Abstract
Background
With an increasing number of motor vehicle crashes, there is an urgent need in emergency departments (EDs) to assess patients with multiple trauma quickly, easily, and reliably. Trauma severity can range from a minor to major threats to life or bodily function. In-hospital mortality and trauma severity prediction in such cases is crucial in the ED for the management of multiple trauma and improvement of the outcome of these patients. Previous studies have examined the performance of Modified Early Warning Score (MEWS) or Circulation, Respiration, Abdomen, Motor, and Speech (CRAMS) score based solely on mortality prediction or injury severity prediction. However, to the best of our knowledge, the performances of both scoring systems on in-hospital mortality and trauma severity prediction have not been compared previously. This retrospective study evaluated the value of MEWS and CRAMS score to predict in-hospital mortality and trauma severity in patients presenting to the ED with multiple traumatic injuries.
Methods
All study subjects were multiple trauma patients. Medical data of 1,127 patients were analyzed between January 2014 and April 2018. The MEWS and CRAMS score were calculated, and logistic regression and receiver operating characteristic curve analysis were conducted to investigate their performances regarding in-hospital mortality and trauma severity prediction.
Results
For in-hospital mortality prediction, the areas under the receiver operating characteristic curve (AUROCs) for MEWS and CRAMS score were 0.90 and 0.91, respectively, indicating that both of them were good in-hospital mortality predictors. Further, our study indicated that the CRAMS score performed better in trauma severity prediction, with an AUROC value of 0.84, which was higher than that of MEWS (AUROC = 0.77). For trauma severity prediction, the optimal cut-off value for MEWS was 2, while that of the CRAMS score was 8.
Conclusions
We found that both MEWS and CRAMS score can be used as predictors for trauma severity and in-hospital mortality for multiple trauma patients, but that CRAMS score was superior to MEWS for trauma severity prediction. CRAMS score should be prioritized in the prediction of trauma severity due to its excellence as a multiple trauma triage tool and potential contribution to rapid emergency rescue decisions.
Keywords: Scoring system, MEWS, CRAMS, Multiple trauma
Introduction
Multiple trauma is reported as the fifth leading cause of mortality in China (Wang, Pan & Pan, 2017; Yin, Liang & Liu, 2015). Over 400,000 people die from trauma caused by motor vehicle crashes or industrial accidents each year in China, among which multiple trauma patients comprise about 1.0–1.8% (Zhang, Hong & Gregory, 2017; Yingcheng et al., 2014). Emergency departments (EDs) in China are faced with challenges in the management of multiple trauma due to its high mortality risk.
An efficient trauma triage system aims to support medical personnel in the identification of life-threatening conditions, performing timely assessments and prioritization of treatment according to the severity of the patient’s medical condition (Wangara et al., 2019). Because multiple trauma is critical and complex, early and proper triage of multiple trauma patients must be carried out as soon as the patient is admitted to the ED.
However, there is still no standard trauma triage tool that can be promptly and easily used by emergency physicians, surgeons, and intensivists to improve the morbidity and mortality in EDs. Various scoring systems, mainly based on vital signs, anatomical score, and neurological score, have been developed and used as trauma triage tools. Anatomical-based scoring systems include the abbreviated injury scale (Gennarelli & Wodzin, 2006) and its derived score injury severity score (ISS) (Wang, Pan & Pan, 2017; Yin, Liang & Liu, 2015; Yingcheng et al., 2014). ISS is used for injury severity assessment (Yin, Liang & Liu, 2015; Yingcheng et al., 2014) and mortality prediction in elderly patients (Wang, Pan & Pan, 2017), but requires injury site diagnosis by trauma specialists which is inconvenient and time-consuming in the ED. Neurological-based scoring systems include Alert, Confused, Drowsy, Unresponsive (ACDU) scales; Alert, Confused, Pain and Unresponsive (AVPU) scales; and Glasgow Coma Scale (GCS) (Kelly, Upex & Bateman, 2004; McNarry & Goldhill, 2004, Raman et al., 2011). ACDU and AVPU are derived from the GCS, and GCS is superior to AVPU (Zadravecz et al., 2015) and favored for brain trauma triage in elderly patients (Wasserman et al., 2015). The GCS is useful for evaluating damage to the central nervous system and determining prognosis, but is susceptible to interference by ethanol, drugs, tracheal intubation, and other factors (GX, GT & ZM, 2015). In addition, sophisticated scoring systems (Jones, Trzeciak & Kline, 2009; Goodacre, Turner & Nicholl, 2006; Olsson, Terént & Lind, 2004; Olsson & Lind, 2003; Shapiro et al., 2003; Boyd, Tolson & Copes, 1987; Long, Bachulis & Hynes, 1986; Sartorius et al., 2010; Hung et al., 2017; Knaus et al., 1985) incorporating both vital signs and neurologic or anatomic-based scores, such as trauma score (TS) (Long, Bachulis & Hynes, 1986), trauma and injury severity score (Boyd, Tolson & Copes, 1987), acute physiology and chronic health evaluation (APACHE) II score (Knaus et al., 1985), Rapid Acute Physiology Score (RAPS) (Goodacre, Turner & Nicholl, 2006), Rapid Emergency Medicine Score (REMS) (Olsson & Lind, 2003), and Mortality in Emergency Department Sepsis Score (MEDS) (Shapiro et al., 2003), have been proposed for mortality prediction and injury severity assessment. TS is simple and fast to use but is easily affected by physiological compensation, hypovolemia, hypoxia, tracheal intubation, and other factors. MEDS is mainly used in ED patients with suspected sepsis, especially for suspected infection cohorts (Shapiro et al., 2003). REMS and RAPS are mainly used in non-surgical patients; REMS is derived from RAPS. Further, REMS is superior to RAPS for mortality prediction in emergency medical admissions (Goodacre, Turner & Nicholl, 2006) and in-hospital mortality prediction (Olsson, Terént & Lind, 2004), and MEDS is superior to both of them for in-hospital mortality prediction for splenic abscess patients (Hung et al., 2017). REMS has the same predictive accuracy as the APACHE II score for in-hospital mortality prediction (Olsson & Lind, 2003). These scoring systems have been reported as reliable tools for mortality prediction and injury severity assessment, but are complicated and inconvenient for calculation (e.g., APACHE II requires 14 variables), which make it difficult to meet the needs of a rapid risk stratification tool in a regular ED setting.
Faced with the requirement of a simple, rapid, and effective trauma triage tool in the ED, Modified Early Warning Score (MEWS) (Subbe et al., 2001) and Circulation, Respiration, Abdomen, Motor, and Speech (CRAMS) score (Gormican, 1982) have been widely used for mortality prediction and trauma severity assessment in China. MEWS is a modified version of the early warning score (Goldhill et al., 2005). MEWS has been used to assess hospital admission (Subbe et al., 2001; Burch, Tarr & Morroni, 2008), in-hospital mortality (Burch, Tarr & Morroni, 2008; Le Onn Ho et al., 2013), detecting pre-hospital critical illness (Fullerton et al., 2012), fast track care for femoral fracture patients (Ollivere et al., 2012), and severe conditions of patients in intensive care unit (Tavares et al., 2008). On the other hand, CRAMS score has been used to triage trauma patients (Clemmer et al., 1985), and both retrospective and prospective studies have shown that CRAMS score is a trauma triage tool which is easy to use and accurate in identifying major trauma victims with high specificity and sensitivity (Oprita, Aignatoaie & Gabor-Postole, 2014). Both MEWS and CRAMS score are meritorious in that they can be calculated immediately because each of the variables in these scoring systems can be measured simply and rapidly, allowing the quick clinical determination of critically-ill patients requiring urgent intervention (Fullerton et al., 2012; Subbe et al., 2001; Oprita, Aignatoaie & Gabor-Postole, 2014). However, previous literature has investigated the performance of MEWS or CRAMS score based solely on mortality prediction or trauma severity prediction. To the best of our knowledge, no study has compared the performance of both systems in predicting in-hospital mortality and injury severity. Further, the patients examined previously were mainly trauma patients rather than multiple trauma patients.
In this study, we evaluated the value of MEWS and CRAMS score for predicting in-hospital mortality and trauma severity in patients presenting to the ED with multiple traumatic injuries, and compare the performance of MEWS and CRAMS score for assessing trauma severity and predicting in-hospital mortality in the victims.
Materials and Methods
Ethical statement
This retrospective research project was approved by the research ethics committee of Shanghai Ninth People’s Hospital, affiliated to Shanghai JiaoTong University School of Medicine (approval no.: 2018146-T132). The need for informed consent from study participants was waived. All data were processed anonymously.
Settings and subjects, and study design
Shanghai Ninth People’s Hospital is a non-profit university-affiliated tertiary teaching hospital located in Huangpu and Baoshan district in Shanghai, China. Its ED has 50 beds and is the second largest emergency center in Shanghai, equipped with medical detection devices and advanced emergency treatment instruments (www.9hospital.com.cn). The hospital admits approximately 20,000 trauma patients, 1.5% of which suffer from multiple trauma each year.
All adult medical patients consecutively admitted to the ED at Shanghai Ninth People’s Hospital, who had been conclusively diagnosed with multiple trauma from January 2014 to April 2018, were studied retrospectively to compare MEWS and CRAMS score outcomes for trauma injury severity and in-hospital mortality prediction. Here, imaging examinations, such as computed tomography (CT) scan, were used to diagnose multiple trauma by checking for the presence of two or more separate injuries, and if one or a combination of more than one endangered the patient’s life.
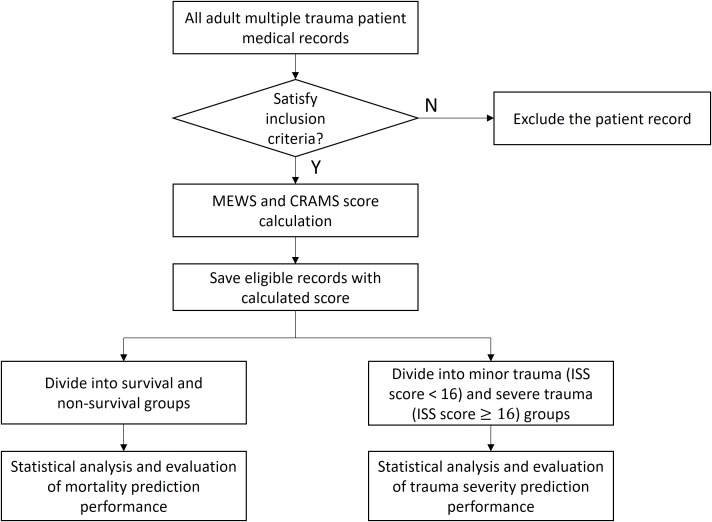
Figure 1 shows the flow diagram of the study. Inclusion criteria were: clear history of trauma, and final diagnosis of multiple injuries examined by imaging; age not younger than 16 years; complete clinical and medical history; no stroke; no dysfunction of the heart, liver, kidney, or other important organs before injuries; and no sepsis, pneumonia, and other histories of systemic infections before injuries. This study focused on the outcomes of multiple trauma patients so that only patients finally diagnosed with multiple trauma were included. The heart rate (HR) and systolic blood pressure (SBP) in the MEWS and SBP in the CRAMS is based on a range of normal adult values, so only patients aged sixteen years or older were included. Missing data with missing values of all vital signs related to MEWS and CRAMS score were excluded because they could not be imputed. Further, patients with stroke; dysfunction of the heart, liver, kidney, or other important organs before injuries; and sepsis, pneumonia, and other history of systemic infections before injuries were excluded, because it was difficult to identify the cause-and-effect of the in-hospital mortality and trauma severity. Further, we aimed to investigate in-hospital mortality, so dead-on-arrival patient data were excluded.
Figure 1. Study design.
The MEWS and CRAMS score were calculated for each subject based on the corresponding measured variables in their medical record (see sections on “MEWS” and “CRAMS score”). The medical records and calculated scores were saved to the database for further statistical analysis.
To investigate the outcome of in-hospital mortality prediction, the subjects were divided into survival and non-survival groups based on living condition within 28 days of hospitalization. Meanwhile, to investigate the outcome of trauma severity prediction, the same subjects were grouped into minor trauma and severe trauma groups based on the ISS—a “gold standard” among the anatomic injury severity indicators that is widely used in clinical science. The ISS was calculated using electronic medical records based on the diagnosis by imaging detection as well as surgical results. The ISS was only used for trauma classification in this study. Among the subjects, an ISS score < 16 was classified as minor trauma, while an ISS score ≥ 16 was classified as severe trauma (Baker et al., 1974; Gennarelli & Wodzin, 2006; Baker & O’Neill, 1976; Copes et al., 1988).
MEWS
The MEWS is widely used in the clinical setting as a quantified scoring system based on HR (beats per minute), SBP (mmHg), respiratory rate (RR, cycles per minute), temperature (T, °C), and AVPU. As reported previously, the AVPU is estimated from the GCS as follows: A = 14–15, V = 9–13, P = 4–8, U = 3 (Kelly, Upex & Bateman, 2004; McNarry & Goldhill, 2004; Raman et al., 2011; Wasserman et al., 2015; Zadravecz et al., 2015). The corresponding score, ranging from zero to three, for each variable is shown in Table 1 (Subbe et al., 2001; Clemmer et al., 1985).
Table 1. Modified early warning score (MEWS).
| Variable | Score | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| Systolic blood pressure (mmHg) | 101–199 | 81–100 | 70–80 | <70 |
| ≥200 | ||||
| Heart rate (/min) | 51–100 | 40–50 | <40 | ≥130 |
| 101–110 | 111–129 | |||
| Respiratory rate (/min) | 9–14 | 15–20 | <9 | ≥30 |
| 21–29 | ||||
| Temperature (°C) | 35–38.4 | <35 | ||
| ≥38.5 | ||||
| AVPU score | Alert | Reacts to voice | Reacts to pain | Unresponsive |
CRAMS score
The CRAMS score was calculated based on the following five variables: circulation, RR, abdomen, motor, and speech. Among these, circulation, RR, and speech are particularly important parameters for monitoring the health status of trauma patients (Gormican, 1982; Clemmer et al., 1985; Peng et al., 2017). The corresponding score, ranging from zero to two, for each variable is shown in Table 2. In contrast to MEWS, a lower CRAMS score indicates worse state of patients.
Table 2. Circulation, Respiration, Abdomen, Motor, and Speech (CRAMS) score.
| Variable | Score | ||
|---|---|---|---|
| 2 | 1 | 0 | |
| Circulation | Normal capillary refill and SBP ≥ 100 | Delay capillary refill or 85 ≤ SBP < 100 | No capillary refill or SBP < 85 |
| Respiratory rate | Normal | Labored or shallow or >35 bpm | Absent |
| Abdomen | Abdomen and thorax nontender | Abdomen or thorax tender | Abdomen rigid or flail chest |
| Motor | Normal | Responds only to pain, no posturing | No response or postures |
| Speech | Normal | Confused or inappropriate | No or unintelligible sounds |
Statistical analysis
The performance of MEWS and CRAMS score for in-hospital mortality and trauma severity prediction among multiple trauma patients were compared. Categorical variables were compared using Pearson’s chi-squared test and were described as frequencies (%). Numerical variables were compared by the non-parametric Mann–Whitney’s U-test and reported as median (interquartile range (IQR)).
Modified Early Warning Score and CRAMS score for all eligible subjects were computed based on Tables 1 and 2 and were compared using the non-parametric Mann–Whitney’s U-test and were reported as median (IQR).
Missing data with missed values of all four vital signs (T, HR, RR, and SBP) were excluded because they could not be imputed. Multiple imputation was performed to handle the missing data with missed values containing less than four vital signs.
To investigate the predictive values of MEWS and CRAMS score for trauma severity, logistic regression analysis was performed and the areas under the receiver operating characteristic curve (AUROCs) were evaluated for minor and severe trauma. To investigate the predictive values of MEWS and CRAMS score for in-hospital mortality, the same logistic regression and AUROC analysis framework was used based on survival and non-survival. The following model was employed for logistic regression analysis:
| (1) |
where β0 is the intercept; β1 is the score coefficient; and X1 is the score.
The R version 3.5.2 (www.r-project.org), a free software environment for statistical computing and graphics, was used to perform the logistic regression, and the R project package pROC (Robin et al., 2018) was used to compute AUROCs, and sensitivity, specificity, and accuracy rates for the corresponding optimal cut-off points.
Results
Setting and subjects
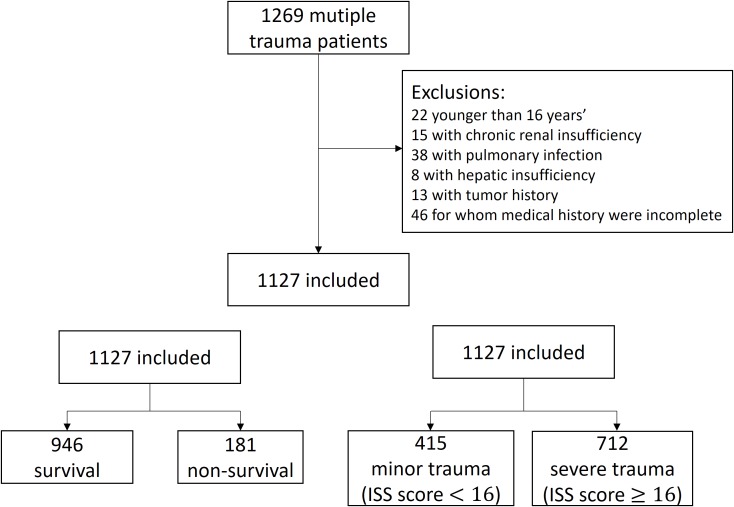
Figure 2 describes our study population. Medical records of 1,269 patients with multiple trauma were collocated, and 1,127 cases satisfying the inclusion criteria were included. The study population comprised 73.7% males, with a median (IQR) age of 48 (38–59). All patients underwent ground transportation without air transportation. Most patients (91.5%) were transported by ambulance. The median (IQR) length of stay (LOS) of the patients was 12 (4–21) days. Patients in severe trauma group (LOS, 14.5 (3–25) days) were admitted for a longer duration than those in the minor trauma group (LOS, 9 (5–15) days). Majority of patients sustained injuries in motor vehicle crashes (55.5%). The primary injury sites of both survivors and non-survivors were the head and neck (39.7% vs. 70.2%, respectively), while those of minor trauma and severe trauma populations were bony pelvis and extremities (43.1%) and the head and neck (58.3%), respectively. There were 51 (4.5%) patients with missing data, including 30 with missing values of three vital signs, 10 with missing values of two vital signs, and 11 with missing values of one vital sign.
Figure 2. Study population.
To investigate the outcome of in-hospital mortality prediction, the 1,127 cases were divided into survival and non-survival groups. The 1,127 eligible cases included 946 (83.9%) survivors and 181 (16.1%) non-survivors. Meanwhile, to investigate the outcome of trauma severity prediction, the same 1,127 cases were divided into minor trauma (ISS score < 16) (415 (36.8%) patients) and severe trauma (712 (63.2%)) groups.
Table 3 shows the characteristics of the study population in the survival and non-survival groups. Comparison of the survivors and non-survivors revealed the following factors to be statistically significant (p < 0.05) (Median (IQR))–RR: 20 (18–20) vs. 25 (20–29); temperature: 37.0 (36.8–37.0) vs. 36.5 (36.0–37.0) °C; and AVPU: 0 (0–0) vs. 3 (2–3).
Table 3. Characteristics of the survival and non-survival groups.
| Total | Survival | Non-survival | P-value | |
|---|---|---|---|---|
| No. | 1,127 | 946 | 181 | |
| Male, n (%) | 831 (73.7) | 697 (73.7) | 134 (74.0) | 0.994 |
| Age (years) | 48 (38–59) | 48 (38–58) | 48 (37–62) | 0.494 |
| Temperature (°C) | 36.9 (36.7–37.0) | 37.0 (36.8–37.0) | 36.5 (36.0–37.0) | <0.001 |
| Heart rate (/min) | 84 (75–96) | 84 (75–94) | 87.5 (68–117) | 0.065 |
| Respiratory rate (/min) | 20 (18–20) | 20 (18–20) | 25 (20–29) | <0.001 |
| Systolic blood pressure (mmHg) | 130 (114–148) | 130 (116–147) | 124 (89–159) | 0.099 |
| AVPU | 0 (0–1) | 0 (0–0) | 3 (2–3) | <0.001 |
| LOS | 12 (4–21) | 14 (8–22) | 1 (0–4) | <0.001 |
| Time of transport (hour) | 2 (1–3) | 2 (1–3) | 1 (1–1) | <0.001 |
| Cause of injury, n (%) | 0.001 | |||
| Motor vehicle crashes | 626 (55.5) | 511 (54.0) | 115 (63.5) | |
| High fall | 213 (18.9) | 183 (19.3) | 30 (16.6) | |
| Crushing injury | 32 (2.8) | 20 (2.1) | 12 (6.6) | |
| Cut/pierce | 41 (3.6) | 35 (3.7) | 6 (3.3) | |
| Burn | 3 (0.3) | 2 (0.2) | 1 (0.6) | |
| Tumble injury | 149 (13.2) | 141 (14.9) | 8 (4.4) | |
| Struck | 63 (5.6) | 54 (5.7) | 9 (5.0) | |
| Primary injury site, n (%) | <0.001 | |||
| Face | 18 (1.6) | 18 (1.9) | 0 (0.0) | |
| Head and neck | 503 (44.6) | 376 (39.7) | 127 (70.2) | |
| Thorax | 267 (23.7) | 239 (25.3) | 28 (15.5) | |
| Abdomen and visceral pelvis | 106 (9.4) | 93 (9.8) | 13 (7.2) | |
| Bony pelvis and extremities | 232 (20.6) | 220 (23.3) | 12 (6.6) | |
| External structures | 1 (0.1) | 0 (0.0) | 1 (0.6) | |
| Discharge status, n (%) | <0.001 | |||
| Expired in the hospital | 181 (16.1) | 0 (0.0) | 181 (100.0) | |
| Discharge home | 524 (46.5) | 524 (55.4) | 0 (0.0) | |
| Discharge against medical advice | 67 (5.9) | 67 (7.1) | 0 (0.0) | |
| Discharge home with self-care | 311 (27.6) | 311 (32.9) | 0 (0.0) | |
| Transfer to another hospital | 44 (3.9) | 44 (4.7) | 0 (0.0) | |
| Score | ||||
| MEWS | 2 (1–3) | 1 (1–2) | 5 (4–8) | <0.001 |
| CRAMS | 9 (7–10) | 9 (8–10) | 5 (4–6) | <0.001 |
Note:
Data are reported as median (IQR).
Table 4 shows the characteristics of the study population in minor trauma and severe trauma groups. Upon comparison of minor trauma and severe trauma, the following factors were found to be statistically significant (p < 0.05) (Median (IQR))–SBP: 136 (121–151) vs. 127 (107–145) mmHg; RR: 20 (19–20) vs. 20 (18–21); HR: 82(75–90) vs. 85 (75–100); temperature: 37.0 (36.8–37.0) vs. 36.8 (36.5–37.0) °C; and AVPU: 0 (0–0) vs. 0 (0–2).
Table 4. Characteristics of the minor trauma and severe trauma groups.
| Total | Minor trauma | Severe trauma | P-value | |
|---|---|---|---|---|
| No. | 1,127 | 415 | 712 | |
| Male, n (%) | 831 (73.7) | 279 (67.2) | 552 (77.5) | <0.001 |
| Age (years) | 48 (38–59) | 48 (38–60) | 48 (38–58) | 0.496 |
| Temperature (°C) | 36.9 (36.7–37.0) | 37.0 (36.8–37.0) | 36.8 (36.5–37.0) | <0.001 |
| Heart rate (/min) | 84 (75–96) | 82 (75–90) | 85 (75–100) | 0.019 |
| Respiratory rate (/min) | 20 (18–20) | 20 (19–20) | 20 (18–21) | 0.003 |
| Systolic blood pressure (mmHg) | 130 (114–148) | 136 (121–151) | 127 (107–145) | <0.001 |
| AVPU | 0 (0–1) | 0 (0–0) | 0 (0–2) | <0.001 |
| LOS | 12 (4–21) | 9 (5–15) | 14.5 (3–25) | <0.001 |
| Time of transport (hour) | 2 (1–3) | 2.0 (1.0–2.0) | 2.0 (1.0–3.0) | 0.005 |
| Cause of injury, n (%) | <0.001 | |||
| Motor vehicle crashes | 626 (55.5) | 187 (45.1) | 439 (61.7) | |
| High fall | 213 (18.9) | 66 (15.9) | 147 (20.6) | |
| Crushing injury | 32 (2.8) | 6 (1.4) | 26 (3.7) | |
| Cut/pierce | 41 (3.6) | 27 (6.5) | 14 (2.0) | |
| Burn | 3 (0.3) | 2 (0.5) | 1 (0.1) | |
| Tumble injury | 149 (13.2) | 95 (22.9) | 54 (7.6) | |
| Struck | 63 (5.6) | 32 (7.7) | 31 (4.4) | |
| Primary injury site–n (%) | <0.001 | |||
| Face | 18 (1.6) | 17 (4.1) | 1 (0.1) | |
| Head and neck | 503 (44.6) | 88 (21.2) | 415 (58.3) | |
| Thorax | 267 (23.7) | 88 (21.2) | 179 (25.1) | |
| Abdomen and visceral pelvis | 106 (9.4) | 42 (10.1) | 64 (9.0) | |
| Bony pelvis and extremities | 232 (20.6) | 179 (43.1) | 53 (7.4) | |
| External structures | 1 (0.1) | 1 (0.2) | 0 (0.0) | |
| Discharge status, n (%) | <0.001 | |||
| Expired in the hospital | 181 (16.1) | 2 (0.5) | 179 (25.1) | |
| Discharge home | 524 (46.5) | 261 (62.9) | 263 (36.9) | |
| Discharge against medical advice | 67 (5.9) | 29 (7.0) | 38 (5.3) | |
| Discharge home with self-care | 311 (27.6) | 95 (22.9) | 216 (30.3) | |
| Transfer to another hospital | 44 (3.9) | 28 (6.7) | 16 (2.2) | |
| Score | ||||
| MEWS | 2 (1–3) | 1 (1–2) | 2 (1–4) | <0.001 |
| CRAMS | 9 (7–10) | 10 (9–10) | 8 (6–9) | <0.001 |
Note:
Data are reported as median (IQR).
MEWS and CRAMS score
Table 3 and 4 show the MEWS and CRAMS score of the study population. Comparing survivor and non-survivor populations, the median MEWS (IQR) was 1 (1–2) vs. 5 (4–8) (p < 0.001); the median CRAMS score (IQR) was 9 (8–10) vs. 5 (4–6) (p < 0.001).
Comparing minor trauma with severe trauma, the median MEWS (IQR) score was 1 (1–2) vs. 2 (1–4), p < 0.001; the median CRAMS (IQR) was 10 (9–10) vs. 8 (6–9), p < 0.001.
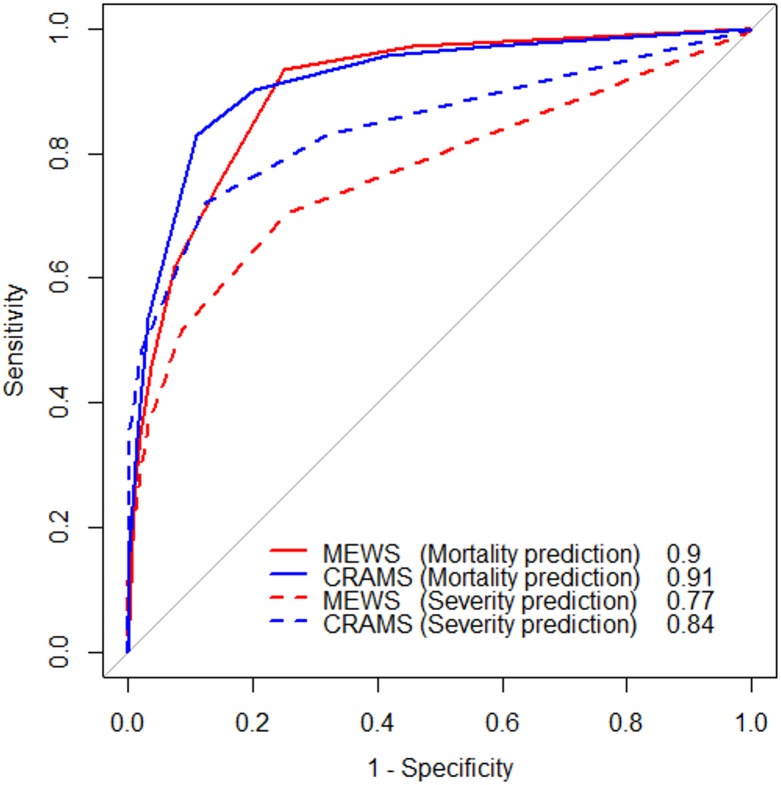
Figure 3 shows the receiver operating characteristic curves of the study population. For in-hospital mortality prediction, the AUROCs of MEWS and CRAMS score were 0.90 (95% confidence interval [CI] [0.88–0.92]) and 0.91 (95% CI [0.89–0.94]), respectively, indicating that both MEWS and CRAMS score were good predictors of in-hospital mortality. For multiple trauma severity prediction, the AUROCs of MEWS and CRAMS score were 0.77 (95% CI [0.74–0.79]) and 0.84 (95% CI [0.82–0.87]), respectively, indicating that CRAMS score was a better predictor of trauma severity. Table 5 shows the optimal cut-off values and their corresponding accuracy, sensitivity, and specificity values. For in-hospital mortality prediction, the optimal cut-off values of MEWS and CRAMS score were ≥3 and ≤6, respectively. For multiple trauma severity prediction, optimal cut-off values of MEWS and CRAMS score were ≥2 and ≤8, respectively.
Figure 3. Receiver operating characteristic (ROC) curve of the study population.
The red solid line is the ROC curve of MEWS in-hospital mortality prediction. The blue solid line is the ROC curve of CRAMS in-hospital mortality prediction. The red dashed line is the ROC curve of MEWS trauma severity prediction. The blue dashed line is the ROC curve of CRAMS trauma severity prediction.
Table 5. Optimal cut-off values and their corresponding sensitivities, specificities, and accuracy rates for in-hospital mortality and trauma severity prediction.
| In-hospital mortality prediction | Trauma severity prediction | |||||||
|---|---|---|---|---|---|---|---|---|
| Optimal cut-off | Accuracy | Sensitivity | Specificity | Optimal cut-off | Accuracy | Sensitivity | Specificity | |
| MEWS | ≥3 | 0.78 | 0.93 | 0.75 | ≥2 | 0.72 | 0.70 | 0.74 |
| CRAMS | ≤6 | 0.88 | 0.83 | 0.89 | ≤8 | 0.78 | 0.72 | 0.87 |
Discussion
The ED is the main location for treatment of emergency trauma patients, and trauma injury severity is an essential factor for evaluating the quality of trauma treatment and for predicting prognosis in the ED, especially for patients with multiple injuries (Boyd, Tolson & Copes, 1987; Long, Bachulis & Hynes, 1986).
In contrast to previous studies (Le Onn Ho et al., 2013; Ollivere et al., 2012; Sartorius et al., 2010; Steyerberg et al., 2008) that mainly focused on mortality prediction or injury severity prediction outcomes of the scoring systems, the present study, to the best of our knowledge, is the first to evaluate the performance of MEWS and CRAMS score in both in-hospital mortality prediction and trauma severity prediction. Further, our study included multiple trauma patients.
Our results demonstrated that both MEWS and CRAMS score were good predictors of in-hospital mortality, based on the AUROC values of 0.90 and 0.91, respectively. However, the trauma severity prediction performance of CRAMS score was better than that of MEWS. Furthermore, the performances of MEWS and CRAMS score in in-hospital mortality prediction were better than their performances in severity prediction. Hence, both MEWS and CRAMS score can be used for in-hospital mortality prediction, whereas CRAMS score can be used for trauma severity prediction with higher priority while triaging multiple trauma patients in the ED.
Both MEWS and CRAMS score are good predictors of in-hospital mortality because they both include vital signs (e.g., SBP and RR) and neurological variables (e.g., AVPU, Motor, and Speech), which are strongly related to mortality risk. Nevertheless, we argue that the CRAMS score is a better predictor of trauma severity due to the additional inclusion of the anatomical variable (i.e., Abdomen, a scoring criteria for abdominal and thoracic severity), which might enhance the injury assessment of CRAMS score. Further evaluation will be conducted to investigate this view in the future work.
Furthermore, CRAMS score is more convenient and rapid than MEWS because of fewer vital sign measurements and simpler score calculation. CRAMS score requires fewer vital sign measurements (2 (SPB and RR) vs. 4 (SBP, HR, RR, and T)) and fewer score stratifications for calculation (3 (0–2) vs. 4 (0–3)) than MEWS. Previous studies have demonstrated that CRAMS score can be assessed by the medical staff of the ED within 1–2 min of arrival of injured patients at the hospital, and it has high maneuverability because it is not limited by instruments and the location of injured patients (Burch, Tarr & Morroni, 2008; Tavares et al., 2008; Goldhill et al., 2005).
No standard multiple triage method is available in EDs in China. This study presented two rapid and convenient scoring systems for multiple trauma patient management. Our results showed that patients meeting the cut-off MEWS ≥ 3 or CRAMS score ≤ 6 should be treated as critically wounded patients; even if their vital signs are relatively stable, they might require immediate medical intervention, prompt imaging (e.g., whole-body CT), as well as preparation for surgery. Furthermore, among patients predicted to survive (CRAMS score > 6), those with CRAMS score ≤ 8 should be given more attention with respect to monitoring for disease-related changes for urgent rescue.
However, our study is not devoid of limitations. This retrospective study was confined to small samples. Although there was no difference in pre-hospital treatment, factors such as varying times of transition to the hospital may have resulted in bias of the analysis. In addition, the retrospective nature of the study is a limitation as it was not conducted in real time and results of scoring by multiple readers in a crunch could have been different. The population size is also a limiting factor because data were obtained from a single hospital. A larger sample from multiple hospitals is required to confirm our findings. We plan to collect more data for further investigation of injury severity prediction by MEWS and CRAMS score.
Conclusions
Both MEWS and CRAMS score can be used as predictors of trauma severity and in-hospital mortality for multiple trauma patients. CRAMS score is superior to MEWS for trauma severity prediction and should be prioritized when predicting trauma severity. It can serve as an excellent multiple trauma triage tool and will contribute to rapid emergency rescue decisions.
Supplemental Information
All variables related to MEWS and CRAMS calculation. Please refer to the CodeBook for the specific description of each variable (column label).
The meaning of each column label is described in this codebook.
Funding Statement
The authors received no funding for this work.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Xiaobin Jiang conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Ping Jiang conceived and designed the experiments, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Yuanshen Mao prepared figures and/or tables, approved the final draft.
Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
The research project was approved by the research ethics committee of Shanghai Ninth People’s Hospital Ethics Committee, affiliated to Shanghai JiaoTong University School of Medicine (approval no.: 2018146-T132), waiving the need for consent from study participants.
Data Availability
The following information was supplied regarding data availability:
All patient data are available in the Supplemental File.
References
- Baker & O’Neill (1976).Baker SP, O’Neill B. The injury severity score: an update. Journal of Trauma and Acute Care Surgery. 1976;16(11):882–885. doi: 10.1097/00005373-197611000-00006. [DOI] [PubMed] [Google Scholar]
- Baker et al. (1974).Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma and Acute Care Surgery. 1974;14(3):187–196. [PubMed] [Google Scholar]
- Boyd, Tolson & Copes (1987).Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the triss method. Trauma score and the injury severity score. Journal of Trauma. 1987;27(4):370–378. [PubMed] [Google Scholar]
- Burch, Tarr & Morroni (2008).Burch V, Tarr G, Morroni C. Modified early warning score predicts the need for hospital admission and inhospital mortality. Emergency Medicine Journal. 2008;25(10):674–678. doi: 10.1136/emj.2007.057661. [DOI] [PubMed] [Google Scholar]
- Clemmer et al. (1985).Clemmer TP, Orme JF, Jr, Thomas F, Brooks KA. Prospective evaluation of the crams scale for triaging major trauma. Journal of Trauma: Injury, Infection, and Critical Care. 1985;25(3):188–191. doi: 10.1097/00005373-198503000-00003. [DOI] [PubMed] [Google Scholar]
- Copes et al. (1988).Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The injury severity score revisited. Journal of Trauma and Acute Care Surgery. 1988;28(1):69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- Fullerton et al. (2012).Fullerton JN, Price CL, Silvey NE, Brace SJ, Perkins GD. Is the modified early warning score (mews) superior to clinician judgement in detecting critical illness in the pre-hospital environment? Resuscitation. 2012;83(5):557–562. doi: 10.1016/j.resuscitation.2012.01.004. [DOI] [PubMed] [Google Scholar]
- Gennarelli & Wodzin (2006).Gennarelli TA, Wodzin E. Ais 2005: a contemporary injury scale. Injury. 2006;37(12):1083–1091. doi: 10.1016/j.injury.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Goldhill et al. (2005).Goldhill D, McNarry A, Mandersloot G, McGinley A. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthesia. 2005;60(6):547–553. doi: 10.1111/j.1365-2044.2005.04186.x. [DOI] [PubMed] [Google Scholar]
- Goodacre, Turner & Nicholl (2006).Goodacre S, Turner J, Nicholl J. Prediction of mortality among emergency medical admissions. Emergency Medicine Journal. 2006;23(5):372–375. doi: 10.1136/emj.2005.028522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gormican (1982).Gormican SP. Crams scale: field triage of trauma victims. Annals of Emergency Medicine. 1982;11(3):132–135. doi: 10.1016/s0196-0644(82)80237-0. [DOI] [PubMed] [Google Scholar]
- GX, GT & ZM (2015).GX S, GT C, ZM L. Application of trauma scoring system in disaster rescue. Disaster Medicine and Rescue (Electronic Edition) 2015;4(2):66–68. [Google Scholar]
- Hung et al. (2017).Hung S-K, Ng C-J, Kuo C-F, Goh ZNL, Huang L-H, Li C-H, Chan Y-L, Weng Y-M, Seak JC-Y, Seak C-K, Seak C-J. Comparison of the mortality in emergency department sepsis score, modified early warning score, rapid emergency medicine score and rapid acute physiology score for predicting the outcomes of adult splenic abscess patients in the emergency department. PLOS ONE. 2017;12(11):e0187495. doi: 10.1371/journal.pone.0187495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, Trzeciak & Kline (2009).Jones AE, Trzeciak S, Kline JA. The sequential organ failure assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Critical Care Medicine. 2009;37(5):1649–1654. doi: 10.1097/ccm.0b013e31819def97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, Upex & Bateman (2004).Kelly CA, Upex A, Bateman DN. Comparison of consciousness level assessment in the poisoned patient using the alert/verbal/painful/unresponsive scale and the Glasgow Coma Scale. Annals of Emergency Medicine. 2004;44(2):108–113. doi: 10.1016/j.annemergmed.2004.03.028. [DOI] [PubMed] [Google Scholar]
- Knaus et al. (1985).Knaus WA, Draper EA, Wagner DP, Zimmerman JE. Apache ii: a severity of disease classification system. Critical Care Medicine. 1985;13(10):818–829. [PubMed] [Google Scholar]
- Le Onn Ho et al. (2013).Le Onn Ho HL, Shahidah N, Koh ZX, Sultana P, Ong MEH. Poor performance of the modified early warning score for predicting mortality in critically ill patients presenting to an emergency department. World Journal of Emergency Medicine. 2013;4(4):273. doi: 10.5847/wjem.j.issn.1920-8642.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long, Bachulis & Hynes (1986).Long WB, Bachulis BL, Hynes GD. Accuracy and relationship of mechanisms of injury, trauma score, and injury severity score in identifying major trauma. American Journal of Surgery. 1986;151(5):581–584. doi: 10.1016/0002-9610(86)90553-2. [DOI] [PubMed] [Google Scholar]
- McNarry & Goldhill (2004).McNarry A, Goldhill D. Simple bedside assessment of level of consciousness: comparison of two simple assessment scales with the Glasgow Coma Scale. Anaesthesia. 2004;59(1):34–37. doi: 10.1111/j.1365-2044.2004.03526.x. [DOI] [PubMed] [Google Scholar]
- Ollivere et al. (2012).Ollivere B, Rollins K, Brankin R, Wood M, Brammar T, Wimhurst J. Optimising fast track care for proximal femoral fracture patients using modified early warning score. Annals of The Royal College of Surgeons of England. 2012;94(4):267–271. doi: 10.1308/003588412x13171221501744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsson & Lind (2003).Olsson T, Lind L. Comparison of the rapid emergency medicine score and apache ii in nonsurgical emergency department patients. Academic Emergency Medicine. 2003;10(10):1040–1048. doi: 10.1111/j.1553-2712.2003.tb00572.x. [DOI] [PubMed] [Google Scholar]
- Olsson, Terént & Lind (2004).Olsson T, Terént A, Lind L. Rapid emergency medicine score: a new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. Journal of Internal Medicine. 2004;255(5):579–587. doi: 10.1111/j.1365-2796.2004.01321.x. [DOI] [PubMed] [Google Scholar]
- Oprita, Aignatoaie & Gabor-Postole (2014).Oprita B, Aignatoaie B, Gabor-Postole D. Scores and scales used in emergency medicine. Practicability in toxicology. Journal of Medicine and Life. 2014;7(Spec Iss 3):4–7. [PMC free article] [PubMed] [Google Scholar]
- Peng et al. (2017).Peng L, Hu H, He Y, Zeng M, Wang H, Hao D, Yao P, Shao Y, Cao Y. Kts and crams were useful trauma scores in a resource-limited settings. American Journal of Emergency Medicine. 2017;35(9):1372–1373. doi: 10.1016/j.ajem.2017.03.028. [DOI] [PubMed] [Google Scholar]
- Raman et al. (2011).Raman S, Sreenivas V, Puliyel JM, Kumar N. Comparison of alert-verbal-painful-unresponsiveness scale and the Glasgow Coma Score. Indian Pediatrics. 2011;48(4):331–332. [PubMed] [Google Scholar]
- Robin et al. (2018).Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J-C, Müller M, Siegert S. pROC: display and analyze ROC curves. 2018. https://CRAN.R-project.org/package=pROC https://CRAN.R-project.org/package=pROC
- Sartorius et al. (2010).Sartorius D, Le Manach Y, David J-S, Rancurel E, Smail N, Thicope M, Wiel E, Ricard-Hibon A, Berthier F, Gueugniaud P-Y, Riou B. Mechanism, Glasgow Coma Scale, age, and arterial pressure (mgap): a new simple prehospital triage score to predict mortality in trauma patients. Critical Care Medicine. 2010;38(3):831–837. doi: 10.1097/ccm.0b013e3181cc4a67. [DOI] [PubMed] [Google Scholar]
- Shapiro et al. (2003).Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in emergency department sepsis (meds) score: a prospectively derived and validated clinical prediction rule. Critical Care Medicine. 2003;31(3):670–675. doi: 10.1097/01.ccm.0000054867.01688.d1. [DOI] [PubMed] [Google Scholar]
- Steyerberg et al. (2008).Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, Murray GD, Marmarou A, Roberts I, Habbema JDF, Maas AIR. Predicting outcome after traumatic brain injury: Development and international validation of prognostic scores based on admission characteristics. PLOS Medicine. 2008;5(8):e165. doi: 10.1371/journal.pmed.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbe et al. (2001).Subbe C, Kruger M, Rutherford P, Gemmel L. Validation of a modified early warning score in medical admissions. QJM. 2001;94(10):521–526. doi: 10.1093/qjmed/94.10.521. [DOI] [PubMed] [Google Scholar]
- Tavares et al. (2008).Tavares RCF, Vieira AS, Uchoa LV, Peixoto Júnior AA, Meneses FAD. Validation of an early warning score in pre-intensive care unit. Revista Brasileira de Terapia Intensiva. 2008;20(2):124–127. [PubMed] [Google Scholar]
- Wang, Pan & Pan (2017).Wang G, Pan Z, Pan L. Analysis of the factors affecting the death of patients with multiple injuries in emergency. Tianjin Medical Journal. 2017;45:885–888. [Google Scholar]
- Wangara et al. (2019).Wangara AA, Hunold KM, Leeper S, Ndiawo F, Mweu J, Harty S, Fuchs R, Martin IBK, Ekernas K, Dunlop SJ, Twomey M, Maingi AW, Myers JG. Implementation and performance of the south african triage scale at kenyatta national hospital in nairobi, kenya. International Journal of Emergency Medicine. 2019;12(1):5. doi: 10.1186/s12245-019-0221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman et al. (2015).Wasserman EB, Shah MN, Jones CM, Cushman JT, Caterino JM, Bazarian JJ, Gillespie SM, Cheng JD, Dozier A. Identification of a neurologic scale that optimizes ems detection of older adult traumatic brain injury patients who require transport to a trauma center. Prehospital Emergency Care. 2015;19(2):202–212. doi: 10.3109/10903127.2014.959225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin, Liang & Liu (2015).Yin Q, Liang Y, Liu Z. Analysis of the emergency death risk factors and death causes for multiple trauma. Journal of Clinical Emergency. 2015;16:591–593. [Google Scholar]
- Yingcheng et al. (2014).Yingcheng X, Chaofang S, Yong X, Er L. Clinical analysis of emergency assessment and treatment of 216 severe multiple trauma patients. Modern Journal of Integrated Traditional Chinese and Western Medicine. 2014;23(19):2094–2097. [Google Scholar]
- Zadravecz et al. (2015).Zadravecz FJ, Tien L, Robertson-Dick BJ, Yuen TC, Twu NM, Churpek MM, Edelson DP. Comparison of mental-status scales for predicting mortality on the general wards. Journal of Hospital Medicine. 2015;10(10):658–663. doi: 10.1002/jhm.2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Hong & Gregory (2017).Zhang Z, Hong Y, Gregory JS. Trauma care in china: a systematic review. Journal of Emergency and Critical Care Medicine. 2017;1(11):33. doi: 10.21037/jeccm.2017.10.05. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
All variables related to MEWS and CRAMS calculation. Please refer to the CodeBook for the specific description of each variable (column label).
The meaning of each column label is described in this codebook.
Data Availability Statement
The following information was supplied regarding data availability:
All patient data are available in the Supplemental File.