Abstract
Objective
The aim of this study was to represent the findings and long-term clinical results of the children who underwent hip arthroscopy because of Legg-Calve-Perthes Disease (LCPD).
Methods
This study included the retrospective findings of ten patients (mean age: 12.7 ± 2.75; range 7–16 years) who underwent arthroscopic hip debridement between 2010 and 2016 for LCPD disease. All of the patients underwent arthroscopic excision of the unstable osteochondral fragment following unsuccessful conservative treatment. In the statistical analysis, age, side, follow-up, Stulberg and Waldenström classification, preoperative and postoperative modified Harris Hip Score (mHHS) were evaluated.
Results
The mean follow-up period was 55.4 ± 13.05 months (range: 40–72 months). There was no statistically significant association between good postoperative results and age, side, and the stage of the disease (p > 0.05). However, there was a significant difference between preoperative and postoperative mHHS (p = 0.005).
Conclusion
This study demonstrates an increase in the functional results and life quality of the patients who underwent hip arthroscopy due to LCPD. It is thought that hip arthroscopy, a minimally invasive procedure, may have an important role in the algorithm of LCPD treatment, especially in patients with severe pain and mechanical symptoms.
Level of evidence
Level IV, therapeutic study.
Keywords: Perthes disease, Hip arthroscopy, Treatment, Modified Harris hip score, Limitation of motion
Introduction
Legg-Calvè-Perthes disease (LCPD) is a non-inflammatory disease of the femoral head which is thought to be a result of vascular insufficiency. It is a self-limited disease which has an important place in the painful pathologies of childhood. At the femoral head, resorption and repair with necrosis and collapse can be observed at the same time. While trying to solve the problems caused by ischemia in a region, a new ischemic event may occur in a neighbouring area.1, 2
In a significant proportion of LCPD patients, the disease can heal with good or excellent results without the need for any treatment. Physical therapy is the first treatment choice of LCPD in active period for pain control and acquisition of the range of the joint motion. Therefore, bed rest, anti-inflammatory drugs and the skin or skeletal traction can be used for this purpose.3 Procedures such as cast/orthosis, adductor tenotomy and medial capsulotomy are employed to increase abduction, in addition, femoral or pelvic osteotomies are applied in order to increase joint compliance.2, 3, 4, 5
In a study published in 1994, Suzuki et al performed the first diagnostic arthroscopy on 19 patients and detected hypertrophic hyperfibrinous tissue with labral tear.6 As well as hypertrophic hyperfibrinous tissue with labral tear, unstable fragments, femoral head defects and femoroacetabular impingement pathologies are reported to cause pain and mechanical symptoms.7 Most of these pathologies can be intervened by hip arthroscopy procedures, which are minimally invasive methods.8, 9
Some of the patients’ complaints persist after the healing because of the mechanical obstacle secondary to the free unstable osteochondral fragments developed during the fragmentation stage. Although those unstable fragments tend to resorb in time spontaneously,10 they may cause pain and impairment in quality of life scores even the disease reaches its healing phase. Therefore, debridement of these fragments by hip arthroscopy in symptomatic children may promise good outcomes and early return to daily activity.
This study aimed to represent the findings and long-term clinical results of the children who underwent hip arthroscopy because of LCPD.
Material and methods
This study includes the retrospective findings of ten patients who underwent arthroscopic hip debridement between 2010 and 2016 for LCPD disease. All of the procedures were executed in the same institute by the senior surgeon of this study and were followed-up at least three years postoperatively. Institutional review board approval was provided before starting the investigation.
All patients were initially treated with conservative methods including non-steroid anti-inflammatory drugs and weight-bearing and activity restriction. Intra-articular steroid injection does not exist in our institute's daily practice for this patient group because of its side-effects to the articular cartilage. The patients who have reduction in walking distance, difficulty in sitting and normal daily activities due to reduced range of motion, and MRI or radiographic findings indicating any unstable articular osteochondral fragment were candidates for arthroscopic surgery.
Our goal in this surgical procedure was to reduce the mechanical symptoms of patients. So, we applied hip arthroscopy to younger children, a minimal invasive procedure for improving the quality of patient's life. This patient group is a homogeneous group of patients, who are exclusively subjected to unstable osteochondral fragment excision. Patients who had only synovitis or partial labrum pathology (patients without mechanical symptoms) were excluded from the study. The minimum follow-up duration for being included in the study was determined as 3-year postoperatively.
Age, side, symptom duration before surgery, follow-up time, preoperative Waldenström classification, postoperative Stulberg classification, preoperative and postoperative modified Harris Hip Score (mHHS) were recorded. Preoperative mHHS questionnaires, anteroposterior and frog position radiographs of the pelvis and magnetic resonance images were retrieved from the clinical records. However, preoperative MRI-arthrography was not performed in all patients. The patients were evaluated with their radiographs, graded using the Stulberg classification, and finally called for follow-up control to re-evaluate with mHHS.
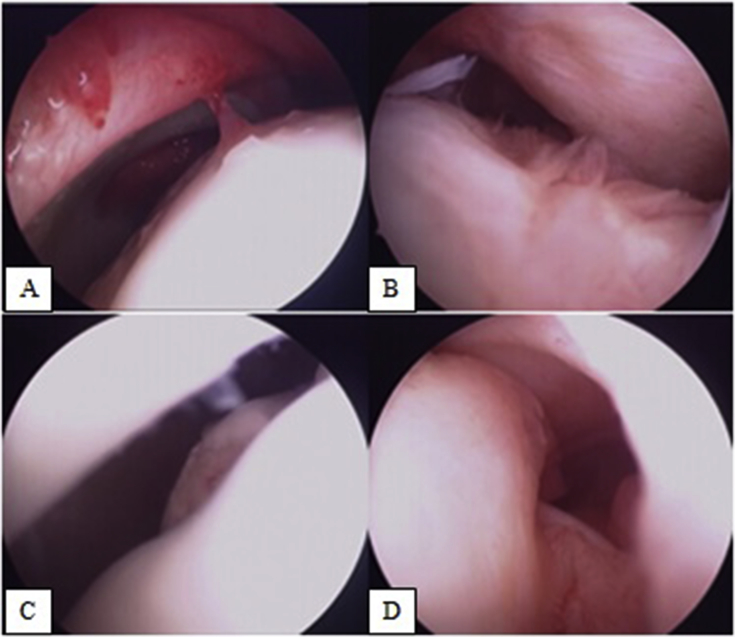
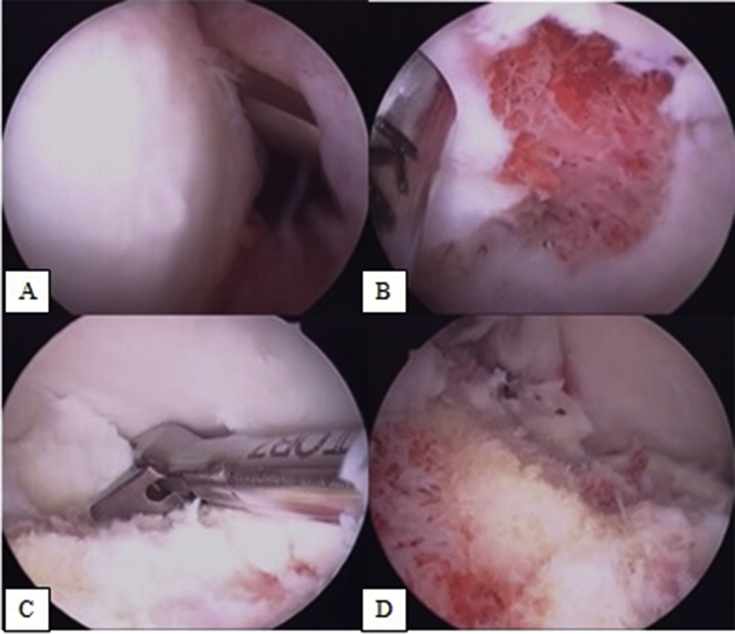
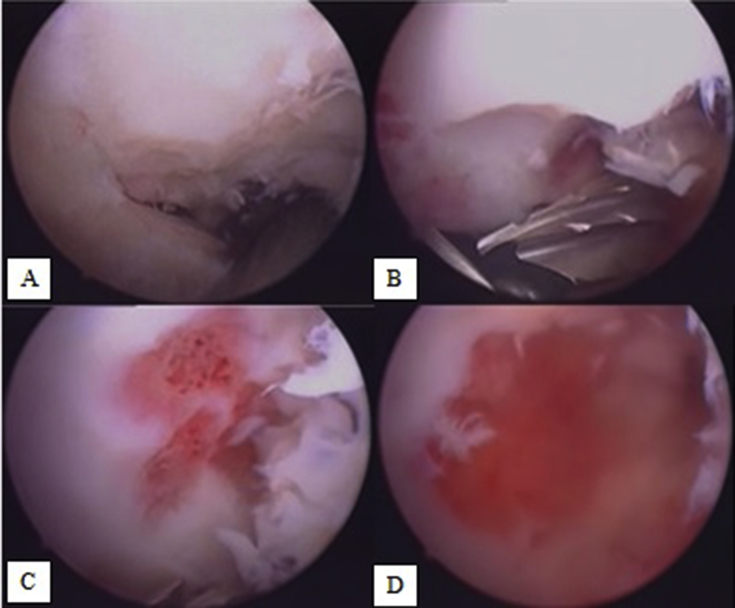
Hip arthroscopy was carried out in the standard supine position for all the patients. The surgical procedure was performed with the hip at 20–30 degrees of abduction and 15 degrees of internal rotation. The other hip was placed in a 70° abduction position for comfortable use of the fluoroscope. In addition, the hip joint space was distracted about 1 cm with the traction table. Standard lateral and anterolateral portals with the help of fluoroscopy were used. After the intra-articular examination, intraoperative findings were recorded (Fig. 1), and hypertrophic reactive synovial tissues were resected and free or unstable osteochondral fragments were excised (Fig. 2). The remaining osteochondral defect area was also debrided until reaching to the blood-forming tissue (Fig. 3).
Fig. 1.
Intraoperative findings. A–B. Hypertrophic reactive synovial tissues. C. Instabil osteochondral fragment. D. Degenerate ligamentum teres.
Fig. 2.
Resection of unstable osteochondral fragment. A. Joint examination with the help of a spinal needle. B–C. Resection of the fragment with shaver and punch. D. Post-excision image of instabil fragment.
Fig. 3.
A–B. Resection of the fragment with shaver and punch. C–D. The remaining osteochondral defect area was also debrided until reaching to the blood-forming tissue.
In the postoperative period, patients were given partial weight-bearing with a 4-week arm-chair. A rehabilitation program was initiated immediately after the surgery to maintain the range of the joint motion and muscle strength. Strenuous exercises were banned for six months.
SPSS Version 18.0 software programme was used for statistical analysis for the data gathered. In the statistical analysis, age, side, follow-up, Stulberg classification, preoperative and postoperative mHHS were evaluated. Nonparametric data were evaluated using Spearman's Rho and Wilcoxon tests.
The study's protocol was approved by the ethics committee of XXXXXXX Medical Faculty. (25 January 2016)/(Number:25901600/56).
Results
Ten patients were included in this study. The mean age at the time of surgery was 12.7 (range of age: 7–16, SD: 2,75) when the patients were operated. The mean time of symptom duration before surgery was 27 months (range 19–31 months). The mean follow-up period was 55.4 months (range: 40–72 months, SD: 13,05) (Table 1).
Table 1.
Demographic datas and pre-operative clinical outcomes of patients.
| Patient number | Age | Symptom duration before surgery (months) | Follow-up | Preoperative Grade (Waldenström classification) | Postoperative Grade (Stulberg classification) | Preoperative mHHS | Postoperative mHHS |
|---|---|---|---|---|---|---|---|
| 1. | 12 | 29 | 40 | 4 | 5 | 32 | 76 |
| 2. | 14 | 28 | 72 | 4 | 5 | 36 | 95 |
| 3. | 15 | 25 | 42 | 4 | 2 | 47 | 83 |
| 4. | 13 | 28 | 48 | 4 | 2 | 54 | 93 |
| 5. | 14 | 26 | 40 | 4 | 3 | 52 | 85 |
| 6. | 7 | 19 | 70 | 3 | 5 | 42 | 95 |
| 7. | 15 | 29 | 58 | 4 | 3 | 34 | 93 |
| 8. | 16 | 27 | 50 | 4 | 2 | 37 | 93 |
| 9. | 10 | 31 | 63 | 4 | 4 | 47 | 85 |
| 10. | 11 | 28 | 71 | 4 | 2 | 52 | 93 |
When preoperative radiographs were evaluated according to Waldenström classification, six patients were in stage 2, and four patients were in stage 3. When postoperative radiographs were evaluated according to Stulberg classification, four patients were in stage 2, two patients were in stage 3, one patient was in stage 4, and three patients were in stage 5.
The mean preoperative mHHS of the patients was 43.3 (32–54) (SD:8.17). When the scores were categorized, four patients were in the "bad" category and six patients were in the "middle" category (Table 1). At the last follow-ups, the mean postoperative mHHS of the patients was 89,1 (76–95) (SD:6.43). Four patients were in the "very good" category, six patients were in the "excellent” category (Table 1).
There was no statistically significant association between good postoperative results and age, side, symptom duration before surgery and the stage of the disease (p > 0,05). However, there was a significant difference between preoperative and postoperative mHHS (p = 0,005).
No complications were observed in short or long term.
Discussion
LCPD is often a self-limited disease. Pain management and physical therapy are usually enough to maintain the range of the joint motion. The disease may heal with good or excellent results without requiring advanced surgical treatment. If conservative methods fail, procedures of cast/orthosis, adductor tenotomy, medial capsulotomy, hip arthroscopy, or femoral/pelvic osteotomies are performed.1, 2, 3, 4, 5
In this study, ten patients in the adolescent age group who underwent hip arthroscopy were included in the treatment of LCPD. All patients were initially treated conservatively. The vast majority of patients were resolved with conservative treatment practices and the natural course of the disease. The patients who are not resolved in the natural course of the disease and have reduction in walking distance, difficulty in performing daily activities, difficulty sitting due to reduced range of motion underwent arthroscopy. Preoperative conditions of the patients were also revealed by the low modified Harris Hip Scores. The LCPD, aka coxa plana, is characterized with lateral subluxation of the femoral head and cam-type hip impingement, especially in the Stulberg stage III, IV, and V, during its natural progress. Femoral or acetabular osteotomy may have been emerged as early as in the fragmentation stage. However, today, debridement with hip arthroscopy is only recommended after the healing stage. This study included satisfactory outcomes of LCPD after arthroscopy even it is perfomed before the healing stage.
Hip arthroscopy was performed in supine position with fluoroscopy and through the standard ports. As an arthroscopic finding; synovitis, impingement, and chondral lesions were similar in all cases. Unstable osteochondral fragments at the femoral head, which could cause cam-type impingement, was excised. The most basic finding of this study was the significant improvement in functional outcomes. The average increase in mHHS was found as 45,8 on an average follow-up of 55 months, which is the longest follow-up period in the literature as far as is known.
Good clinical outcomes were observed in the studies in the literature. Snow et al performed arthroscopic debridement and fragment excision on four patients with LCPD, and followed for approximately two years. At the end of the second postoperative year, three patients were asymptomatic and one patient required additional surgery.11 Bowen et al also performed arthroscopic osteochondral fragment excision and debridement on three patients and they found that the patients were asymptomatic in the first postoperative year.7 O'Leary et al reported nine patients with LCPD with a mean age of 33,6. At the end of a 30 month of follow-up period, eight patients were asymptomatic and one patient underwent total hip arthroplasty.9 In 2013, Freeman et al treated hypertrophic synovial tissues, labral tears and osteochondral lesions with excision and microfracture in a study on 22 patients with an average age of 27. In the 24th month of the postoperative period, an average of 28 point increase was detected in mHHS.12 Similar to the results of this study, they did not find any relationship between age and stage of the disease and postoperative clinical outcomes.
There are several studies in the literature regarding adolescent age group for example, Roy et al applied hip arthroscopy to nine adolescent LCPD patients and followed them for two years. Eight of their patients were previously treated with additional hip surgery such as pelvic osteotomy, capsule loosening, and apophysodesis. Seven of them were asymptomatic, and two patients required total hip arthroplasty.13 Kocher et al also performed hip arthroscopy to eight adolescent LCP patients. At the end of one year, they found an average increase of 30 points in the mHHS.14 The average age of the patients in this study is lower and the increase in mHHS is higher than the other studies in the literature.
As for the advantages of this research, all the patients were in the same age group, treated by the same surgeon, and the same surgical procedure (excision of the unstable osteochondral fragment) was performed. To the knowledge of the researchers, this study has the longest follow-up period in the literature. There are also limitations of this study. Retrospective design of the study and low number of patients are the main limitations. And, Stulberg classification is used for description of the femoral head shape and hip congruence at the end of the growth. But, it is used to evaluate mature hips. In this study, only one patient's hip joint has not maturation (grade 3-Waldenström classification). Hip arthroscopy was performed to this 7-year old patient, considering that the excessive complaints.
In conclusion, this study demonstrates an increase in the functional results and life quality of the patients who underwent hip arthroscopy due to LCPD. Conservative treatment should be the first treatment option for this disease. Short-term good results of hip arthroscopy have been reported in previous studies and this study has shown that long-term results are also good. Interestingly, although there is no radiologically significant improvement in patients, clinical outcomes of this procedure is very good. Therefore, it is thought that hip arthroscopy, a minimally invasive procedure, plays an important role in the algorithm of LCPD treatment, especially in patients with severe pain and mechanical symptoms, even if it does not changes the natural course of the disease (Fig. 4, Fig. 5). It is important to reduce the mechanical symptoms of the patients even though the disease is not fully healed.
Fig. 4.
Preoperative (A–B) and postoperative (C–D) radiographies of the hip. There was a 36-point increase in the patient's mHHSs, although there was no radiological improvement in the hips.
Fig. 5.
Preoperative (A–B) and postoperative (C–D) radiographies of the hip. There was a 44-point increase in the patient's mHHSs, although the misshapen femoral head.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Stulberg S.D., Cooperman D.R., Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 2.Kerimoglu S., Cıtlak A., Baki C., Aydın H. The long-term results of brace treatment in Perthes disease. Joint Dis Relat Surg. 2012;23:25–29. [PubMed] [Google Scholar]
- 3.Killian J.T., Niemann K.M. Preoperative skeletal traction in Legg-Perthes disease. South Med J. 1985;78:928–932. doi: 10.1097/00007611-198508000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Aksoy M.C., Cankus M.C., Alanay A., Yazici M., Caglar O., Alpaslan A.M. Radiological outcome of proximal femoral varus osteotomy for the treatment of lateral pillar group-C Legg-Calve-Perthes disease. J Pediatr Orthop B. 2005;14:88–91. doi: 10.1097/01202412-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Thompson G.H. Salter osteotomy in Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31:192–197. doi: 10.1097/BPO.0b013e318223b59d. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki S., Kasahara Y., Seto Y. Arthroscopy in 19 children with Perthes' disease. Pathologic changes of the synovium and the joint surface. Acta Orthop Scand. 1994;65:581–584. doi: 10.3109/17453679408994608. [DOI] [PubMed] [Google Scholar]
- 7.Bowen J.R., Kumar V.P., Joyce J.J., III, Bowen J.C. Osteochondritis dissecans following Perthes' disease. Arthroscopic operative treatment. Clin Orthop Relat Res. 1986;209:49–56. [PubMed] [Google Scholar]
- 8.Polat G., Dikmen G., Erdil M., Aşık M. Arthroscopic treatment of femoroacetabular impingement: early outcomes. Acta Orthop Traumatol Turc. 2013;47:311–317. doi: 10.3944/aott.2013.3041. [DOI] [PubMed] [Google Scholar]
- 9.O'Leary J.A., Berend K., Vail T.P. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy. 2001;17:181–188. doi: 10.1053/jars.2001.21481. [DOI] [PubMed] [Google Scholar]
- 10.Rowe S.M., Moon E.S., Yoon T.R., Jung S.T., Lee K.B., Lee J.J. Fate of the osteochondral fragments in osteochondritis dissecans after Legg-Calve-Perthes' disease. J Bone Joint Surg Br. 2002;84:1025–1029. doi: 10.1302/0301-620x.84b7.13227. [DOI] [PubMed] [Google Scholar]
- 11.Snow S.W., Keret D., Scarangella S., Bowen J.R. Anterior impingement of the femoral head: a late phenomenon of Legg-Calvé-Perthes’ disease. J Pediatr Orthop. 1993;13:286–289. doi: 10.1097/01241398-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Freeman C.R., Jones K., Byrd J.W. Hip arthroscopy for Legg-Calvè-Perthes disease: minimum 2-year follow-up. Arthroscopy. 2013;29:666–674. doi: 10.1016/j.arthro.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 13.Roy D.R. Arthroscopic findings of the hip in new onset hip pain in adolescents with previous Legg-Calve-Perthes disease. J Pediatr Orthop. 2005;14:151–155. doi: 10.1097/01202412-200505000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Kocher M.S., Kim Y.J., Millis M.B. Hip arthroscopy in children and adolescents. J Pediatr Orthop. 2005;25:680–686. doi: 10.1097/01.bpo.0000161836.59194.90. [DOI] [PubMed] [Google Scholar]