Abstract
Objective:
Breast cancer risk is a chronic stressor associated with depression. Optimism is associated with lower levels of depression among breast cancer survivors. However, to our knowledge, no studies have explored the relationship between optimism and depression among women at risk for breast cancer. We hypothesized that women at risk for breast cancer who have higher levels of optimism would report lower levels of depression and that social support would mediate this relationship.
Method:
Participants (N = 199) with elevated distress were recruited from the community and completed self-report measures of depression, optimism, and social support. Participants were grouped based on their family history of breast cancer. Path analysis was used to examine the cross-sectional relationship between optimism, social support, and depressive symptoms in each group.
Results:
Results indicated that the variance in depressive symptoms was partially explained through direct paths from optimism and social support among women with a family history of breast cancer. The indirect path from optimism to depressive symptoms via social support was significant (β = −.053; 90% CI = −.099 to −.011, p = .037) in this group. However, among individuals without a family history of breast cancer, the indirect path from optimism to depressive symptoms via social support was not significant.
Conclusions:
These results suggest that social support partially mediates the relationship between optimism and depression among women at risk for breast cancer. Social support may be an important intervention target to reduce depression among women at risk for breast cancer.
Background
Optimism is a personality trait in which one generally expects positive outcomes [1]. Optimism has been linked to positive outcomes in numerous studies. For example, optimism is related to positive health outcomes and better mood [2,3]. In addition, optimism has been shown to be protective against depression among women facing chronic stressors, such as poverty [4] and cancer diagnosis and treatment [5]. Optimistic breast cancer survivors also report having better mental health [6,7]. Conversely, lower optimism has been found to predict higher levels of depression among cancer survivors [8,9]. Increased risk of cancer due to family history can be considered a chronic stressor [10], and optimism may be protective against depression that is associated with such stress. However, to our knowledge, no study has examined the relationship between optimism and depression among women with a family history of breast cancer (FH+).
FH+ women are at greater risk for elevated levels of distress than women in the general population [11,12]. One study, when comparing FH+ women to a similar group of women without family history of the disease (FH−), found that FH+ women were significantly more distressed even after receiving normal mammography results [13]. While it is clear that these women are at increased risk for distress, less is known about their risk for depression and the protective role of optimism in this population.
Social support is another protective factor for FH+ women and has been shown to predict lower levels of depression and general distress [14,15]. Research supports the notion that optimistic individuals are more likely to receive positive support from others compared with pessimistic individuals [16]. In addition, researchers have speculated that among breast cancer survivors, those who are more optimistic provide less stressful environments for their family and friends by not placing intense emotional demands on others, which leads to decreased overall distress [17]. Furthermore, significant others of breast cancer survivors are likely to withdraw their support if they are overwhelmed by their partner’s emotional needs [18]. Thus, it is likely easier to provide emotional support to optimistic women, resulting in lower levels of emotional distress.
Social support has been shown to mediate the relationship between optimism and general distress among breast cancer survivors [17]. In addition, studies have examined the relationships between social support, optimism, and emotional distress in other at-risk populations, such as those at risk for cardiovascular disease [19,20] and type 2 diabetes [21]. However, the relationship between social support, optimism, and emotional distress remains unclear among FH+ women. Both a cancer diagnosis and the risk of getting cancer are considered stressors, but the feelings associated with the risk of getting breast cancer in the future are not identical to the experience of survivorship, where women must cope with treatment-related stressors and the threat of recurrence [22]. Thus, it is important to examine how optimism and social support influence depression among FH+ women. Furthermore, while women cannot change their family history or a stable personality trait, such as optimism, they can improve their social support, making it an important area for intervention.
The purpose of the present study was to examine the relationships between optimism, social support, and depression among FH+ women. We hypothesized that (1) women with higher optimism would report lower levels of depression and (2) social support would mediate the relationship between optimism and depression.
Method
Participants
The present study is a secondary data analysis from a larger longitudinal study on the effect of a cognitive–behavioural stress management (CBSM) intervention on depressive symptoms, perceived stress, and cancer worry among women at risk for breast cancer [23]. Participants were recruited from the greater Seattle area through a variety of means: letters sent via mail, flyers posted in the community, newspaper and radio advertisements, community health events, brochures distributed at medical centres, word of mouth, and employee newsletters. Eligible participants were between the ages of 18 and 60 years, and reported having a healthy immune system and elevated levels of distress. Participants were considered FH+ if they reported having any family history of breast cancer. Elevated levels of distress were included as an inclusion criterion because individuals who are not experiencing elevated levels of distress were considered unlikely to benefit from an intensive CBSM intervention that was the focus of the larger longitudinal study. Participants were screened for elevated general or cancer specific distress using the four-item Perceived Stress Scale (PSS; [24]) and the Cancer Worry Scale [25]. Cut-off scores for both screening instruments were 0.5 standard deviation above the population mean for each instrument. Exclusion criteria included prior diagnosis of cancer or autoimmune disease, current major depressive episode, history of psychotic disorder, smoking, substance dependence, consuming more than 10 drinks of alcohol a week, and previous Hepatitis A diagnosis or vaccination. All study procedures were approved by the Fred Hutch Institutional Review Board.
Procedure
Eligible participants completed a self-report questionnaire prior to randomization and at four follow-up time points. For the present study, we analysed only baseline data.
Measures
Distress
The four-item PSS was used to screen for distress during a phone interview. The four-item version of the PSS was developed for screening and has validated community sample norms. In the present study, the cut-off score for distress screening was 6, based on the mean PSS for women aged 45–54 years (the mean age of the present sample) in a US normative sample (mean = 4.4, SD = 2.9; [24,26]).
Additionally, the Cancer Worry Scale was used during the phone screening interview to assess cancer specific distress. The Cancer Worry Scale is a four-item self-report measure designed to assess worry about the risk of breast cancer and the extent of interference it has on daily functioning [25]. Participants rate items on a scale of 1 (rarely or not at all) to 4 (a lot). In a community-based sample of women in the Seattle area, the mean total breast cancer worry score was 5.51 (SD = 1.62; [27]). The results from our previous work with this scale were used to generate a cut-off score of 7.
Optimism
Optimism was assessed using the Life Orientation Test Revised (LOT-R; [28]). The LOT-R has 10 items, six of which are active and four of which are fillers. Example items include ‘I hardly ever expect things to go my way’ and ‘If something can go wrong for me it will.’ Responses are measured on a Likert scale and range from 1 (I agree a lot) to 5 (I disagree a lot). The Cronbach’s alphas in the present samples are reported in Table 1.
Table 1.
Demographics
| Demographic variable | FH+ |
FH− |
|||||
|---|---|---|---|---|---|---|---|
| M | SD | % | M | SD | % | ||
| t (p) | |||||||
| Age | 43.79 | 10.55 | 42.61 | 12.56 | −.687 (.49) | ||
| Education (in years) | 16.86 | 2.38 | 17.09 | 3.10 | .559 (.58) | ||
| Pearson χ2 (p) | |||||||
| Marital status | 1.258 (.94) | ||||||
| Single | 39.8 | 41.6 | |||||
| Married | 39.8 | 36.4 | |||||
| Living with partner | 9.8 | 11.7 | |||||
| Separated | 0.8 | 1.3 | |||||
| Divorced | 7.3 | 9.1 | |||||
| Widowed | 0.8 | 0.0 | |||||
| Ethnicity | 2.57 (.63) | ||||||
| White | 82.9 | 79.2 | |||||
| African American | 4.9 | 7.8 | |||||
| Asian | 5.7 | 5.2 | |||||
| Other | 4.9 | 7.8 | |||||
Social support
We used the Interpersonal Support Evaluation List-12 to assess social support [29]. The measure has 12 items asking to what degree the participant agrees with each statement. Example items include ‘If I were sick, I could easily find someone to help me with my daily chores’ and ‘When I need suggestions on how to deal with a personal problem, I know someone I can turn to.’ Responses range from 0 (definitely false) to 3 (definitely true), and scores can range from 0 to 36. The Cronbach’s alphas in the present samples are reported in Table 1.
Depression
Depressive symptoms were evaluated using the Center for Epidemiologic Studies Depression Scale (CES-D; [30]). This 20-item measure was designed to assess depressed feelings and behaviours that have occurred in the past week. Examples of items include ‘I was bothered by things that don’t usually bother me’ and ‘My sleep was restless.’ The measure is scored on a four-point Likert scale (0 = rarely/never to 3 = most/all of the time), and scores range from 0 to 60. A clinical cut-off score of 16 is used to indicate people at greater risk for clinical depression. The CES-D has demonstrated good internal consistency in a wide range of populations, including breast cancer patients [31]. The Cronbach’s alphas in the present samples are reported in Table 2.
Table 2.
Means, standard deviations, correlations, and internal consistency
| FH+ |
FH− |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | LOT-R | ISEL | CES-D | M | SD | LOT-R | ISEL | CES-D | |
| LOT-R | 15.89 | 4.95 | .84 | 16.64 | 4.26 | .77 | ||||
| ISEL | 27.01 | 5.97 | .19* | .59 | 28.87 | 6.49 | .19 | .74 | ||
| CES-D | 14.51 | 8.89 | −.40** | −.35** | .88 | 10.93 | 7.98 | −.55** | −.46** | .61 |
Note. CES-D, Center for Epidemiologic Studies Depression Scale. ISEL, Interpersonal Support Evaluation List; LOT-R, Life Orientation Test Revised. Pearson correlations are presented below the diagonal.
denotes p < .05;
denotes p < .01. Cronbach’s alpha values are listed on the diagonal. FH+ and FH− individuals differed on ISEL, F(1, 197) = 4.26; p = .04, and CES-D scores, F(1, 197) = 8.21; p = .01, but not LOTR scores, F(1, 197) = 1.22; p = .27.
Data analytic plan
A cross-sectional analysis of the data was conducted. Data were analysed using path analysis via the statistical program SPSS Amos 22.0 (IBM SPSS Statistics for Windows, Version 22.0, IBM Corp., Armonk, NY, USA). Given that path analysis is based on analysis of co-variance and that kurtosis affects tests of variance and co-variance, we first evaluated the data for normality and the presence of outliers. All data were found to be normally distributed with no outliers present.
In addition, we conducted preliminary regression analyses to determine the need for control variables. Preliminary analyses did not indicate associations between demographic variables and the mediator or outcome variable; therefore, we did not control for any variables in the model. Next, we examined the correlations between optimism and depressive symptoms as well as between optimism and social support and between social support and depression.
Researchers frequently recommend that bootstrap sampling procedures be used to test for the significance of indirect effects in mediated models. This process involves using the sample as a population reservoir from which a large number of random samples are drawn and continuously replaced so that they have an equal likelihood of being randomly selected on all subsequent drawings [32]. In the present study, we specified 1000 bootstrap iterations using 90% bias-corrected confidence intervals and bootstrap estimates of indirect, direct, and total effects.
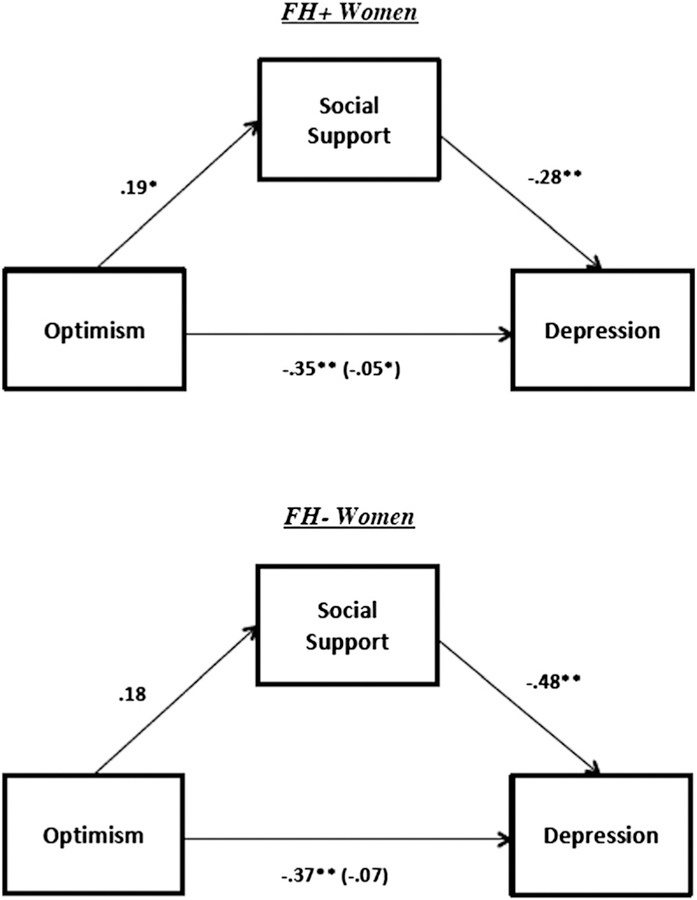
We examined the bivariate a, b, and c′ paths of the hypothesized mediated model, as well as the c (total effect) paths and indirect effects (Figure 1). A relationship is considered mediated if the indirect effect is statistically significant and if the direct effect decreases when the mediator is included in the model (i.e., when there is a decrease from the total effect, c, to c′, which includes the mediator). We examined the relationship between optimism and depressive symptoms with and without social support to determine whether social support functioned as a mediator. Additionally, we conducted a cross-sectional mediation analysis of the same variables on data collected from distressed women without a family history of breast cancer (FH−) for comparison. As there can be considerable bias in cross-sectional mediation, we also conducted two separate longitudinal mediations on the data from individuals who did and did not receive the stress management intervention.
Figure 1.
Among women with a family history of breast cancer (FH+), social support partially mediated the relationship between optimism and depression. However, among women without a family history of breast cancer (FH−), social support does not mediate the relationship between optimism and depression. Value inside parentheses indicates standardized beta for the indirect effect. *p < .05, **p < .01
Results
Participants were 199 mostly white FH+ and FH− women from the Seattle, Washington area. They ranged in age from 22 to 60 years. Demographic information can be found in Table 1.
Preliminary results
Descriptive statistics including means, standard deviations, and bivariate correlations among study variables are presented in Table 2. As expected, in the FH+ group, there were significant negative correlations between optimism and depression (r = −.40, p <.01) and between social support and depression (r = −.35, p <.01). Additionally, there was a significant positive correlation between social support and optimism in FH+ individuals (r = .19, p <.05). In the FH− group, there was a significant negative correlation between optimism and depression (r = −.55, p <.01) and between social support and depression (r = −.46, p <.01), but no significant correlation between optimism and social support (r = .19).
Primary results
The standardized results from the hypothesized model are shown in Table 3. Among FH+ women, all paths were significant, including the test of the indirect effect, or c–c′ path (β = −.053; 90% CI = −.099 to .011, p = .032). In addition, the total effects, or c paths (β = −.403; 90% CI = −.539 to .255, p = .002), of optimism on depression decreased and remained significant when controlling for social support (c′ paths; β = −.351; 90% CI = −.482 to .204, p <.002). The results of this analysis suggest that the relationship between optimism and depression is partially mediated by social support in FH+ women. However, among FH− women, there was not a significant relationship between optimism and social support (a path; β = .185; 90% CI = −.090 to .433, p = .102). The test of the indirect effect or c–c′ path was also not significant (β = −.069; 90% CI = −.179 to .030, p = .277). The results of this analysis suggest that the relationship between optimism and depression is not mediated by social support in FH− women. In addition, we conducted a longitudinal analysis to determine if optimism and social support predicted depression over time. None of the relationships were found to be significant, possibly because the participants had to be split into two separate groups (intervention and control) for this analysis, resulting in smaller sample sizes and a loss of power.
Table 3.
Hypothesized model—bootstrap results to test significance of main and indirect effects(standardized values)
| 90% CI |
|||||
|---|---|---|---|---|---|
| Path/effect | β | SE | Lower | Upper | p |
| FH+ | |||||
| a Optimism→social support | .188 | .092 | .043 | .345 | .035* |
| b Social support→depression | −.281 | .078 | −.396 | −.146 | .002** |
| c Optimism→depression | −.403 | .085 | −.539 | −.255 | .002** |
| c′ Optimism→depression | −.351 | .085 | −.482 | −.204 | .002** |
| c–c′ Optimism→ depression | −.053 | .028 | −.099 | −.011 | .037* |
| FH− | |||||
| a Optimism→social support | .185 | .158 | −.090 | .433 | .102 |
| b Social support→depression | −.479 | .105 | −.596 | −.346 | .002** |
| c Optimism→depression | −.547 | .097 | −.687 | −.365 | .002** |
| c′ Optimism→depression | −.370 | .077 | −.535 | −.178 | .002** |
| c–c′ Optimism→depression | −.069 | .065 | −.179 | .030 | .277 |
p < .05;
p < .01.
Conclusions
In this study, we tested the relationship between optimism, social support, and depression among FH+ women. Both our primary hypothesis and our secondary hypothesis were supported. Specifically, greater optimism predicted lower levels of depression, and the total effects of optimism on depression decreased and remained significant when controlling for social support. Thus, our results suggest that the relationship between optimism and depression is partially mediated by social support in FH+ women but not in FH− women. To our knowledge, ours is the first study to report that social support mediates the relationship between optimism and depression in this population.
Although our study is the first to investigate this relationship specifically among FH+ women, the present findings are consistent with the established bodies of literature on distress among FH+ women and the relationships among optimism, social support, and depression. First, several studies have indicated that FH+ women are at a greater risk for general and chronic psychological distress, including depression [10–13]. Depression is an important outcome in populations with health concerns as it is a common reaction to the threat of long-term and potentially fatal diseases [33] and may have deleterious effects on physical health [34]. Second, multiple studies have explored the relationships among optimism, social support, and depression in other populations. Optimism has previously been shown to be protective against depression in individuals experiencing chronic stress [4,5], and social support has been shown to mediate the relationship between optimism and distress among breast cancer survivors [17]. Our findings corroborate previous research that demonstrates the relationships among optimism, social support, and depression, and extends these findings to a new population, FH+ women, who are thus at a greater risk for depression and negative physical health outcomes. Additionally, by testing this model in both FH+ and FH− women, we have demonstrated that individuals’ social support may play an especially important role in preventing symptoms of depression among women with a family history of breast cancer.
There are several limitations that should be noted when interpreting the results of this study. The primary limitation of this study is that it is correlational in nature. Data were collected in a cross-sectional manner and analysed using path analysis. Additional longitudinal analyses did not reveal a significant outcome, which may be because of a loss of power. Although it is clear that there are significant relationships among social support, optimism, and depression, it cannot be concluded that optimism and strong social support cause lower levels of depression. Future studies should conduct longitudinal analyses of these variables with larger samples over a longer period of time to allow for greater change in social support. Although we were able to demonstrate a difference between FH+ and FH− women, this too may be due to a loss of power, as we had fewer FH− participants. Additionally, depression may adversely affect social support. The nature of the relationships among optimism, social support, and depression is likely bidirectional; however, testing these bidirectional relationships was beyond the scope of the present study. It must also be noted that participants were volunteers recruited from the greater Seattle area. This increases the possibility that there is a bias present in the sample and reduces the generalizability of our results. Additionally, because all key variables were assessed using self-report measures, the validity of our results may have been affected by social desirability bias, demand characteristics, and under or over reporting of symptoms. Lastly, while some research suggests that anxiety is a key variable to study in FH+ women, examining anxiety in addition to depression was beyond the scope of the current study; therefore, future studies would benefit from including anxiety as an outcome measure.
Bearing these limitations in mind, the present study has important implications for research and practice in the area of health psychology. Improving social support is easier than changing optimism and may be an effective intervention to reduce depressive symptoms among FH+ women. Future research should develop and test interventions to increase social support with a goal of reducing depression among FH+ women. This would provide a framework from which clinicians could address the issues specific to this population and allow for the determination of a causal relationship among social support, optimism, and depression.
Footnotes
Supporting Information
Additional supporting information may be found in the online version of this article at the publisher’s web site.
References
- 1.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 1985;4(3):219–247. DOI: 10.1037/0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 2.Scheier MF, Carver CS. Effects of optimism on psychological and physical well-being: theoretical overview and empirical update. Cognit Ther Res 1992;16(2):201–228. DOI: 10.1007/BF01173489. [DOI] [Google Scholar]
- 3.Segerstrom SC, Taylor SE, Kemeny ME, Fahey JL. Optimism is associated with mood, coping, and immune change in response to stress. J Pers Soc Psychol 1998;74(6):1646–1655. DOI: 10.1037/0022-3514.74.6.1646. [DOI] [PubMed] [Google Scholar]
- 4.Grote NK, Bledsoe SE, Larkin J, Lemay ER, Brown C. Stress exposure and depression in disadvantaged women: the protective effects of optimism and perceived control. Soc Work Res 2007;31(1):19–33. DOI: 10.1093/swr/31.1.19. [DOI] [Google Scholar]
- 5.Gustavsson-Lilius MM, Julkunen JJ, Keskivaara PP, Lipsanen JJ, Hietanen PP. Predictors of distress in cancer patients and their partners: the role of optimism in the sense of coherence construct. Psychol Health 2012;27(2):178–195. DOI: 10.1080/08870446.2010.484064. [DOI] [PubMed] [Google Scholar]
- 6.Carver CS, Smith RG, Antoni MH, Petronis VM, Weiss S, Derhagopian RP. Optimistic personality and psychosocial well-being during treatment predict psychosocial well-being among long-term survivors of breast cancer. Health Psychol 2005;24(5):508–516. DOI: 10.1037/0278-6133.24.5.508. [DOI] [PubMed] [Google Scholar]
- 7.Colby DA, Shifren K. Optimism, mental health, and quality of life: a study among breast cancer patients. Psychol Health Med 2013;18(1):10–20. DOI: 10.1080/13548506.2012.686619. [DOI] [PubMed] [Google Scholar]
- 8.Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rosenfeld B, Breitbart W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psycho-Oncology 2014;23(3):299–306. DOI: 10.1002/pon.3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zenger M, Brix C, Borowski J, Stolzenburg J, Hinz A. The impact of optimism on anxiety, depression and quality of life in urogenital cancer patients. Psycho-Oncology 2010;19 (8):879–886. DOI: 10.1002/pon.1635. [DOI] [PubMed] [Google Scholar]
- 10.Valdimarsdottir HB, Zakowski SG, Gerin W, Mamakos J, Pickering T, Bovbjerg DH. Heightened psychobiological reactivity to laboratory stressors in healthy women at familial risk for breast cancer. J Behav Med 2002;25(1):51–65. DOI: 10.1023/A:1013589718212. [DOI] [PubMed] [Google Scholar]
- 11.Erblich J, Bovbjerg DH, Valdimarsdottir HB. Looking forward and back: distress among women at familial risk for breast cancer. Ann Behav Med 2000;22(1):53–59. DOI: 10.1007/BF02895167. [DOI] [PubMed] [Google Scholar]
- 12.den Heijer M, Seynaeve C, Vanheusden K, et al. Long-term psychological distress in women at risk for hereditary breast cancer adhering to regular surveillance: a risk profile. Psycho-Oncology 2013;22(3):598–604. DOI: 10.1002/pon.3039. [DOI] [PubMed] [Google Scholar]
- 13.Valdimarsdottir HB, Bovbjerg DH, Kash K. Psychological distress in women with a familial risk of breast cancer. Psycho-Oncology 1995;4 (2):133–141. DOI: 10.1002/pon.2960040207. [DOI] [Google Scholar]
- 14.Holahan CJ, Moos RH. Social support and psychological distress: a longitudinal analysis. J Abnorm Psychol 1981;90(4):365–370. DOI: 10.1037/0021-843X.90.4.365. [DOI] [PubMed] [Google Scholar]
- 15.Symister P, Friend R . The influence of social support and problematic support on optimism and depression in chronic illness: a prospective study evaluating self-esteem as a mediator. Health Psychol 2003;22(2):123–129. DOI: 10.1037/0278-6133.22.2.123. [DOI] [PubMed] [Google Scholar]
- 16.Carver CS, Kus LA, Scheier MF. Effects of good versus bad mood and optimistic versus pessimistic outlook on social acceptance versus rejection. J Soc Clin Psychol 1994;13(2):138–151. DOI: 10.1521/jscp.1994.13.2.138. [DOI] [Google Scholar]
- 17.Trunzo JJ, Pinto BM. Social support as a mediator of optimism and distress in breast cancer survivors. J Consult Clin Psychol 2003;71(4):805–811. DOI: 10.1037/0022-006X.71.4.805. [DOI] [PubMed] [Google Scholar]
- 18.Bolger N, Foster M, Vinokur AD, Ng R. Close relationships and adjustment to a life crisis: the case of breast cancer. J Pers Soc Psychol 1996;70(2):283–294. DOI: 10.1037//0022-3514.70.2.283. [DOI] [PubMed] [Google Scholar]
- 19.Aggarwal B, Ming L, Allegrante JP, Mosca L. Low social support level is associated with non-adherence to diet at 1 year in the Family Intervention Trial for Heart Health (FIT Heart). J Nutr Educ Behav 2010;42(6):380–388. DOI: 10.1016/j.jneb.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen E, Lee WK, Cavey L, Ho A. Role models and the psychological characteristics that buffer low-socioeconomic-status youth from cardiovascular risk. Child Dev 2013;84 (4):1241–1252. DOI: 10.1111/cdev.12037. [DOI] [PubMed] [Google Scholar]
- 21.Razee H, van der Ploeg H, Blignault I, et al. Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promot J Aust 2010;21(2):130–137. [DOI] [PubMed] [Google Scholar]
- 22.Kenen R, Ardern-Jones A, Eeles R. Living with chronic risk: healthy women with a family history of breast/ovarian cancer. Health Risk Soc 2003;5(3):315–331. DOI: 10.1080/13698570310001607003. [DOI] [Google Scholar]
- 23.McGregor BA, Dolan ED, Highland KB. Stress management reduces distress among healthy women at risk for breast cancer, a randomized, controlled trial [abstract]. Psychosom Med 2013;75(3):A100. [Google Scholar]
- 24.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In The Social Psychology of Health: Claremont Symposium on Applied Social Psychology, Spacapan S, Oskamp S (eds.), Sage: Newbury Park, CA, 1988;31–67. [Google Scholar]
- 25.Lerman C, Trock B, Rimer BK, Jepson C, Brody D, Boyce A. Psychological side effects of breast cancer screening. Health Psychol 1991;10(4):259 DOI: 10.1037//0278-6133.10.4.259. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24(4):385–396. DOI: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 27.McGregor BA, Antoni MH, Boyers A, Alferi SM, Blomberg BB, Carver CS. Cognitive–behavioral stress management increases benefit finding and immune function among women with early-stage breast cancer. J Psychosom Res 2004;56(1):1–8. DOI: 10.1016/S0022-3999(03)00036-9. [DOI] [PubMed] [Google Scholar]
- 28.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67(6):1063–1078. DOI: 10.1037/0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Underwood L, Gottlieb B (Eds). Social Support Measurement and Interventions: A Guide for Health and Social Scientists, Oxford: New York, 2000. [Google Scholar]
- 30.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385–401. DOI: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 31.Hann D, Winter K, Jacobsen P . Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). J Psychosom Res 1999;46 (5):437–443. DOI: 10.1016/S0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 32.Mallinckrodt B, Abraham W, Wei M, Russell DW. Advances in testing the statistical significance of mediation effects. J Couns Psychol 2006;53(3):372–378. DOI: 10.1037/0022-0167.53.3.372. [DOI] [Google Scholar]
- 33.Wellisch DK, Lindberg NM. A psychological profile of depressed and nondepressed women at high risk for breast cancer. Psychosomatics 2001;42(4):330–336. [DOI] [PubMed] [Google Scholar]
- 34.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol psychiatry 2003;54(3):216–226. [DOI] [PubMed] [Google Scholar]