Abstract
Objective:
A recent meta-analysis identified optimal items for assessing sluggish cognitive tempo (SCT) as distinct from attention-deficit/hyperactivity disorder inattention (ADHD-IN), and a preliminary study with teacher ratings of children in the United States found strong support for the convergent and discriminant validity of 15 SCT items. The current study evaluated whether the same 15 SCT items demonstrated convergent and discriminant validity from ADHD-IN in a large, community-based sample of children in Spain, and whether validity results were replicated across mother, father, and teacher ratings.
Methods:
Mothers, fathers, and teachers completed measures of SCT, ADHD-IN, ADHD-hyperactivity/impulsivity (HI), oppositional defiant disorder (ODD), limited prosocial emotions (LPE), anxiety, depression, shyness, peer rejection, social impairment, and academic impairment on 2,142 Spanish children (49.49% girls; ages 8-13).
Results:
The 15 SCT symptoms demonstrated convergent validity along with discriminant validity with ADHD-IN across all three informants. The SCT symptom ratings also showed measurement invariance across the informants. In addition, SCT and ADHD-IN factors had different and unique associations with the other symptom and impairment factors.
Conclusions:
The 15 SCT symptoms identified in this study – consistent across mother, father, and teacher ratings – appear appropriate to serve as a standard symptom set for assessing SCT in children. Use of a common set of symptoms in future studies will advance our understanding of the SCT construct, including its etiology and developmental progression, associations with ADHD and other psychopathologies, links to impairment, and implications for clinical intervention.
Keywords: sluggish cognitive tempo, ADHD, assessment, attention, factor analysis, measurement
Psychometrically sound measurement is at the heart of research and practice in child and adolescent psychopathology, and when measuring specific symptoms “it is crucial that the same items and instructions are used across assessment occasions” (Hunsley & Mash, 2005, p. 371). As detailed below, the lack of such a symptom set has been a major limitation in the study of sluggish cognitive tempo (SCT), a set of symptoms characterized by excessive daydreaming, staring and ‘spacing out’ behaviors, mental confusion and fogginess, and slowed thinking/behavior (Becker et al., 2016). There is now strong evidence that SCT symptoms are distinct from, yet strongly related to, the inattention symptoms of attention-deficit/hyperactivity disorder (ADHD-IN) (Becker et al., 2016). There is also growing indication that SCT is associated with mental health, academic, and socio-emotional impairments, though far more research is needed in this regard (Barkley, 2014; Becker, 2017; Becker et al., 2016; Mueller et al., 2014).
For the study of SCT to further advance, there is a clear need to identify a standard symptom set informed by rigorous psychometric analysis (Becker et al., 2016; Mueller et al., 2014). Studies examining SCT before the late 2000’s almost always relied on post hoc measures comprised of just two or three items (Carlson & Mann, 2002; Lahey et al., 1988; McBurnett, Pfiffner, & Frick, 2001). More rigorous psychometric work has been conducted in recent years, with a number of parent and teacher ratings scales subsequently emerging from these efforts (Barkley, 2013; Lee, Burns, Snell, & McBurnett, 2014; McBurnett et al., 2014; Penny, Waschbusch, Klein, Corkum, & Eskes, 2009; Willcutt et al., 2014). To be sure, these efforts have each made significant advances to our understanding of the SCT construct, though some thorny issues have also emerged. First, investigators have often used different item pools when developing measures, making it difficult to compare findings across studies. Second, and relatedly, different items – and factor structures – have been used across parent and teacher informants, making it difficult to know if differences are due to informant differences or measurement differences. Third, and perhaps most importantly, some existing measures appear to include at least some items (e.g., lacks initiative, effort on tasks fades quickly) that are not optimal for assessing SCT, at least as distinct from ADHD-IN, which has made it difficult to draw conclusions from the emerging findings (Becker & Langberg, 2014; Smith & Langberg, 2017; Tamm et al., 2016).
To address this latter issue, a meta-analysis recently identified 13 SCT items that consistently demonstrated – across sample types, age ranges, informants, and factor analytic techniques – a primary factor loading on an SCT factor rather than an ADHD-IN factor (Becker et al., 2016). It was concluded that “future studies examining SCT use measures that capture most if not all of these 13 SCT item constructs/domains…It is thus likely that measures will need to be modified and/or new measures developed” (Becker et al., 2016, p.173). As such, the meta-analytic findings led to a careful review and revision of the SCT module of the Child and Adolescent Behavior Inventory (CABI; Burns, Lee, Servera, McBurnett, & Becker, 2015a, 2015b), the most frequently used measure of SCT (Becker et al., 2016). The SCT module of the CABI (previously referred to as the CADBI since it initially focused on only Disruptive behaviors but has since been expanded to include internalizing symptoms) was initially published in 2014 (Lee et al., 2014) and has since undergone careful psychometric evaluation in clinical and nonclinical samples of children and adolescents (spanning from preschool through adolescence) in Asia, Europe, North America, and South America (Belmar, Servera, Becker, & Burns, 2017; Bernad, Servera, Becker, & Burns, 2016; Bernad, Servera, Grases, Collado, & Burns, 2014; Burns, Becker, Servera, Bernad, & García-Banda, 2017; Burns, Servera, Bernad, Carrillo, & Cardo, 2013; Fenollar Cortés, Servera, Becker, & Burns, 2017; Khadka, Burns, & Becker, 2016; Lee, Burns, Beauchaine, & Becker, 2016; Lee, Burns, & Becker, 2016, 2017; Preszler et al., 2017; Servera, Bernad, Carrillo, Collado, & Burns, 2016). However, it was clear following the meta-analytic findings that not all items on the CABI SCT module were optimal for assessing SCT, and conversely, some optimal SCT items were not represented in the CABI measure. Thus, items were reworded or added to align with the 13 items identified in the meta-analysis, and three additional items assessing mental confusion since there was some indication that it would be premature to discard these items from the SCT symptom set (McBurnett et al., 2014).
Becker and colleagues recently provided an initial examination of the revised 16-item CABI SCT module (Becker, Burns, Schmitt, Epstein, & Tamm, 2017). Specifically, teachers provided ratings on SCT and ADHD-IN, as well as global measures of academic and social impairment, for 1,349 children in second through fifth grades. Exploratory structural equation modeling found 15 of the 16 SCT items to demonstrate excellent convergent and discriminant validity with ADHD-IN. The only item that did not demonstrate convergent/discriminant validity was “Lacks motivation to complete tasks (e.g., apathetic)”, which loaded primarily on the ADHD-IN factor rather than the SCT factor. In addition, the 15-item SCT factor was also significantly associated with academic and social impairment above and beyond sex and the ADHD-IN factor (Becker, Burns, et al., 2017). Although promising, this study was preliminary in several regards. Most importantly, it only examined the teacher version of the CABI, was limited to two broad measures of impairment to evaluate external validity, and included students from a single school district in the United States. Clearly, additional studies are needed to evaluate the CABI SCT module across parent and teacher informants, in different cultural contexts, and in relation to range of external correlates.
With these considerations in mind, the present study had four objectives:
To examine the convergent and discriminant validity of the 16 SCT and nine ADHD-IN symptoms with ratings by mothers, fathers, and teachers of Spanish children in a large community sample. This first objective involved two questions— (1) Do the SCT symptoms have substantial loadings on the SCT factor and substantially higher loadings on the SCT factor than the ADHD-IN factor? and (2) Do the ADHD-IN symptoms have substantial loadings on the ADHD-IN factor and substantial higher loadings on the ADHD-IN factor than the SCT factor? The same 15 of 16 SCT symptoms that showed convergent and discriminant validity in the initial study with teacher ratings of United States children (Becker, Burns, et al., 2017) were also expected to show validity for the three sources in the current study. It was also predicted that the nine ADHD-IN symptoms would show convergent and discriminant validity for the three sources.
To evaluate the correlations of SCT and ADHD-IN factors with externalizing behaviors (i.e., ADHD hyperactivity impulsivity [ADHD-HI], oppositional defiant disorder [ODD], and limited prosocial emotions [LPE]), internalizing symptoms (i.e., anxiety and depression), and impairment (i.e., shyness, peer rejection, social impairment, and academic impairment). We examined the correlations of the SCT and ADHD-IN factors with the other symptom and impairment factors for the three sources. Higher SCT and ADHD-IN scores were expected to be associated with higher scores on the externalizing, internalizing, and impairment factors, though we hypothesized differential magnitudes of these correlations based on extant literature (Barkley, 2014; Becker, 2017; Becker et al., 2016; Mueller et al., 2014). First, we expected ADHD-IN to have significantly higher correlations than SCT with ADHD-HI, ODD, and LPE. Second, we expected SCT and ADHD-IN to have approximately equal correlations with anxiety and depression. Third, we expected SCT to have a significantly higher correlation than ADHD-IN with shyness, whereas we expected ADHD-IN to have significantly higher correlations than SCT with peer rejection and global social impairment, especially peer rejection. Finally, we expected ADHD-IN to have a significantly stronger correlation than SCT with global academic impairment.
To determine if the SCT and ADHD-IN factors demonstrate unique associations with the externalizing (ADHD-HI, ODD, and LPE), internalizing (anxiety and depression), and impairment (shyness, peer rejection, social impairment, and academic impairment) factors. First, we hypothesized that higher ADHD-IN scores would predict higher ADHD-HI, ODD, and LPE scores after controlling for SCT whereas higher SCT scores would predict lower ADHD-HI, ODD, and LPE scores after controlling for ADHD-IN (or show no unique relationship after controlling for ADHD-IN) (Becker, Luebbe, Fite, Stoppelbein, & Greening, 2014; Bernad et al., 2016; McBurnett et al., 2014; Penny et al., 2009; Servera et al., 2016). Second, we hypothesized that both SCT and ADHD-IN would have unique positive relationships with anxiety and depression (Bauermeister, Barkley, Bauermeister, Martinez, & McBurnett, 2012; Lee, Burns, & Becker, 2016). Third, we expected SCT to have a unique positive relationship with shyness whereas ADHD-IN’s unique relationship with shyness would be non-significant after controlling for SCT. In contrast, ADHD-IN was expected to have unique positive relationships with peer rejection and social impairment whereas the unique effect of SCT with peer rejection and social impairment factors was predicted to be non-significant, especially with the peer rejection factor (Becker, Garner, Tamm, Antonini, & Epstein, 2017; Khadka et al., 2016; Willcutt et al., 2014). The last prediction was that both ADHD-IN and SCT would have unique relationships with academic impairment yet the unique relationship for ADHD-IN was expected to be stronger (Belmar et al., 2017; Bernad et al., 2016; Khadka et al., 2016; Lee, Burns, Beauchaine, et al., 2016).
To determine if SCT symptom ratings had similar measurement (i.e., invariant like-symptom loadings and thresholds) and structural (i.e., latent factor means) properties across the ratings by mothers, fathers, and teachers. We expected that the symptoms would have similar measurement properties and factor means across the three sources.
Summary of the Present Study
The current study uses the most rigorous procedures to date to identify an optimal set of symptoms to define the SCT construct in children (i.e., SCT symptoms with strong convergent validity as well as discriminant validity with the ADHD-IN construct). The identification of an optimal and standard set of SCT symptoms would make a major contribution in advancing the study – and clinical implications – of SCT, particularly if a standard symptom set is identified across mother, father, and teacher informants. Consistent external validity results for SCT for the three sources would also further strengthen the validity of the construct.
Methods
Participants and Procedures
All 257 elementary schools on the Balearic Islands (Spain) were invited to participate in the study (i.e., a study to improve the assessment and understanding of common child behaviors). A total of 48 schools expressed an interest in the study with 37 schools randomly selected from these 48 schools for additional contact (i.e., grant resources allowed for the recruitment of approximately 37 schools). The investigators met with the principals of these 37 schools to determine the ability of the schools to participate in the study (e.g., the principals’ opinion about the expected level of participation of mothers, fathers, and teachers and available school space to facilitate data collection). A total of 32 of these 37 schools were then selected for the study. There were 5,376 3rd-6th-grade children in these 32 schools.
The principals next provided study staff with a list of the teachers from these 32 schools that wanted to learn more about the study (i.e., if a teacher indicated no interest in the project, then this eliminated the students in the teacher’s class from consideration in the project). The school was also asked to exclude children who did not speak Spanish or had severe special education needs (e.g., educated in a self-contained classroom). These exclusionary criteria (teacher did not wish to learn more about the study, child did not speak Spanish in school, child had severe special education needs) resulted in 3,855 children whose parents were contacted by the researchers. All the teachers who indicated a desire to learn more about the study subsequently agreed to participate in the study after permission was obtained from parents to ask the teachers to participate. Each of the schools was paid approximately 100 dollars for their participation.
An informed consent form was given to the parents of the 3,855 children and with parental written approval a similar informed consent form was given to the teachers. This procedure could result in the completion of the rating scale only by teachers (i.e., teacher completed the ratings while the parent did not return the scales). The participants were mothers, fathers, and teachers of 2,142 children (50.51% boys) from these 32 schools. Mothers and fathers provided ratings on 1,648 and 1,358 children, respectively (i.e., 1,777 unique children were rated by parents). A total of 196 teachers provided ratings on 1,773 children with each teacher rating an average of 10.93 (SD = 6.05, range = 1 to 27) children. The number of children from the third, fourth, fifth, and sixth grades were 598, 616, 400, and 528, respectively, with the mean age of the children being 10.30 (SD = 1.21, range = 8 to 13) years. Approximately 90% of the children were Caucasian and 10% North African (ethnicity was not collected on the individual children with these percentages representing the demographics of the 32 schools).
Diagnostic characteristics of the children.
Parents were asked to indicate if their child had any chronic illness, mental disorder, or learning problem. Parents indicated that a total of 5.13% of the children had an ADHD diagnosis with 4.86% learning problems, 3.84% medical problems (mostly asthma), 0.72% pervasive developmental disorders, 0.24% intellectual disability, 0.12% tics, and 0.06% enuresis.
Characteristics of mothers and fathers.
Table 1 shows the educational, marital, and employment status of the mothers and fathers. The primary and secondary educational categories correspond to 10 and 12 (high school diploma) years of school, respectively. The vocational training category involves technical degree programs (e.g., electricians, plumbers, mechanics, administrators) of three to five years after the high school diploma with the university category involving graduation from a university.
Table 1.
Characteristics (Percent) of Mothers and Fathers
| Mothers | Fathers | |
|---|---|---|
| Education | ||
| Primary | 17.17 | 24.52 |
| Secondary | 19.05 | 21.72 |
| Vocational Training | 23.06 | 20.77 |
| University | 37.14 | 29.31 |
| Missing | 3.58 | 4.68 |
| Family Status | ||
| Married | 84.04 | 85.79 |
| Divorced | 10.86 | 9.35 |
| Widowed | 0.67 | 0.37 |
| Single | 2.91 | 1.69 |
| Missing | 1.52 | 2.80 |
| Employment | ||
| Homemaker | 11.17 | 2.95 |
| Unemployed benefits | 4.92 | 2.80 |
| Unemployed no benefits | 3.28 | 1.55 |
| Occasional employment | 12.50 | 10.75 |
| Permanent employment | 62.01 | 70.91 |
| Retired | 0.12 | 0.88 |
| Missing | 6.00 | 10.16 |
Note. Primary education was 10 years of education and secondary education was 12 years of education (i.e., high school graduation). The number of participants for mothers and fathers were 1,648 and 1,358, respectively.
Measures
Child and Adolescent Behavior Inventory (CABI).
Parents and teachers completed their respective versions of the CABI (Burns et al., 2015a, 2015b). The CABI measures SCT (16 symptoms), ADHD-IN (nine symptoms), ADHD-HI (nine symptoms), ODD (eight symptoms), prosocial emotions (four symptoms of the DSM-5 Limited Prosocial Emotions specifier), anxiety (six symptoms) depression (six symptoms), social impairment (four items for parents [quality of interactions with parents, other adults, siblings, and peers] and two items for teachers [quality of interactions with adults and peers], and academic impairment (five items: quality of homework/classwork, reading skills, arithmetic skills, writing skills, and global academic skills). Table 3 shows the wording of the 16 SCT symptoms. Earlier studies show the wording of the anxiety and depression symptoms (Lee, Burns, & Becker, 2016) and the prosocial emotions symptoms (Seijas, Servera, García-Banda, Barry, & Burns, 2017).
Table 3.
Standardized Primary and Secondary Factor Loadings of Sluggish Cognitive Tempo and ADHD Inattention Symptoms on Sluggish Cognitive Tempo and ADHD-Inattention Factors
| Mothers |
Fathers |
Teachers |
||||
|---|---|---|---|---|---|---|
| Item | SCT | IN | SCT | IN | SCT | IN |
| Sluggish Cognitive Tempo Symptoms | ||||||
| 1. Behavior is slow | 0.86* | −0.23* | 0.81* | −0.21* | 1.17* | −0.43 |
| 2. Lost in a fog | 0.62* | 0.24* | 0.70* | 0.16* | 0.79* | 0.18* |
| 3. Stares blankly into space | 0.69* | 0.06ns | 0.77* | −0.01ns | 0.87* | 0.08ns |
| 4. Drowsy or sleepy during the day | 0.82* | −0.18* | 0.71* | −0.05ns | 0.97* | −0.12* |
| 5. Daydreams | 0.58* | 0.06ns | 0.63* | −0.07ns | 0.76* | 0.11ns |
| 6. Loses train of thought | 0.74* | 0.13* | 0.72* | 0.13* | 0.74* | 0.20* |
| 7. Low level of activity | 0.95* | −0.30* | 0.89* | −0.28* | 1.14* | −0.31* |
| 8. Gets lost in own thoughts | 0.66* | 0.17* | 0.74* | 0.11ns | 0.81* | 0.14* |
| 9. Easily tired or fatigued | 0.86* | −0.22* | 0.79* | −0.21* | 0.86* | −0.01ns |
| 10. Forgets what was going to say | 0.79* | 0.00 | 0.78* | 0.03ns | 0.72* | 0.20* |
| 11. Easily confused | 0.76* | 0.11* | 0.75* | 0.13* | 0.81* | 0.15* |
| 12. Low motivation to complete tasks | 0.23* | 0.63* | 0.23* | 0.62* | 0.28* | 0.67* |
| 13. Spaces or zones out | 0.59* | 0.29* | 0.64* | 0.26* | 0.64* | 0.34* |
| 14. Gets mixed up | 0.78* | 0.12* | 0.73* | 0.16* | 0.79* | 0.18* |
| 15. Thinking is slow | 0.84* | 0.01ns | 0.75* | 0.12* | 0.82* | 0.10ns |
| 16. Difficulty expressing thoughts | 0.75* | 0.05ns | 0.73* | 0.06ns | 0.78* | 0.10ns |
| ADHD-Inattention Symptoms | ||||||
| 1. Close attention to details | 0.07* | 0.78* | 0.01ns | 0.83* | 0.13* | 0.82* |
| 2. Sustaining attention | 0.01ns | 0.91* | 0.00ns | 0.92* | 0.14* | 0.85* |
| 3. Listening when spoken to directly | 0.15* | 0.72* | 0.18* | 0.71* | 0.21* | 0.72* |
| 4. Follow through on instructions | −0.04ns | 0.91* | −0.02ns | 0.90* | 0.00ns | 0.96* |
| 5. Organizational skills | −0.03ns | 0.86* | 0.01ns | 0.88* | 0.00ns | 0.96* |
| 6. Avoids tasks requiring sustained effort | 0.03ns | 0.86* | 0.03ns | 0.87* | 0.10* | 0.84* |
| 7. Loses things | 0.00ns | 0.77* | −0.04ns | 0.79* | −0.09* | 0.97* |
| 8. Easily distracted | 0.03ns | 0.90* | 0.03ns | 0.89* | 0.08* | 0.87* |
| 9. Forgetful | −0.01ns | 0.89* | 0.01ns | 0.87* | 0.01ns | 0.94* |
Note. Partial standardized regression coefficients can be larger than 1.00 with cross-loadings and correlated factors. ADHD = attention-deficit/hyperactivity disorder. IN = inattention. SCT = sluggish cognitive tempo.
p < .05;
= non-significant.
Parents and teachers were instructed to base their ratings on the past month. Parents were also told to make their ratings independently. The SCT, ADHD, ODD, anxiety, and depression symptoms were rated on a 6-point scale (i.e., almost never [never or about once per month], seldom [about once per week], sometimes [several times per week], often [about once per day], very often [several times per day], and almost always [many times per day]. The prosocial emotions symptoms were rated on a slightly different 6-point scale (i.e., almost never [0 to 10% of the time], seldom [11 to 20% of the time], sometimes [21 to 49% of the time], often [50 to 79% of the time], very often [80 to 89% of the time], and almost always [90 to 100% of the time]. A 7-point scale was use for the academic and social impairment items (i.e., severe difficulty, moderate difficulty, slight difficulty, average performance [average interactions] for grade level, slightly above average, moderately above average, and excellent performance [excellent interactions] for grade level). The prosocial emotions, academic impairment, and social impairment items were reverse keyed so that higher scores represent lower (limited) prosocial emotions, greater academic impairment, and greater social impairment, respectively. The prosocial emotions scale will now be referred to as a measure of limited prosocial emotions (LPE) to indicate that higher scores represent lower levels of prosocial emotions.
Earlier studies provide support for the reliability (internal consistency, test-retest, inter-rater) and validity of scores from the ADHD-IN, ADHD-HI, ODD, LPE, anxiety, depression, social impairment, and academic impairment subscales (Becker, Burns, et al., 2017; Belmar et al., 2017; Bernad et al., 2016; Bernad et al., 2014; Burns et al., 2017; Khadka et al., 2016; Lee et al., 2016, 2017; Seijas et al., 2017). Cronbach’s alpha and the inter-rater factor correlations for the CABI scales for this study are shown in Table 2. Each of the CABI scales showed good (anxiety scale) to excellent (all other scales) internal consistency (alpha). The interrater factor correlations were also good to excellent for mothers with fathers with most of the across setting (i.e., mothers with teachers, fathers with teachers) factor correlations being good for across settings values. The reliability of the revised SCT scale of the CABI is discussed in in the Results section below.
Table 2.
Reliability Coefficients (Cronbach’s Alpha) and Interrater Factor Correlations (Standard Errors)
| Alpha values |
Inter-rater factor correlations |
|||||
|---|---|---|---|---|---|---|
| Mothers | Fathers | Teachers | Mothers with Fathers | Mothers with Teachers | Fathers with Teachers | |
| Sluggish Cognitive Tempo | .93 | .92 | .97 | .81 (.02) | .43 (.02) | .42 (.03) |
| Inattention | .95 | .95 | .97 | .83 (.01) | .55 (.02) | .54 (.03) |
| Hyperactivity/Impulsivity | .93 | .93 | .96 | .79 (.02) | .40 (.03) | .44 (.03) |
| Oppositional Defiant Disorder | .92 | .91 | .95 | .75 (.02) | .30 (.03) | .30 (.04) |
| Limited Prosocial Emotions | .84 | .85 | .88 | .67 (.02) | .22 (.03) | .15 (.03) |
| Anxiety | .72 | .75 | .85 | .66 (.03) | .19 (.04) | .15 (.04) |
| Depression | .87 | .84 | .92 | .73 (.03) | .43 (.03) | .37 (.04) |
| Shyness | .78 | .78 | .82 | .75 (.02) | .16 (.04) | .20 (.04) |
| Social Impairment | .90 | .91 | .87 | .70 (.02) | .18 (.03) | .14 (.03) |
| Academic Impairment | .94 | .95 | .97 | .87 (.01) | .72 (.02) | .69 (.02) |
| Peer Rejection | -- | -- | .85 | -- | -- | -- |
Note. The peer rejection measure was only completed by teachers. All inter-rater factor correlations significant at p < .001
Child Social Preference Scale (CSPS).
The CSPS (Coplan, Prakash, O’Neil, & Armer, 2004) was developed as a parent-report measure of children’s conflicted shyness (experiencing social fears/withdrawal despite a desire to interact socially) and social disinterest (lacking a strong motivation to engage in social interaction). Only the conflicted shyness subscale (7 items; e.g., “My child will turn down social initiations from other children because he/she is shy,” “My child seems to want to play with others but is sometimes nervous to”) was used in the current study. Previous research supports the reliability and validity of the CSPS conflicted shyness scales, including associations with temperamental wariness of social novelty, teacher-rated anxiety and behavioral withdrawal, and observed reticent behavior and parallel play during free play with peers (Coplan et al., 2004). For the present study, the CSPS was adapted for completion by teachers (changing “My child…” to “This child…”) in addition to mothers and fathers. For each item, parents (teachers) responded to the question “How much is your child (this child) like that?” on a five-point scale (ranging from 1 = not at all to 5 = a lot). The internal consistency values ranged from .78 to .87 with the interrater correlation for mothers with fathers being .75 and the values for mothers with teachers and fathers with teachers being .16 and .20, respectively.
Dishion Social Acceptance Scale (DSAS).
Two items from the DSAS (Dishion, 1990) were used to create a latent variable of peer rejection. Specifically, teachers rated the proportion of classmates who “like” and “dislike” the child on a 5-point scale ((very few [less than 25%]; some [25 to 49%]; about half [50%]; many [51% to 75%]; and almost all [greater than 75%]), and these two items were used to index peer rejection (the “like” item reversed). The reliability coefficient for the two-item measure was .85.
Analytic Approach
Estimation and clustering.
The analyses used the Mplus statistical software, version 8.0 (Muthén & Muthén, 1998-2017). The items were treated as categorical indicators with the use of the robust weighted least squares estimator (WLSMV). Given the children were clustered within teachers, the Mplus type=complex option was used to correct the standard errors.
Criteria for model fit.
Global model fit was evaluated with the comparative fit index (CFI; acceptable fit ≥.90 and close fit ≥.95), Tucker Lewis Index (TLI; acceptable fit ≥.90 and close fit ≥.95), and the root-mean-square error of approximation (RMSEA; acceptable fit ≤.08 and close fit ≤.05) (Little, 2013). These procedures were used to evaluate global model fit given the chi-square value is not a practical measure of fit with large sample sizes (Little, 2013).
Study Objective 1: Convergent and discriminant validity of SCT and ADHD-IN symptoms.
An exploratory two-factor confirmatory factor analysis (CFA) model was applied to the 16 SCT and 9 ADHD-IN symptoms (Asparouhov & Muthén, 2009). These analyses allowed the SCT symptoms to cross-load on the ADHD-IN factor and the ADHD-IN symptoms to cross-load on the SCT factor. For an SCT symptom to have convergent validity, the loading needed to be greater than approximately .60. For an SCT symptom to have discriminant validity, the cross loading on the ADHD-IN factor had to be less than approximately .30 (a cross-loading close to zero would be ideal) with the primary loading being greater than approximately .60. These criteria were used to identify a set of SCT symptoms with convergent and discriminant validity across the three sources. The same procedure was used to evaluate the ADHD-IN symptoms. These loadings are partial standardized regression coefficients because the analysis allows cross-loadings and correlations between the two factors (Brown, 2015; chap. 2). It is possible for such loadings to be larger than 1.00.
Study Objective 2: Correlations of SCT and ADHD-IN factors with other symptom and impairment factors.
An exploratory CFA model was applied to the measures for the three sources (i.e., three different analyses). For these analyses, the SCT and ADHD-IN factors had cross-loadings while the other symptom (ADHD-HI, ODD, LPE, anxiety, and depression) and impairment (shyness, peer rejection, social impairment, and academic impairment) factors were not allowed to have cross-loadings with each other or with the SCT and ADHD-IN factors. This procedure results in more accurate correlations of the SCT and ADHD-IN factors with the other symptom and impairment dimensions (Asparouhov & Muthén, 2009). The Mplus model constraint procedure was used to determine if the SCT and ADHD-IN factor correlations with the other symptom and impairment factor differed significantly.
Study Objective 3: Unique associations of SCT and ADHD-IN factors with other symptom and impairment factors.
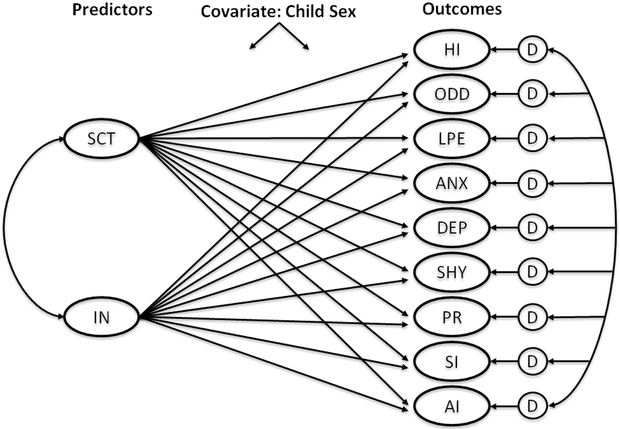
An exploratory structural regression analysis (Asparouhov & Muthén, 2009) was used to determine the unique associations of the SCT and ADHD-IN factors with other symptom (ADHD-HI, ODD, LPE, anxiety, and depression) and impairment (shyness, peer rejection, social impairment, and academic impairment) factors. For these analyses, the SCT and ADHD-IN factors had cross-loadings while the other symptom and impairment factors were not allowed to have cross-loadings with each other or with the SCT and ADHD-IN factors. This procedure results in more accurate partial regression coefficients of the SCT and ADHD-IN factors with the other symptom and impairment dimensions (Asparouhov & Muthén, 2009). These analyses also controlled for the effect of the children’s sex on the predictors and outcomes (Little, 2013). Figure 1 shows the structural regression path diagram for these analyses.
Figure 1.
Exploratory structural regression analysis. The SCT manifest variables (items) were allowed to cross-load on ADHD-IN and the ADHD-IN manifest variables were allowed to cross-load on SCT. None of the other manifest variables were allowed to cross-load on the other factors. Manifest variables are not shown to simply the figure. Predictors and outcomes were regressed on the covariate, child sex. SCT = sluggish cognitive tempo; IN = ADHD-inattention; HI = ADHD-hyperactivity/impulsivity; ODD = oppositional defiant disorder; LPE = limited prosocial emotions; ANX = anxiety; DEP = depression; SHY = shyness; PR = peer rejection; SI = global social impairment; AI = global academic impairment; D = disturbance.
Study Objective 4: Invariance of SCT symptom ratings across raters.
Invariance analyses were performed to determine the invariance of SCT symptom ratings across raters. These analyses also determined if there were significant differences on the SCT factor mean as a function of rater. Two procedures were used to evaluate the invariance of like-symptom loadings and thresholds. First, if the decrease in the CFI was less than .01 and the increase in the RMSEA value was less than .015, then the constraints on like-symptom loadings and thresholds were considered tenable (Little, 2013). Second, if the model with the constraints on like-symptom loadings and like-symptom thresholds did not result in a significant decrement in fit (p < .001), then the results were considered to suggest invariance. The p-value for this test was set at p < .001 given the large size of the sample (Little, 2013). If these two guidelines both suggest invariance, then such would be strong support for the invariance of like-symptom loadings and thresholds.
Results
Missing Information
Covariance coverage was greater than 99% for all variances and covariances for each source. Mothers, fathers, and teachers thus left very few items blank.
Convergent and Discriminant Validity of SCT and ADHD-IN Symptoms
Table 3 shows the loadings for SCT and ADHD-IN symptom ratings for mothers, fathers, and teachers. The SCT symptom lacks motivation to complete tasks failed to have a substantial loading on the SCT factor for mothers, fathers, and teachers (i.e., 0.23 to 0.28). This SCT symptom also had higher loadings on the ADHD-IN factor (i.e., 0.62 to 0.67) than the SCT factor (i.e., 0.23 to 0.28) for the three sources. The other 15 SCT symptoms had substantial loadings on the SCT factor (i.e., 0.58 to 1.17) and much lower loadings on the ADHD-IN factor (i.e., −0.41 to .34) for the three sources. These 15 SCT symptoms defined the SCT construct for the subsequent analyses (i.e., 15 SCT symptoms with the loading in bold in Table 3). The nine ADHD-IN symptoms showed substantial loadings on the ADHD-factor (i.e., 0.71 to 0.96) with loadings close to 0.00 on the SCT factor (i.e., −0.09 to 0.21). An SCT (15 symptoms) and ADHD-IN (9 symptoms) two-factor model provided a significantly (ps < .0001) better fit than a one-factor model for each source.
Reliability of 15 SCT Symptoms with Convergent and Discriminant Validity
The reliability (Cronbach’s alpha) values of the 15 SCT symptoms were 0.93, 0.92, and 0.97 for mothers, fathers, and teachers, respectively. The mother with father SCT factor correlation for SCT was .81 (SE = .02) with the SCT factor correlations for mothers with teachers and fathers with teachers being .43 (SE = .02) and .42 (SE = .03), respectively.
Fit of the Exploratory CFA Models
An exploratory CFA was used to evaluate the fit of a model with the SCT and ADHD-IN factors along with the other symptom and impairment factors for the three sources. Each of these three analyses yielded a close fit (CFI range: 0.969 to 0.973, TLI range: 0.967 to 0.973, RMSEA range: 0.029 to 0.035 with the largest upper value for the 90% confidence interval being 0.036).
Correlations of SCT and ADHD-IN Factors
The correlation between the SCT and ADHD-IN factors was .67 (95% CI: .607, .729), .72 (95% CI: .632, .813), and .81 (95% CI: .769, .845) for mothers, fathers, and teachers, respectively. For mothers, the two factors shared 45% of their true score variance with 55% of the true score variance being unique with the respective values for fathers being 52% and 48% and for teachers 66% and 34%.
Correlations of SCT and ADHD-IN Factors with Other Symptom and Impairment Factors
Table 4 shows the correlations of the SCT and ADHD-IN factors with the symptom and impairment factors. We summarize these correlations in the context of externalizing (i.e., ADHD-HI, ODD, and LPE factors), internalizing (i.e., anxiety and depression factors), social impairment (i.e., shyness, peer rejection, and social impairment factors), and academic impairment (i.e., academic impairment factor) dimensions.
Table 4.
Correlations of SCT and ADHD-IN Factors with Outcome Factors
| HI r (SE) |
ODD r (SE) |
LPE r (SE) |
ANX r (SE) |
DEP r (SE) |
SHY r (SE) |
SI r (SE) |
AI r (SE) |
PR r (SE) |
|
|---|---|---|---|---|---|---|---|---|---|
| Mother SCT and IN with Mother Outcomes | |||||||||
| SCT | 0.35 (.03)a | 0.43 (.03)a | .20 (.03)a | 0.57 (.02)a | 0.67 (.02)a | 0.36 (.03)a | 0.30 (.03)a | .50 (.03)a | -- |
| IN | 0.66 (.02)b | 0.61 (.02)b | .30 (.03)b | 0.48 (.02)b | 0.69 (.02)a | 0.24 (.03)b | 0.33 (.02)a | .69 (.01)b | -- |
| Fathers SCT and IN with Father Outcomes | |||||||||
| SCT | 0.45 (.04)a | 0.47 (.03)a | .25 (.03)a | 0.60 (.02)a | 0.69 (.02)a | 0.35 (.03)a | 0.30 (.03)a | .51 (.04)a | -- |
| IN | 0.69 (.02)b | 0.63 (.02)b | .30 (.03)a | 0.46 (.03)b | 0.63 (.02)b | 0.20 (.03)b | 0.34 (.02)a | .68 (.02)b | -- |
| Teacher SCT and IN with Teacher Outcomes | |||||||||
| SCT | 0.27 (.04)a | 0.34 (.03)a | .39 (.03)a | 0.61 (.02)a | 0.78 (.02)a | 0.62 (.02)a | 0.50 (.03)a | .72 (.02)a | .50 (.03)a |
| IN | 0.64 (.02)b | 0.59 (.02)b | .50 (.03)b | 0.58 (.03)a | 0.77 (.02)a | 0.49 (.03)b | 0.54 (.02)a | .79 (.01)b | .58 (.03)b |
Note. All correlations significant a p < .001. Correlations for the same outcome with different superscripts differ at p < .001 with the exception of SCT and IN with depression for fathers (p < .02). SCT=sluggish cognitive tempo; IN=inattention; HI=hyperactivity/impulsivity; ODD = oppositional defiant disorder; ANX=anxiety; DEP=depression; SHY=shyness; SI=social impairment; AI=academic impairment; PR= peer rejection.
Externalizing symptom dimensions.
Higher scores on the SCT and ADHD-IN factors were associated with significantly (ps < .001) higher scores on the ADHD-HI, ODD, and LPE factors for each of the three sources. In addition, the ADHD-IN factor had significantly (ps < .001) stronger correlation than the SCT factor with the ADHD-HI, ODD, and LPE factors for each source.
Internalizing symptom dimensions.
Higher scores on the SCT and ADHD-IN factors were associated with significantly (ps < .001) higher scores on the anxiety and depression factors. For two of the three comparisons for anxiety (mothers and fathers but not teachers) and one of the three comparisons for depression (father only), the SCT factor showed a significantly (ps < .02) stronger correlation than the ADHD-IN factor.
Social impairment dimensions.
Higher scores on the SCT and ADHD-IN factors were associated with significantly higher (ps < .001) scores on the shyness, social impairment, and peer rejection factors. For the shyness factor, SCT showed a significantly (ps < .001) stronger relationship than ADHD-IN for each of the three sources. For the peer rejection factor (a teacher measure only), in contrast, ADHD-IN showed a significantly (p < 001) stronger relationship than SCT. The SCT and ADHD-IN factors correlations with the social impairment factor did not differ significantly (ps > .05).
Academic impairment.
Higher scores on the SCT and ADHD-IN factors were associated with significantly (ps < .001) higher scores on the academic impairment factor. The ADHD-IN factor had a significantly (ps < .001) stronger correlation than the SCT factor with academic impairment.
Correlation of Child Sex with SCT and ADHD-IN Factors
The correlation of sex (girls = 0, boys = 1) with the SCT factor for ratings by mothers, fathers, and teachers was .06 (SE = .03, p = .03), .08 (SE = .03, p = .01), and .14 (SE = .03, p < .001), respectively. The respective values for sex with the ADHD-IN factor were .15 (SE = .03, p < .001), .16 (SE = .03, p < .001), and .23 (SE = .03, p < .001). Sex had a significantly (ps < .001) larger correlation with the ADHD-IN factor than the SCT factor for each source. Sex was also significantly (ps < .05) correlated with 21 of 25 of the other symptom and impairment factors for the three sources. Sex was thus used as a covariate for the predictors (SCT and ADHD-IN factors) and outcomes (other symptom and impairment factors) for the structural regression analysis in the next section (Figure 1).
Unique Relationships of SCT and ADHD-IN with Other Symptom and Impairment Factors
Table 5 shows the standardized partial regression coefficients for the unique relationships of SCT and ADHD-IN factors with the symptom and impairment factors.
Table 5.
Partial Standardized Regression Coefficients for the Associations of SCT and ADHD-IN Factors with Outcome Factors
| HI β (SE) |
ODD β (SE) |
LPE β (SE) |
ANX β (SE) |
DEP β (SE) |
SHY β (SE) |
SI β (SE) |
AI β (SE) |
PR β (SE) |
|
| Mother SCT and IN with Mother Outcomes | |||||||||
| SCT | −0.16 (.03)** | 0.04 (.04)ns | 0.01 (.04)ns | 0.42 (.04)** | 0.39 (.04)** | 0.36 (.04)** | 0.15 (.04)** | .07 (.03)* | -- |
| IN | 0.77 (.03)** | 0.58 (.03)** | 0.27 (.04)** | 0.21 (.04)** | 0.42 (.04)** | 0.00 (.04)ns | 0.22 (.04)** | .65 (.03)** | -- |
| Father SCT and IN with Father Outcomes | |||||||||
| SCT | −0.09 (.04)* | 0.05 (.04)ns | 0.07 (.05)ns | 0.55 (.06)** | 0.51 (.05)** | 0.44 (.06)** | 0.12 (.05)* | .05 (.04)ns | -- |
| IN | 0.75 (.03)** | 0.59 (.04)** | 0.24 (.04)** | 0.07 (.04)ns | 0.25 (.07)** | −0.12 (.07)ns | 0.25 (.05)** | .64 (.04)** | -- |
| Teacher SCT and IN with Teacher Outcome | |||||||||
| SCT | −0.68 (.07)** | −0.38 (.06)** | −0.01 (.05)ns | 0.38 (.05)** | 0.44 (.04)** | 0.64 (.06)** | 0.19 (.06)** | .17 (.03)** | .08 (.06)ns |
| IN | 1.15 (.06)** | 0.88 (.06)** | 0.48 (.05)** | 0.29 (.05)** | 0.42 (.04)** | −0.03 (.06)ns | 0.38 (.05)** | .67 (.03)** | .52 (.06)** |
Note. These analyses also controlled for the sex of the child. SCT=sluggish cognitive tempo; IN=inattention; HI=hyperactivity/impulsivity; ODD = oppositional defiant disorder; ANX=anxiety; DEP=depression; SHY=shyness; SI=social impairment; AI=academic impairment; PR= peer rejection.
p < .05;
p < .001;
= non-significant.
Externalizing symptom dimensions.
Higher scores on the ADHD-IN factor were still associated with significantly (ps < .05) higher scorers on the ADHD-HI, ODD, and LPE factors after controlling for the SCT factor (all three sources), while higher scores on the SCT factor were associated with significantly (ps < .05) lower scores on the ADHD-HI factor (all three sources) and the ODD factor (teachers only) after controlling for ADHD-IN factor. SCT was no longer significantly (ps > .15) related to ODD (mothers and fathers) and LPE (all three sources) after controlling for ADHD-IN.
Internalizing symptom dimensions.
Higher scores on the SCT factor were still associated with significantly (ps < .001) higher scores on the anxiety and depression factors after controlling for ADHD-IN for each source. Higher scores on the ADHD-IN factor were also still associated with significantly (ps < .001) higher scores on anxiety and depression after controlling for SCT with one exception (for fathers, ADHD-IN was not uniquely associated with anxiety).
Social impairment dimensions.
Higher scores on the SCT factor were still associated with significantly (ps < .001) higher scores on the shyness factor after controlling for the ADHD-IN factor (all three sources), while the ADHD-IN factor was no longer significantly (ps > .05) associated with the shyness factor after controlling for SCT (all three sources). For the social impairment factor, higher scores on SCT and ADHD-IN both uniquely predicted higher levels of social impairment (ps < .05). In contrast, only higher scores on the ADHD-IN factor uniquely predicted higher scores on the peer rejection factor (p < .001).
Academic impairment.
Higher scores on the ADHD-IN factor were associated with significantly (ps < .001) higher scores on the academic impairment factor even after controlling for SCT (all three sources), while higher scores on the SCT factor were associated with significantly (ps < .05) higher scores on the academic impairment factor after controlling for ADHD-IN for only mothers and teachers (not fathers).1
Invariance of 15 SCT Symptom Ratings across Mothers, Fathers, and Teachers
Mothers with fathers.
The model with no constraints on like symptom loadings and thresholds across the SCT symptom ratings for mothers and fathers yielded an acceptable fit, χ2(389) = 3382, p < .001, CFI = .944, TLI = .937, and RMSEA = .065 (.063, .067). The model with constraints on like symptom loadings and thresholds also yielded an acceptable fit with no decrement in fit values, χ2(462) = 3202, p < .001, CFI = .948, TLI = .951, and RMSEA = .058 (.056, .060). In addition, the WLSMV χ2 difference test indicated that the model with the constraints on like symptom loadings and thresholds did not result in a statistically significant decrement in fit relative to the baseline model, χ2 difference test (73) = 61.46, p = .83. The SCT factor mean did not differ significantly for mothers and fathers (i.e., Mdifference = 0.01, SE = .03, p = .84, Cohen’s latent d = .01, SE = .03, p = .84).
Parents with teachers.
With the constraints on like symptom loadings and thresholds remaining in place for mothers with fathers, the addition of teacher ratings of the SCT symptoms yielded a baseline model with close fit, χ2(971) = 3935, p < .001, CFI = .973, TLI = .973, and RMSEA = .038 (.037, .039). In this model symptom loadings and thresholds for teachers were not constrained equal to parents. Constraining like symptom loadings and thresholds for teachers equal to parents also yielded a model with close fit as well as no decrement in global fit values, χ2(1044) = 4067, p < .001, CFI = .973, TLI = .974, and RMSEA = .037 (.036, .038). These results suggest the SCT symptoms had similar measurement properties across parents and teachers. The WLSMV χ2 difference test, however, indicated that the model resulted in a significant decrement in fit, χ2 difference test (73) = 325, p < .001 (the loadings for teachers tended to be higher). The SCT factor means did not differ significantly for parents and teachers (Mdifference = 0.13, SE = .08, p = .11, Cohen’s latent d = .08, SE = .06, p = .13). Conclusions about this mean difference should be considered tentative given the inconsistency between the lack of a decrease in global fit values and the significant χ2 difference test.
Exploratory Analyses Examining Unique Effects of SCT and IN with Parent-Reported Diagnoses and Problems
Table 6 shows partial probit regression coefficients for the regression of three binary outcomes (i.e., ADHD diagnosis [5.13%], learning problems [4.86%], and medical problems [3.84%, mostly asthma]) on the SCT and ADHD-IN factors [cross-loadings allowed on SCT and ADHD-IN factors]). These analyses also controlled for sex of the child. For mothers, fathers, and teachers, higher scores on ADHD-IN were uniquely associated (ps < .001) with an ADHD diagnosis while higher scores on SCT were uniquely (p < .001) associated with an ADHD diagnosis only for fathers. Higher scores on ADHD-IN uniquely (ps < .05) predicted learning problems for mothers and teachers while higher scores SCT uniquely (p < .001) predicted learning problems for only mothers. Finally, higher scores on SCT uniquely (ps < .05) predicted medical problems for mothers and fathers while higher scores on ADHD-IN uniquely (ps < .07) predicted the absence of medical problems for mothers and fathers.
Table 6.
Partial Probit Regression Coefficients for the Associations of SCT and ADHD-IN Factors with ADHD Diagnosis, Learning Problems, and Medical Problems Outcomes
| ADHD Diagnosis | Learning Problems | Medical Problems | |
|---|---|---|---|
| Source | b (SE) | b (SE) | b (SE) |
| Mothers | |||
| Sluggish cognitive tempo | 0.10 (.08)ns | 0.31 (.07)** | 0.39 (.08)** |
| ADHD-Inattention | 0.61 (.08)** | 0.20 (.07)* | −0.21 (.04)* |
| Fathers | |||
| Sluggish cognitive tempo | 0.32 (.08)** | 0.36 (.12)* | 0.25 (.10)* |
| ADHD-Inattention | 0.41 (.08)** | 0.16 (.13)ns | −0.17 (.10)+ |
| Teachers | |||
| Sluggish cognitive tempo | 0.09 (.10)ns | 0.16 (.10)ns | 0.20 (.14)ns |
| ADHD-Inattention | 0.51 (.09)** | 0.26 (.10)* | −0.08 (.14)ns |
Note. These analyses also controlled for the sex of the child (i.e., the three binary outcomes were regressed on the sluggish cognitive tempo and ADHD-Inattention factors along with the sex of child). Asthma was the primary medical problem listed. ADHD = attention-deficit/hyperactivity disorder. SCT = sluggish cognitive tempo.
p < .10;
p < .05;
p < .001;
= non-significant.
Descriptive Information on the SCT Measure
Table 7 shows descriptive information on the SCT measure for girls and boys. This information is presented to facilitate the comparison of mean scores using this measure in future studies as well as provide tentative norms for Spanish children within this age range (8 to 13 years) as well as Spanish-speaking families within the United States. The 90th (95th) SCT scores (0 to 5 scale) for boys were 1.53 (2.00), 1.47 (1.93), and 2.80 (3.47) for ratings by mothers, fathers, and teachers, respectively. The 90th (95th) SCT scores for girls were 1.47 (1.93), 1.33 (1.73), and 2.20 (3.00) for ratings by mothers, fathers, and teachers, respectively.
Table 7.
Descriptive Information on 15 Item Sluggish Cognitive Tempo Manifest Measure
| Girls | Boys | |||||||
|---|---|---|---|---|---|---|---|---|
| N | M | SD | Range | N | M | SD | Range | d |
| Ratings by Mothers | ||||||||
| 822 | 0.56a | 0.68 | 0 to 3.67 | 826 | 0.63b | 0.72 | 0 to 4.33 | .10 |
| Ratings by Fathers | ||||||||
| 669 | 0.51a | 0.63 | 0 to 4.40 | 689 | 0.59b | 0.65 | 0 to 3.67 | .13 |
| Ratings by Teachers | ||||||||
| 865 | 0.73a | 1.09 | 0 to 4.80 | 908 | 0.99b | 1.16 | 0 to 5.00 | .24 |
Note. Sluggish cognitive tempo was rated on a 0 to 5 scale. Row means with different superscripts differ a p < .05. Higher scores represent greater symptom occurrence. The children were in third to sixth grades (ages 8-13 years). d = Cohen’s d for manifest variable means.
Discussion
Findings from this study mark a major step towards the goal to “identify the best symptom set for defining and assessing SCT” (Becker et al., 2016, p. 175). The assessment of SCT has progressed significantly since the SCT construct initially emerged in the scientific literature in the 1980’s (Becker, Marshall, & McBurnett, 2014), with a major rise in the interest in SCT measurement emerging in the late 2000’s (Penny et al., 2009). Given the number of items used to assess the SCT construct across different studies and measures, a recent meta-analysis identified optimal aspects of SCT that were separable from ADHD-IN (Becker et al., 2016). Propelled by the meta-analytic findings, the SCT module of the CABI (previously called the CADBI) was revised in an effort to move the field towards a standard symptom set for assessing SCT in children. An initial study collected teacher ratings of the revised SCT measure in a sample of children from the United States and found that 15 of the 16 items demonstrated excellent convergent and discriminant validity with ADHD-IN, as well as preliminary evidence of external validity with academic and social impairment (Becker, Burns, et al., 2017). The current study replicated and extended these findings in multiple important ways. First, the same 15 SCT items demonstrated convergent and discriminant validity from ADHD-IN as in the initial validation study examining the revised CABI SCT module (Becker, Burns, et al., 2017). Second, and perhaps most crucially, the same 15 items demonstrated convergent and discriminant validity across mother, father, and teacher informants. Third, we significantly extended the external validity evidence for the revised CABI SCT module, with the association between SCT and external correlates examined for mothers, fathers, and teachers. Fourth, the previous study examining this measure included children from four schools in a single school district in the United States, whereas the current study included children from 32 schools in Spain, providing a larger sample of children from a different continent and cultural group. In short, findings from the current study provide strong support for moving the field toward a standard symptom set for assessing SCT in children.
Of the 16 SCT items evaluated in this study, only the “low motivation to complete tasks (e.g., apathetic)” item failed to demonstrate convergent and discriminant validity with ADHD-IN. This item loaded with the ADHD-IN factor, just as it did in the initial study using teacher ratings in the United States (Becker, Burns, et al., 2017). It is worth noting that although this item was identified in the meta-analysis as an optimal item for assessing SCT, it was the optimal item with the fewest number of studies contributing to its meta-analytic evaluation and also had the weakest overall loading on an SCT factor across raters (Becker et al., 2016). Our findings across mother, father, and teacher ratings, in tandem with the findings from the United States study (Becker, Burns, et al., 2017), indicate that low motivation and apathy are likely not optimal for characterizing the SCT construct. The remaining 15 items, however, appear well-positioned to be part of a standard symptom set for assessing SCT across raters. Further, we found SCT symptoms to have similar measurement properties across mother and father ratings, as well as perhaps between parent and teacher ratings. These findings are notable given the importance of using a multi-informant assessment approach in child and adolescent mental health (De Los Reyes et al., 2015).
The 15-item SCT factor was also found in the present study to be associated with a number of external correlates, including higher internalizing symptoms, increased shyness, and global impairment in social functioning and academics. In structural regression analyses that controlled for sex and ADHD-IN, SCT remained associated with increased internalizing symptoms, greater academic impairment, and greater social impairment. In addition, when controlling for ADHD-IN, SCT was unassociated with externalizing behaviors or associated with fewer externalizing behaviors. These findings replicate previous findings (Barkley, 2014; Becker, 2017; Becker et al., 2016; Mueller et al., 2014) and extend them to a study using a multi-informant, multi-setting design.
In addition, we found SCT to be uniquely associated with increased conflicted shyness whereas ADHD-IN was unassociated with shyness when controlling for SCT. Conversely, ADHD-IN was uniquely associated with increased peer rejection whereas SCT was unassociated with peer rejection when controlling for ADHD-IN. This type of double dissociation is important for validating the SCT construct as distinct from ADHD (Barkley, 2014) and indicates that SCT and ADHD-IN may have different etiologies and outcomes linked to social impairment. Our findings are consistent with previous studies showing SCT to be uniquely associated with increased peer withdrawal, isolation, and loneliness (Becker, Garner, et al., 2017; Becker, Luebbe, & Joyce, 2015; Carlson & Mann, 2002; Marshall, Evans, Eiraldi, Becker, & Power, 2014; Willcutt et al., 2014) and extend these findings to shyness specifically. A preliminary study suggests that SCT is associated with punishment sensitivity (Becker et al., 2013), and both shyness and punishment sensitivity are associated with the temperament domain of behavioral inhibition which itself has a robust literature base informed by neurobiology and developmental theory (Fox, Henderson, Marshall, Nichols, & Ghera, 2005; Henderson, Pine, & Fox, 2015). If SCT is indeed related to behavioral inhibition (a hypothesis yet to be formally tested), new research directions should quickly follow that will shed light on the possible etiology, biology, socio-cognitive processes, and impairments of SCT across childhood in clinical and nonclinical samples. Furthermore, given the shy and withdrawn behaviors associated with SCT, social skills training interventions should be considered as possible treatment approach for children who display elevated SCT symptomatology (Becker, Garner et al., 2017).
Finally, despite calls to examine SCT in children with medical conditions (Becker, 2013), few studies have done so. Our study provides preliminary evidence of SCT being associated with increased likelihood of having a parent-reported medical problem (with asthma the most commonly reported medical problem reported in our sample). Previous studies have found elevated SCT in children with prenatal alcohol/tobacco exposure (Camprodon-Rosanas et al., 2017; Graham et al., 2013) and children with leukemia (Reeves et al., 2007). Our findings, which should be considered preliminary given the use of a broad measure of parent-reported medical diagnosis, join a small but growing body of literature pointing to the need for further examine SCT in the context of prenatal exposures and medical conditions.
Limitations and Future Directions
Despite the strengths of this study described above and the promise of the 15 items identified in this study as a standard symptom set for assessing SCT, more work remains and several limitations are important to note. First, this was a cross-sectional study and we were therefore unable to examine the longitudinal stability or predictive validity of our 15-item SCT measure. There is some evidence that SCT is a stable construct over time (perhaps increasing as children enter adolescence; Leopold et al., 2016; Preszler et al., 2017), though more studies are needed, particularly with a standard symptom set of SCT. The lack of longitudinal information remains a major gap in our knowledge base regarding the prospective consequences of – as well as predictors of – SCT (Becker, 2017; Becker & Barkley, in press; Becker et al., 2016; Mueller et al., 2014). Given the cross-sectional design of our study, we cannot make causal claims regarding the associations identified. Second, in order to recruit a large number of participants for measurement development analyses, we were limited to rating scale measures of functioning and impairment. Multi-method studies examining the 15-item SCT measure in relation to external correlates will be highly informative in order to evaluate whether SCT is associated with clinician-determined internalizing diagnoses, fewer aggressive and antisocial behaviors (e.g., contact with the juvenile justice system), peer reports of social functioning (e.g., sociometric nominations), and lower academic achievement and lower grades. Third, we used a school/community-based sample in this study, which is important for initial psychometric work (Barkley, 2013, 2014), though it will be important to evaluate the revised CABI SCT module in clinical samples, including ADHD, anxiety/depression, autism spectrum disorder (ASD), and sleep-disordered samples. Fourth, our examination of the revised CABI SCT module was limited to school-aged children (as was the initial study using teacher ratings of children in the United States; Becker, Burns et al., 2017), and additional studies will be needed to determine whether the same 15 items identified in these studies are optimal for assessing SCT in younger children and adolescents. Finally, we are unable to determine if the parents and teachers who chose to participate differed from the parents and teachers who did not participate, though the large sample size recruited from 32 schools increases the confidence in the generalizability of the findings.
It should also be noted that the “sluggish cognitive tempo” term is not optimal and has been critiqued for being both misleading (in implying a cognitive etiology that is not actually known) and derogatory/offensive (Barkley, 2014, 2016; Becker & Barkley, in press). It is clear that a change in terminology will be needed as sufficient empirical evidence emerges that can guide such a decision. Although our study was not designed to examine possibly mechanisms underlying SCT, we hope that such research emerges in the near future and that our rating scale will be helpful in such efforts.
Conclusion
Over 150 items have historically been used when assessing SCT, and while many of these items have been variations on a theme (e.g., daydreaming, daydreams, daydreamer), there is no agreed-upon set of SCT symptoms that readily allows for comparison of findings across studies (Becker et al., 2016). The primary objective of this study was to evaluate whether a standard symptom set, based on meta-analytic findings, could be identified across mother, father, and teacher ratings in a large, community-based sample of children in Spain. The 15 items identified in this study, identical to the 15 items identified in a recent study of children in the United States (Becker, Burns et al., 2017), appear well-positioned as a standard symptom set to be used across studies and parent/teacher informants. More studies are surely needed before an evidence-based assessment of SCT can be established, but the items in the present study using the CABI SCT module are a springboard towards reaching that goal.
Supplementary Material
Acknowledgments
This research was supported by a grant from the Ministry of Economy and Competitiveness of Spanish Government under award number PSI2014-52605-R (AEI/FEDER, UE) and a predoctoral fellowship co-financed by MINECO (Spanish Government) and the European Social Fund (BES-2015-075142). Stephen Becker is supported by award number K23MH108603 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH) or the Spanish Government. We thank Cristina Trias for assistance with the study.
Footnotes
The correlation and regression analyses were repeated across sources. The findings were similar to the within source analyses (see supplemental tables for the across source results).
Contributor Information
Belén Sáez, University of the Balearic Islands, Palma, Spain.
Mateu Servera, University of the Balearic Islands, Palma, Spain.
Stephen P. Becker, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Ave MLC 10006, Cincinnati, OH 45251
G. Leonard Burns, Washington State University, Pullman, WA.
References
- Asparouhov T, & Muthén B (2009). Exploratory structural equation modeling. Structural Equation Modeling-a Multidisciplinary Journal, 16, 397–438. doi: 10.1080/10705510903008204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child and Adolescent Psychology, 42, 161–173. doi: 10.1080/15374416.2012.734259 [DOI] [PubMed] [Google Scholar]
- Barkley RA (2014). Sluggish cognitive tempo (concentration deficit disorder?): Current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42, 117–125. doi: 10.1007/s10802-013-9824-y [DOI] [PubMed] [Google Scholar]
- Barkley RA, (2016). Sluggish cognitive tempo: A (misnamed) second attention disorder? Journal of the American Academy of Child and Adolescent Psychiatry, 55, 157–158. doi: 10.1016/j.jaac.2015.12.007 [DOI] [PubMed] [Google Scholar]
- Bauermeister JJ, Barkley RA, Bauermeister JA, Martinez JV, & McBurnett K (2012). Validity of the sluggish cognitive tempo, inattention, and hyperactivity symptom dimensions: Neuropsychological and psychosocial correlates. Journal of Abnormal Child Psychology, 40, 683–697. doi: 10.1007/s10802-011-9602-7 [DOI] [PubMed] [Google Scholar]
- Becker SP (2013). Topical review: Sluggish cognitive tempo: Research findings and relevance for pediatric psychology. Journal of Pediatric Psychology, 38, 1051–1057. doi: 10.1093/jpepsy/jst058 [DOI] [PubMed] [Google Scholar]
- Becker SP (2017). “For some reason I find it hard to work quickly”: Introduction to the Special Issue on sluggish cognitive tempo. Journal of Attention Disorders, 21, 615–622. doi: 10.1177/1087054717692882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, & Barkley RA (in press). Sluggish cognitive tempo In Banaschewski T, Coghill D, & Zuddas A (Eds.), Oxford textbook of attention deficit hyperactivity disorder. Oxford, England: Oxford University Press. [Google Scholar]
- Becker SP, Burns GL, Schmitt AP, Epstein JN, & Tamm L (2017). Toward establishing a standard symptom set for assessing sluggish cognitive tempo in children: Evidence from teacher ratings in a community sample. Assessment. Advance online publication. doi: 10.1177/1073191117715732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Fite PJ, Garner AA, Greening L, Stoppelbein L, & Luebbe AM (2013). Reward and punishment sensitivity are differentially associated with ADHD and sluggish cognitive tempo symptoms in children. Journal of Research in Personality, 47, 719–727. doi: 10.1016/j.jrp.2013.07.001 [DOI] [Google Scholar]
- Becker SP, Garner AA, Tamm L, Antonini TN, & Epstein JN (2017). Honing in on the social difficulties associated with sluggish cognitive tempo in children: Withdrawal, peer ignoring, and low engagement. Journal of Clinical Child and Adolescent Psychology. Advance online publication. doi: 10.1080/15374416.2017.1286595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, & Langberg JM (2014). Attention-deficit/hyperactivity disorder and sluggish cognitive tempo dimensions in relation to executive functioning in adolescents with ADHD. Child Psychiatry and Human Development, 45, 1–11. doi: 10.1007/s10578-013-0372-z [DOI] [PubMed] [Google Scholar]
- Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA,…Willcutt EG (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 163–178. doi: 10.1016/j.jaac.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, Fite PJ, Stoppelbein L, & Greening L (2014). Sluggish cognitive tempo in psychiatrically hospitalized children: Factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. Journal of Abnormal Child Psychology, 42, 49–62. doi: 10.1007/s10802-013-9719-y [DOI] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, & Joyce AM (2015). The Child Concentration Inventory (CCI): Initial validation of a child self-report measure of sluggish cognitive tempo. Psychological Assessment, 27, 1037–1052. doi: 10.1037/pas0000083 [DOI] [PubMed] [Google Scholar]
- Becker SP, Marshall SA, & McBurnett K (2014). Sluggish cognitive tempo in abnormal child psychology: an historical overview and introduction to the special section. Journal of Abnormal Child Psychology, 42, 1–6. doi: 10.1007/s10802-013-9825-x [DOI] [PubMed] [Google Scholar]
- Belmar M, Servera M, Becker SP, & Burns GL (2017). Validity of sluggish cognitive tempo in South America: An initial examination using mother and teacher ratings of Chilean children. Journal of Attention Disorders, 21, 667–672. doi: 10.1177/1087054715597470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernad MD, Servera M, Becker SP, & Burns GL (2016). Sluggish cognitive tempo and ADHD inattention as predictors of externalizing, internalizing, and impairment domains: A 2-year longitudinal study. Journal of Abnormal Child Psychology, 44, 771–785. doi: 10.1007/s10802-015-0066-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernad MD, Servera M, Grases G, Collado S, & Burns GL (2014). A cross-sectional and longitudinal investigation of the external correlates of sluggish cognitive tempo and ADHD-inattention symptoms dimensions. Journal of Abnormal Child Psychology, 42, 1225–1236. doi: 10.1007/s10802-014-9866-9 [DOI] [PubMed] [Google Scholar]
- Brown TA (2015). Confirmatory factor analysis for applied research (2nd Ed.). New York: Guilford. [Google Scholar]
- Burns GL, Becker SP, Servera M, Bernad MD, & García-Banda G (2017). Sluggish cognitive tempo and attention-deficit/hyperactivity disorder (ADHD) inattention in the home and school contexts: Parent and teacher invariance and cross-setting validity. Psychological Assessment, 29, 209–220. doi: 10.1037/pas0000325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Lee S, Servera M, McBurnett K, & Becker SP (2015a). Child and Adolescent Behavior Inventory - Parent Version 1.0. Pullman, WA: Author. [Google Scholar]
- Burns GL, Lee S, Servera M, McBurnett K, & Becker SP (2015b). Child and Adolescent Behavior Inventory - Teacher Version 1.0. Pullman, WA: Author. [Google Scholar]
- Burns GL, Servera M, Bernad MD, Carrillo JM, & Cardo E (2013). Distinctions between sluggish cognitive tempo, ADHD-IN, and depression symptom dimensions in Spanish first-grade children. Journal of Clinical Child and Adolescent Psychology, 42, 796–808. doi: 10.1080/15374416.2013.838771 [DOI] [PubMed] [Google Scholar]
- Camprodon-Rosanas E, Ribas-Fitó N, Batlee-Vila S, Persavento C, Alvarez-Pedrerol M, Sunyer J, & Forns J (2017). Sluggish cognitive tempo: Sociodemographic, behavioral, and clinical characteristics in a population of Catalan school children. Journal of Attention Disorders, 21, 632–641. [DOI] [PubMed] [Google Scholar]
- Carlson CL, & Mann M (2002). Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. Journal of Clinical Child and Adolescent Psychology, 31, 123–129. doi: 10.1207/S15374424JCCP3101_14 [DOI] [PubMed] [Google Scholar]
- Coplan RJ, Prakash K, O’Neil K, & Armer M (2004). Do you “want” to play? Distinguishing between conflicted shyness and social disinterest in early childhood. Developmental Psychology, 40, 244–258. doi: 10.1037/0012-1649.40.2.244 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DA, Burgers DE, & Rabinowitz J (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141, 858–900. doi: 10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ (1990). The peer context of troublesome child and adolescent behavior In Leone PE (Ed.), Understanding troubled and troubling youth: Multiple perspectives (pp. 128–153). Thousand Oaks: Sage. [Google Scholar]
- Fenollar Cortés J, Servera M, Becker SP, & Burns GL (2017). External validity of ADHD inattention and sluggish cognitive tempo dimensions in Spanish children with ADHD. Journal of Attention Disorders, 21, 655–666. doi: 10.1177/1087054714548033 [DOI] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, & Ghera MM (2005). Behavioral inhibition: Linking biology and behavior within a developmental framework. Annual Review of Psychology, 56, 235–262. doi: 10.1146/annurev.psych.55.090902.141532 [DOI] [PubMed] [Google Scholar]
- Graham DM, Crocker N, Deweese BN, Roesch SC, Coles CD, Kable JA,…CIFASD. (2013). Prenatal alcohol exposure, attention-deficit/hyperactivity disorder, and sluggish cognitive tempo. Alcoholism: Clinical and Experimental Research, 37, E338–E346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson HA, Pine DS, & Fox NA (2015). Behavioral inhibition and developmental risk: A dual-processing perspective. Neuropsychopharmacology, 40, 207–224. doi: 10.1038/npp.2014.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsley J, & Mash EJ (2005). Introduction to the special section on developing guidelines for the evidence-based assessment (EBA) of adult disorders. Psychological Assessment, 17, 251–255. [DOI] [PubMed] [Google Scholar]
- Khadka G, Burns GL, & Becker SP (2016). Internal and external validity of sluggish cognitive tempo and ADHD inattention dimensions with teacher ratings of Nepali children. Journal of Psychopathology and Behavioral Assessment, 38, 433–442. doi: 10.1007/s10862-015-9534-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Schaughency EA, Atkins MS, Murphy HA, Hynd G, . . . Lorys-Vernon A (1988). Dimensions and types of attention deficit disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 27, 330–335. doi: 10.1097/00004583-198805000-00011 [DOI] [PubMed] [Google Scholar]
- Lee S, Burns GL, Beauchaine TP, & Becker SP (2016). Bifactor latent structure of attention-deficit/hyperactivity disorder (ADHD)/oppositional defiant disorder (ODD) symptoms and first-order latent structure of sluggish cognitive tempo symptoms. Psychological Assessment, 28, 917–928. [DOI] [PubMed] [Google Scholar]
- Lee S, Burns GL, & Becker SP (2016). Toward establishing the transcultural validity of sluggish cognitive tempo: Evidence from a sample of South Korean children. Journal of Clinical Child and Adolescent Psychology. Advance online publication. doi: 10.1080/15374416.2016.1144192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Burns GL, & Becker SP (2017). Can sluggish cognitive tempo be distinguished from ADHD inattention in very young children? Evidence from a sample of Korean preschool children. Journal of Attention Disorders, 21, 623–631. doi: 10.1177/1087054716680077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Burns GL, Snell J, & McBurnett K (2014). Validity of the sluggish cognitive tempo symptom dimension in children: Sluggish cognitive tempo and ADHD-inattention as distinct symptom dimensions. Journal of Abnormal Child Psychology, 42, 7–19. doi: 10.1007/s10802-013-9714-3 [DOI] [PubMed] [Google Scholar]
- Leopold DR, Christopher ME, Burns GL, Becker SP, Olson RK, & Willcutt EG (2016). Attention-deficit/hyperactivity disorder and sluggish cognitive tempo throughout childhood: Temporal invariance and stability from preschool through ninth grade. Journal of Child Psychology and Psychiatry, 57, 1066–1074. doi: 10.1111/jcpp.12505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD (2013). Longitudinal structural equation modeling. New York: Guilford. [Google Scholar]
- Marshall SA, Evans SW, Eiraldi RB, Becker SP, & Power TJ (2014). Social and academic impairment in youth with ADHD, predominately inattentive type and sluggish cognitive tempo. Journal of Abnormal Child Psychology, 42, 77–90. doi: 10.1007/s10802-013-9758-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBurnett K, Pfiffner LJ, & Frick PJ (2001). Symptom properties as a function of ADHD type: an argument for continued study of sluggish cognitive tempo. Journal of Abnormal Child Psychology, 29, 207–213. [DOI] [PubMed] [Google Scholar]
- McBurnett K, Villodas M, Burns GL, Hinshaw SP, Beaulieu A, & Pfiffner LJ (2014). Structure and validity of sluggish cognitive tempo using an expanded item pool in children with attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 42, 37–48. [DOI] [PubMed] [Google Scholar]
- Mueller AK, Tucha L, Koerts J, Groen Y, Lange KW, & Tucha O (2014). Sluggish cognitive tempo and its neurocognitive, social and emotive correlates: A systematic review of the current literature. Journal of Molecular Psychiatry, 2, 5. doi: 10.1186/2049-9256-2-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2017). Mplus user’s guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Penny AM, Waschbusch DA, Klein RM, Corkum P, & Eskes G (2009). Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychological Assessment, 21, 380–389. doi: 10.1037/a0016600 [DOI] [PubMed] [Google Scholar]
- Preszler J, Burns GL, Litson K, Geiser C, Servera M, & Becker SP (2017). How consistent is sluggish cognitive tempo across occasions, sources, and settings? Evidence from latent state-trait modeling. Assessment. Advance online publication. 1073191116686178. doi: 10.1177/1073191116686178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seijas R, Servera M, García-Banda G, Barry CT, & Burns GL (2017). Evaluation of a four-item DSM-5 limited prosocial emotions specifier scale within and across settings with Spanish children. Psychological Assessment. Advance online publication. doi: 10.1037/pas0000496 [DOI] [PubMed] [Google Scholar]
- Reeves CB, Palmer S, Gross AM, Simonian SJ, Taylor L, Willingham E, & Mulhern RK (2007). Brief report: Sluggish cognitive tempo among pediatric survivors of acute lymphoblastic leukemia. Journal of Pediatric Psychology, 32, 1050–1054. doi: 10.1093/jpepsy/jsm063 [DOI] [PubMed] [Google Scholar]
- Servera M, Bernad MD, Carrillo JM, Collado S, & Burns GL (2016). Longitudinal correlates of sluggish cognitive tempo and ADHD-inattention symptom dimensions with Spanish children. Journal of Clinical Child and Adolescent Psychology, 45, 632–641. doi: 10.1080/15374416.2015.1004680 [DOI] [PubMed] [Google Scholar]
- Smith ZR, & Langberg JM (2017). Predicting academic impairment and internalizing psychopatholgoy using a multidimensional framework of sluggish cognitive tempo with parent- and adolescent reports. European Child and Adolescent Psychiatry. Advance online publication. doi: 10.1007/s00787-017-1003-1 [DOI] [PubMed] [Google Scholar]
- Tamm L, Garner AA, Loren REA, Epstein JN, Vaughn AJ, Ciesielski HA, & Becker SP (2016). Slow sluggish cognitive tempo symptoms are associated with poorer academic performance in children with ADHD. Psychiatry Research, 242, 251–259. doi: 10.1016/j.psychres.2016.05.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Chhabildas N, Kinnear M, DeFries JC, Olson RK, Leopold DR,…Pennington BF (2014). The internal and external validity of sluggish cognitive tempo and its relation with DSM-IV ADHD. Journal of Abnormal Child Psychology, 42, 21–35. doi: 10.1007/s10802-013-9800-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.