As hospital survival for common ICU syndromes like sepsis and respiratory failure continues to improve, recovery has proven more elusive. Nearly a third of patients who survive to hospital discharge die within the subsequent year and up to two thirds are re-hospitalized.(1, 2) Among medical patients, a large proportion of these post-hospital deaths and rehospitalizations are due to exacerbations of chronic diseases like congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD), often termed ambulatory care sensitive conditions due to the role that ambulatory care may play in reducing their severity.(2, 3) Specialized post-ICU clinics and other ambulatory interventions have been developed to better address the multi-faceted needs of ICU survivors.(4, 5) Yet, availability of these clinics remains limited, and little is known about how best to transition patients back to primary care where most survivors of critical illness will ultimately receive their ongoing care.
There is reason to expect that the quality of a patient’s transition back to primary care after surviving critical illness might influence their chances of long-term recovery. In the case of CHF, several strategies to improve the ambulatory care transition have proved useful to reducing readmissions, including pre-arranged ambulatory follow-up plans at hospital discharge, direct delivery of discharge summaries to primary care physicians, partnerships between area hospitals and community physicians, and the designation of specific point people for follow-up of laboratory testing.(6) Likewise, among patients hospitalized for acute exacerbations of COPD, early post-hospital follow-up with use of COPD action plans have effectively reduced readmissions.(7) Recognizing the importance of early and comprehensive post-hospitalization follow-up, Medicare instituted transitional care management payment codes in 2013 to reimburse primary care providers at a higher rate for early post-hospitalization follow-up. Though early analyses suggest slow adoption of transitional care, short-term post-hospital costs and mortality may be lower among patients receiving these services.(8)
Though adapting successful techniques from other conditions may be helpful, critical illness survivors pose unique challenges. First, critically ill patients are cared for by clinicians that span a range of specialties, including internists, surgeons, and anesthesiologists, who may or may not have specialized critical care training. Many critical illnesses also require input from consulting providers, who often play a central role in determining treatment and follow-up plans. While such specialization likely yields benefits for hospital survival, the number and scope of providers involved in inpatient critical care complicates the role of primary care providers, who are expected to obtain a complete picture of a patient’s follow-up needs from a single discharge summary and coordinate care across a range of health conditions and providers.
Second, the inpatient-to-outpatient transition for patients surviving critical illness is often indirect, as patients leaving intensive frequently spend several days or weeks in a step-down or high dependency unit, a general care ward, and in post-acute care settings before transitioning home. Although primary care providers often receive written discharge summaries after a patient’s hospitalization and once again after discharge from post-acute care, the several, often discrete, teams of providers involved at each step of a patient’s journey from ICU to home creates the opportunity for information loss or changing priorities at each step. Primary care providers may never communicate with inpatient or post-acute providers outside of written discharge summaries, which may be adequate for some patients. However, for many patients recovering from critical illness, more direct communication by phone or other method may be beneficial to circumvent potential information loss.
Finally, many complex critical illnesses result in transfer from community hospitals to specialized centers. While such specialization likely yields benefits for hospital survival, it may increase care fragmentation after discharge, as primary care providers may have difficulty accessing inpatient records and laboratory testing or difficulty communicating with subspecialist providers at the specialized center.
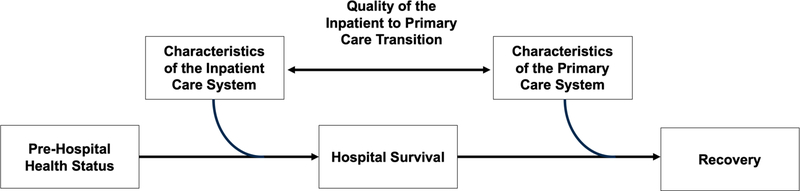
Though efforts to enhance inpatient care have improved short-term survival, their impact on the longer-term morbidity and mortality common to survivors of critical illness is unclear. Post-discharge primary and specialty care are crucial to long-term recovery. Yet, the best means to support this transition while minimizing the added burden to patients and families, who are already strained by critical illness, has not yet been determined (Figure 1).(9) Several specific questions must be answered in future work. First, who should own the transition back to primary care, how should patient handoffs be best implemented, and when should these handoffs occur? This is particularly important in settings where multiple consultants contribute to a patient’s care plan, and when discharge home from the ICU occurs via several intermediate care steps. Additionally, while there is a tendency to transition ambulatory care to a tertiary center after a complex critical illness, this practice contributes to further fragmentation of care among patients who maintain community primary care providers, and so may hinder recovery and hold back goals-of-care discussions. The benefits of specialized medical care must be weighed against the benefits of continuity with local providers and contextualization of critical illness—or even better, we must find a way to combine these services.(9) Further work must also clarify optimal timelines for primary care follow-up after critical illness, and establish the role of timely transitional care when post-ICU clinics are not available. Finally, policy approaches to reduce readmissions and improve transitions home among survivors of critical illness are promising, though strategies to increase their efficacy and uptake while minimizing unintended consequences require further study.
Figure 1.
A framework for improving post-critical illness recovery through primary care (10)
Critical illness survivorship is a clinical and scientific priority, which is a testament to the significant improvements in hospital-based care over the past two decades. By improving critically ill patients’ transitions back to primary care, we can build on the gains in hospital survival and optimize their chances for long-term recovery.
Acknowledgments
Funding Support: This work was supported, in part, by grants from the National Heart, Lung, and Blood Institute (T32HL007749, Dr. Admon). Dr. Tipirneni is additionally supported by a K08 Clinical Scientist Development Award from the National Institute on Aging (1K08AG056591). Dr. Prescott is supported by K08 GM115859 from the National Institutes of Health. The views in this manuscript do not reflect the position or policy of the US government or Department of Veterans Affairs. The funders played no role in preparation of this manuscript.
Footnotes
Conflict of Interest Statement: No authors have conflicts of interest to disclose.
References
- 1.Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med 2014;190:62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hua M, Gong MN, Brady J, Wunsch H. Early and late unplanned rehospitalizations for survivors of critical illness. Crit Care Med, 2015/01/20. 2015;43:430–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prescott HC, Langa KM, Iwashyna TJ. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA - J Am Med Assoc, 2015/03/11. 2015;313:1055–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prescott HC, Angus DC. Enhancing Recovery From Sepsis. JAMA 2018;319:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt K, Worrack S, Von Korff M, Davydow D, Brunkhorst F, Ehlert U, Pausch C, Mehlhorn J, Schneider N, Scherag A, Freytag A, Reinhart K, Wensing M, Gensichen J. Effect of a Primary Care Management Intervention on Mental Health–Related Quality of Life Among Survivors of Sepsis. JAMA 2016;315:2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradley EH, Curry L, Horwitz LI, Sipsma H, Wang Y, Walsh MN, Goldmann D, White N, Piña IL, Krumholz HM. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes 2013;6:444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah T, Press VG, Huisingh-Scheetz M, White SR. COPD Readmissions Addressing COPD in the Era of Value-based Health Care 2016;doi: 10.1016/j.chest.2016.05.002. [DOI] [PMC free article] [PubMed]
- 8.Bindman AB, Cox DF. Changes in Health Care Costs and Mortality Associated With Transitional Care Management Services After a Discharge Among Medicare Beneficiaries. JAMA Intern Med 2018;178:1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, Wang Z, Erwin PJ, Sylvester T, Boehmer K, Ting HH, Murad MH, Shippee ND, Montori VM. Preventing 30-Day Hospital Readmissions. JAMA Intern Med 2014;174:1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res, 1974/01/01. 1974;9:208–20. [PMC free article] [PubMed] [Google Scholar]