway channel and a gastric tube insertion channel (6).
The Baska mask® (Proact Medical Ltd, Frenchs Forest NSW, Australia) is a new supraglottic non-inflatable airway device that has a self-sealing membranous cuff that inflates during inspiration and deflates during expiration. An inbuilt tab facilitates insertion of the device. It also has an oesophageal drainage inlet, a side channel to facilitate aspiration of gastric contents and an integrated bite-block (7).
Being a contemporary, untrodden device, possessing the Baska mask® in one’s armamentarium can serve a diversified use in spontaneous and controlled ventilation. However, this invention is still in its early roots, and its competence on various fronts has to be evaluated.
We hypothesised that the Baska mask®, a recently introduced airway device, has a higher first-time insertion success rate, requires lesser time for insertion, has a higher sealing pressure and has fewer airway complications.
Methods
After approval from the institutional ethical committee, (No KIMS/PGS/ETHICS/405/2017-2018) this randomised single-blinded study was conducted on 50 American Society of Anesthesiologists’ physical status I and II female patients aged 18–40 years who underwent minor surgical procedures (duration <60 minutes) under general anaesthesia. Patients who underwent elective surgical procedures with a fasting period of minimum 6 hours and Mallampati scores of I, II or III between July 2017 and Dec 2017 were included in the study. During the pre-operative visit, the detailed history was recorded and clinically examined. Informed written consent was obtained from all the patients. Patients with neck pathology, anticipated difficult airway, pregnant women, those with increased risk of aspiration, with mouth opening <2.5 cm and those having body mass index >30 kg.m−2 were excluded from the study.
The patients were randomly categorised into two groups of 25 each (group B: Baska mask® and group I: I-gel) by computer-generated random numbers that were enclosed in a sealed envelope opened only at the time of induction. The sizes of the I-gel and Baska mask® devices were as per the manufacturer’s recommendation and were based on the patients’ body weight, i.e. Size 3 for weight 30–60 kg and size 4 for 50–90 kg for the I-gel; and size 3 for weight 30–50 kg, size 4 for 50–70 kg and size 5 for 70–100 kg for the Baska mask®.
After securing intravenous access, all patients were monitored using non-invasive blood pressure, electrocardiogram (ECG), pulse oximeter (SpO2) and capnography.
All patients were pre-medicated with i.v. glycopyrrolate 0.004 mg kg−1, ranitidine 1 mg kg−1, midazolam 1.5–2 mg and fentanyl 2 μg kg−1. Following pre-oxygenation with 100% oxygen for 3 minutes, anaesthetic induction was initiated with i.v. propofol 2 mg kg−1. Succinylcholine 0.25 mg kg−1 was used to facilitate insertion of the device. The head was placed in neutral position on a pillow. The device was inserted by a qualified anaesthesiologist with more than 3 years of experience. Sixty seconds after administration of succinylcholine, a well lubricated Baska mask® was compressed between the thumb and two fingers and negotiated along the palate-pharyngeal curvature until resistance was encountered. The device was either reinserted or the size of the device was changed if an obvious leak was observed. If the insertion failed even after three attempts, an alternative device was used and the patient was excluded from the study. Successful device placement was concurred by the appearance of a square wave capnograph trace and bilateral chest movements on ventilation. Anaesthesia was maintained with 33% oxygen and nitrous oxide on spontaneous ventilation. A bolus dose of ketamine 1 mg kg−1 and propofol 1 mg kg−1 was administered soon after securing the device. Subsequently, an additional dose of propofol bolus was administered if required, and the total dose of propofol administered was noted.
The I-gel was introduced using a standard technique in which the device was firmly grasped, with the cuff outlet facing the chin and then gently guided along the hard palate until resistance was felt.
The primary outcome was to measure the first-time insertion success rate and the number of attempts required for successful placement of the device.
The secondary outcome was to measure the effective device insertion time, sealing pressure, ease of insertion of gastric tube and complications.
The effective device insertion time was measured in seconds from the time the device was picked up by the operator until the square wave of capnograph trace was obtained.
The airway sealing pressure was measured using a handheld manometer. After closing the adjustable pressure limiting valve of the breathing system and with a fixed gas flow of 5 L min−1 with positive pressure ventilation, the manometer reading was recorded at the point at which minimum leak was heard. After the device was successfully placed, a lubricated size 10 French G gastric tube was inserted. The ease of insertion was graded as easy, difficult and impossible.
The patients’ heart rate (HR), mean arterial blood pressure (MAP) and SpO2 were recorded for 25 minutes. SpO2<95 was considered as oxygen desaturation. Occurrence of intra-operative laryngospasm, bronchospasm, gastric distension, cough and hiccups were observed.
Following surgery, the device was removed when the patient was awake and responsive. The integrity of the device and the presence of blood stains were noted. The patient was inspected for any injury to the lips, tongue and teeth. On removal of the device, cough, signs of regurgitation and aspiration were recorded. All patients were followed up for 24 hours for any dysphagia and sore throat.
Statistical analysis
The sample size was calculated using OpenEpi version 3 and sample size calculator. The mean sealing pressure of I-gel was 23.58±4.9 cm H2O in a previous study (8). A minimum difference of at least 5 cm H2O in the sealing pressures was anticipated. The expected mean value of the other group was 28.58 cm H2O. The expected standard deviation of 6.0 was calculated from the coefficient of variation from the previous study. With a power of 80% and confidence interval of 95%, a sample size of 19 patients was estimated for each group. To make up for losses due to failure to insert the device, 25 patients were recruited into each group. The data were analysed using Epidata V2.2.186 and SPSS 20.0 software. Continuous variables, such as age, height, weight, device insertion time, sealing pressure and propofol infused, were compared between the two groups using unpaired t-test or Mann-Whitney U test. Categorical variables, such as Mallampati score, device insertion attempts, ease of insertion of gastric tube and complications were compared using Chi-square test. The haemodynamic variables were compared using repeated measures of ANOVA. The p value <0.05 was considered to be statistically significant.
Results
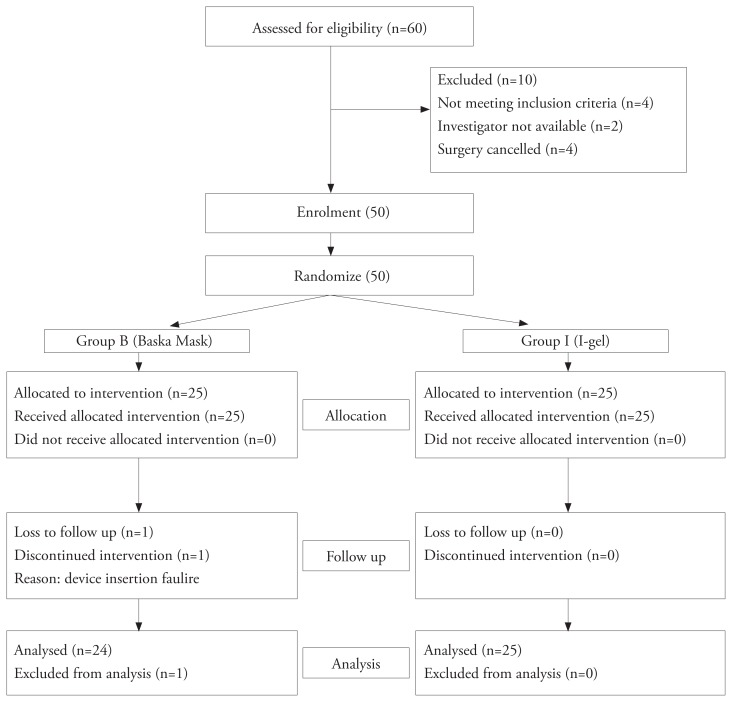
A total of 50 female patients were enrolled in the study and randomly categorised into two groups. The surgeries included abdominal tubectomy, fibroadenoma excision, drainage of breast abscess, dilatation and curettage. One patient from group B was excluded from the final analysis as the device could not be placed successfully despite three attempts (Figure 1). The demographics, Mallampati scores and duration of anaesthesia were comparable in both the groups (Table 1 and 2). Further, the overall success rate was comparable between the groups (Table 2). The insertion time of the Baska mask® was marginally higher compared with that of the I-gel; however, the difference was not statistically significant (Table 2). The sealing pressure of group B was more than that of group I and was statistically significant (p=0.001) (Table 2).
Figure 1.
Consort flow chart
Table 1.
Comparison of age, weight, height and Mallampati score
| Patient characteristics | Group B Mean±SD n=25 |
Group I Mean±SD n=25 |
p |
|---|---|---|---|
|
| |||
| Age (years) | 25.6±4.0 | 26.0±3.0 | 0.664 |
| Weight (kg) | 51.9±6.9 | 53.6±9.3 | 0.450 |
| Height (cm) | 152.2±9.3 | 154.7±5.2 | 0.065 |
| Mallampati score | 15/9/1 | 15/10/0 | 0.591 |
SD: standard deviation
Table 2.
Device insertion attempts, insertion time, sealing pressure, duration of anaesthesia, ease of gastric tube insertion
| Group B n=24 |
Group I n=25 |
p | |
|---|---|---|---|
|
| |||
| Insertion attempts | n (%) | n (%) | 0.585 |
| 1 | 21 (87.5) | 23 (92) | |
| 2 | 2 (8.33) | 2 (8) | |
| 3 | 1 (4.16) | 0 | |
| Insertion time (seconds) | 14.9±6.2 | 14.7±4.4 | 0.877 |
| Sealing pressure (cm H2O) | 28.9±3.5 | 25.9±2.5 | 0.001* |
| Duration of anaesthesia (minutes) | 23.9±8.2 | 24.8±9.8 | 0.747 |
| Insertion of gastric tube | n (%) | n (%) | 0.368 |
| Easy | 23 (95.83) | 24 (96) | |
| Difficult | 0 | 1 (4) | |
| Impossible | 1 (4.17) | 0 | |
significant
There was no significant haemodynamic difference among the groups. (Table 3 and 4) Intra-operatively, no patient had laryngospasm, bronchospasm, gastric distension, cough or hiccups. There was no statistically significant difference in the complications after removal of the device between the groups (Table 5). The intra-operative requirement of propofol was comparable between the groups (p=1.000).
Table 3.
Comparison of mean heart rate changes between the two groups
| HR | Group B | Group I | p |
|---|---|---|---|
|
| |||
| Baseline | 93.7±11.5 | 91.3±12.2 | 0.478 |
| 1 minute | 93.7±10.0 | 90.1±13.1 | 0.280 |
| 2 minutes | 93.5±10.2 | 88.8±14.0 | 0.188 |
| 3 minutes | 90.1±9.5 | 87.4±16.5 | 0.367 |
| 4 minutes | 91.0 ±12.2 | 85.4±15.3 | 0.165 |
| 5 minutes | 90.5±10.2 | 84.5±13.4 | 0.086 |
| 10 minutes | 90.3±12.8 | 85.2±13.4 | 0.181 |
| 15 minutes | 90.6±10.8 | 87.1±10.5 | 0.261 |
| 20 minutes | 89.7±13.7 | 85.4±11.8 | 0.244 |
| 25 minutes | 91.2±13.5 | 85.6±12.1 | 0.127 |
HR: heart rate
Table 4.
Comparison of mean arterial pressure changes between the two groups
| MAP | Group B | Group I | p |
|---|---|---|---|
|
| |||
| Baseline | 90.5±11.6 | 99.1±10.7 | 0.010 |
| 1 minute | 93.0±11.8 | 92.2±14.4 | 0.850 |
| 2 minutes | 92.3±13.8 | 90.1±15.1 | 0.590 |
| 3 minutes | 92.5±10.4 | 88.0±14.1 | 0.208 |
| 4 minutes | 92.1±15.5 | 89.9±12.4 | 0.579 |
| 5 minutes | 95.8±13.4 | 89.0±12.3 | 0.071 |
| 10 minutes | 95.2±12.4 | 87.0±14.9 | 0.040 |
| 15 minutes | 92.7±13.4 | 87.9±12.4 | 0.202 |
| 20 minutes | 93.2±12.1 | 88.6±10.2 | 0.157 |
| 25 minutes | 93.9±13.9 | 88.9±11.9 | 0.174 |
MAP: mean arterial pressure
Table 5.
Complications after device removal
| Group B n=24 (%) |
Group I n=25 (%) |
p | |
|---|---|---|---|
|
| |||
| Cough | 1 (4.17) | 1 (4) | 0.488 |
| Signs of regurgitation | 0 | 0 | 1.000 |
| Signs of aspiration | 0 | 0 | 1.000 |
| Trauma | 0 | 0 | 1.000 |
| Blood stains | 1 (4.17) | 1 (4) | 0.488 |
| Dysphagia | 0 | 0 | 1.000 |
| Sore throat | 3 (12.5) | 0 | 0.220 |
Discussion
The Baska mask® is a recently introduced device with unique improvements over other devices to enhance patient safety and ease of insertion. The device has been stated to serve an additional advantage of higher sealing pressures compared with other non-inflatable devices such as I-gel. Because both the Baska mask® and I-gel have a non-inflatable self-sealing mechanism, these two devices were compared.
In our study, the success rate of insertion of the Baska mask® was comparable to that of the I-gel. In a study by Alexiev et al. (9) where the Baska mask® was compared with the single-use laryngeal mask airway in low-risk female patients, the Baska mask® proved to be more difficult to insert, required additional insertion attempts and had longer insertion time. The first-time success rate of the Baska mask® was 52/71 (73%) when compared to that of the laryngeal mask airway, which was 77/79 (98%). In our study, the first-time success rate of the Baska mask® was 21/24 (87.5%) when compared to that of the I-gel, which was 23/25 (92%). The lower success rates achieved for the Baska mask® may be attributable to the morphology of the device and unique expertise needed to insert the device.
In the study by Al-Rawahi et al. (8), the Baska mask® was compared with the proseal laryngeal mask; the mean insertion time of the Baska mask® was significantly shorter when compared with the proseal laryngeal mask (16.43±4.54 s vs. 21.45±6.13 s). They implicated their results to the non-inflatable cuff and the use of tab for insertion of the device. The insertion time of the Baska mask® in our study was 14.9±6.2 s and that of the I-gel was 14.7±4.4 s. The disparity in these results could be because of the cuffless nature of the devices used in our study.
Difficulties in placing the device successfully were encountered in a pilot study that was undertaken before commencing the present study. A small dose of succinylcholine enhanced the ease of placement of the device. With the use of muscle relaxant, the insertion time of the Baska mask® and I-gel was reduced. No patient in either group had cough or hiccups while placing the device. No additional dose of propofol for device placement in the second or third attempt was required.
Succinylcholine 0.25 mg kg−1 facilitated insertion of the laryngeal mask airway, reduced adverse events and proved to be a cost-effective drug for short surgical procedures in developing countries, where mivacurium and remifentanil are not easily available (10). In the present study, it was found that none of the patients required manipulation with the tab or additional manoeuvres for the appropriate placement of the device.
In our study, the mean sealing pressure of the Baska mask® was significantly higher than that of the I-gel (28.9±3.5 cm H2O vs. 25.9±2.5 cm H2O). The mean sealing pressure of the Baska mask® was 29.98±8.51 cm H2O in the study by Al-Rawahi et al. (8). The sealing pressures were more than 30 cm H2O in various other studies (11). Similar to the earlier study, even in our study, an adjustment of the depth of the device resulted in a superior seal (9, 11). Further, similar to previous studies, the membranous cuff of the Baska mask® adapting to the patients’ laryngopharynx, inflating during each breath and providing superior seal over time was observed in our study (11).
The mean sealing pressure of the I-gel was 23.58±4.9 cm H2O in a study by Kini et al. (12) and much higher in the study by Liew et al. (10), which was 27.31±0.92 cm H2O. The thermoplastic properties of the gel cuff provided an effective seal around the larynx over time (13).
No untoward complications were observed during the intra-operative period. One patient had oxygen saturation (SpO2) 95% intra-operatively and the same patient had sore throat in the post-operative period. On enquiring, this patient had history of dry cough and fever 2 weeks prior to the surgery, which was well controlled with a course of antibiotics. No difficulty in maintaining oxygenation or ventilation in the remaining patients was noted. There was no evidence of regurgitation, aspiration or gastric distension. The gastric tube could not be passed in one patient; in this patient, there was no gastric distension, laryngospasm or bronchospasm intra-operatively.
The post-operative complications were comparable between the groups. Three patients (12.5%) in group B had sore throat during the post-operative period, including one patient who had history of dry cough. Pre-operative dry cough could result in adverse respiratory events such as sore throat (14). No patient in group I had sore throat.
The lower incidence of sore throat in our study could be because of the short duration of surgery, thereby resulting in less tissue damage, and the administration of succinylcholine, which enhanced the ease of placing the device.
One patient each in group I and B had blood stains on the device.
In the study by Al-Rawahi et al. (8), 43.3% of patients had sore throat, and 20% of patients had hoarseness of voice with the use of the Baska mask®. In another study, 1% of patients had laryngospasm on emergence and 18% had blood staining on the Baska mask® on removal (7).
Fasciculations induced by succinylcholine could increase the incidence of sore throat. However, a recent study reported similar incidences of sore throat with the use of succinylcholine and rocuronium (15).
The incidence of sore throat was comparatively lower in various studies using the I-gel, which is probably due to the absence of inflatable cuff (16–18).
Study limitations
Only patients with Mallampati class I, II and III were included in the study. Bronchoscopy was not performed to evaluate the appropriate placement of the device as the study included only minor surgical procedures. The sealing pressure was measured only once immediately after placement of the device because the patient was not paralysed for the surgery. Only female patients aged 18–40 years were included in the study as a matter of convenience.
Conclusion
The Baska mask® with its unique morphological design and air shaft has first-time success rates and time of insertions that are comparable to those of the I-gel. The sealing pressures of the Baska mask® are superior to those of the I-gel and can serve as an exemplary, alternative airway device for short surgical procedures with minimum complications.
Acknowledgements
Dr. Mrudula, Dr. Arpitha, Dr. Raksha, Dr. Jayashree Post-graduate students, Dept of Anaesthesia, KIMS, Hubli, Karnataka, India.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Karnataka Institute of Medical Sciences (Approval number KIMS/PGS/ETHICS/405/2017-2018).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - R.S., S.I.S., V.K.B.; Design - R.S., S.I.S., V.K.B.; Supervision - R.S., S.I.S.; Data Collection and/or Processing - R.S., M.V.M., V.J., D.A.L.; Analysis and/or Interpretation - R.S., S.I.S., V.K.B., M.M.; Literature Search - R.S., S.I.S., M.M.; Writing Manuscript - R.S., M.M., V.J., D.A.L.; Critical Review - R.S., S.I.S., M.M., V.J., D.A.L.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Brandt L. The first reported oral intubation of the human trachea. Anesth Analg. 1987;66:1198–9. doi: 10.1213/00000539-198711000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Dyer RA, Llewellyn RL, James MF. Total i.v anesthesia with propofol and the laryngeal mask for orthopaedic surgery. Br J Anaesth. 1995;74:123–8. doi: 10.1093/bja/74.2.123. [DOI] [PubMed] [Google Scholar]
- 3.Cork RC, Depa RM, Standen JR. Prospective comparison of use of the laryngeal mask and endotracheal tube for ambulatory surgery. Anesth Analg. 1994;79:719–27. doi: 10.1213/00000539-199410000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt SB, Kendall AP, Lin ES, Oh TE. Resistance and additional inspiratory work imposed by the laryngeal mask airway. A comparison with tracheal tubes. Anesthesia. 1992;47:343–7. doi: 10.1111/j.1365-2044.1992.tb02179.x. [DOI] [PubMed] [Google Scholar]
- 5.Higgins PP, Chung F, Mezei G. Post operative sore throat after ambulatory surgery. Br J Anaesth. 2002;88:582–4. doi: 10.1093/bja/88.4.582. [DOI] [PubMed] [Google Scholar]
- 6.Levitan RM, Kinkle WC. Initial anatomic investigation of I-gel airway: A novel supraglottic airway without inflatable cuff. Anaesthesia. 2005;60:1022–6. doi: 10.1111/j.1365-2044.2005.04258.x. [DOI] [PubMed] [Google Scholar]
- 7.Alexiev V, Salim A, Kevin LG, Laffey JG. An observational study of the Baska mask®: a novel supraglottic airway. Anaesthesia. 2012;67:640–5. doi: 10.1111/j.1365-2044.2012.07140.x. [DOI] [PubMed] [Google Scholar]
- 8.Al-Rawahi SAS, Aziz H, Malik AM, Khan RM, Kaul N. A comparative analysis of the Baska® Mask vs Proseal laryngeal mask for general anesthesia with IPPV. Anaesth Pain & Intensive Care. 2013;17:233–6. [Google Scholar]
- 9.Alexiev V, Ochana A, Abdelrahman D, Coyne J, McDonnell JG, O’Toole DP, et al. Comparison of the Bask ® mask with the single-use laryngeal mask airway in low-risk female patients undergoing ambulatory surgery. Anaesthesia. 2013;68:1026–32. doi: 10.1111/anae.12356. [DOI] [PubMed] [Google Scholar]
- 10.Liew GHC, Yu ED, Shah SS, Kothandan H. Comparison of the clinical performance of i-gel, LMA Supreme and LMA ProSeal in elective surgery. Singapore Med J. 2016;57:432–7. doi: 10.11622/smedj.2016133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zundert TV, Gatt S. The Baska ® Mask ®- A new concept in Self-sealing membrane cuff extraglottic airway devices, using a sump and two gastric drains: A critical evaluation. J Obstet Anaesth Crit Care. 2012;2:23–30. doi: 10.4103/2249-4472.99313. [DOI] [Google Scholar]
- 12.Kini G, Devanna GM, Mukkapati KR, Chaudhuri S, Thomas D. Comparison of I-gel with proseal LMA in adult patients undergoing elective surgical procedures under general anesthesia without paralysis: A prospective randomized study. J Anaesthesiol Clin Pharmacol. 2014;30:183–7. doi: 10.4103/0970-9185.130008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabbott DA, Beringer R. The i-gel supraglottic airway: A potential role for resuscitation? Resuscitation. 2007;73:161–2. doi: 10.1016/j.resuscitation.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 14.Von Ungern-Sternberg BS, Ramgolam A, Hall GL, Sly PD, Habre W. Peri-operative adverse respiratory events in children. Anaesthesia. 2015;70:440–4. doi: 10.1111/anae.12946. [DOI] [PubMed] [Google Scholar]
- 15.Mencke T, Knoll H, Schreiber, Uwe J, Matthias E, Sarah K, et al. Rocuronium is not associated with more vocal cord injuries than succinylcholine after rapid-sequence induction: a randomized, prospective, controlled trial. Anesthesia Analgesia. 2006;102:943–9. doi: 10.1213/01.ane.0000194509.03916.02. [DOI] [PubMed] [Google Scholar]
- 16.De Montblanc J, Ruscio L, Maziot JX, Benhamou D. A systematic review and and meta-analysis of the i-gel® vs laryngeal mask airway in adults. Anaesthesia. 2014;69:1151–62. doi: 10.1111/anae.12772. [DOI] [PubMed] [Google Scholar]
- 17.Park SK, Choi GJ, Choi YS, Ahn EJ, Kang H. Comparison of the i-gel and the laryngeal mask airway proseal during general anesthesia: a systematic review and mete-analysis. PLoS One. 2015;10:e0119469. doi: 10.1371/journal.pone.0119469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen X, Jiao J, Cong X, Liu L, Wu X. A comparison of the performance of the i-gelTM vs the LMA laryngeal mask-SupremeTM during anesthesia: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e71910. doi: 10.1371/journal.pone.0071910. [DOI] [PMC free article] [PubMed] [Google Scholar]