Abstract
The deformed and enlarged femoral head secondary to hip diseases such as Legg Calve Perthes and Developmental Dysplasia usually causes impingement between the aspherical head and the acetabulum. To restore and reduce the size of enlarged femoral head, a femoral head reduction technique has been described previously. The goal is to obtain a spherical femoral head and to cover the gliding surface with best available cartilage. Planning of osteotomy to achieve spherical head is the crucial point of surgery. It is usually done intra-operatively and dependent on experience of surgeon. Preoperative 3- Dimension (D) modeling of femoral head is commonly preferred to minimize this risk. In this technical note, preoperative planning with 3-D printing was demonstrated in two separate patients with Legg-Calve-Perthes Disease and developmental hip dysplasia. Surgical time was approximately 150 and 120 min, respectively. Blood loss was 230 and 300 cc, respectively. Patients were followed up 9 months and 12 months, respectively. None of the patients in this study developed avascular necrosis; however, the follow-up period is very limited. Moreover, none of the patients developed post-operative complications or required additional surgery. With a more detailed preoperative planning done on computer model and printed in 3-D, one can mimic the surgical procedure before the procedure. Finally, this technique is advantageous both for the patient and surgeon.
Keywords: Deformation, Femoral head, Preoperative planning, Hip, Three dimensional printing
Introduction
The deformed and enlarged femoral head secondary to hip diseases such as Legg Calve Perthes and developmental dysplasia usually causes impingement between the aspherical head and the acetabulum. To restore and reduce the size of enlarged femoral head, a femoral head reduction technique has been described by Ganz R.1 The goal is to obtain a spherical femoral head and to cover the gliding surface with best available cartilage.2, 3 Planning of osteotomy to achieve spherical head is the crucial point of surgery. It is usually done intra-operatively and dependent on experience of surgeon. Preoperative 3-dimensional (3-D) modeling of femoral head is commonly preferred to minimize this risk. Dobbe et al described computer-assisted and patient-specific 3-D planning in femoral osteotomy.4 They concluded that 3-D simulation has revealed good results, but it needed the improvement of computer algorithm and automation. There is a lack of planning method for femoral head restoration. Advances in 3-D printing and medical technology can make it possible. Now we have 3-D-printed implants, 3-D-printed models for surgical practice, 3-D-printed bone replacements, and even 3-D-printed human tissue. 3-D-printed models for surgical practice may decrease surgical time and surgery may be done precisely.5 We aimed to use 3-D printing for deformed femoral head and preoperative simulation of surgical technique because of its complexity.
Material and methods
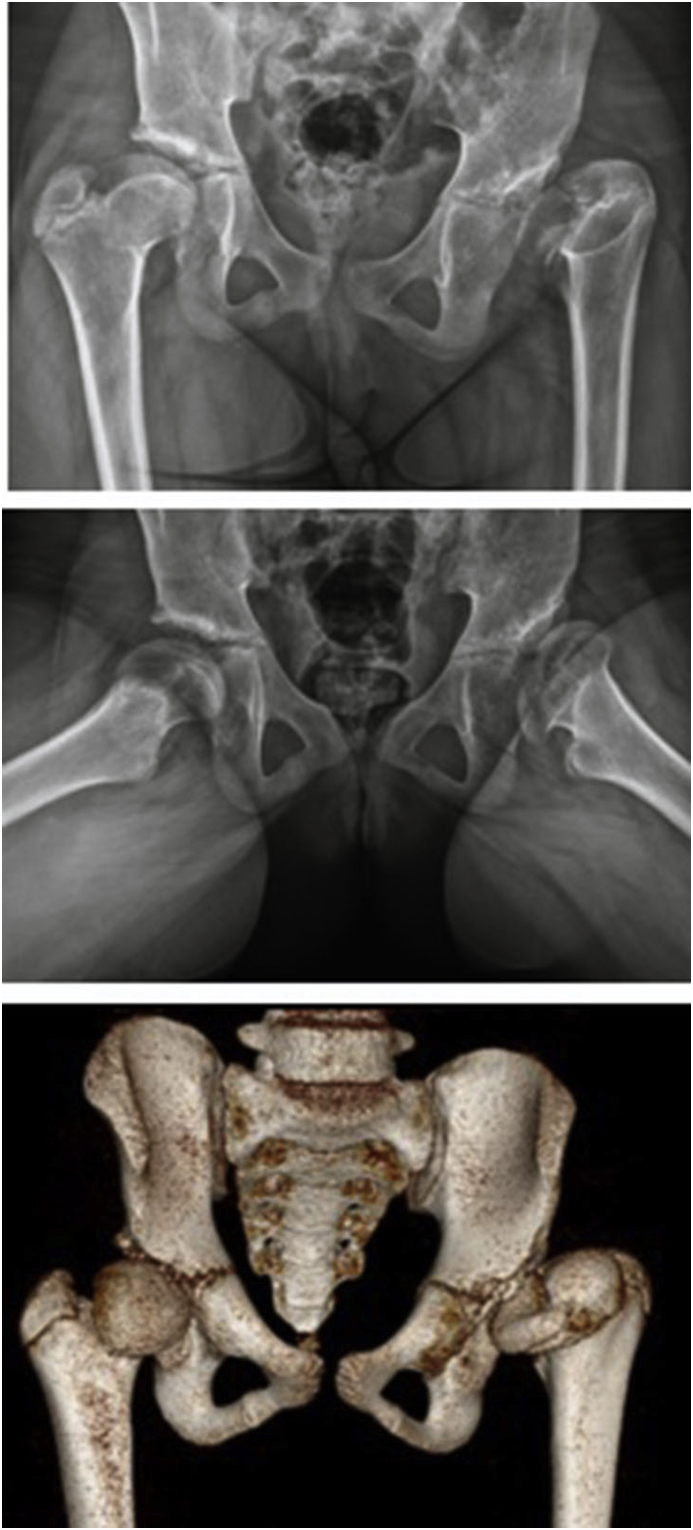
Two patients were included in this study following ethical committee approval. First case was 9 years old and had a sequel of Legg Calve Perthes disease (Fig. 1). The second case was 11 years old and had a sequel of avascular necrosis secondary to developmental dislocation (dysplasia) of hip (Fig. 2). Both cases were enrolled after the acquisition of the 3-D models made from their CT scans. Planning for two cases was femoral head reduction technique which was described by Ganz et al and Leunig et al after surgical dislocation of the hip.1, 2
Fig. 1.
a-b. Radiographs show a 9 years old boy with a sequel of Legg Calve Perthes disease.
Fig. 2.
Radiographs and 3-D tomography present a 11 years old boy had a sequel of avascular necrosis secondary to developmental dislocation (dysplasia) of hip.
Planning
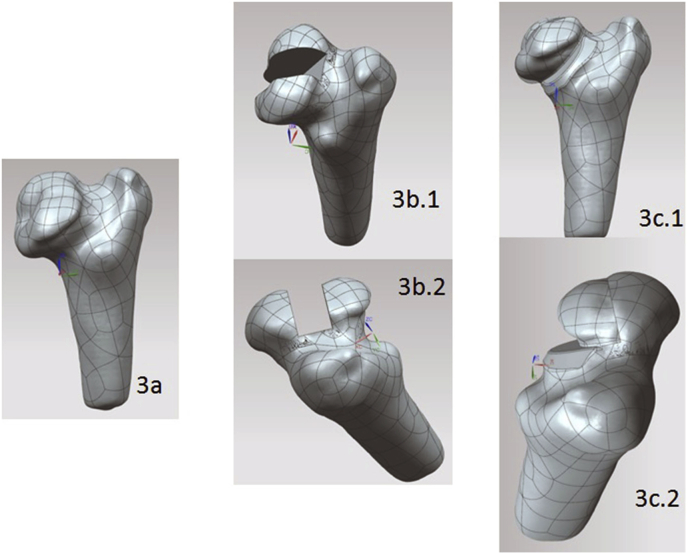
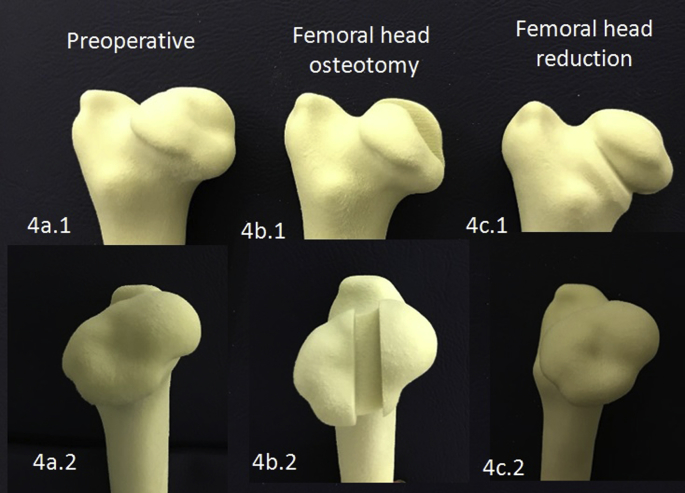
For each patient's CT scan, Digital Imaging and Communication in Medicine (DICOM) image stacks were processed using MIMICS v17.0 (Materialise, Leuven, Belgium). A femoral head reduction surgery is performed on the 3-D model obtained from the CT images (Fig. 3a.1, a.2). Femoral head osteotomy is simulated on the images (Fig. 3b.1, b.2). Because the most spherical femoral head is aimed, osteotomy site is revised accordingly (Fig. 3c.1, c.2). The surgical procedure is first performed on the computer; then with a 3-D printer preoperative, osteotomy carried out and postoperative femoral head was printed (Fig 4a–c). Sphericity of femoral head and acetabular compliance were inspected. Sufficient femoral head to acetabulum compliance were achieved in both of our patients.
Fig. 3.
A femoral head reduction surgery is performed on the 3D model obtained from the CT images (3a). Femoral head osteotomy is simulated on the images (3b.1, 3b.2). The most spherical femoral head is achieved (3c.1, 3c.2).
Fig. 4.
Figures show femoral head obtained from 3-D printer. Preoperative (4a.1, 4a.2), osteotomy carried out (4b.1, 4b.2) and femoral head reduction (4c.1, 4c.2). Sphericity of femoral head is inspected.
Results
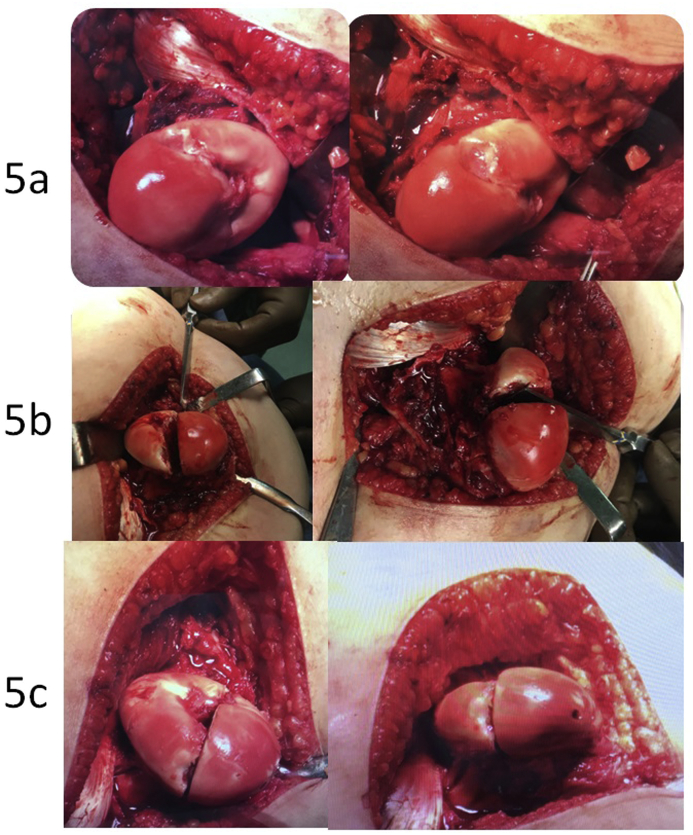
Intra-operatively, femoral head reduction technique was achieved according to surgical plan (Fig 5a–c). Surgical time was approximately 150 and 120 min, respectively. Blood loss was 230 and 300 cc, respectively. Patients were followed up 9 months (Case 1) (Fig. 6a,b) and 12 months (Case 2) (Fig. 7a,b).
Fig. 5.
Femoral head reduction technique was achieved according to surgical plan. a. Preoperative representation of femoral head. b. Following resection. c. After femoral head reconstruction.
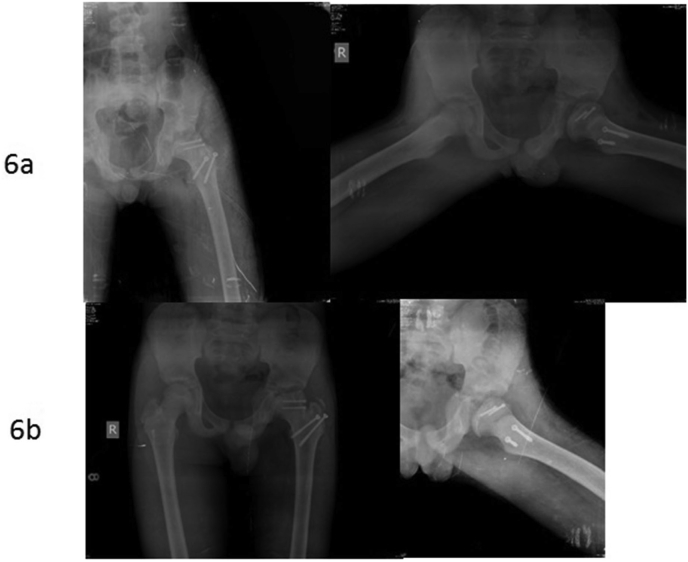
Fig. 6.
Postoperative (6a) and follow up (6b) radiographs for case 1.
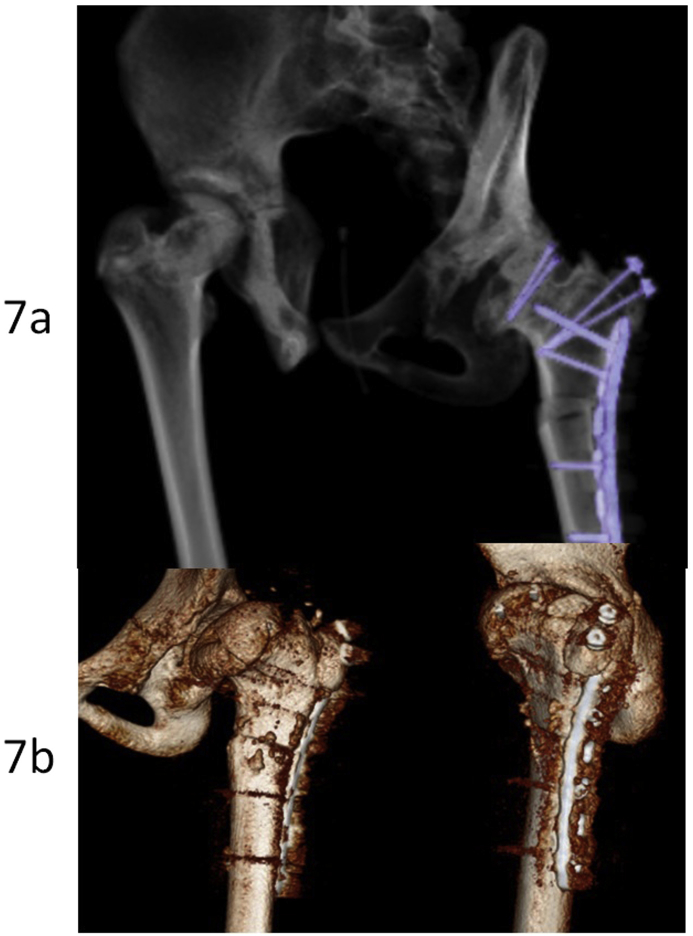
Fig. 7.
Postoperative (7a) and follow up (7b) 3-D CT scans for case 2.
None of the patients in this study developed avascular necrosis; however, the follow-up period is very limited. Moreover, none of the patients developed post-operative complications or required additional surgery.
Discussion
Ganz et al has first described the technique of femoral head reduction osteotomy to reduce the size and restore the spherical shape of the femoral head.1 Several studies have been published since then however; it still has not become a common surgical technique.2, 3, 6, 7 This can be attributed to a long learning curve and being dependent on the surgeon intra-operatively. To increase surgical outcome, advanced radiological techniques such as MRI, 3-D CT are being used. Even with the use of these methods, a postoperative spherical femoral head may not be achieved. In the recent years, 3-D planning has been in use to overcome these obstacles.8
When it comes to planning complex surgical procedures, the usual methods have been drawings on X-ray, cutting and pasting certain radiologic bone fragments to determine the amount of correction preoperatively. However; all these techniques are on a 2-D basis which limits our understanding of the deformity that can be in 3 planes (coronal, sagittal and axial). There have been several studies that focus on 3-D printed planning of complex bone deformities prior to surgery.5, 8 The result of these studies shows decreased surgery time and less fluoroscopy use as well as improved surgical outcome. These results can be attributed to the better understanding of the individually unique deformities.
In our study, we have used 3-D femur models printed from their computer images (preoperative, osteotomy carried out and postoperative) to achieve optimal femoral head reduction surgery on two patients. Although we have no control group to compare results, we believe simulation of surgery in 3-D model offers a better understanding of each patient's femoral head reduction osteotomy and determine the exact resection of femoral head to obtain spherical femoral head. Performing such an operation can cause a negative effect on growth of the proximal femur if proximal physis of the patient is still active. In this case, this procedure may be relatively contraindicated.3
Our patient number is limited due to reasons such as cost-effectiveness and limited use of 3-D printers even today. We are hopeful that this study will pave the way for future developments in femoral osteotomy planning. Additionally the patients have to be followed-up at least skeletal maturity to exclude avascular necrosis.
Conclusion
The findings of our study show that with the use of preoperative 3-D modeling we can have a better understanding of femora-acetabular deformities. With a more detailed preoperative planning done on computer model and printed in 3-D, we can mimic the surgical procedures beforehand. Although limited patient number in current study, we believe this planning enables us to be more familiar with complex deformities specific to every patient.
Funding
There was no funding about this study.
Conflict of interest
Authors Önder Kalenderer, Serkan Erkuş, Ali Turgut and İrem Hazal İnan declare that they have no conflict of interest.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Ganz R.1, Huff T.W., Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instr Course Lect. 2009 Jan;58:241–255. [PubMed] [Google Scholar]
- 2.Leunig M., Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull NYU Hosp Joint Dis. 2011 Jan;69(Suppl 1):S62–S67. [PubMed] [Google Scholar]
- 3.Paley D. The treatment of femoral head deformity and coxa magna by the Ganz femoral head reduction osteotomy. Orthop Clin North Am. 2011 July;42(3):389–399. doi: 10.1016/j.ocl.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Dobbe J.G.G., du Pré K.J., Kloen P., Blankevoort L., Streekstra G.J. Computer-assisted and patient-specific 3-D planning and evaluation of a single-cut rotational osteotomy for complex long-bone deformities. Med Biol Eng Comput. 2011 Dec;49(12):1363–1370. doi: 10.1007/s11517-011-0830-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cherkasskiy L., Caffrey J.P., Szewczyk A.F. Patient-specific 3D models aid planning for triplane proximal femoral osteotomy in slipped capital femoral epiphysis. J Child Orthop. 2017 Apr;11(2):147–153. doi: 10.1302/1863-2548-11-170277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siebenrock K.A., Anwander H., Zurmühle C.A., Tannast M., Slongo T., Steppacher S.D. Head reduction osteotomy with additional containment surgery improves sphericity and containment and reduces pain in Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2015 Apr;473(4):1274–1283. doi: 10.1007/s11999-014-4048-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ziebarth K., Slongo T., Siebenrock K.A. Residual perthes deformity and surgical reduction of the size of the femoral head. Oper Tech Orthop. 2013 Sep;23(3):134–139. [Google Scholar]
- 8.Won Tak Man, Jin Jimmy, Lau Tak Wing. The use of three-dimensional printing technology in orthopaedic surgery: a review. J Orthop Surg. 2017 Jan;25(1):1–7. doi: 10.1177/2309499016684077. [DOI] [PubMed] [Google Scholar]