Abstract
Background
Multimorbidity is common among older adults and strongly associated with physical functioning decline and increased mortality. However, the full spectrum of direct and indirect effects of multimorbidity on physical functioning and survival has not been quantified. We aimed to determine the longitudinal relationship of multimorbidity on physical functioning and quantify the impact of multimorbidity and multimorbidity-attributed changes in physical functioning on mortality risk.
Methods
The Health and Retirement Study (HRS) is a nationally representative population-based prospective cohort of adults aged 51 or older. In 2000, participants were interviewed about physician-diagnosed chronic conditions, from which their multimorbidity-weighted index (MWI) was computed. Between 2000 and 2011, participants reported their current physical functioning using a modified Short Form-36. With MWI as a time-varying exposure, we jointly modeled its associations with physical functioning and survival.
Results
The final sample included 74,037 observations from 18,174 participants. At baseline, participants had a weighted mean MWI of 4.6 ± 4.2 (range 0–36.8). During follow-up, physical functioning declined: −1.72 (95% confidence interval [CI] −1.77, −1.67, p < .001) HRS physical functioning units per point MWI in adjusted models. Over follow-up, 6,362 (34%) participants died. Mortality risk increased 8% (hazard ratio 1.08, 95% CI 1.07–1.08, p < .001) per point MWI in adjusted models. Across all population subgroups, MWI was associated with greater physical functioning decline and mortality risk.
Conclusions
Multimorbidity and its associated decline in physical functioning were significantly associated with increased mortality. These associations can be predicted with an easily interpreted and applied multimorbidity index that can better identify and target adults at increased risk for disability and death.
Keywords: Multiple chronic conditions, Comorbidity, Functional status, Joint modeling, Survival
Introduction
Multimorbidity is common in older adults (1) and has profound consequences for patients, families, and health care systems. Adults with multimorbidity experience declines in physical functioning, decreased health-related quality of life, and increased disability and mortality risk (2,3). Multimorbidity is commonly measured using simple disease counts or traditional comorbidity indices that weight diseases by mortality risk in hospitalized patients (4,5). However, physical functioning, a universally valued outcome, is increasingly being recognized by health care systems and payers as a key measure of healthcare quality and value.
Top research priorities for older adults with multimorbidity include health-related quality of life; tools to capture function, quality of life, and symptom burden; and disability (6). To help address these priorities, a better understanding of the relationship between multimorbidity and current and future physical functioning is needed. Physical functioning is strongly associated with mortality (7–9), but less is known about how it may act as a mediator between multimorbidity and mortality. We postulate that the full impact of multimorbidity includes the concomitant processes of multimorbidity accumulation and functional decline.
Multimorbidity is strongly associated with physical functioning, mobility limitations, and mortality (2,10–12), where more conditions and greater disease severity predict worse outcomes (12). Such associations have typically been examined separately (2,10,11). However, multimorbidity and physical functioning are dynamic and change over time. On average, multimorbidity increases while physical functioning declines with aging. Failure to account for the impact of multimorbidity-related deficits in physical functioning on mortality could underestimate the true impact of multimorbidity on mortality. The dynamic nature of this association has not been assessed in previous studies using a mediation framework (13) with repeated measurements of both constructs.
Thus, we sought to disentangle the pathway between multimorbidity and mortality by examining physical functioning as a mediator of this association. First, we determined the longitudinal effects of multimorbidity and other predictors on physical functioning using a newly developed and validated multimorbidity-weighted index (MWI) for community-dwelling adults with chronic conditions (3,14). Next, we quantified the impact of these multimorbidity-attributed changes in physical functioning on mortality risk. We employed a joint modeling approach and compared results with classic separate and two-stage methods. Finally, we used joint modeling to examine multimorbidity with long-term physical functioning and mortality within participant subgroups. We hypothesized that multimorbidity would have direct and indirect effects on mortality through its longitudinal impact on physical functioning.
Methods
Study Population
The Health and Retirement Study (HRS) is an ongoing population-based prospective cohort study of more than 38,000 U.S. adults aged 51 and older followed since 1992. Biennially, participants complete questionnaires on physician-diagnosed medical conditions, functional status, health behaviors, living situation, household income, employment, and health insurance status, described previously (15).
Beginning in the 2000 cohort wave (interview field date February 2000–January 2001) and biennially until the 2010 cohort wave (interview field date February 2010–November 2011), participants were interviewed about physician-diagnosed chronic conditions, from which their MWI was computed. Participants also reported their physical functioning using a modified Short Form (SF)-36 physical functioning scale (range 0–100). We identified 18,612 participants in the 2000 interview. Of these eligible respondents, 194 (1.0%) were missing covariates of interest and 244 (1.3%) had no follow-up observations and were thus excluded. We conducted a sensitivity analysis of included and excluded participants. The final descriptive and multivariate analyses were based on a sample of 18,174 participants who were nationally representative of more than 64.3 million U.S. adults aged 52 years and older in 2000.
Multimorbidity Assessment
We measured multimorbidity using a newly developed and validated MWI described previously (3,14). Briefly, chronic conditions were weighted by their cross-sectional association with the SF-36 physical functioning scale and then summed to form each individual’s MWI at baseline and each biennial wave (Supplementary Appendix 1). A major strength of MWI is its easy, two-fold clinical interpretation: each one-point increase in MWI represents a one-point decrease in the SF-36 physical functioning scale as well as an individual’s present overall burden of chronic diseases. To place these results in context, the effect of one point in current MWI on 4- to 8-year physical functioning was approximately equal to 3–4 additional years of age (2).
For the present analysis, we applied our previously established MWI weights (Supplementary Table 1) to conditions reported biennially between 2000 and 2011 to create a baseline and cumulative updated MWI for each participant. Conditions in the MWI for this study included self-reported physician-diagnosed conditions assessed in the HRS including dementia, stroke, chronic lung disease, hypertension, angina, myocardial infarction, congestive heart failure, arrhythmia, other heart condition, diabetes, cancer excluding skin cancer, arthritis, knee replacement, hip replacement, connective tissue disease, and glaucoma. MWI was assessed as a discrete time-varying covariate in models predicting physical functioning and mortality.
Physical Functioning Assessment
A physical functioning scale resembling the SF-36 10-item physical functioning scale (16) was constructed in the HRS using methods described previously (3). Briefly, we used nine physical functioning items equivalent to the SF-36 physical functioning scale and imputed the 10th item “walking more than a mile” that was intermediate between two questions assessed in the HRS, “walking several blocks” and “running/jogging about a mile.” The final 10 physical functioning items included vigorous activities such as running, moderate activities such as pushing large objects, lifting or carrying over 10 pounds, climbing several flights of stairs, climbing one flight of stairs, kneeling or stooping, walking more than a mile, walking several blocks, walking one block, and bathing or dressing oneself. For the HRS physical functioning measure to be comparable to the SF-36, we weighted items according to the SF-36 physical functioning equivalents, rescaled, and standardized the score according to the SF-36 protocol (16). The final HRS physical functioning scale was based on 10 items and ranged from 0 to 100, where 100 represents no difficulty performing any physical functioning item and 0 represents difficulty with all items.
We examined long-term physical functioning every 2 years between 2000 and 2011. Given the hypothesized correlation between the MWI (which weights diseases by concurrent physical functioning) and trajectory function of physical functioning as a mediator of the association between the MWI and mortality, we assessed for potential multicollinearity by computing the variance inflation factor in the regression models (17).
Mortality Assessment
At the end of each biennial wave, reported deaths were recorded and attempts were made to contact next-of-kin for post-mortem interviews. The National Death Index was also searched for death information, including cause of death. Linkage to the National Death Index was complete through the end of 2011. Individuals lost to follow-up and who survived beyond 2011 were censored based on the last date of known contact. Loss to follow-up was minimal due to comprehensive tracking interviews with next-of-kin and National Death Index (97% deaths) data (18).
Covariate Assessment
We assessed the distribution of baseline continuous and categorical variables through the mean, SD, and proportions. Baseline covariates included age (continuous), sex, race/ethnicity (white, black, Hispanic, other), body mass index (BMI <18.5, 18.5–24.9, 25–30, ≥30 kg/m2), smoking status (never, past, current), education (<12, 12, 13–15, ≥16 years), household net worth (quartiles), and marital/living status (married or living with a domestic partner, unmarried and living with someone other than a domestic partner such as a child or parent, and unmarried and living alone). For participants missing one or more values for BMI (N = 70), we used mean imputation for the missing observations. Participants missing smoking status (N = 121) and race/ethnicity (N = 3) were of similar age but more likely to be male, Hispanic, and overweight or obese. There were no significant differences by MWI or physical functioning at baseline (Supplementary Table 2), and as such, we excluded these participants.
Statistical Analysis
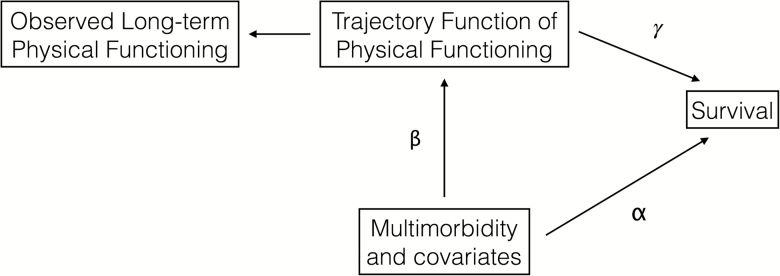
We used joint modeling to simultaneously model the association between multimorbidity with physical functioning and survival (19). Basic joint model components included 1) the longitudinal association between MWI and other predictors on physical functioning using linear mixed effects with random intercept and slope, and 2) the Weibull model for survival (20). In the causal diagram (Figure 1) and Supplementary Appendix 2, the direct effect of MWI (adjusted for baseline covariates) on survival is denoted as α. The direct effect of MWI and covariates on the longitudinal trajectory of physical functioning is denoted as β. The impact of multimorbidity-related changes in physical functioning on survival is denoted as γ. γ is the indirect effect of predictors of the longitudinal physical functioning trajectory on survival, whereby physical functioning serves as a mediator of the multimorbidity–mortality association. With joint modeling, we determined the direct (α), indirect (γ), and overall effect (βγ + α) of MWI and covariates on survival (21). We presented the association between MWI and covariates on physical functioning as regression coefficients and overall effect of MWI on survival as hazard ratios (HRs), all with 95% confidence intervals (CIs).
Figure 1.
Causal diagram for joint modeling of multimorbidity on long-term physical functioning and mortality. α, direct effect of multimorbidity (adjusted for covariates) on survival. β, direct effect of multimorbidity (adjusted for covariates) on long-term physical functioning, also referred to as the ‘trajectory function of physical functioning’. The trajectory function of physical functioning may be considered as a mediator of the association between multimorbidity and survival. γ, indirect effect of association between predictors (multimorbidity and covariates) and long-term physical functioning trajectory model on survival adjusted for predictors (multimorbidity and covariates). A value of γ = 0 implies the trajectory function of physical functioning has no significant effect on survival and thus there is no improvement of using joint modeling over separate survival analysis. A value of γ <0 implies that the hazard ratio decreases and that better physical functioning is protective for survival. The overall (direct and indirect) effect of multimorbidity on survival is denoted as βγ + α.
We also used joint modeling to examine the simultaneous association between multimorbidity, physical functioning, and mortality for population subgroups. We again examined MWI as a continuous, time-varying covariate adjusted for baseline covariates and presented the regression coefficient for physical functioning and HR for mortality (with 95% CIs) for each point increase in MWI.
To assess the robustness and efficiency of the joint modeling, we compared results obtained from 1) separate longitudinal and survival methods and 2) two-stage modeling, and compared these results with those obtained from joint modeling. First, we performed classical linear mixed-effects models to determine the association between MWI and physical functioning after adjusting for covariates, using a random intercept and slope. Similarly, we examined the Weibull regression model (20) (and confirmed results with the Cox proportional hazards model (22) to determine the association between MWI with mortality. Second, we compared results obtained from two-stage modeling. In the two-stage modeling, we added predicted physical functioning obtained from the linear mixed-effects model (stage one) as a covariate in the multimorbidity and survival association using the Weibull model (stage two). For all comparison models and the joint model, MWI was a continuous time-varying covariate adjusted for baseline covariates. Finally, we used the Kaplan–Meier estimator to determine survival estimates across MWI quartiles at baseline. All hypothesis tests were two-sided and conducted using STATA, version 14.0 (StataCorp, College Station, TX, 2015).
Results
Participant Characteristics
In 2000, 18,612 participants completed a questionnaire on physical functioning and self-reported physician-diagnosed chronic conditions, from which their MWI was computed. The final sample included 18,174 participants who contributed a mean of 4.1 (SD 1.4) observations during follow-up. Participants had a mean MWI of 4.6 (SD 4.4) (Table 1). Over follow-up, there were 6,351 (34%) deaths.
Table 1.
Participant Characteristics in the Health and Retirement Study (HRS) at Baseline in 2000, Adjusted for the HRS Complex Sampling Design
| Characteristic, Range | HRS, N = 18,174 | ||
|---|---|---|---|
| No. (%) | Mean | SD | |
| Age, years | 66.7 | 10.4 | |
| Sex, female | 10,404 (55.5) | ||
| Race/ethnicity | |||
| White | 13,931 (82.3) | ||
| Black | 2,505 (9.3) | ||
| Hispanic | 1,386 (6.3) | ||
| Other | 352 (2.1) | ||
| Body mass index, kg/m2 | 27.1 | 5.4 | |
| <18.5 | 399 (2.1) | ||
| 18.5–24.9 | 6,264 (34.4) | ||
| 25–29.9 | 7,157 (39.5) | ||
| ≥ 30 | 4,354 (24.1) | ||
| Smoking status | |||
| Never smoker | 7,499 (40.7) | ||
| Past smoker | 8,006 (43.7) | ||
| Current smoker | 2,666 (15.6) | ||
| Education, years | 12.3 | 3.2 | |
| <12 | 5,417 (26.2) | ||
| 12 | 6,124 (33.9) | ||
| 13–15 | 3,360 (19.7) | ||
| ≥16 | 3,273 (20.3) | ||
| Household net worth, $ | 306,970 | 928,359 | |
| ≤14,000 | 3,059 (16.1) | ||
| 14,001–113,000 | 5,862 (31.1) | ||
| 113,001–323,700 | 5,232 (29.5) | ||
| ≥323,701 | 4,021 (23.3) | ||
| Marital status/living arrangement | |||
| Married and/or living with domestic partner | 11,849 (63.5) | ||
| Unmarried and living with someone other than domestic partner |
2,032 (11.5) | ||
| Unmarried and living alone | 4,293 (25.0) | ||
| Multimorbidity-weighted index, 0–36.8 | 4.6 | 4.2 | |
| Chronic conditions, number, 0–12 | 2.1 | 1.5 | |
| HRS physical functioning scale, 0–100 | 65.2 | 30.8 | |
Joint Modeling of Multimorbidity, Physical functioning, and Mortality
Multimorbidity had both direct and indirect effects, through physical functioning, on mortality. The direct effect of multimorbidity on survival (α) was a 3% increased risk of mortality per point increase in MWI in the adjusted model (HR 1.03; 95% CI 1.03, 1.04, p < .001). There was no evidence of multicollinearity between the MWI and trajectory function of physical functioning association (variance inflation factor of 1.9 in unadjusted models; variation inflation factor of 1.4 in adjusted models).
Multimorbidity also had a significant indirect effect on mortality through its association with long-term physical functioning. Each point increase in MWI was associated with a 2-point decline in long-term physical functioning in the unadjusted model (β = −2.02, 95% CI −2.07, −1.97, p < .001) with some attenuation in the adjusted model (β = −1.72, 95% CI −1.77, −1.67, p < .001) (Table 2). To place these results in context, each point increase in current MWI was associated with a 10-year physical functioning decline approximately equal to aging by 2.5 years (assuming no additional increase in MWI or change in covariates over that time). A better physical functioning trajectory was associated with decreased mortality risk after adjusting for other covariates: the indirect effect of physical functioning on mortality was γ = −0.03 (95% CI −0.03, −0.02, p < .001). Thus, the overall association of multimorbidity with mortality, accounting for direct and indirect effects, was a 10% higher mortality risk per point increase in MWI (HR 1.10, 95% CI 1.09, 1.10, p < .001), with attenuation to 8% in the adjusted model (HR 1.08, 95% CI 1.07, 1.08, p < .001) (Table 3).
Table 2.
Effect of Time-Varying Multimorbidity and Baseline Covariates on Longitudinal Physical Functioning Trajectory Using Joint Modeling
| Model Predictors | β Coefficient (95% CI) | p Value |
|---|---|---|
| Multimorbidity-weighted index | −1.72 (−1.77, −1.67) | <.001 |
| Age, years | −1.00 (−1.03, −0.96) | <.001 |
| Years since baseline | −0.70 (−0.76, −0.64) | <.001 |
| Sex, female | −9.67 (−10.35, −8.98) | <.001 |
| Race/ethnicity | ||
| Black | 0.06 (−0.92, 1.04) | .909 |
| Hispanic | 0.22 (−1.04, 1.47) | .736 |
| Other | −0.39 (−2.67, 1.89) | .735 |
| White (reference) | 0 | |
| Body mass index, kg/m2 | ||
| <18.5 | −10.46 (−12.75, −8.16) | <.001 |
| 18.5–24.9 (reference) | 0 | |
| 25–29.9 | −1.72 (−2.46, −0.98) | <.001 |
| ≥ 30 | −10.90 (−11.77, −10.03) | <.001 |
| Smoking status | ||
| Never smoker | 0 | |
| Past smoker | −1.62 (−2.32, −0.92) | <.001 |
| Current smoker | −6.30 (−7.29, −5.30) | <.001 |
| Education, years | ||
| <12 (reference) | 0 | |
| 12 | 4.59 (3.75, 5.43) | <.001 |
| 13–15 | 5.49 (4.51, 6.48) | <.001 |
| ≥16 | 7.29 (6.25, 8.33) | <.001 |
| Household net worth, $ | ||
| ≤14,000 (reference) | 0 | |
| 14,001–113,000 | 7.16 (6.18, 8.15) | <.001 |
| 113,001–323,700 | 11.59 (10.51, 12.67) | <.001 |
| ≥323,701 | 13.86 (12.68, 15.04) | <.001 |
| Marital status/living arrangement | ||
| Married and/or living with domestic partner (reference) | 0 | |
| Unmarried and living with someone other than domestic partner | −2.55 (−3.65, −1.45) | <.001 |
| Unmarried and living alone | −0.95 (−1.79, −0.11) | .027 |
Note: CI = confidence interval.
Table 3.
Overall (direct and indirect) Effect of Time-Varying Multimorbidity and Baseline Covariates on Mortality Using Joint Modeling
| Model Predictors | HR (95% CI) | p Value |
|---|---|---|
| Multimorbidity-weighted index | 1.08 (1.07, 1.08) | <.001 |
| Age, years | 1.09 (1.08, 1.09) | <.001 |
| Sex, female | 0.63 (0.60, 0.67) | <.001 |
| Race/ethnicity | ||
| Black | 1.02 (0.94, 1.11) | .587 |
| Hispanic | 0.89 (0.80, 0.99) | .039 |
| Other | 0.89 (0.72, 1.09) | .245 |
| White (reference) | 1.0 | |
| Body mass index, kg/m2 | ||
| <18.5 | 2.27 (1.99, 2.60) | <.001 |
| 18.5–24.9 (reference) | 1.0 | |
| 25–29.9 | 0.76 (0.72, 0.81) | <.001 |
| ≥ 30 | 0.81 (0.75, 0.88) | <.001 |
| Smoking status | ||
| Never smoker (reference) | 1.0 | |
| Past smoker | 1.21 (1.14, 1.28) | <.001 |
| Current smoker | 1.80 (1.65, 1.96) | <.001 |
| Education, years | ||
| <12 (reference) | 1.0 | |
| 12 | 0.90 (0.84, 0.96) | .002 |
| 13–15 | 0.85 (0.78, 0.92) | <.001 |
| ≥16 | 0.85 (0.78, 0.93) | <.001 |
| Household net worth, $ | ||
| ≤14,000 (reference) | 1.0 | |
| 14,001–113,000 | 0.79 (0.73, 0.85) | <.001 |
| 113,001–323,700 | 0.68 (0.62, 0.74) | <.001 |
| ≥323,701 | 0.58 (0.53, 0.64) | <.001 |
| Marital status/living arrangement | ||
| Married and/or living with domestic partner (reference) | 1.0 | |
| Unmarried and living with someone other than domestic partner | 1.20 (1.10, 1.31) | <.001 |
| Unmarried and living alone | 1.19 (1.11, 1.27) | <.001 |
Note: CI = confidence interval; HR = hazard ratio.
We also examined the effect of other covariates on physical functioning and mortality using joint modeling. Women had on average nearly a 10-point lower physical functioning score than men (β = −9.67, 95% CI −10.35, −8.98, p < .001) (Table 2) but also a 37% lower mortality risk (Table 3). Underweight and obese adults also had a 10-point lower physical functioning score compared with adults with a normal BMI (Table 2). Underweight (likely a proxy for poor health) was associated with increased mortality risk, while overweight and obesity were not (Table 3). Older age, smoking (past and current), and being unmarried were associated with significantly worse physical functioning (Table 2) and greater mortality risk (Table 3). In contrast, higher education and household net worth were associated with a monotonic increase in physical functioning (Table 2) and decrease in mortality risk (Table 3).
Results obtained from subgroup analyses of participant characteristics for the joint multimorbidity, physical functioning, and mortality associations did not differ greatly from those obtained from the overall cohort. Physical functioning declined with increasing MWI for all subgroups of participants (all p < .001) (Supplementary Table 3). Participants in all subgroups had more than a 1-point decrease in physical functioning for each point increase in MWI. Results were nearly identical to those obtained for the overall cohort in Table 2. Similarly, mortality risk increased with greater MWI for participants in all subgroups (all p < .001) (Supplementary Table 4). Each point increase in MWI was associated with a 7%–10% increased mortality risk that was similar to the 8% increased mortality risk observed for the overall cohort (Table 2).
Multimorbidity and Physical Functioning: Comparison With Classic Linear Mixed-Effects Models
Multimorbidity was significantly associated with long-term physical functioning using separate linear mixed-effects models. Each point increase in MWI was associated with a 1.70-point decline in future long-term physical functioning (β = −1.70, 95% CI −1.74, −1.65, p < .001) in the adjusted model (Supplementary Table 5).
Multimorbidity and Mortality: Comparison With Classic Survival Analysis and Two-Stage Modeling
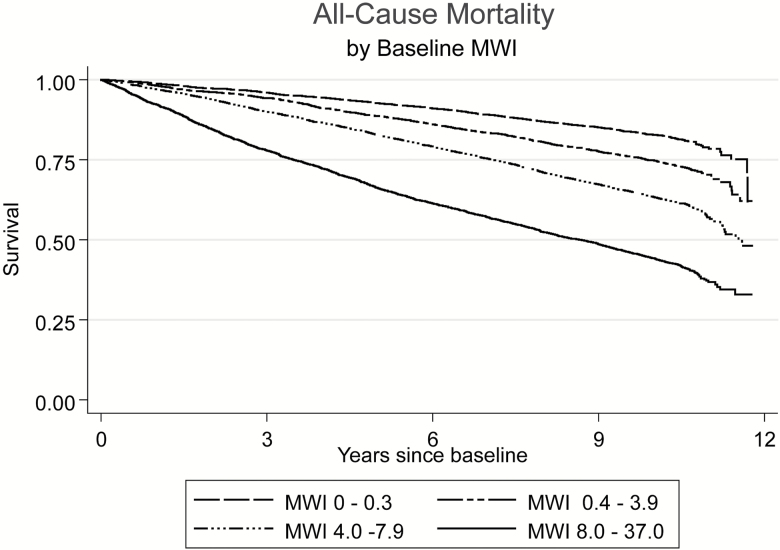
Classic Weibull hazard regression demonstrated that for each point increase in MWI, the hazard of mortality was 1.04 (95% CI 1.04, 1.05, p < .001) in the adjusted model. The Cox proportional hazard model estimate and error were identical to those obtained using the Weibull model. For increasing MWI quartiles at baseline, there was a dose–response relationship with hazard rates of mortality, as shown in the Kaplan–Meier survival curve (Figure 2).
Figure 2.
Kaplan–Meier survival curves for mortality by multimorbidity-weighted index (MWI) quartiles at baseline in 2000. Participants were followed from the 2000 to 2010 study waves. Due to various times, participants were entered within each 2-year study wave, participants were followed up to 12 years.
We next compared the HR of mortality obtained from two-stage modeling using the physical functioning result obtained from classic linear mixed-effects model and including it as a covariate in the classic survival model. The Weibull hazard regression with the two-stage approach demonstrated that for every point increase in MWI, the hazard of mortality was 1.04 (95% CI 1.03, 1.04, p < .001) in the adjusted model (Supplementary Table 5).
Discussion
In this prospective cohort nationally representative of more than 64.3 million U.S. adults in 2000, a multimorbidity index weighted to current Short-Form-36 physical functioning was strongly associated with long-term physical functioning decline and increased mortality risk over up to 12 years of follow-up using a robust joint modeling approach. For a participant with the average age of 67 years and average MWI of 4.6, the effect of total current MWI on 10-year physical functioning decline was approximately equal to an additional 11.5 years of aging in this participant. Both multimorbidity and multimorbidity-attributed physical functioning decline over time were associated with increased risk of mortality for all participant subgroups. The associations for multimorbidity and physical decline and mortality from joint modeling were greater and more efficient than those obtained from separate longitudinal and survival analysis and two-stage modeling.
Several baseline characteristics were associated with both decreased physical functioning and increased mortality during follow-up. These included multimorbidity, age, underweight, smoking (current and former), and being unmarried or not living with a domestic partner. Women and obese adults had greater physical functioning decline but lower mortality compared with men and adults with normal BMI, respectively. Higher education and household net worth were associated with better physical functioning and decreased mortality risk, with a monotonic gradient with increasing years of education and quartiles of net worth. Finally, better physical functioning at baseline was also associated with decreased mortality.
Prior studies have demonstrated associations between multimorbidity, functional decline, mobility limitations, disability, and mortality using separate linear regression, mixed models, or survival but not a joint modeling approach. In a cross-sectional analysis of women aged 80 years and greater in the Women’s Health Initiative, multimorbidity, using a count definition of 2 to 12 chronic conditions that included overweight or obesity, was associated with lower SF-36 physical functioning (23). Studies with nationally representative samples have examined risk factors for physical functioning decline in adults with multimorbidity. A longitudinal study in the HRS that treated chronic diseases as time-varying variables reported that women, older adults, and adults with low education and financial wealth had greater difficulty performing 10 physical functioning items (24). Women also reported greater limitations with basic and instrumental activities of daily living than men, regardless of multimorbidity status, in the cross-sectional National Health and Nutrition Examination Survey (24).
In longitudinal analyses of the Nurses’ Health Study and Health Professionals Follow-up Study, baseline multimorbidity using MWI was associated with a persistent decline in SF-36 physical functioning after 4 and 8 years of follow-up, with a greater decline reported in women (2). While greater functional decline is a risk factor for mortality, it may not necessarily be on the direct causal pathway to mortality. Further, there may be a survival bias where women survive longer but acquire more diseases and concomitant functional decline. The present study adjusted for age and calendar time but this does not eliminate potential survival bias.
A major strength of this study was the use of joint modeling of physical functioning and survival models to assess these simultaneous associations with multimorbidity. Joint modeling provided more accurate results for examining longitudinal and simultaneous outcomes and had several advantages over classic methods. The main advantage was the ability to investigate the dynamic association between multimorbidity and time-varying covariates on longitudinal physical functioning decline, as well as the simultaneous impact of these multimorbidity-related changes in physical functioning on survival, with greater accuracy than independent models. When an exposure is also associated with survival, joint modeling produces larger and unbiased associations between the exposure and longitudinal outcome. Concomitantly, if the association between the exposure and longitudinal outcome were ignored, this could result in a flawed estimate of the exposure on survival. Compared with independent and two-stage modeling approaches, joint modeling produced larger estimates and comparable SEs (21).
Our study has several potential limitations. First, multimorbidity may be underestimated. Mental and cognitive conditions including depression and mild cognitive impairment were not assessed in the binary self-reported physician-diagnosed conditions and thus not included in this analysis. Geriatric syndromes such as urinary incontinence and fall risk were also not captured. MWI was ultimately confined to the inventory of chronic conditions assessed in the HRS. Despite this, the conditions assessed were prevalent, encompassed several organ systems, and included several conditions commonly assessed in other national surveys. Further, we have demonstrated that a MWI weighted to current physical functioning even predicts subsequent mental health-related quality of life, providing reassurance that an index weighted in this manner captures both mental and physical health domains of illness (25). Second, some participants lacked follow-up data. However, this was a small portion of our sample. We were able to include participants missing partial covariate data through imputation and thus retain all available observations from these individuals. Finally, this HRS sample is limited to adults aged 52 years and older and thus results are not yet generalizable to younger adults, although they are the least likely to have multimorbidity.
This study demonstrates that the full impact of multimorbidity encompasses concomitant processes of physical functioning decline and increased mortality risk as diseases accumulate over time. This underscores the importance of capturing multimorbidity and physical functioning measures early in the clinical setting, when it is critical to intervene in patients to slow disease accumulation and preserve function. While mortality is an important outcome, physical functioning and health-related quality of life are universally valued among disease survivors. Multimorbidity was associated with worse physical functioning and mortality risk across all subgroups of participants, and physical functioning acted as a mediator of the multimorbidity and mortality association. While some participants such as women had greater survival, they also reported the greatest physical functioning decline. Thus, efforts to improve survival should also consider the impact on functioning and risk for disability. The burden of multimorbidity is profound, and interventions are urgently needed to reduce its progression and impact on physical functioning decline and mortality.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (grant number U01 AG009740) and conducted at the Institute for Social Research, University of Michigan. Dr. Galecki and Mr. Kabeto received support from the National Institute on Aging at the National Institutes of Health (grant numbers P30 AG024824, P30 AG08808). Dr. Langa received support from the National Institute on Aging at the National Institutes of Health (grant numbers P30 AG053760, P30 AG024824). Dr. Wei received support from the National Institute on Aging at the National Institutes of Health (grant number K23 AG056638). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs. Sponsor’s role: The NIA had no role in the design, methods, participant recruitment, data collection, analysis, and preparation of this paper.
Conflict of interest statement
None declared.
Supplementary Material
Acknowledgment
The authors thank Dr. Kenneth Mukamal for providing helpful comments that improved this manuscript.
References
- 1. Staimez LR, Wei MY, Kim M, Narayan KMV, Saydah SH. Multimorbidity of four cardiometabolic and chronic pulmonary disease groups: prevalence and attributable fraction in US adults, 2007–2012. J Comorb. 2017;7:22–32. doi:10.15256/joc.2017.7.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wei MY, Mukamal KJ. Multimorbidity, mortality, and long-term physical functioning in 3 prospective cohorts of community-dwelling adults. Am J Epidemiol. 2018;187:103–112. doi:10.1093/aje/kwx198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wei MY, Kabeto MU, Langa KM, Mukamal KJ. Multimorbidity and physical and cognitive function: performance of a new multimorbidity-weighted index. J Gerontol A Biol Sci Med Sci. 2018;73:225–232. doi:10.1093/gerona/glx114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 5. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 6. Tisminetzky M, Bayliss EA, Magaziner JS, et al. Research priorities to advance the health and health care of older adults with multiple chronic conditions. J Am Geriatr Soc. 2017;65:1549–1553. doi:10.1111/jgs.14943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brock DB, Lemke JH, Branch LG, Evans DA, Berkman LF. Mortality and physical functioning in epidemiologic studies of three older populations. J Aging Soc Policy. 1994;6:21–37. [DOI] [PubMed] [Google Scholar]
- 8. Goldman N, Glei DA, Rosero-Bixby L, Chiou ST, Weinstein M. Performance-based measures of physical function as mortality predictors: incremental value beyond self-reports. Demogr Res. 2014;30:227–252. doi:10.4054/DemRes.2013.30.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi:10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williams JS, Egede LE. The association between multimorbidity and quality of life, health status and functional disability. Am J Med Sci. 2016;352:45–52. doi:10.1016/j.amjms.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 11. Olaya B, Moneta MV, Demenech-Abella J, et al. Mobility difficulties, physical activity and all-cause mortality risk in a nationally-representative sample of older adults. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx121 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 12. Ryan A, Wallace E, O’Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13:168. doi:10.1186/s12955-015-0355-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17–32. doi:10.1146/annurev-publhealth- 032315-021402 [DOI] [PubMed] [Google Scholar]
- 14. Wei MY, Kawachi I, Okereke OI, Mukamal KJ. Diverse cumulative impact of chronic diseases on physical health-related quality of life: implications for a measure of multimorbidity. Am J Epidemiol. 2016;184:357–365. doi:10.1093/aje/kwv456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43:576–585. doi:10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ware JE Jr., Snow KK, Kosinski M, Gandek B.. SF-36 Health Survey Manual and Interpretation Guide. Boston, MA: The Health Institute; 1993. [Google Scholar]
- 17. Belsley DA, Kuh E, Welsch RE.. Regression Diagnostics: Identifying Influential Data and Sources of Collinearity. Hoboken, NJ: Wiley & Sons, Inc; 1980. [Google Scholar]
- 18. Weir DR. Validating Mortality Ascertainment in the Health and Retirement Study 2016. https://hrs.isr.umich.edu/sites/default/files/biblio/Weir_mortality_ascertainment.pdf. Accessed July 1, 2017.
- 19. Crowther MJ, Abrams KR, Lambert PC. Joint modeling of longitudinal and survival data. Stata J. 2013;13:165–184. [Google Scholar]
- 20. Nelson W. Applied Life Data Analysis. New York: John Wiley & Sons, Inc; 1982. [Google Scholar]
- 21. Ibrahim JG, Chu H, Chen LM. Basic concepts and methods for joint models of longitudinal and survival data. J Clin Oncol. 2010;28:2796–2801. doi:10.1200/JCO.2009.25.0654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34:187–220. [Google Scholar]
- 23. Rillamas-Sun E, LaCroix AZ, Bell CL, Ryckman K, Ockene JK, Wallace RB. The impact of multimorbidity and coronary disease comorbidity on physical function in women aged 80 years and older: the women’s health initiative. J Gerontol A Biol Sci Med Sci. 2016;71 (Suppl. 1):S54–S61. doi:10.1093/gerona/glv059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jindai K, Nielson CM, Vorderstrasse BA, Quiñones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005–2012. Prev Chronic Dis. 2016;13:E151. doi:10.5888/pcd13.160174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wei MY, Mukamal KJ. Multimorbidity and long term physical and mental health-related quality of life in community-dwelling adults. J Gen Intern Med. 2016;31(Suppl. 2):S306. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.